MicroParasitology Lec Finals: Protozoans
1/133
Earn XP
Description and Tags
I LOVE YOU MISS GARCIA
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
134 Terms
What are protozoa?
Single-celled organisms.
What are helminths?
Multi-celled organisms.
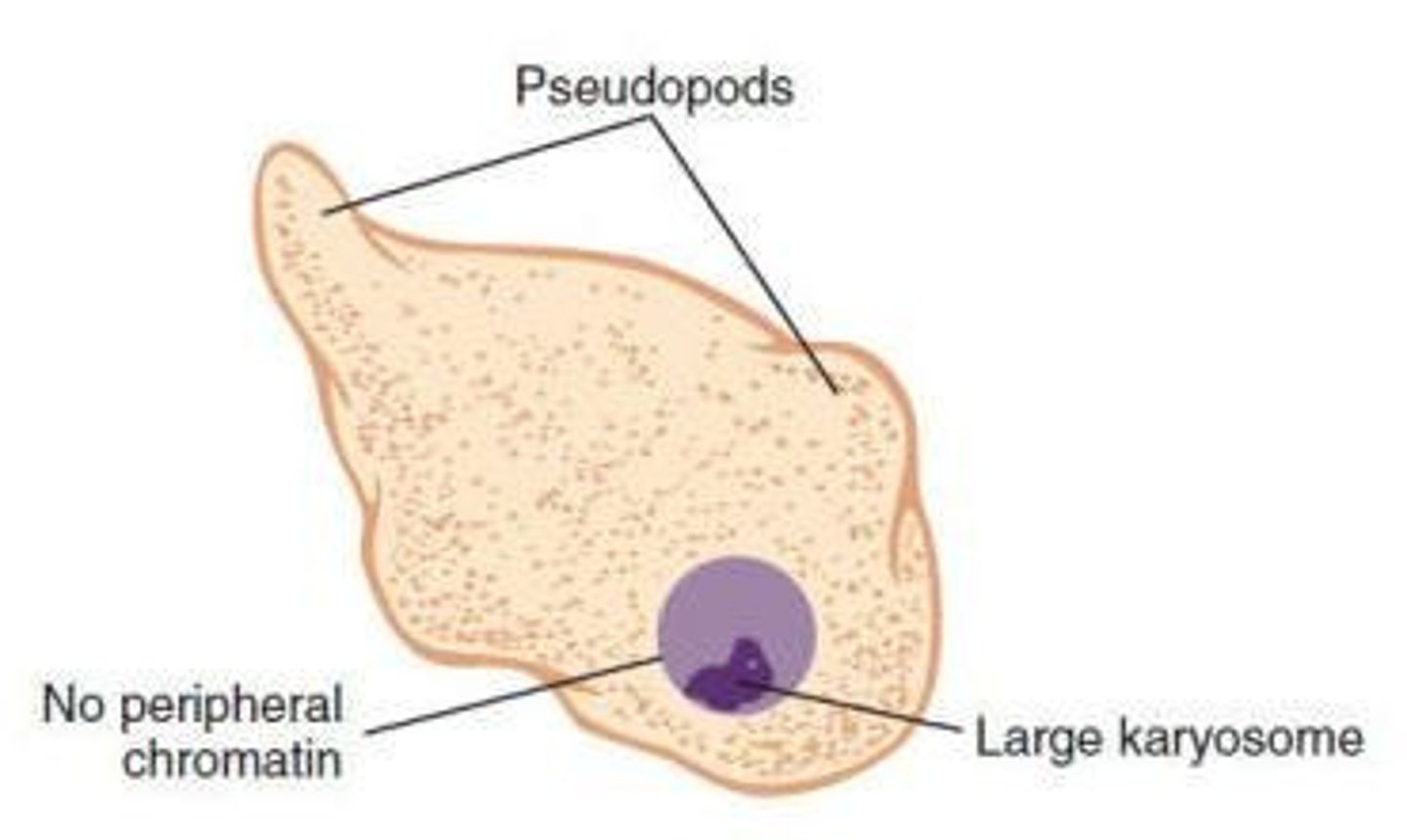
How do amoebas move?
Amoebas are characterized by their pseudopods.
What are the two stages of the amoeba life cycle?
Trophozoite and cyst stages.
What is the trophozoite stage of an amoeba?
A fragile and delicate form that reproduces through binary fission.
What is encystation in amoebas?
The process that occurs in the intestine, leading to the formation of cysts.
How are amoebas transmitted?
Through ingestion of infective cysts in contaminated food and water.
How long can cysts remain viable?
Cysts can remain viable in feces for extended periods.
What is the diagnostic stage of amoebas?
Trophozoite found in liquid, soft, or loose stools; cyst is the formed stage.
What lab methods are used for diagnosing amoebas?
Wet mount and permanent stain.
What disease is caused by Entamoeba histolytica?
Intestinal amoebiasis, amoebic colitis, amoebic dysentery, and extraintestinal amoebiasis.
What is the mode of transmission for Entamoeba histolytica?
Ingestion of mature quadrinucleated cysts through hand-to-mouth contact or contaminated food/water.
What are the characteristics of young cysts of Entamoeba histolytica?
They may contain chromatoidal bars and a glycogen mass.
What occurs during excystation?
It occurs in the small intestine, producing 8 motile trophozoites.
What is the epidemiology of Entamoeba histolytica?
It is a leading cause of parasitic death worldwide, thriving in tropical and subtropical areas with poor sanitation.
What are the symptoms of asymptomatic amoebiasis?
Asymptomatic due to low virulence strains, low inoculation, or a competent immune system.
What are the symptoms of symptomatic amoebiasis?
Amoebic colitis leading to amoebic dysentery, including diarrhea, abdominal pain, chronic weight loss, anorexia, and fatigue.
What are the symptoms of extraintestinal amoebiasis?
Upper right abdominal pain with fever, weakness, weight loss, sweating, nausea, and vomiting.
What is the treatment for asymptomatic amoebiasis?
Paromomycin, Diloxanide furoate (Furamide), and Metronidazole (Flagyl).
What is the treatment for symptomatic amoebiasis?
Iodoquinol.
What are some prevention methods for amoebiasis?
Boiling water with iodine crystals, filtration, good personal hygiene, and sanitation practices.
What is E. dispar?
A nonpathogenic amoeba similar to E. histolytica, differentiated by DNA probes and electrophoresis techniques.
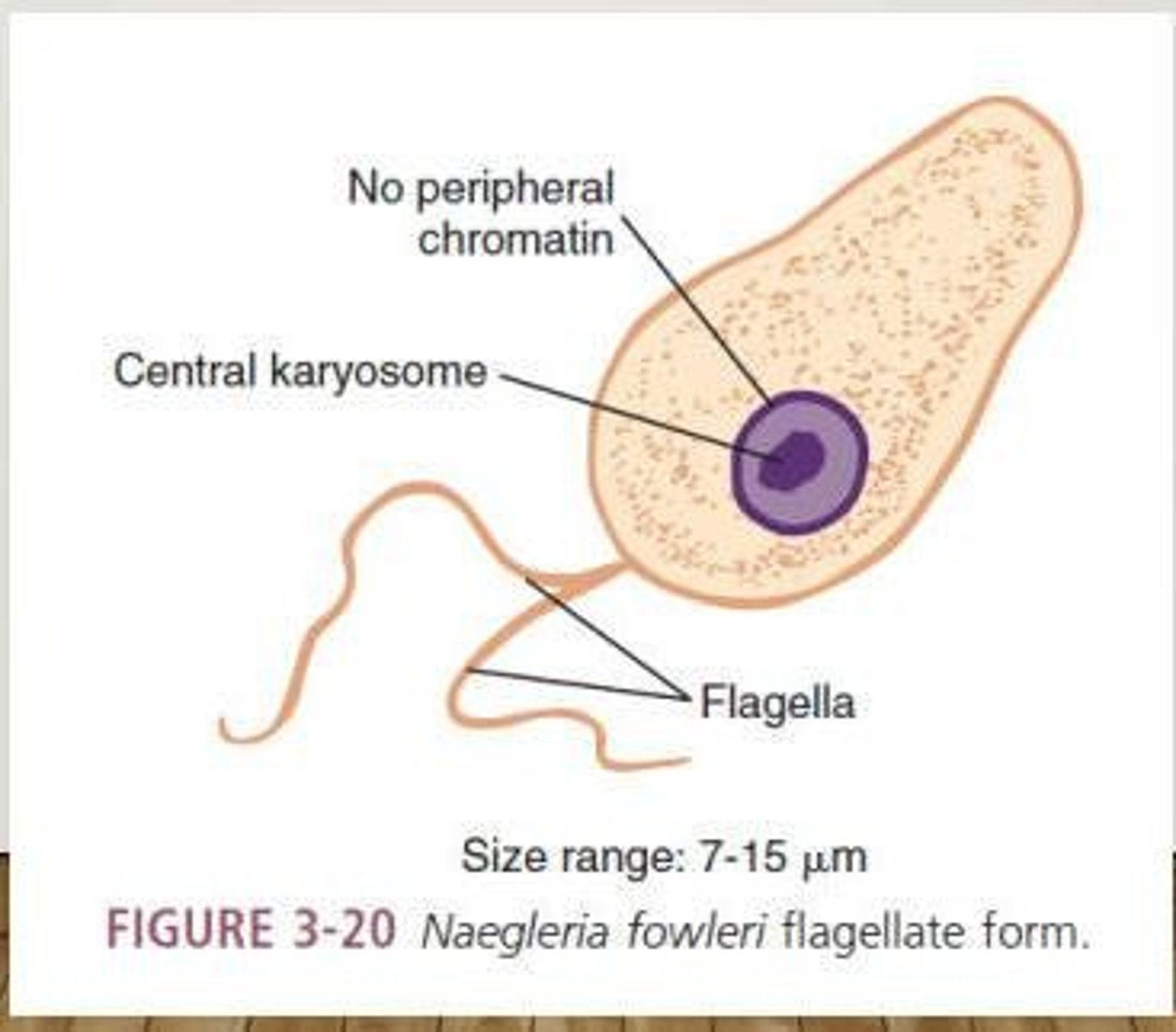
What is Naegleria fowleri?
A free-living amoeba that causes Primary Amoebic Meningoencephalitis (PAM).
What are the symptoms of Naegleria fowleri infection?
Fever, headache, sore throat, nausea, vomiting, leading to stiff neck and seizures (Kernig's sign). Death usually occurs in 3-6 days without treatment.
Where is Naegleria fowleri commonly found?
In warm bodies of water such as lakes, streams, ponds, and swimming pools.
What are the three morphologic forms of Naegleria fowleri?
Trophozoites, flagellates, and cysts.
Which form of Naegleria fowleri is known to infect humans?
Trophozoites.
How does Naegleria fowleri replicate?
Through binary fission.
What is the mode of transmission (MOT) for Naegleria fowleri?
Swimming in infected water.
What treatments are available for Naegleria fowleri infection?
Amphotericin B and miconazole.
What disease does Acanthamoeba spp. cause?
Granulomatous Amoebic Encephalitis (GAE) and Acanthamoeba keratitis.
What are the characteristics of Acanthamoeba?
Spinelike pseudopods known as acanthopodia.
What are the clinical manifestations of Granulomatous Amoebic Encephalitis?
Headaches, seizures, stiff neck, nausea, and vomiting; granulomatous lesions in the brain may contain trophozoites and cysts.
What is the most successful treatment for Acanthamoeba keratitis?
Propamidine.
What is the main habitat of Giardia intestinalis?
The small intestine, cecum, and colon, specifically the duodenum.
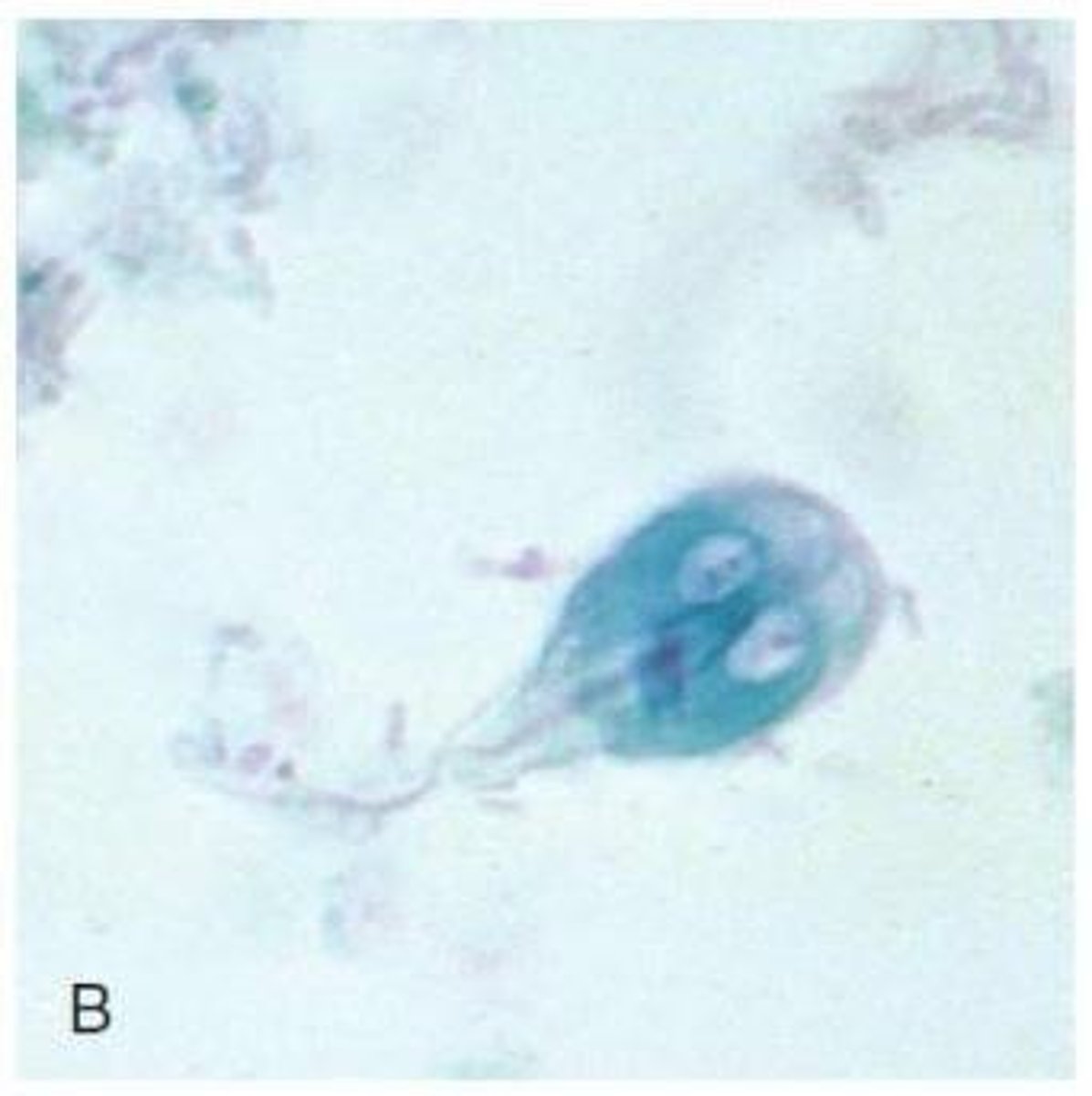
What disease is caused by Giardia intestinalis?
Giardiasis, commonly known as traveler's diarrhea.
What is the mode of transmission for Giardia intestinalis?
Ingestion of contaminated food and water.
What are the clinical presentations of giardiasis?
Mild diarrhea, abdominal cramps, anorexia, flatulence, steatorrhea, malabsorption syndrome.
What is the treatment for giardiasis?
Tinidazole (Tindamax) and Nitazoxanide (Alinia).
How can contaminated water be disinfected to prevent giardiasis?
Using a double-strength saturated iodine solution.
What is the mode of transmission for Chilomastix mesnili?
Ingestion of contaminated food and water or hand-to-mouth.
What is known about Dientamoeba fragilis?
The exact mode of transmission is unknown; may be transmitted via the eggs of E. vermicularis and A. lumbricoides.
What is the typical state of infection for Dientamoeba fragilis?
Most infections are asymptomatic, but symptomatic cases can present with diarrhea and abdominal pain.
What is the cyst stage status of flagellates?
Flagellates do not have a cyst stage.
What triggers the encystation of Giardia intestinalis?
Unfavorable conditions for trophozoites in the large intestine.
What is the treatment for Trichomonas infections?
Iodoquinol for treatment and Flagyl for symptomatic cases.
What are the preventive measures for Trichomonas infections?
Maintaining personal and public sanitary conditions and avoiding unprotected homosexual practices.
What is the Hakansson phenomenon?
Granules exhibit Brownian motion in wet mount preparations.
What is the mode of transmission (MOT) for Trichomonas hominis?
Ingestion of infected milk or fecal-oral route.
What specimen is used to diagnose Trichomonas hominis?
Stool.
What are the symptoms of Trichomonas vaginalis infection in males?
Persistent urethritis, enlarged prostate, dysuria, nocturia, and epididymitis.
What specimen is used for diagnosing Trichomonas vaginalis?
Vaginal discharge, urethral and prostatic secretions.
How does Trichomonas vaginalis invade the body?
Through sexual intercourse, rarely via sharing douche supplies and communal bathing.
What are the clinical presentations of Trichomonas vaginalis in females?
Persistent vaginitis with thin, white urethral discharge, dysuria, urinary frequency, and foul-smelling greenish-yellow vaginal discharge.
What are the two main groups of hemoflagellates?
Leishmania spp. and Trypanosoma spp.
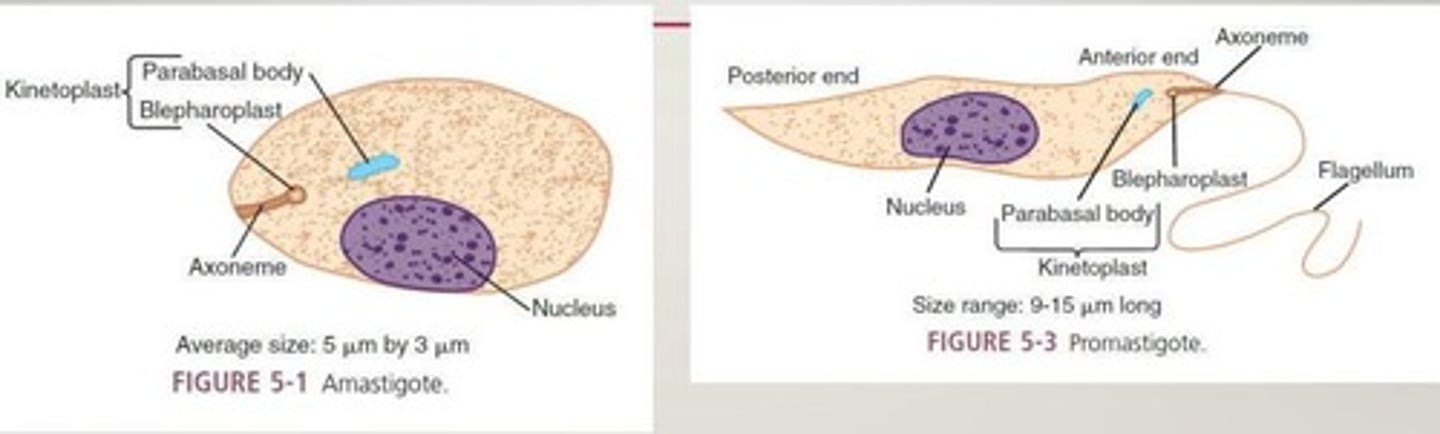
What are the forms of hemoflagellates?
Amastigote, promastigote, epimastigote, and trypomastigote.
What is the diagnostic stage for Leishmania?
Amastigote.
What is the diagnostic stage for Trypanosoma?
Trypomastigote, except for Trypanosoma cruzi, where amastigotes may also be found.
What disease does Leishmania braziliensis complex cause?
Mucocutaneous leishmaniasis.
What is the vector for Leishmania braziliensis?
Sandflies (Lutzomyia and Psychodopygus).
What is the infective stage of Leishmania braziliensis?
Promastigote.
What is the treatment for mucocutaneous leishmaniasis?
Antimony compounds (sodium stibogluconate, Pentosam).
What disease does Leishmania donovani complex cause?
Visceral leishmaniasis, also known as kala-azar or dum dum fever.
What are the symptoms of visceral leishmaniasis?
Hepatosplenomegaly and nondescript abdominal illness.
What is the Montenegro skin test used for?
Screening large populations at risk of leishmaniasis.
What is the mode of transmission for Leishmania donovani?
Through the bite of an insect vector, specifically Phlebotomus and Lutzomyia.
What are the early symptoms of visceral leishmaniasis?
Fever and chills, resembling malaria or typhoid fever.
What is the drug of choice for treating advanced stages of leishmaniasis?
Amphotericin B (Ambisome)
What complex causes New World Leishmaniasis and what are its symptoms?
Leishmania mexicana complex causes cutaneous leishmaniasis, characterized by small red papules, single pus-containing ulcers that are self-healing.
Which species are included in the Leishmania mexicana complex?
L. mexicana, L. pifanoi, L. amazonensis, L. garnhami.
What is the primary vector for the Leishmania mexicana complex?
Lutzomyia venezuelensis.
What is the treatment of choice for New World Leishmaniasis?
Pentavalent antimonials (sodium stibogluconate, Pentosam).
What complex causes Old World cutaneous leishmaniasis and what are its symptoms?
Leishmania tropica complex causes oriental sores, characterized by one or more ulcers with pus that generally self-heal.
Which species are included in the Leishmania tropica complex?
L. tropica, L. aethiopica, L. major.
What is the vector for the Leishmania tropica complex?
Phlebotomus fly.
What laboratory diagnosis is used for Old World cutaneous leishmaniasis?
Giemsa-stained aspiration of fluid from the ulcer.
What is Diffuse Cutaneous Leishmaniasis (DCL) and its treatment?
DCL occurs especially in anergic cases, presenting as thick plaques of skin with multiple lesions/nodules. Treatment is sodium stibogluconate (Pentosam).
What disease does Trypanosoma brucei cause and what are its vectors?
T. brucei causes nagana and sleeping sickness, with vectors being Glossina palpalis and Glossina tachinoides.
What is the infective and diagnostic stage of Trypanosoma brucei?
Trypomastigotes.
What are the symptoms of West African sleeping sickness caused by Trypanosoma brucei gambiense?
Painful chancre, fever, malaise, headache, anorexia, Winterbottom's sign, and CNS involvement symptoms.
What is the treatment for West African sleeping sickness?
Melarsoprol, suramin, pentamidine, and eflornithine.
What distinguishes Trypanosoma brucei rhodesiense from gambiense?
T. brucei rhodesiense causes East African sleeping sickness, is more rapid, and involves the CNS.
What disease does Trypanosoma cruzi cause and how is it transmitted?
T. cruzi causes Chagas' disease, transmitted via the bite of a reduviid bug, blood transfusions, sexual intercourse, and transplacental transmission.
What is Romaña's sign and in which disease is it observed?
Romaña's sign is conjunctivitis with unilateral edema of the eyelids, observed in Chagas' disease.
What is the initial symptom of Chagas' disease?
An erythematous nodule (chagoma) that lasts for 2-3 months.
What is the treatment for Chagas' disease?
Nifurtimox (Lampit).
What are the two main genera included in the SPOROZOA category?
Plasmodium spp. and Babesia spp.
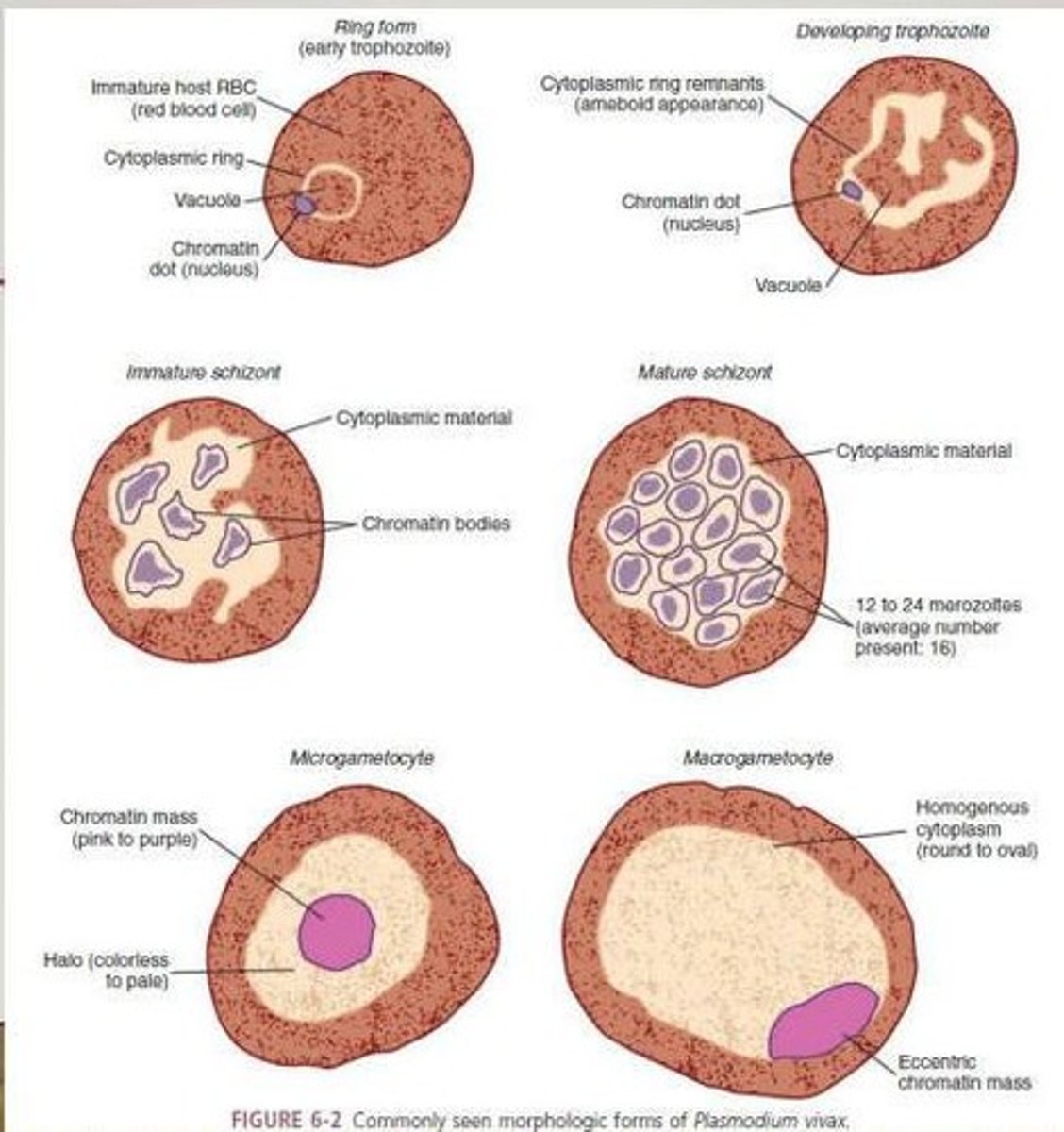
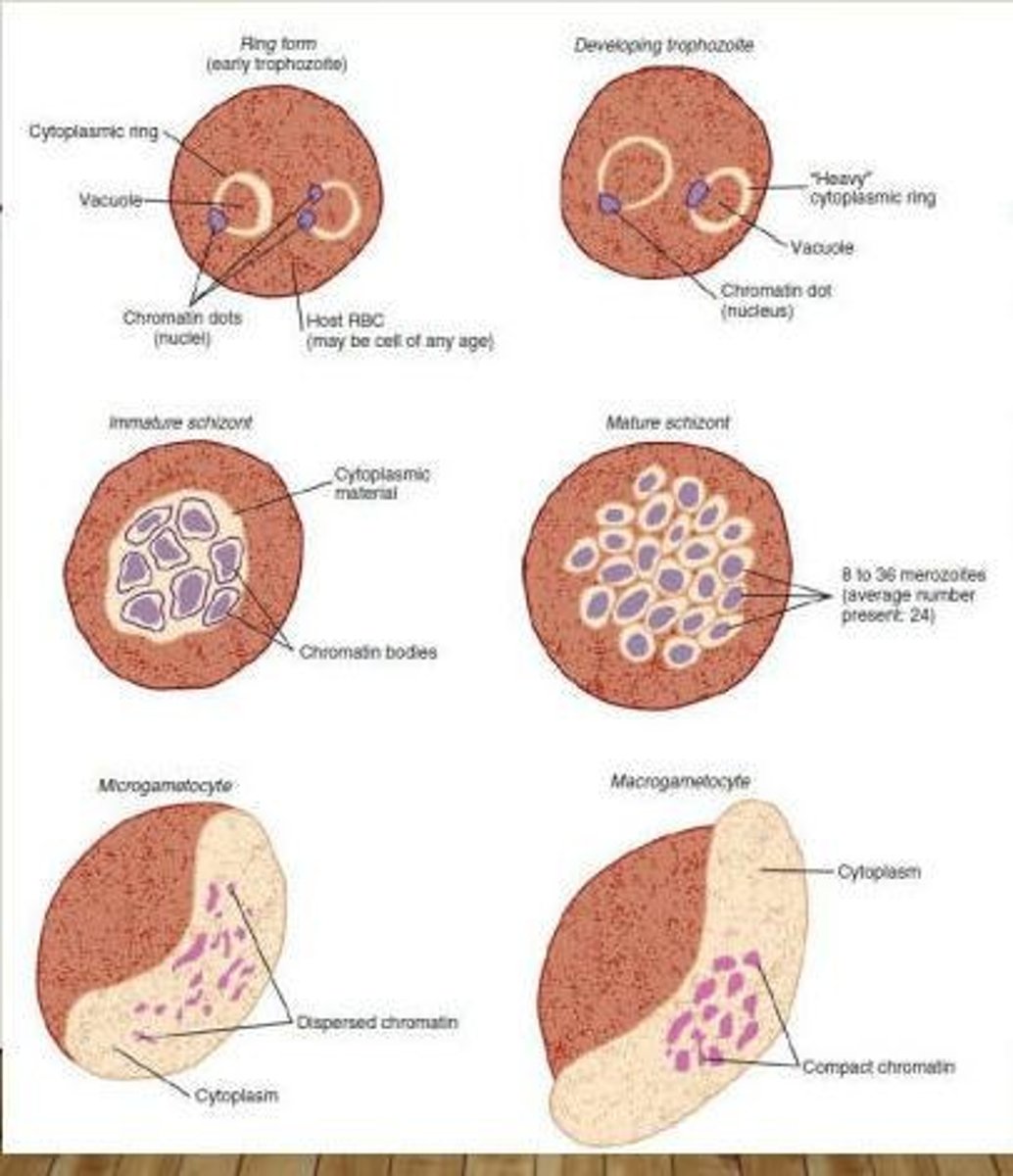
What are the morphological forms of Plasmodium species after the invasion of RBCs?
Ring form/Early trophozoite, Developing trophozoite, Immature schizont, Mature schizont, Microgametocyte, and Macrogametocyte.
What is the mode of transmission (MOT) for malaria?
Bite of Anopheles mosquito with infective sporozoites, blood transfusion, sharing of needles.
Describe the lifecycle of sporozoa in malaria. What happens after sporozoites reach hepatocytes?
Sporozoites undergo schizogony in hepatocytes, releasing merozoites that infect RBCs and may develop into micro and macrogametocytes.
What occurs in the mosquito's stomach during the sexual cycle of Plasmodium?
Male and female gametocytes form zygotes/ookinetes, which mature into oocysts releasing mature sporozoites.
What is the best time to collect blood specimens for malaria diagnosis?
During paroxysms: 15-60 mins cold stage followed by 2-6 hrs of fever, leading to profuse sweating and extreme fatigue.
What are the symptoms of malaria?
Headache, lethargy, anorexia, ischemia, and paroxysms of fever.
What type of malaria does Plasmodium vivax cause?
Benign tertian malaria, also known as vivax malaria.
Where is Plasmodium vivax commonly found?
In the tropics, subtropics, and temperate regions.
When do symptoms of Plasmodium vivax infection typically begin?
10-17 days post-exposure.
What are the symptoms associated with Plasmodium vivax?
Nausea, vomiting, headache, muscle pains, and photophobia.
How often do paroxysms occur in Plasmodium vivax malaria?
Every 48 hours.
What type of malaria does Plasmodium ovale cause?
Benign tertian malaria, also known as ovale malaria.
How long do untreated infections of Plasmodium ovale typically last?
Approximately 1 year.