Chapter 9: Homeostasis
1/47
Earn XP
Description and Tags
Made by @agreyr
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Homeostasis
Relatively stable internal environment optimized for cellular activity
Factors of homeostasis
Acidity, salt, water, oxygenation, temperature, energy availability
Example of homeostasis
Thermoregulation
Mammals are endotherms, meaning we make hear inside our bodies using metabolism and muscular activity; there is a dedicated, precisely regulated system for creating warmth
Set point
Desired homeostatic value (98.6°F or 37°C)
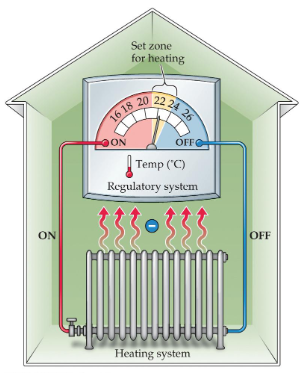
Negative feedback
Deviation leads to compensatory action of the system
Restoring the set point turns off the response
Redundancy
Each system has multiple mechanisms for monitoring stores, conserving remaining supplies, obtaining new resources, and shedding excesses
Example: pre-optic and lateral areas of the hypothalamus controlling temp
Behavioral Compensation
Behaviors that change the exposure of the body surface, external insulation, and/or surroundings
Allostasis
Dynamic process whereby the system shifts responses depending on prior experience and the environment
DSM-identified eating disorders
Anorexia Nervosa, Bulimia Nervosa, Binge-Eating Disorder
Anorexia Nervosa
Voluntary self-starvation despite more response to the presence of food than controls
Complex combination of genetic, endocrine, personality, cognitive, and environmental factors
Similar symptoms to Bulimia Nervosa, often difficult to distinguish
Bulimia Nervosa
Bingeing and purging
Similar symptoms to Anorexia Nervosa, often difficult to distinguish
Binge-Eating Disorder
Tendency to gorge oneself way past the point of fullness
Causes not well understood but thought to involve over activation of dopamine reward mechanisms
Obesity
Determined based on Body Mass Index (BMI)
Body Mass Index (BMI) calculation
kg/mxm OR 703(lb/inxin)
Starvation BMI category
Under BMI 15
Underweight BMI category
BMI 15 to 18.5
Normal BMI category
BMI 18.5 to 25
Overweight BMI category
BMI 25 to 30
Obese BMI category
BMI 30 or higher
Weight loss treatment
Is often extremely difficult; minimal success rates
Should ideally involve both diet and exercise
Requires permanent, substantial lifestyle changes; minimal evidence of long term success
Utility of drugs/supplements or surgery; strictly complementary to lifestyle changes
How can drugs promote weight loss?
Decreasing appetite, increasing metabolism, inhibition of fat tissue, blocking absorption of calories, reducing reward/cravings for specific foods, decreasing meal size (make you feel fuller faster)
To perform these functions, drugs may act in the CNS or the digestive tract
Health at Every Size (HAES)
Weight loss doesn’t have to be a goal; instead, the idea is to support people in adopting healthy habits for the sake of health and well-being (rather than weight control)
Recognizes that health and fitness can exist at all sizes

Hypothalamus
Complex effects on ingestive behavior
Regulation of energy balance; regulation of metabolism; motor behaviors
Depends critically on interconnections with other brain regions
Two regions of hypothalamus implicated
Ventromedial hypothalamus (VMH) and Lateral hypothalamus (LH)
Two types of peptide hormones
Satiety peptides and Hunger peptides
Satiety peptides
Decreases appetite
Cholecystokinin (CCK), α-MSH, Somatostatin, Leptin, PYY3-36, GLP-1
Hunger peptides
Increase appetite
Neuropeptide Y, Galanin, Orexin-A, Ghrelin
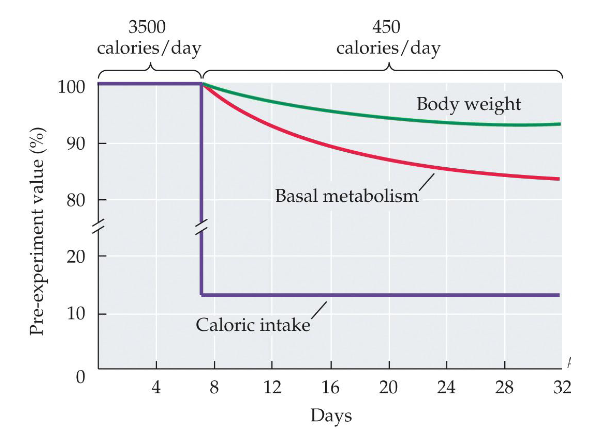
Basal metabolism
The majority of food energy is spent on things like heat, cellular activity, and maintenance of membrane potentials
Energy metabolism is under strict homeostatic control and can be adjusted
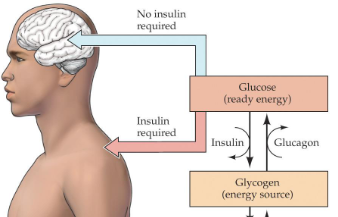
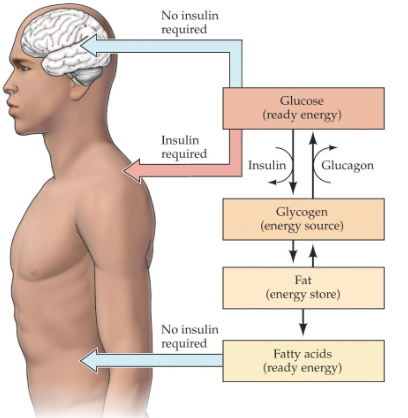
Short term storage
Insulin converts glucose to glycogen to store as reserve fuel
Glucagon converts glycogen back into glucose when stores are low
Long term storage
Insulin triggers lipid (far) storage in adipose tissues, liver, and muscles
Glucagon produces free fatty acids and ketones
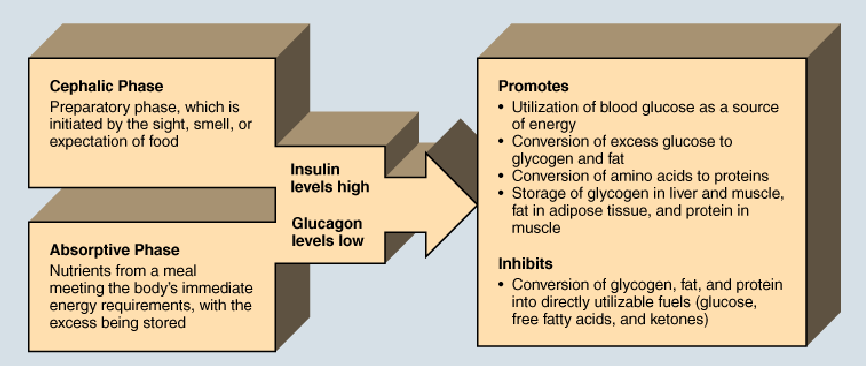
Three phases of energy metabolism
Cephalic phase, Absorptive phase, Fasting phase
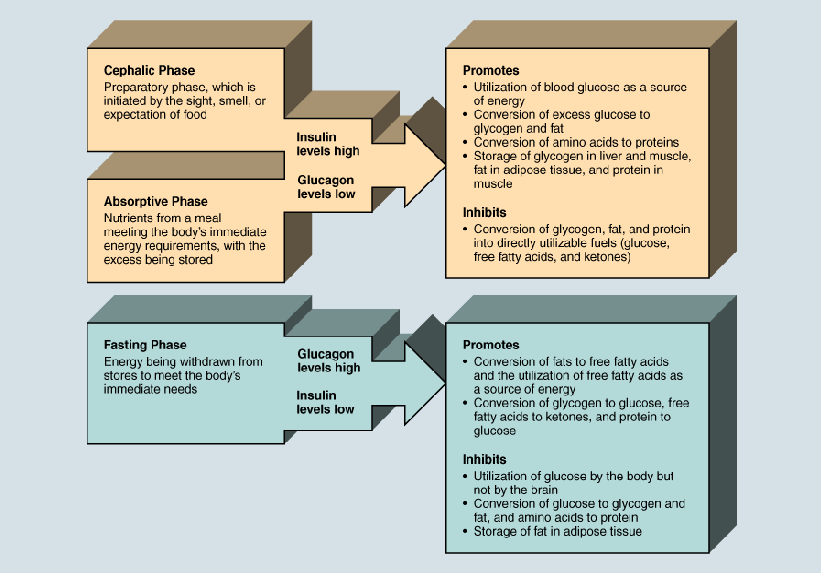
Cephalic phase
Preparatory phase, which is initiated by the sight, smell, or expectation of food
Insulin levels high; glucagon levels low
Absorptive phase
Nutrients from a meal meeting the body’s immediate energy requirements, with the excess being stored
Insulin levels high; glucagon levels low
Insulin levels high; glucagon levels low
Promotes utilization of blood glucose as a source of energy
Promotes conversion of excess glucose to glycogen and fat
Promotes conversion of amino acids to proteins
Promotes storage of glycogen in liver and muscle, fat in adipose tissue, and protein in muscle
Inhibits conversion of glycogen, fat, and protein into directly utilizable fuels (glucose, free fatty acids, and ketones)
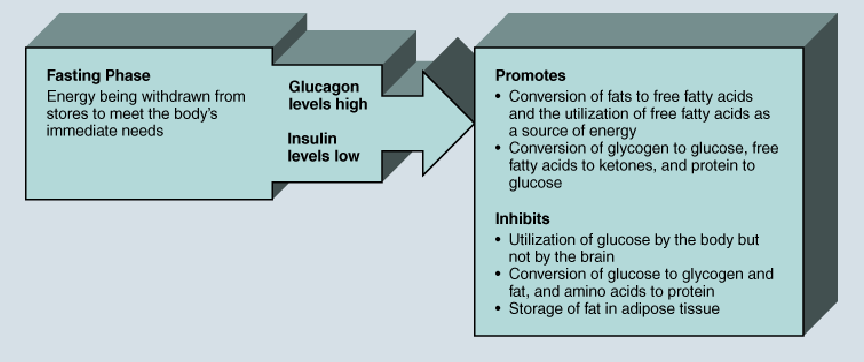
Fasting phase
Energy being withdrawn from stores to meet the body’s immediate needs
Glucagon levels high; insulin levels low
Glucagon levels high; insulin levels low
Promotes conversion of fats to free fatty acids and the utilization of free fatty acids as a source of energy
Promotes conversion of glycogen to glucose, free fatty acids to ketones, and protein to glucose
Inhibits utilization of glucose by the body but not by the brain
Inhibits conversion of glucose to glycogen and fat, and amino acids to protein
Inhibits storage of fat in adipose tissue
Insulin
Required by glucose transporters in the body to allow use of glucose in the body
Diabetes Mellitus
Lack of insulin production or reduced sensitivity to insulin
Theories of hunger
Set point theory and Positive-incentive theory
Set point theory assumption
Hunger is a response to an energy need; we eat to maintain an energy set point
Set point theory problems
Not everyone is the same size
It doesn’t fit evolutionary pressures; energy storage necessary for survival
Reductions in blood glucose or body fat do not reliably induce eating
It doesn’t account for the influence of external factors on eating and hunger (taste, learning, social cues)
Positive incentive theory
We are drawn to eat by the anticipated pleasure of eating
We have evolved to “crave” food
Eating has a positive-incentive value; multiple factors interact to determine this
Accounts for the impact of external factors on eating behavior
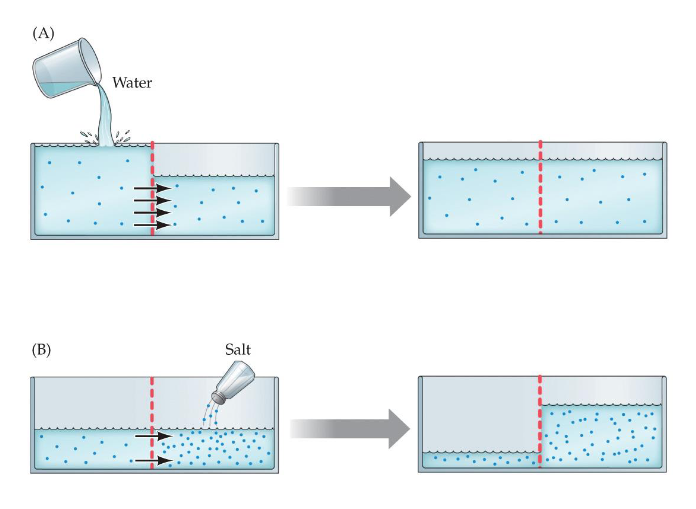
Water Balance
A precise balance of fluids and dissolved salts surround all of the cells of the body to allow proper functioning; approximately like diluted seawater
Important to maintain a decent ratio of water in the intracellular compartment vs the extracellular compartments; happens via diffusion and osmosis
Diffusion
Passive spread of the salt components (ions) to evenly space them in the water
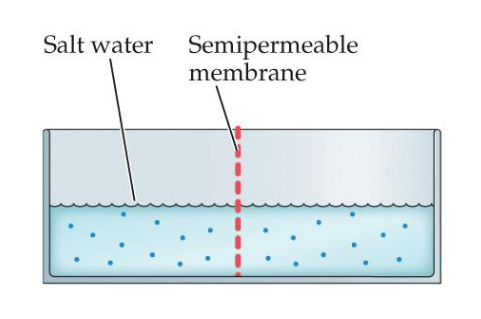
Osmosis
Movement of water molecules to equalize the concentration of two solutions on either side of a semi-permeable membrane
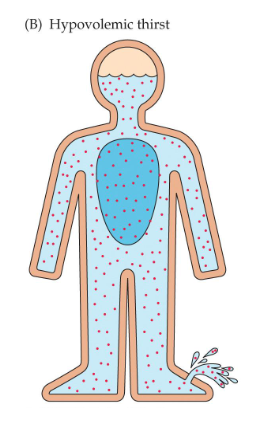
Two types of water imbalance (thirst)
Osmotic thirst and Hypovolemic thirst
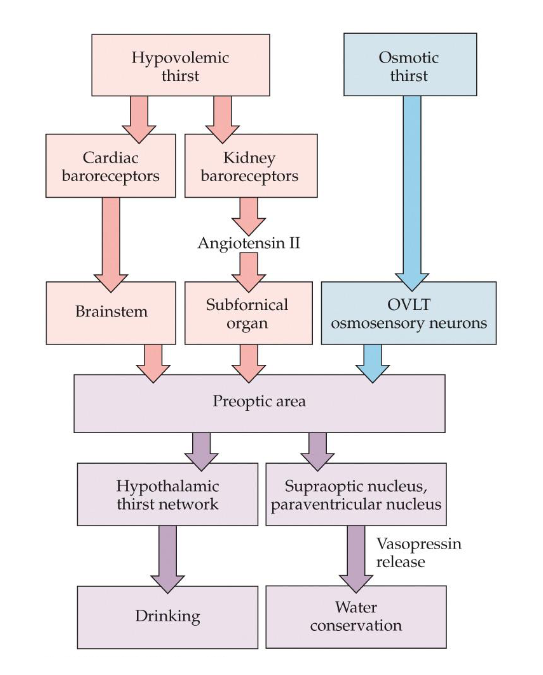
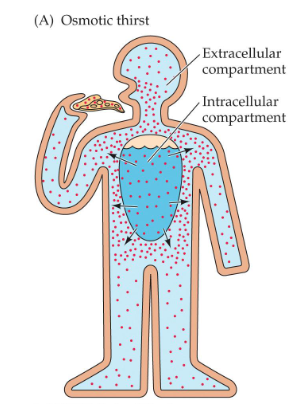
Osmotic thirst
Volume of extracellular fluid is slightly decreased due to obligatory losses
Concentration of salt in the extracellular fluid increases
Results in water being drawn out of the cells
Detected by osmosensory neurons
Hypovolemic thirst
Caused by a more significant decrease in the overall volume of extracellular fluid
Due to vomiting, hemorrhage, or sustained diarrhea; detected by baroreceptors
Doesn’t change concentration, just volume