MOD 5 - Pelvic Fractures – Imaging, Stability, Types, Treatment & Complications
1/32
Earn XP
Description and Tags
Question-and-Answer flashcards reviewing pelvic fracture stability, imaging, subtypes, mechanisms, treatments, and complications.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms

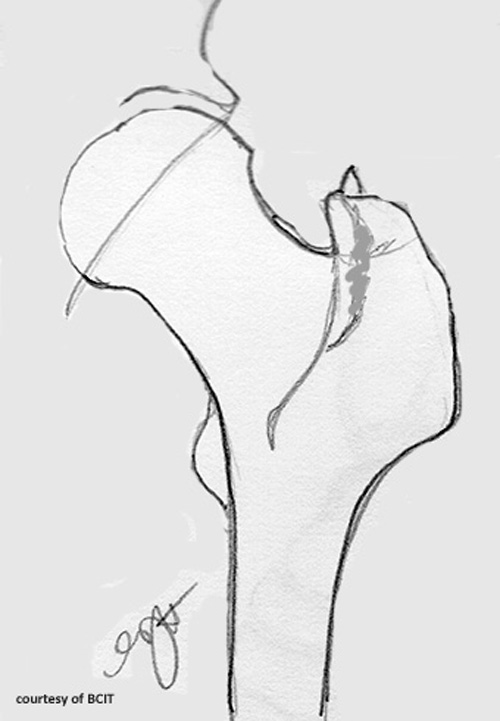
What anatomical features make the pelvis structurally stable?
Strong bones, robust ligaments, and surrounding muscles forming a ring-like structure.
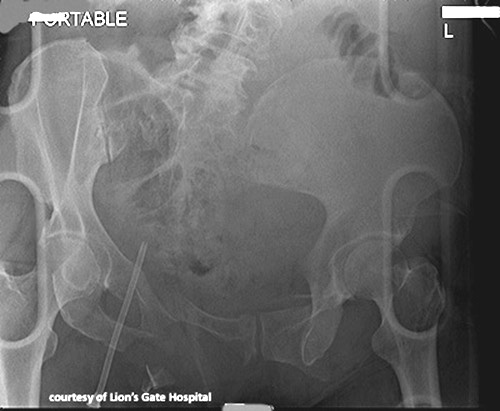
Which standard radiographic views are used to evaluate pelvic fractures?
Anteroposterior (AP), inlet, outlet, and Judet views.
On an inlet pelvic view, what injuries are best visualized?
Posterior displacement of the pelvic ring and widening of the pubic symphysis.
What displacement is highlighted on an outlet pelvic view?
Vertical (cranial or caudal) shift of one hemipelvis relative to the other.
Why are Judet views ordered in pelvic trauma?
To assess acetabular fractures and better define pelvic-ring fracture patterns for surgical planning.
How is a stable pelvic fracture defined?
A single-site fracture that can tolerate normal physiologic stress without deforming the pelvic ring.
Give two common examples of stable pelvic fractures.
Isolated sacral fractures and pubic rami fractures.
What level of trauma usually causes a stable pelvic fracture?
Moderate-energy trauma.
Standard treatment approach for most stable pelvic fractures?
Closed or open reduction with possible internal fixation using screws or plates.
Name two postoperative complications associated with stable pelvic fracture surgery.
Bladder dysfunction and postoperative bowel obstruction.
Which patient population most frequently sustains pelvic avulsion fractures?
Young athletes engaged in high-intensity sports.
Mechanism producing a pelvic avulsion fracture?
Forceful muscle contraction avulsing (pulling off) a small fragment of bone.
List four common anatomical sites of avulsion fractures around the pelvis.
ASIS - (Sartorius), AIIS (Rectus), ischial tuberosity (hamstring), and the greater or lesser trochanter (hip abductor)

Typical management for pelvic avulsion fractures?
Conservative care—rest, activity modification, and gradual return to sports (non-operative).
Do pelvic avulsion fractures usually lead to long-term complications?
No; they generally heal uneventfully.
Definition of an unstable pelvic fracture?
Disruption in both the anterior and posterior elements of the pelvic ring.
What life-threatening complication is common with unstable pelvic fractures?
Significant blood loss resulting in haemorrhagic shock.
Name the four mechanistic subtypes of unstable pelvic fractures.
Anteroposterior compression, lateral compression, vertical shear, and combined mechanical injuries.
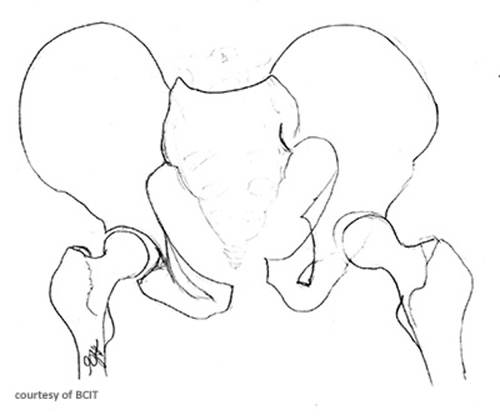
Radiographic hallmark of an anteroposterior compression ("open-book") fracture?
Widening of the pubic symphysis and sacroiliac (SI) joints.
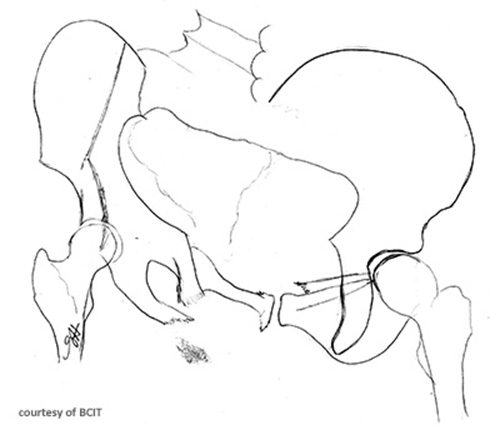
Typical injury mechanism for an open-book ((Anteroposterior compression)) pelvic fracture?
High anteroposterior force, such as hitting a motorcycle tank or falling forward off a horse.

Treatment guideline when pubic symphyseal diastasis is <2.5 cm and no GU injury exists?
Non-operative management with pelvic binder or bed rest.
Management when pubic symphysis diastasis exceeds 2.5 cm or genitourinary trauma is present?
Surgical fixation often combined with external pelvic stabilization.
List three major complications of open-book (Anteroposterior compression) pelvic fractures.
Massive haemorrhage, genitourinary injuries, and rectal injury/contamination.
Describe the bone movement in a lateral compression pelvic fracture.
The impacted hemipelvis is forced inward, folding or buckling the ilium.

Common associated fractures seen with lateral compression injuries?
Superior and inferior pubic rami fractures, sacral fractures, and SI joint widening.
Usual cause of a lateral compression pelvic fracture?
Side-impact collisions, such as a T-bone car accident.
Why are vertical shear (Malgaigne) fractures particularly dangerous?
They completely disrupt the pelvic floor, leading to severe internal bleeding.

Most frequent mechanism producing a vertical shear pelvic injury?
Axial load from a fall from significant height.

Primary treatment components for a vertical shear fracture?
Operative realignment/stabilization and aggressive blood resuscitation.
Two long-term complications often seen after vertical shear fractures.
Chronic back/leg pain with limp and lumbosacral nerve damage.
What generates a combined mechanical pelvic fracture?
Forces applied from multiple directions, commonly in high-energy motor-vehicle accidents.
Besides pelvic stabilization, what is a parallel treatment priority in combined mechanical injuries?
Management of associated head, thoracic, abdominal, or extremity trauma.
Possible chronic sequelae following combined mechanical pelvic fractures?
Persistent pelvic pain and neurologic deficits affecting lower extremities.