The adaptive immune response part 1
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
adaptive immune response
The branch of the immune system that has memory, and can develop a memory as needed to respond to future infections more effectively.
Two main types of adaptive immunity
Cell-mediated immunity (T-cell response)
Humoral immunity (B-cell/antibody response)
What happens when the adaptive immune system is missing?
The body cant mount specific immune responses and can become extremely vulnerable to all infections
this is the case with the boy in the bubble (he had SKID, a conditions where both B and T cells arent functional or there)
How long does it take for adaptive immunity to develop after exposure to a microbe?
Adaptive immunity develops over a 3–4 day period after exposure to an invading microbe.
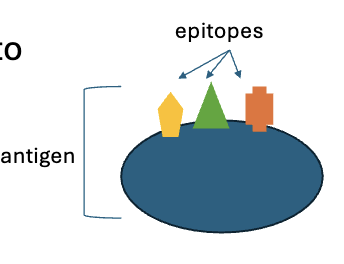
What does the immune system recognize on antigens (for identification)
The immune system recognizes small pieces of an antigen called antigenic determinants or epitopes.
usually 2 or 3
How are epitopes presented to the adaptive immune system?
During phagocytosis, pathogens are broken down into epitopes. These epitopes are then presented on the surface of antigen-presenting cells to alert the adaptive immune system.
like the zombie dog reference of him showing what he did
immunogens
a type of epitope that can generate an immune response on their own.
All immunogens are epitopes, but not all epitopes are immunogens, some are haptens.
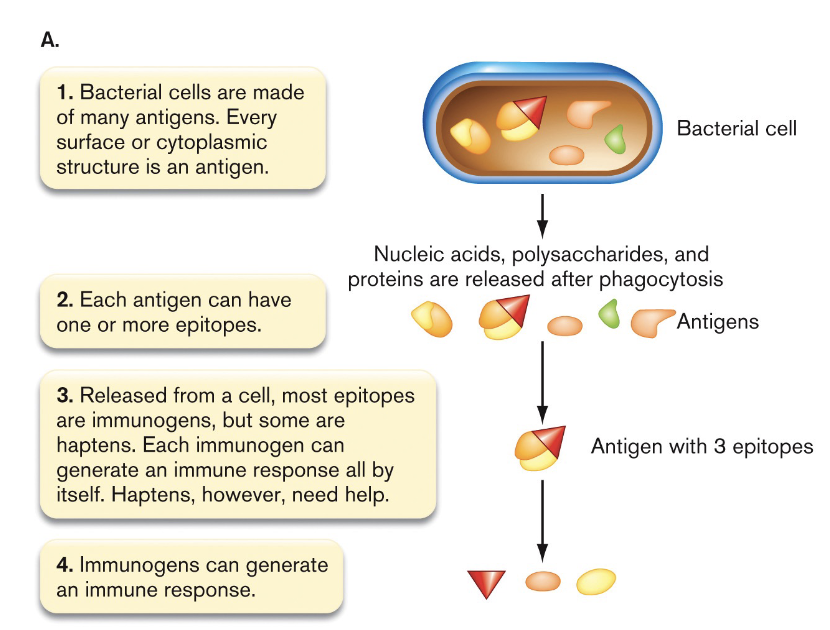
Haptens
A small molecule that cannot elicit an immune response on its own.
When bound to a larger molecule, a hapten can act as an antigen.
ex) nickel, urushiol.
immunogenicity
the effectiveness by which an antigen elicits an immune response. The higher the immunogenicity, the more likely the immune system will react.
What types of biological molecules have increasing immunogenicity?
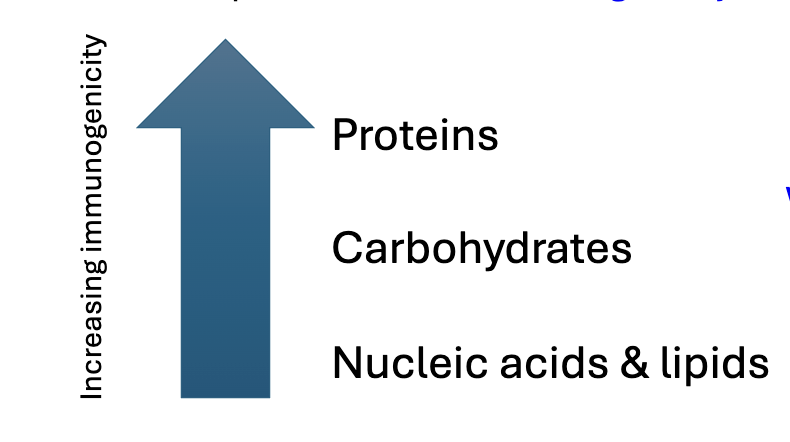
this is because proteins have the most complex structure
T cell education
T cells learn to recognize foreign invaders (pathogens) and avoid attacking the body’s own cells (self).
begins before birth
Where do T cells come from, and how do they get their unique T cell receptors (TCRs)?
T cells come from hematopoietic stem cells in bone marrow, and as they mature each T cell develops its own unique T cell receptor
Each T cell receptor reacts to a different random epitope.
Thymus college
the college for new T cells where they learn to differentiate between self and non self cells.
this occurs in the Thymus gland

Tests for T cells in the thymus college
Positive selection → first test in the thymus to see if they can recognize MHC peptides. If they can understands commands from MHC, they pass.
Negative selection → the second test where they are checked for reactvity against self antigens. If a T cell reacts too strongly to itself, it fails the test and is killed.
98% of T cels that enter the Thymus are killed because they failed the test, only the ones that pass both tests and are allowed ot mature are released into the body.
How do T cells of older adults get an education if Thymus college is not maintained after puberty?
The Thymus starts to shrink and become less functional after puberty. However, most T cell education happens before and shortly after birth. After that, the body maintains a reserve of educated T cells that continue to replicate at balanced rate.
Two types of effector T cells
Cytotoxic T cells (TC) / CD8+ cells → assasins
Helper T cells (TH) / CD4+ cells → intelligence officers
Cytotoxic T cells (TC) / CD8+ cells
The assassins who are trained to seek and destroy cells presenting noxious antigens (indicated they may be infected)
CD8+ marker on their surface
can directly kill host cell thats infected
Helper T cells (TH) / CD4+ cells
These are the intelligence officers’ who are trained to memorize databanks of antigens and to alert B cells if circulating antigen is detected.
have CD4+ marker on their surface
Some TH (helper T cells) diffrentiate into
memory TH cells.
Memory TH cells
remembers antigens from previous experience, and continue to also act as effector cells during reinfection. (both memory and effector)
they dont have a super long life cycle but can clonally replicate and pass down traits to the next generation.
overtime their memory gets hazy.
Regulatory T cells (Treg)
Some naive T cells differentiate into these. They help to restore homeostasis after infection, not by promoting an immune response but by regulating immune system.
lack of Treg is associated with chronic inflammation.
Major Histocompatibility Complex glycoproteins (MHC) proteins
These are the proteins which infected cells or APCs place antigens on display to the immune system
two main types:
MHCI
MHCII
MHCI
These display antigens on the surface of an infected cell (infected cell signals that its been infected)
Cytotoxic T cells (and NK cells) then destroy the infected cell.
MHCII
These display antigens on the surface of antigen-presenting cells (APCs)
Helper T cells recognize these antigens and alert the immune system to take action.
includes (APC like macrophages, dentritic cells)
Why are there two types of MHC proteins?
MHC I and MHC II proteins help distinguish which cells need to be destroyed and which need to alert the immune system.
MHC I is found on all nucleated cells and presents intracellular antigens to cytotoxic T cells (CD8⁺), triggering the destruction of infected or abnormal cells.
MHC II is found on antigen-presenting cells (APCs) and presents extracellular antigens to helper T cells (CD4⁺), activating immune responses like antibody production and macrophage activation.
This distinction prevents the immune system from killing healthy cells that are presenting antigens for immune help.