NPTE: Stroke & TBI
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
what is a CVA?
brain attack, when blood does not reach the brain
what are two types of stroke?
cerebral stroke
brain stem stroke
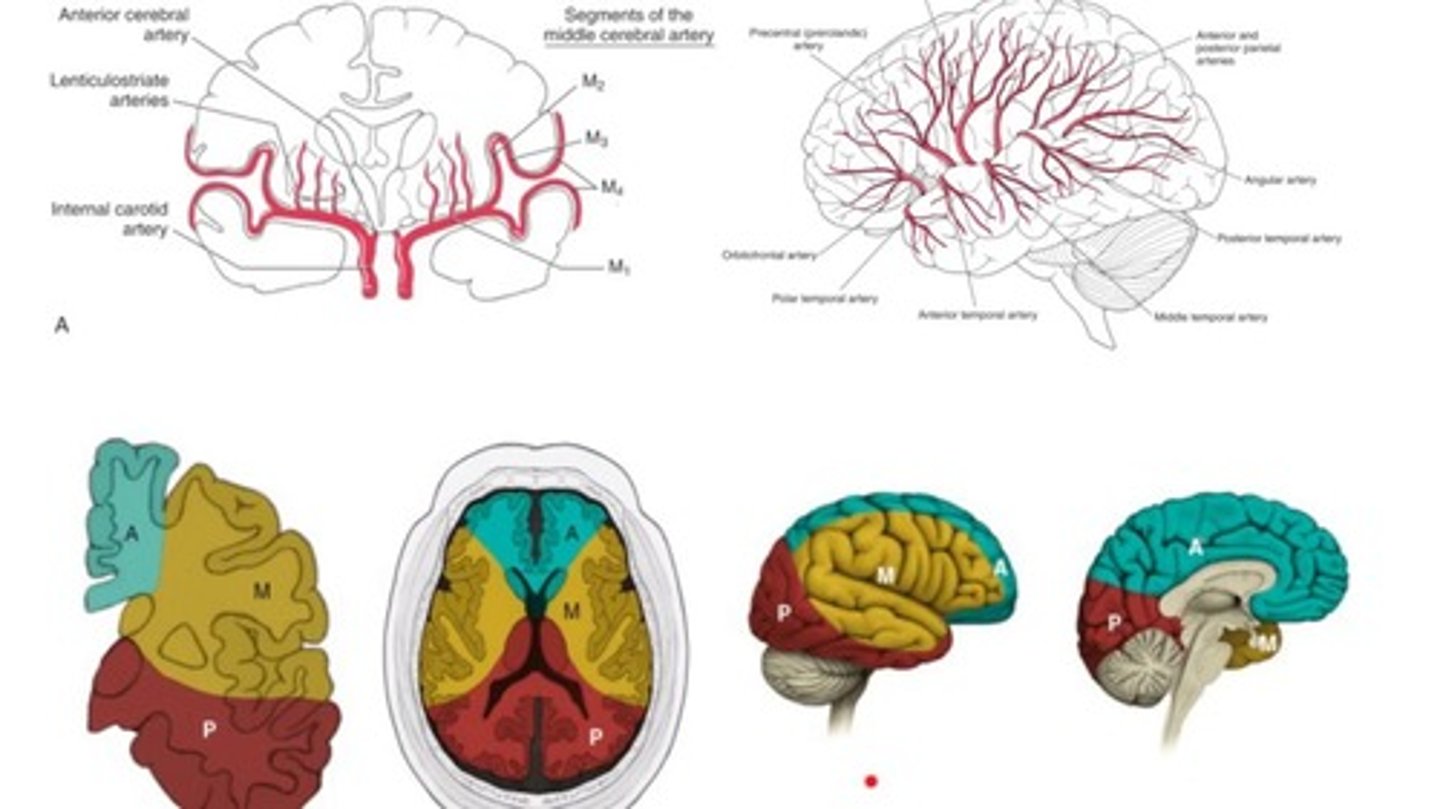
what are the three main arteries into the cerebrum?
MCA: middle
ACA: anterior
PCA: posterior
where does the middle cerebral artery supply blood?
lateral part of the brain
where does the ACA supply blood?
inner/medial side of the brain
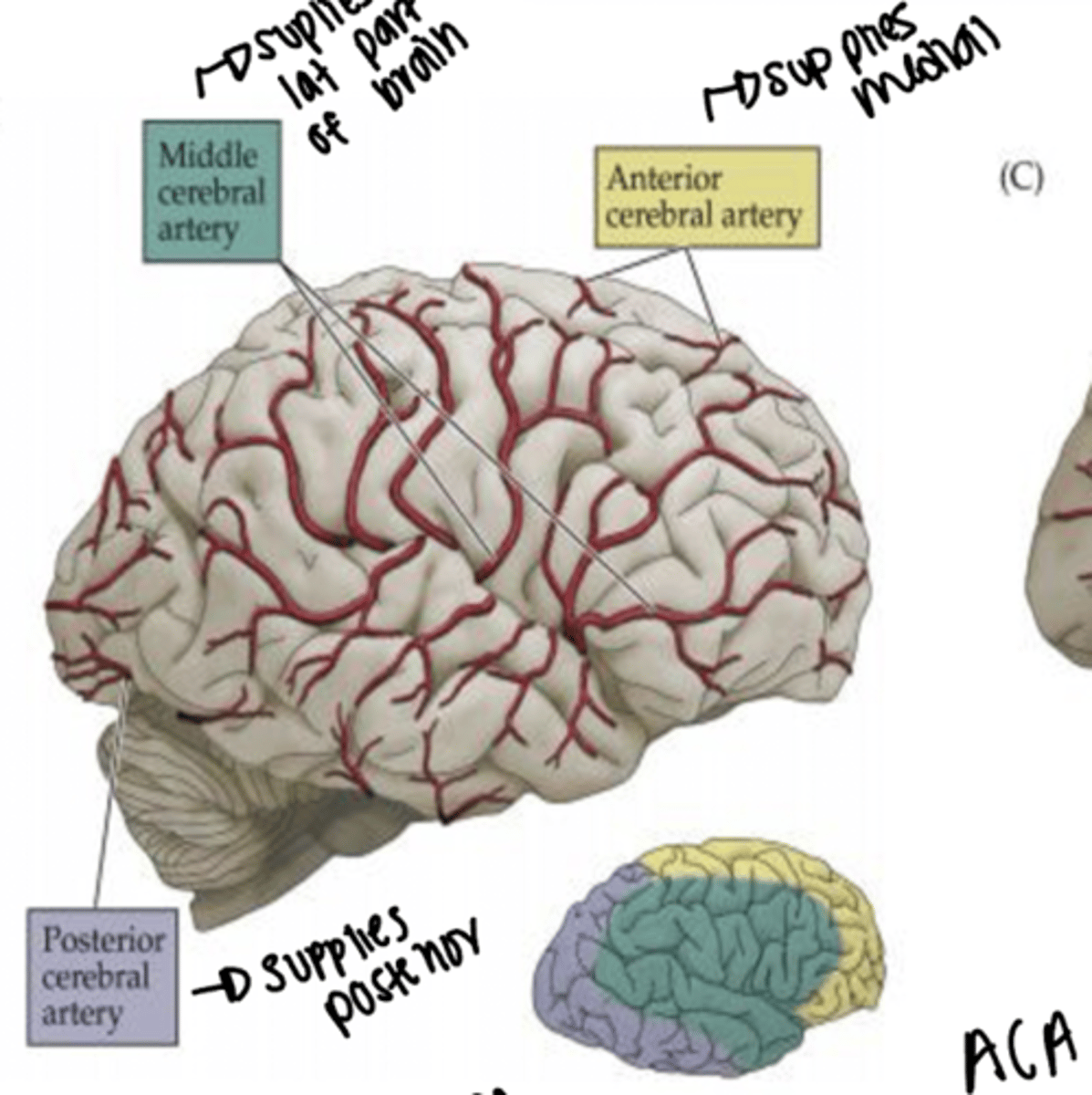
where does the PCA supply blood?
posterior side of the brain
what artery supplies outside of brain? Inside?
middle
anterior
what are the two types of stroke?
ischemic
hemorrhagic
what is an ischemic stroke?
Occurs when a clot blocks or impairs blood flow, depriving the brain of essential oxygen and nutrients
blood flow obstructed
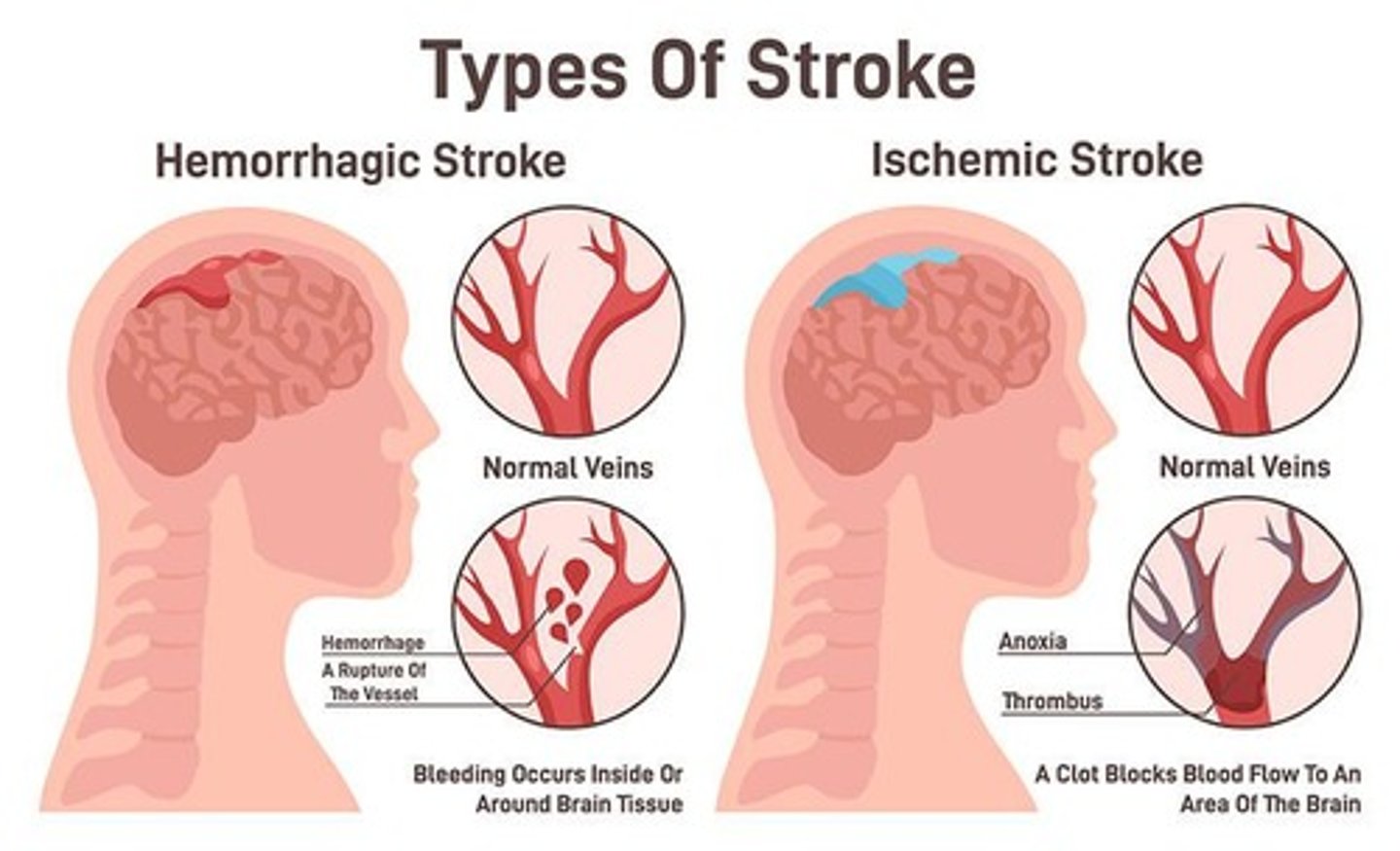
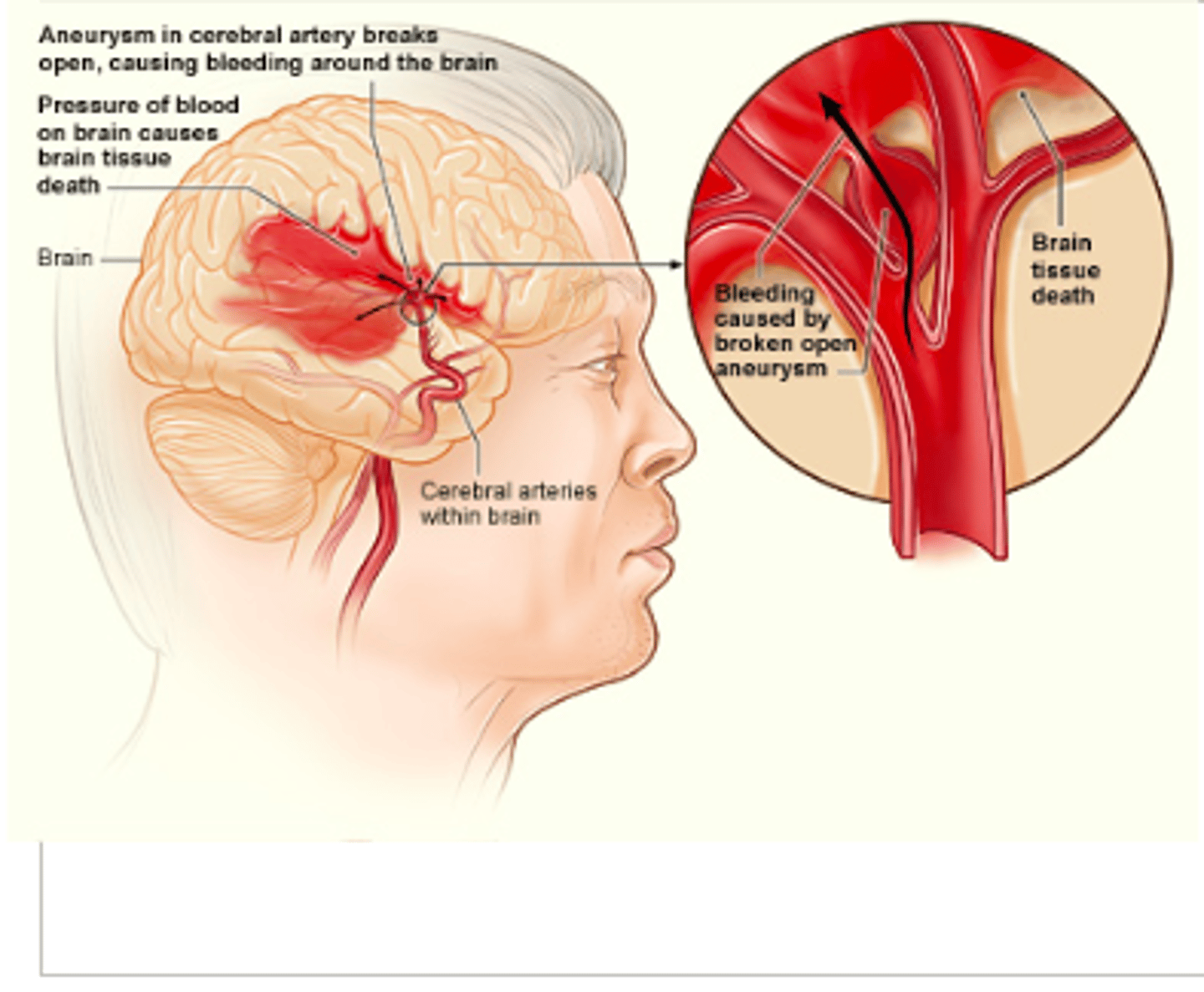
What is a hemmorhagic stroke?
Occurs when blood vessels rupture, causing leakage of blood in or around the brain
worse prognosis due to a ruptured blood vessel leaks blood into the brain
What is a homonculus?
"tiny man" model mapping the body according to the sensory space each part takes up in the cerebral cortex
if someone has an MCA stroke, what is going to be more affected, LE or UE?
UEs and face
if someone has an ACA stroke, what is going to be more affected, LE or UE?
LEs
what are signs and symptoms of ACA stroke?
-Contralateral hemiparesis (LE)
-Contralateral hemisensory loss (LE)
-Urinary incontinence
-Problems with imitation, bimanual tasks, apraxia
-Slowness, delay, motor inaction
-Contralateral grasp reflex, sucking reflex
ACA >>> ABCD >> baby/kid
what are the signs and symptoms of MCA stroke?
-Contralateral hemiparesis (UE and face)
-Contralateral hemisensory loss (UE and face)
-Language speech impairments - Broca, Wernicke, Global aphasia (L MCA)
-Perceptual disorders - e.g., Unilateral neglect (R MCA)
-Contralateral homonymous hemianopsia
Acronym: MPH
what is apraxia?
disorder characterized by the inability to perform purposeful movements or gestures, despite having the physical ability and desire to do so
what is brocas aphasia? where is the lesion? what is the treatment?
Expressive/ Non-fluent aphasia: FRONTAL LOBE
• Patient has slow, hesitant speech
• Treatment: Yes/No questions
what is Wernicke's aphasia? where is the lesion? what is the treatment?
aphasia/Receptive/Fluent aphasia: TEMPORAL LOBE
• Patient cannot comprehend
• Word salad
• Treatment: Gestures and demonstration
what is global aphasia?
wernicke's and broca's aphasia put together
left hemisphere is usually called the _____ hemisphere
dominant
if there is a lesion to the superior branch of MCA, what type of aphasia is present?
brocas
if there is a lesion to the inferior branch of MCA, what type of aphasia is present?
Wernickes
what type of stroke can cause perceptual deficit: unilateral neglect?
R MCA stroke
what is unilateral neglect?
lack of awareness of the weak side of the body post stroke
Patient ignores objects in one half of visual field in perception and imagery
• Referred to as unilateral spatial neglect, hemi-inattention, hemineglect, and unilateral visual
inattention.
what do you want to do if someone presents with unilateral neglect?
Encourage awareness and use of the environment on the hemiparetic side and use of the hemiparetic extremities
Active visual scanning > turning of the head and axial
trunk rotation to the more involved side
What is anosognosia?
• Anosognosia is defined as a lack of awareness, or denial, of a paretic extremity as belonging to the person, or lack of insight concerning, or denial of, paralysis and disability.
• E.g., patient maintains that there is nothing wrong and may disown the paralyzed limbs and refuse to accept responsibility for them. Patient may claim that the limb has a mind of its own or that it was left at home or in a closet.
What is somatoagnosia?
• Somatoagnosia, or impairment in body scheme, is a lack of awareness of the body structure and the relationship of body parts to oneself or to others.
• Also referred to as Autopagnosia or simply body agnosia.
• Difficulty following instructions that require distinguishing body parts and may be unable to imitate movements of the therapist.
• May have difficulty performing transfer activities because he or she does not perceive the meaning of terms related to body parts, e.g., Pivot on your leg and reach for the armrest with your hand.
• Difficulty dressing.
• Hard time participating in exercises that require some body parts to be moved in relation to other body parts, E.g., Bring your arm across your chest and touch your shoulder.
• Lesion area- Dominant parietal lobe.
What is Right-left discrimination?
Inability to identify right and left sides of one's body or that of the examiner.
• Inability to execute movements in response to verbal commands that include the terms right and left.
• Often unable to imitate movements.
What is finger agnosia?
• Inability to identify the fingers of one's own hands or of the hands of examiner.
• Characterized by difficulty in naming the fingers on command, identifying which finger was touched, and, by some definitions, mimicking finger movements.
Spatial relation impairment:
Figure-ground discrimination
• Inability to visually distinguish a figure from the background in which it is embedded
• Patient has difficulty ignoring irrelevant visual stimuli and cannot select the appropriate cue to which to respond. This may lead to distractibility, resulting in a shortened attention span, frustration, and decreased independent and safe functioning.
• E.g., patient cannot locate items in a pocketbook or drawer, locate buttons on a shirt, or distinguish the
armhole from the remainder of a solid-colored shirt.
Spatial relation impairment:
Form discrimination
• Impairment in form discrimination is the inability to perceive or attend to subtle differences in form and shape.
• Patient is likely to confuse objects of similar shape or not to recognize an object placed in an unusual position.
• Patient may confuse a pen with a toothbrush, a vase with a water pitcher, a cane with a crutch
Spatial relation impairment:
Spatial relations
• Inability to perceive the relationship of one object in space to another object, or to oneself. This may lead to, or compound, problems in constructional tasks and dressing.
• Crossing the midline may be a problem for patients with spatial relations deficits.
• Spatial relations skills are required to manage most ADL.
• e.g., patient might find difficult to place the cutlery, plate, and spoon in the proper position when setting the table, unable to tell the time from a clock because of difficulty in perceiving the relative positions of the hands, patient may have difficulty learning the position his or her arms, legs, and trunk in relation to
the wheelchair to prepare for transferring.
Spatial relation impairment:
Position in space
• Inability to perceive and to interpret spatial concepts such as up, down, under, over, in, out, in front of, and behind.
• e.g., if patient is asked to raise the arm "above" the head during the ROM activities or is asked to place the feet "on" the footrests, the patient may behave as if he or she does not know what to do.
Spatial relation impairment:
Topographical discrimination
• Difficulty in understanding and remembering the relationship of one location to another. As a result, the patient is unable to get from one place to another, with or without a map.
• E.g.,pt cannot find a way from his or her room to physical therapy clinic, despite being shown repeatedly.
Spatial relation impairment:
Depth and distance perception
• Experiences inaccurate judgement of direction, distance, and depth.
• E.g., pt may have difficulty navigating stairs, may miss the chair when attempting to sit, or may continue pouring juice once a glass is filled.
Spatial relation impairment
Vertical disorientation
• Refers to a distorted perception of what is vertical.
• Displacement of the vertical position can contribute to disturbance of motor performance, both in posture and in gait.
Visual agnosia
• Most common form of agnosia.
• Inability to recognize familiar objects despite normal function of the eyes and optic tracts.
what are three types of visual agnosia?
1. Simultanagnosia (Balint's syndrome)
▪ Inability to perceive a visual stimulus as a whole
▪ Pt perceives an entire array one part at a time
2. Prosopagnosia
▪ Inability to recognize familiar faces.
3. Color agnosia
▪ Inability to recognize colors; it is not color blindness.
▪ Pt is unable to identify or name colors on command, although color chips can be correctly
paired.
Auditory agnosia
• Inability to recognize nonspeech sounds or to discriminate between them.
• E.g., cannot tell difference between the ring of a doorbell and that of a telephone, or between a dog barking and thunder.
Tactile agnosia or Astereognosis
• Inability to recognize forms by handling them, although tactile, proprioceptive, and thermal sensations may be intact.
• E.g., if a pt is handed a familiar object (key, comb, safety pin) with vision occluded, the pt will fail to recognize it.
Ideational apraxia
• Is a failure in the conceptualization of the
task.
• Inability to perform a purposeful motor
act, either automatically or on command,
because the patient no longer understands
the overall concept of the act, cannot
retain the idea of the task, or cannot
formulate the motor patterns required.
Ideomotor apraxia
• Refers to a breakdown between concepts and
performance.
• There is a disconnection between the idea of a
movement and its motor execution.
• Able to carry out habitual tasks automatically and describe how they are done but is unable to imitate gestures or perform on command.
• E.g., pt is unable to "blow" on command. However, if presented with a bubble wand, the pt will spontaneously blow bubbles.
What is homonymous hemianopsia?
loss of half of the field of view on the same side in both eyes
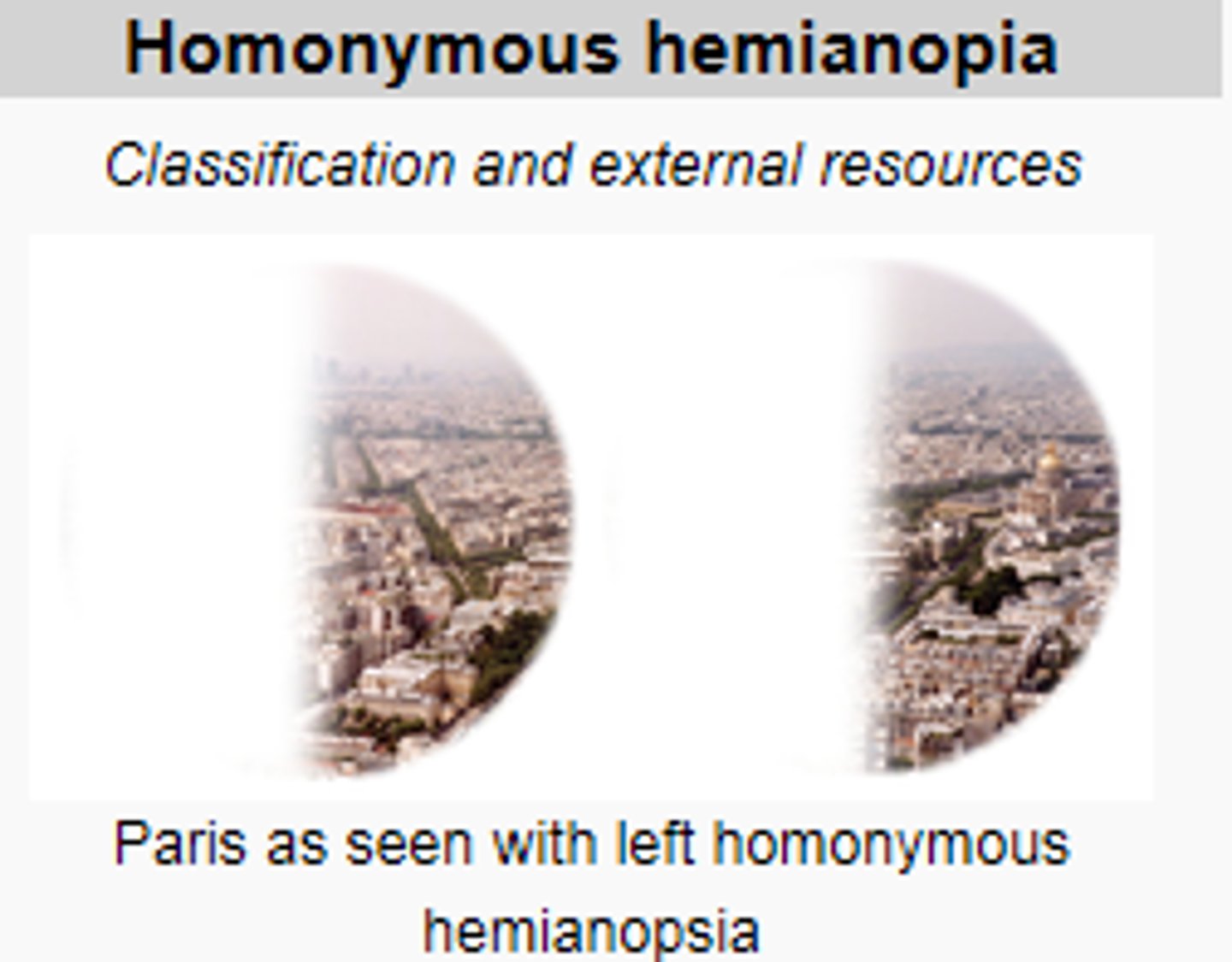
if someone has a R MCA stroke, what type of homonyomous hemianopsia will they present with?
L HH : left half of both eyes will lose vision
L temp R nasal
if a patient presents with R HH, what is the cause? and how will they present? what are their signs and symptoms?
L MCA stroke
R temp, L nasal fields are lost
language deficits, weakness and sensory loss, no perceptual disorders because L MCA
what are the signs and symptoms of PCA stroke in the peripheral territory?
• Contralateral homonymous hemianopsia
• Visual agnosia - PROSOPagnosia
• Dyslexia (difficulty reading) WITHOUT Agraphia (difficulty writing)
• Color discrimination
• Memory deficits
• Topographical disorientation
**more visual signs and symptoms
what are the signs and symptoms of PCA stroke in central territory?
Thalamus: Central Post Stroke
THALAMIC PAIN syndrome
What is prosopagnosia?
inability to recognize faces
Tone/Sensation Right vs Left Hemisphere
Left hemiparesis/hemisensory loss
Right hemiparesis/hemisensory loss
what are the impairments for Right vs Left Hemispheric stroke?
RIGHT:
Visual- perceptual impairments:
- Neglect
- Difficulty with VISUAL cues
LEFT:
Language impairments:
- Aphasias
- Difficulty with VERBAL cues
what are the behavior difference in Right vs Left hemispheric stroke?
RIGHT: Quick, impulsive, safety risk (like a young adult)
LEFT: Slow, cautious (like an older adult)
what are the intellectual differences in Right vs Left Hemispheric stroke?
RIGHT: Rigidity of thought
LEFT: Highly distractible
what are the emotional differences in Right vs Left hemispheric stroke?
RIGHT: Difficulty with negative emotions
LEFT: Difficulty with positive emotions
what is a common feature of Right and Left hemispheric stroke?
HH
what parts of the brain are affected if there is a stroke in the vertebral basilar artery?
cerebellum
medulla
pons
what are signs and symptoms of a stroke in the vertebral basilar artery?
locked in syndrome: patient cannot move or speak but is alert and oriented
-no horizontal eye movement but vertical eye movement and blinking are intact
-pseudo-bulbar palsy due to Cn V-VII paralysis
-rapid progression from hemiparesis to tetraplegia or quadriplegia
Complete Basilar Artery Syndrome
locked in syndrome
- tetraplegia
- bilateral cranial nerve palsy (upward gaze is spared)
- coma
- cognition is spared
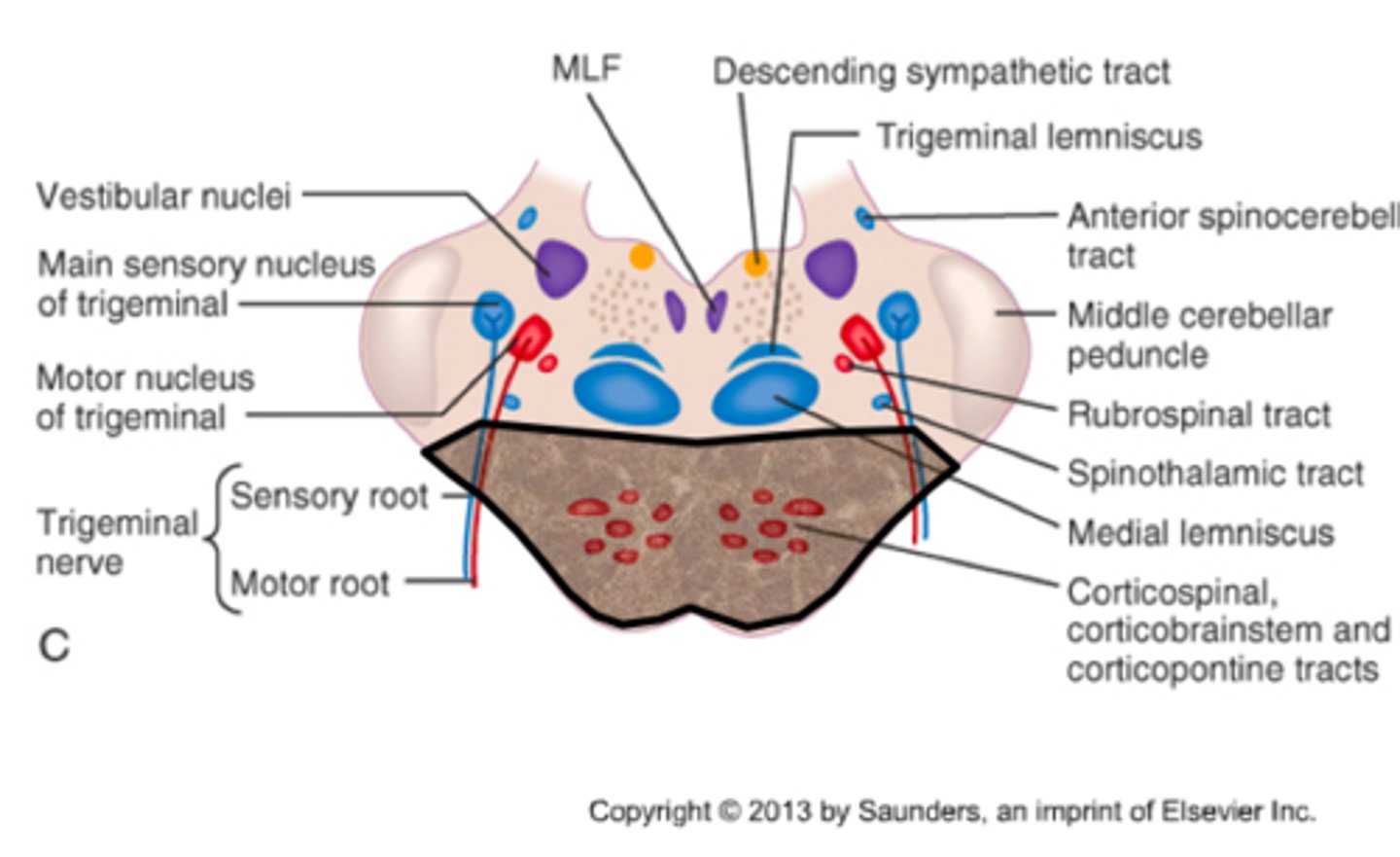
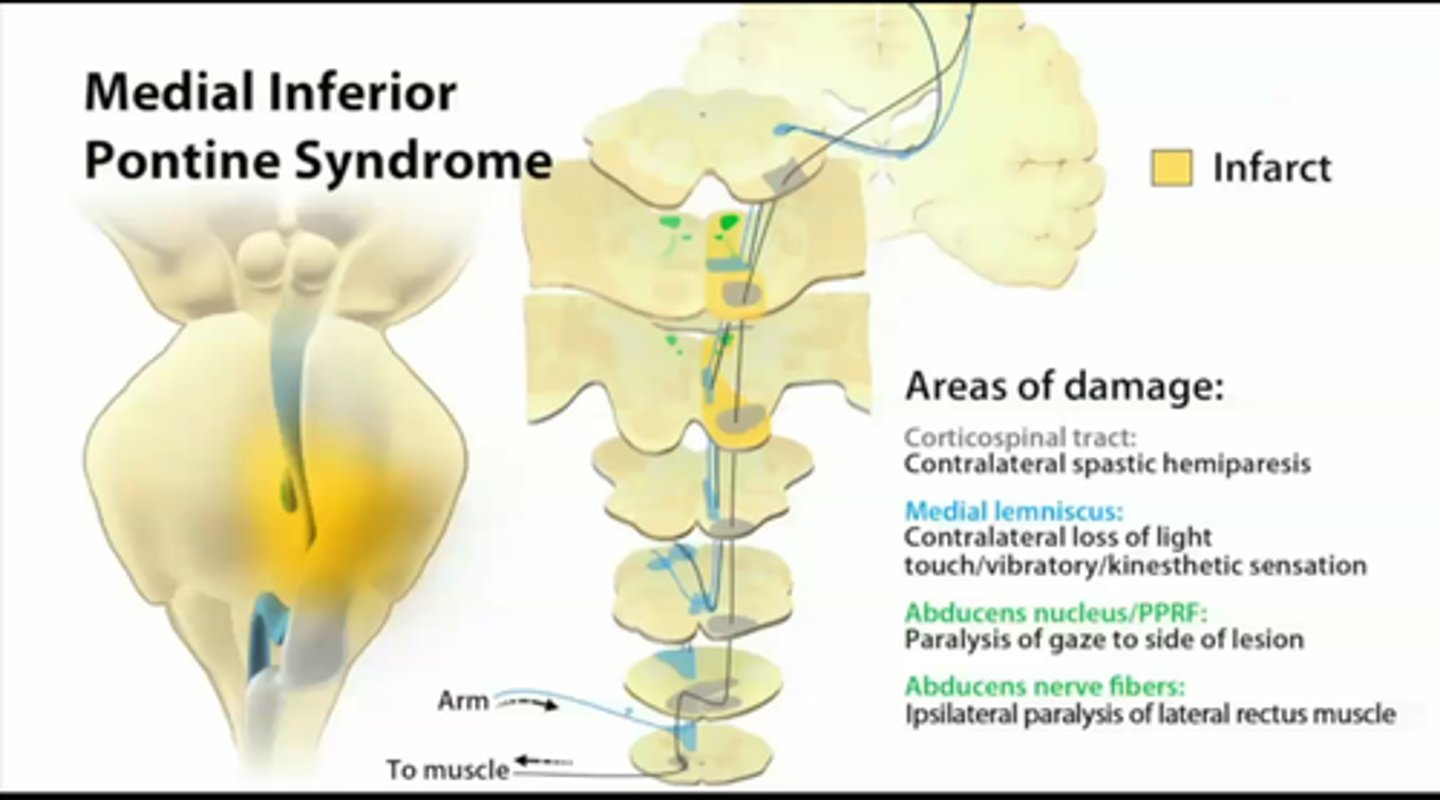
Medial Inferior Pontine Syndrome
Occlusion of the paramedian branch of basilar artery; characteristics:
1. ipsilateral to lesion:
▫ Paralysis of conjugate gaze to side of lesion
(preservation of convergence)
▫ Nystagmus
▫ Ataxia of limbs and gait
▫ Diplopia on lateral gaze
2. contralateral to lesion:
▫ Paresis of FACE, UE & LE
▫ Impaired tactile and proprioceptive sense over 50% of body
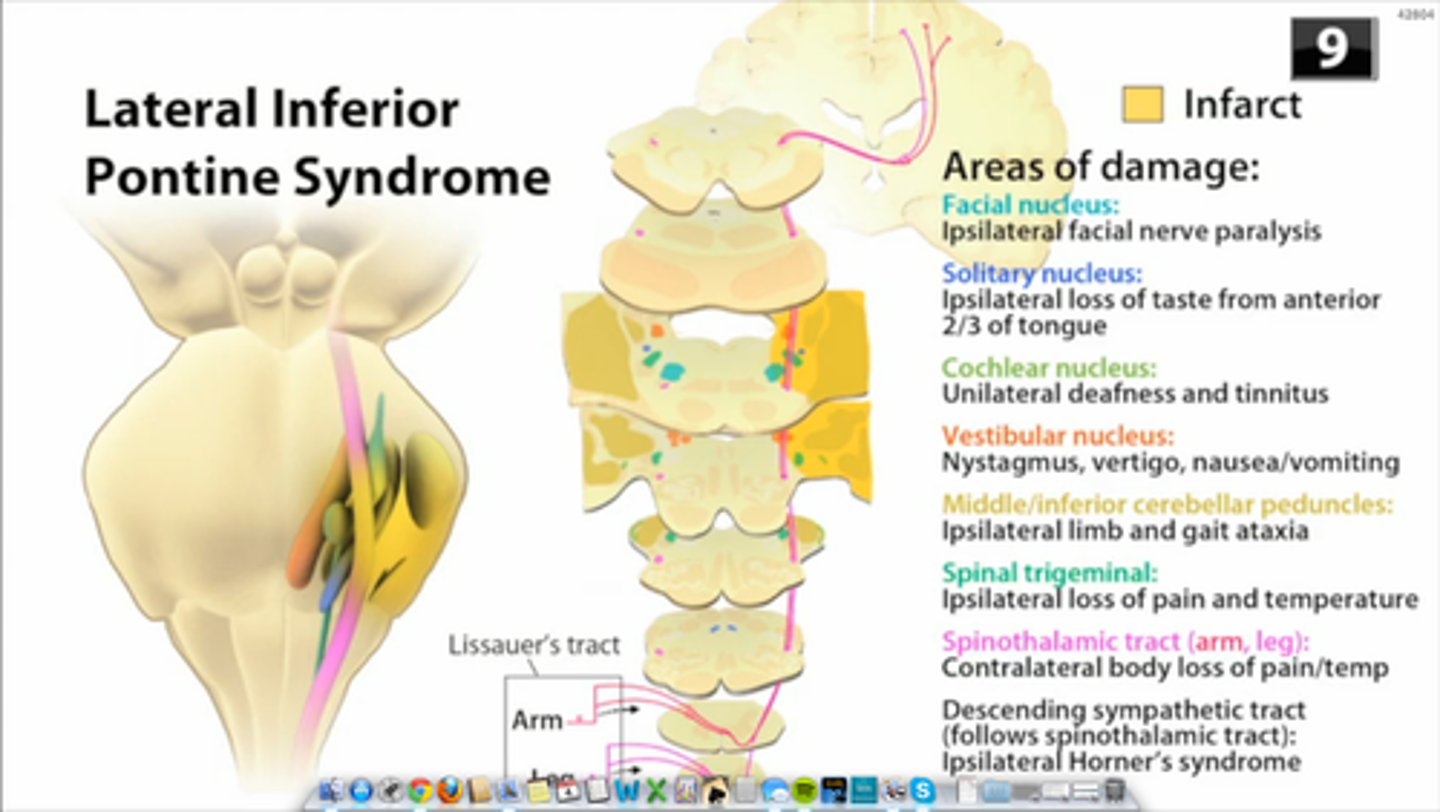
Lateral Inferior Pontine Syndrome
occlusion of the anterior inferior cerebellar artery; Characteristics:
Ipsilateral to lesion: cerebellar ataxia, nystagmus, vertigo, facial paralysis, paralysis of conjugate gaze to side of lesion, deafness, tinnitus, impaired facial sensation
Contralateral to lesion: impaired pain and temperature sensation half of body
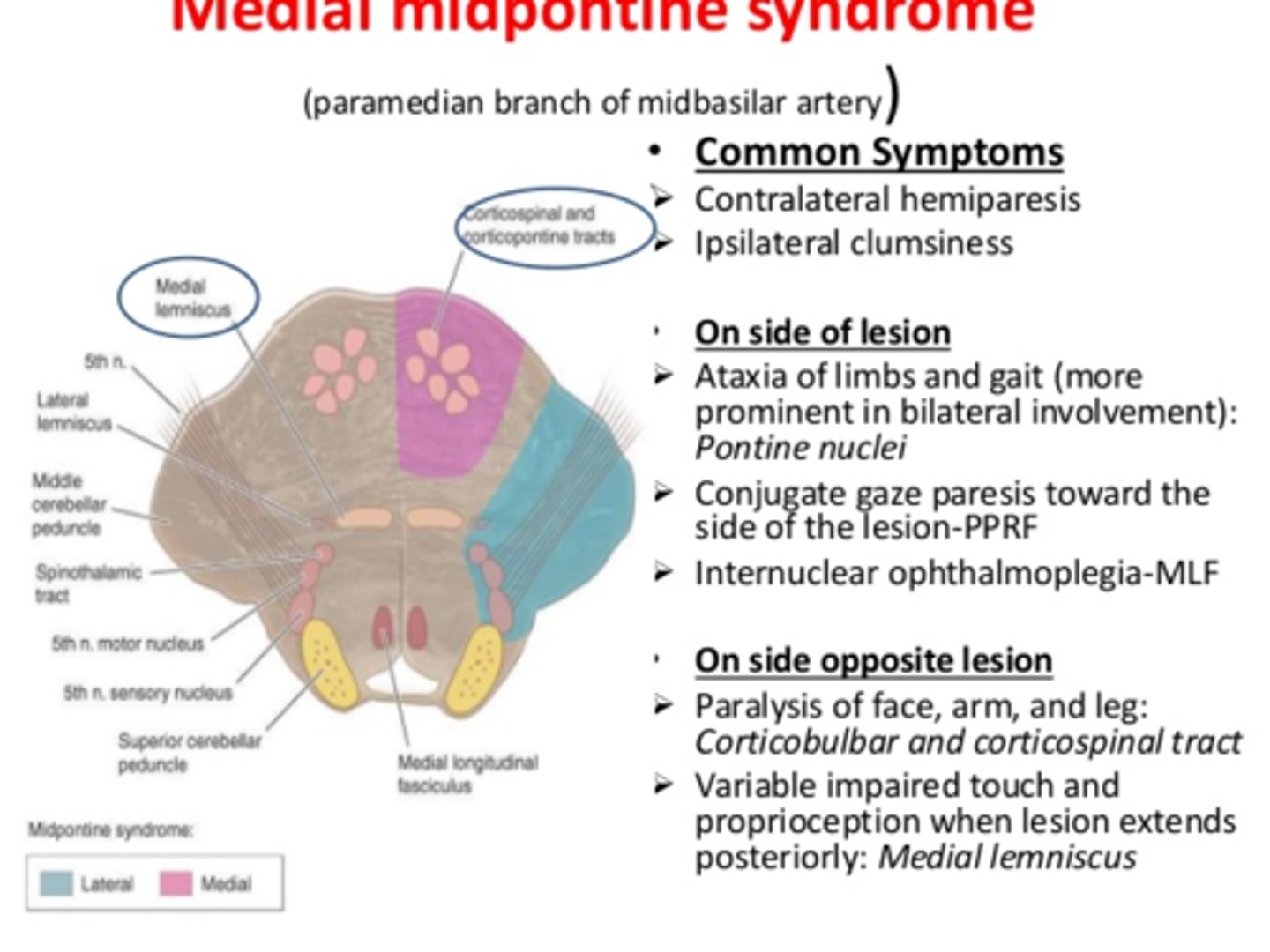
Medial Midpontine Syndrome
-Ipsilateral to lesion: ataxia of limbs and gait
-Contralateral to lesion: paralysis of face, UE, and LE; deviation of eye
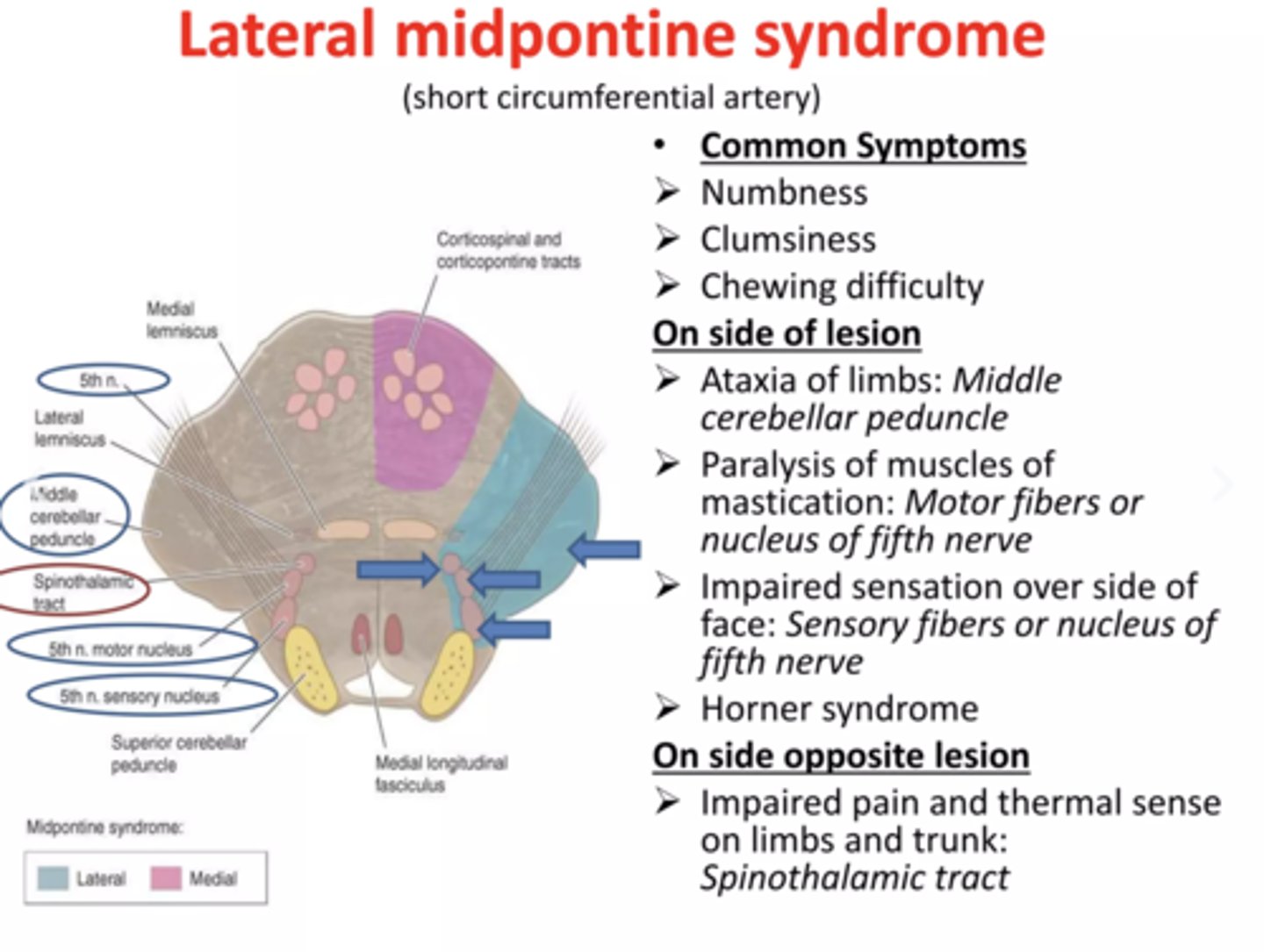
Lateral Midpontine Syndrome
Ipsilateral
▫ Ataxia of limbs
▫ Paralysis of mastication
▫ Impaired sensation over side of face
Contralateral
▫ Paralysis of FACE, UE & LE
spasticity vs synergy
how do you assess each?
increase in muscle tone: assess by PROM (seen at rest)
vs
patterned/combination of mvt: assess by AROM (either flex or extension synergy)
Brunnstrom Stage 1
Flaccidity
• No active limb movement
Brunnstrom Stage 2
Beginning of minimal voluntary movement
• In synergy, with associated reactions
• Increase tone
Brunnstrom Stage 3
Voluntary control of movement synergy (Spasticity at peak)
• Further increase tone to peak level
Brunnstrom Stage 4
Movement outside of synergy
• Decrease tone
Brunnstrom Stage 5
Increase complex movement, greater independence from limb synergies
Brunnstrom Stage 6
Individual joint movement, coordinated movement
Brunnstrom Stage 7
Normal function
what is the spasticity pattern for the UE?
Scapula: Retraction, downward rotation
Shoulder: Adduction, IR, depression
Elbow: Flexion
Forearm: Pronation
Wrist: Flexion, adduction
Hand: Finger flexion, clenched fist thumb, adducted in palm
what is the spasticity pattern for the LE?
Pelvis Retraction (hip hiking)
Hip: Adduction (scissoring), IR, Extension
Knee: Extension
Foot and Ankle
• Plantarflexion
• Inversion
• Equinovarus
• Toes claw (tarsometatarsal extension,
metatarsophalangeal flexion)
• Toes curl (tarso- and
NPTE Final Frontier metatarsophalangeal flexion)
what is the flexion synergy for the UE?
• Scapula retraction/elevation or hyperextension
• Shoulder abduction, external rotation
• Elbow flexion
• Wrist and finger flexion

what is the flexion synergy of the LE?
• Hip flexion, abduction, ER
• Knee flexion
• Ankle DF, inversion
• Toe DF
what is the extension synergy for the UE?
• Scapular protraction
• Shoulder adduction, IR
• Elbow extension
• Forearm pronation
• Wrist and finger flexion
**same as spasticity pattern
what is the extension synergy for the LE?
• Hip extension, adduction, IR
• Knee extension
• Ankle PF, inversion
• Toe PF
what are muscles not usually involved in synergy patterns?
(1) latissimus dorsi, (2) teres major, (3) serratus anterior,
(4) finger extensors, and (5) ankle evertors
what are some interventions used for spasticity?
bring them out of the synergy pattern! usually the opposite of their synergy
What are the Ranchos Los Amigos levels? what acronym should you use?
levels used to assess the function of someone following TBI
RCA= response (1-3), confused (4-6), appropriate (7-8)
RLA Level 1
no response, coma
total assistance
RLA Level 2
Generalized response
Non-purposeful whole body, vocal
Total Assistance
RLA Level 3
Localized response
Purposeful, local and specific but inconsistent
**Follows simple commands - close eyes, squeeze hands
what are interventions appropriate for RLA Levels 1-3?
• Positioning: Head neutral, prevent ulcer, sit (if stable)
• Gentle PROM: Joint integrity, skin integrity
• Respiratory care: Postural drainage, percussion, vibration, suction
• Educate family: What to expect, how to be more involved
RLA Level 4
Confused and AGITATED
• Heightened activity, just coming out of coma
• Aggressive: Doesn't cooperate, verbalization is incoherent,
confabulations
• No selective attention
• No long- and short-term memory
what treatment is appropriate for RLA Level 4? how do you want to address confusion, memory, and agitation?
• Consistent: Same therapist, same staff, family introduce yourself daily. ESTABLISH A ROUTINE, give them options
• Orient the patient: Calendar, clock
• NO CARRYOVER: Use chart and graph to measure progress
Calm behavior. DO NOT confront!
• Environment - Closed - prevent harm to others
RLA Level V
Confused, inappropriate/ non-agitated: Appears alert with fairly consistent reactions, although increased complexity of commands causes more random responses. Starts to SOCIALIZE
-responds CONSISTENTLY to simple commands
-responds INCONSISTENTLY to complex commands
-with structure, able to socialize for short period
Memory impaired. Inappropriate use of objects. Can't learn new task.
Shows inappropriate behavior given complex instructions or when in an unstructured activity. Easily distracted and can still be agitated by certain stimuli in the environment
RLA Level 6
Confused, Appropriate: Moderate Assistance
• Follows simple instruction consistently
• Goal oriented behavior with external input
Memory: Carryover of previous skills present
(self-care)
what do you want to use as treatment for RLA levels 5 and 6?
• Complex commands cannot be followed - Avoid more complex
open environments
RLA Level 7
Automatic, Appropriate: Minimal Assistance for Daily Living Skills
• Oriented in home and hospital
• Daily routine - automatic but robot-like
• Judgement impaired
• Able to initiate social or recreational
activity with structure
RLA Level 8
Purposeful, Appropriate
• Carryover of new skills present
• Impaired judgement in an emergency situation, abstract reasoning and reduced tolerance for stress
**have tough time in high stress or emergency situations
what treatment is appropriate or RLA Levels 7 and 8?
• Focus on re-entry to work and community
• Emphasize skills related to problem solving, social interaction
• Trial period of independent living
• Adaptation at work or school to return to normal life