L2:Epithelial Barriers and Mucosal Immunity (Lecture 2 notes)
1/24
Earn XP
Description and Tags
Question-and-answer flashcards covering epithelial barriers, mucus and mucins, goblet/Paneth/M cells, MALT, barrier failure and related diseases, and innate/adaptive immune cells as described in the lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
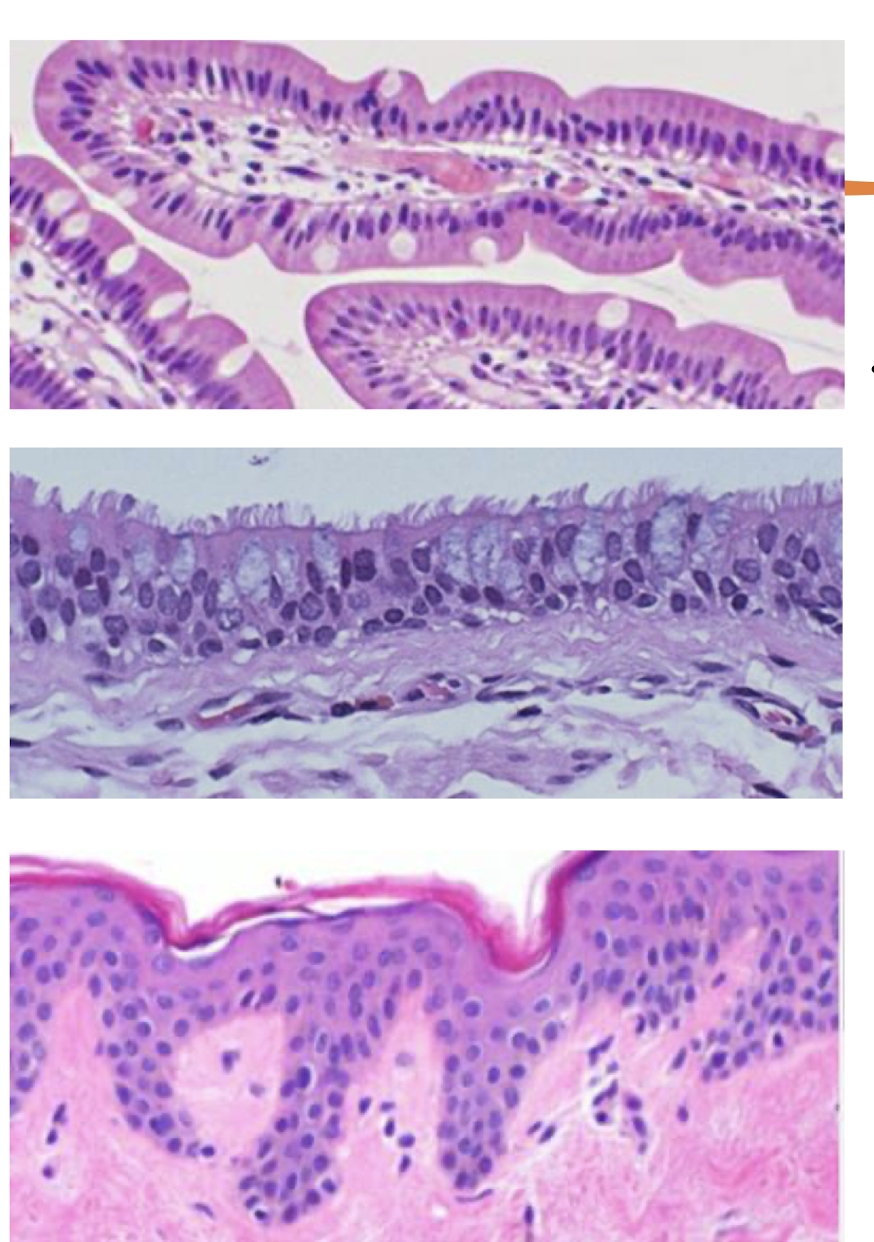
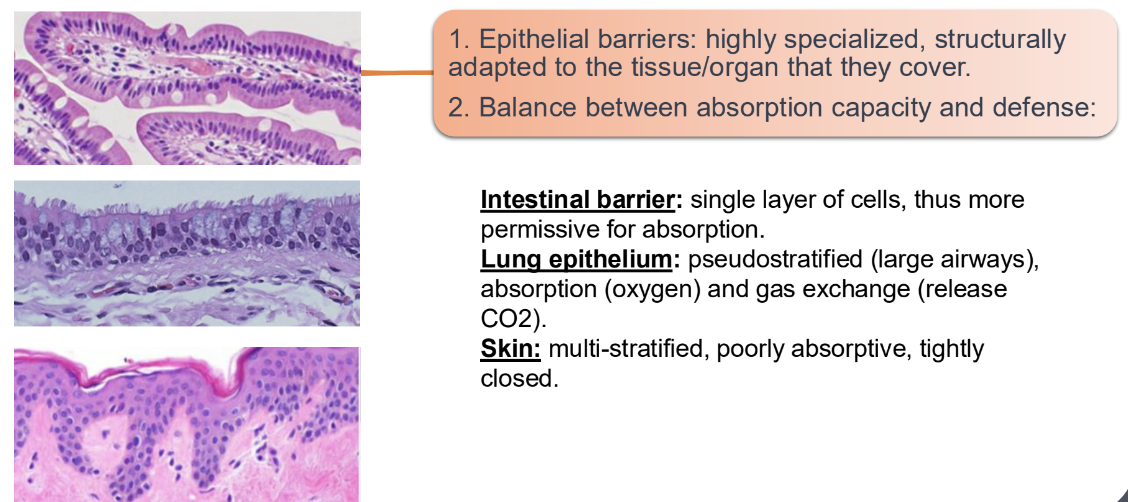
Where are epithelial barriers located and what is their primary defensive role?
Located in the skin, lungs, and digestive tract
Form a physical barrier and contain highly specialised epithelial cells adapted to the tissue/organ they encompass
Balancing absorption with defence.
Name three epithelial cell types that actively contribute to immunity.
Goblet cells, Paneth cells, and M (Microfold) cells.
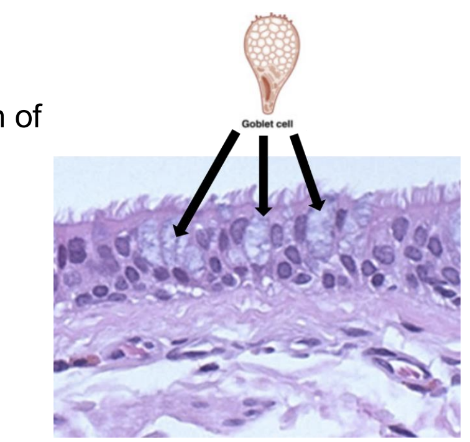
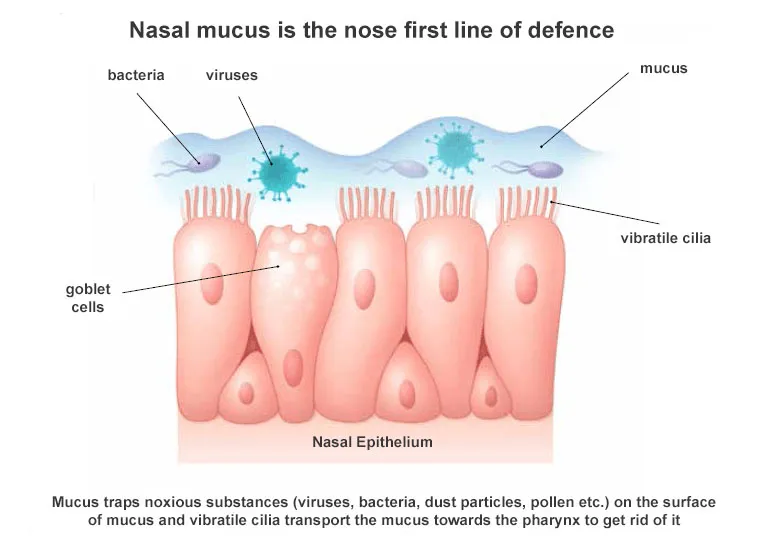
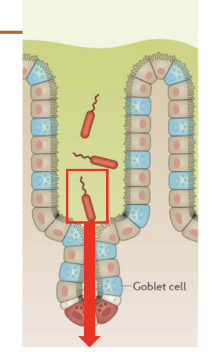
What is the main function of goblet cells in mucosal surfaces?
To produce mucins which are the monomers that oligomerise to form mucus, a film that traps and helps clear microbes from epithelial surfaces.
Mucus is found and produced by goblet cells in the airway and intestine
What is mucus and how is it formed?
Mucus is a gel-like substance that protects epithelial surfaces.
• Mucins are proteins packed into goblet cell granules which release mucin monomers, which oligomerise to form the mucus.
• Mucins expand to form mucus, in a process that requires low Ca2+ and increased pH
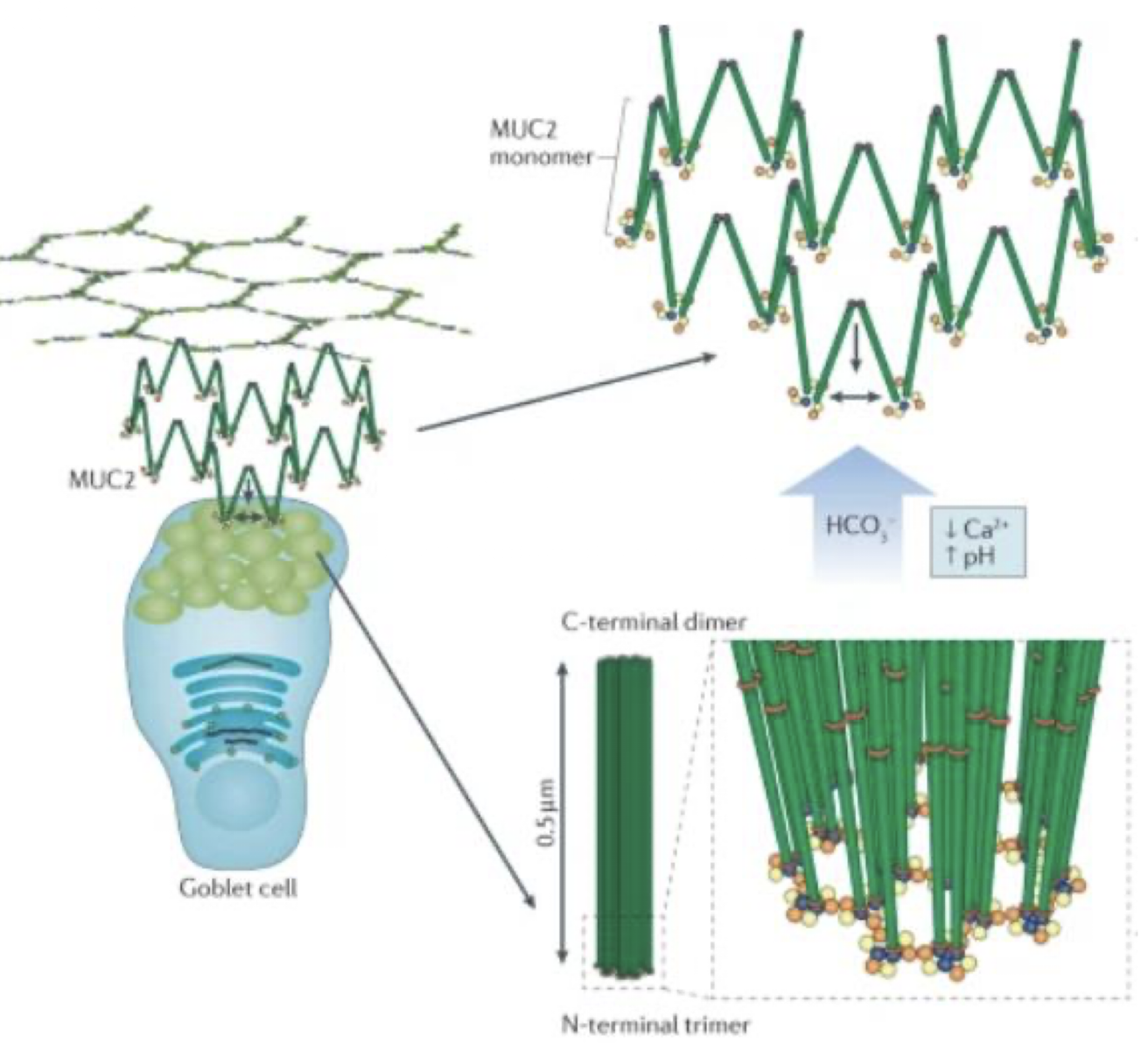
How can we categorise mucin composition?
Mucus can be divided into:
membrane bound
gel forming
Composition is different depending on the tissue and its specific function, including secreted and membrane-associated mucins.
Which mucins are most abundant in the intestine vs the airway?
MUC2 is most abundant in the intestine
MUC5AC and MUC5B are most abundant in the airway.
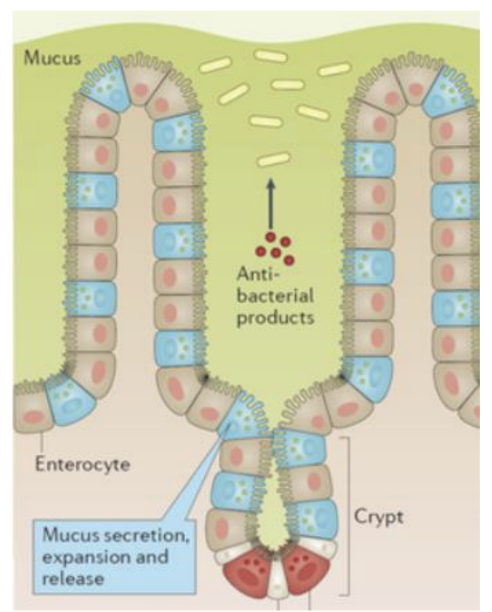
How does mucus help fight pathogens?
Forms an extra layer of protection reducing direct contact b/w microbes and the epithelium by trapping pathogens and facilitating their clearance through ciliary movement.
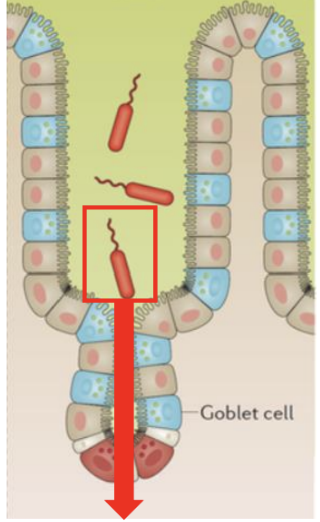
How have certain bacteria evolved to evade mucous?
Infectious agents e.g. Salmonella Typhi often use specialised mechanisms, such as flagella, to “swim” through mucus and reach the epithelium via the crypt where stem cells are found
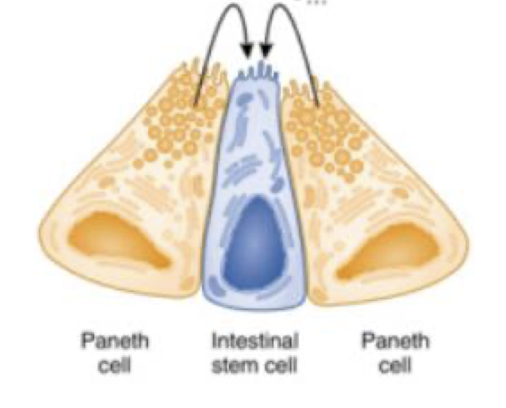
Where are Paneth cells located and what are the 2 types of signals they provide?
Located in intestinal crypts & surround stem cells, supporting homeostasis of cells providing 2 types of signals;
Secrete bactericidal mediators like lysozyme and defensins
Provide stem cell–stimulating factors to promote proliferation and differentiation, allowing the epithelial cells to regrow post injury from infection or damage.
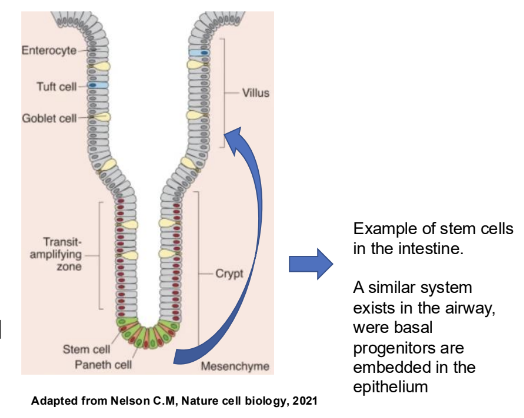
how do epithelial barriers form and maintain themselves?
Via stem cells that continuously divide and differentiate,
Stem cell progenitors can migrate and differentiate into the different types of epithelium
Renewal occurs during homeostasis, replacing old cells or in disease, healing wounded tissues and compensating for loss of cells
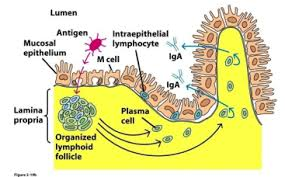
What are M cells and what is their exact role?
M cells are microfold cells in the gut and airway that act like ‘security cameras’ constantly surveying for possible harmful infectious agents that could trigger the immune response.
Found in proximity of MALT
They are responsible for transporting antigens from the lumen to immune cells, facilitating the initiation of an immune response.
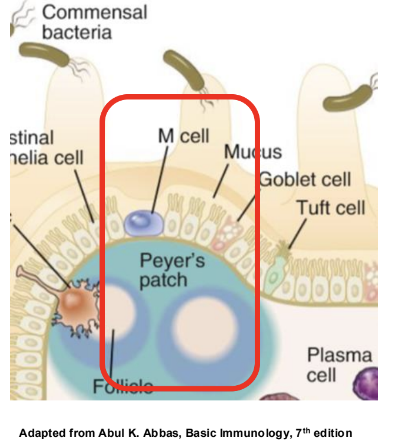
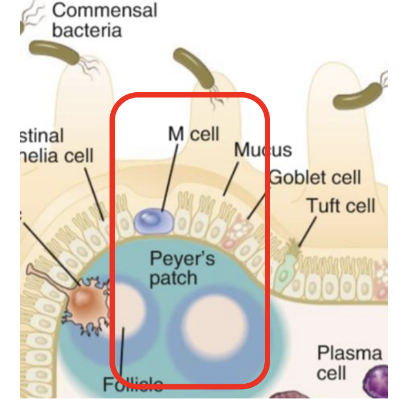
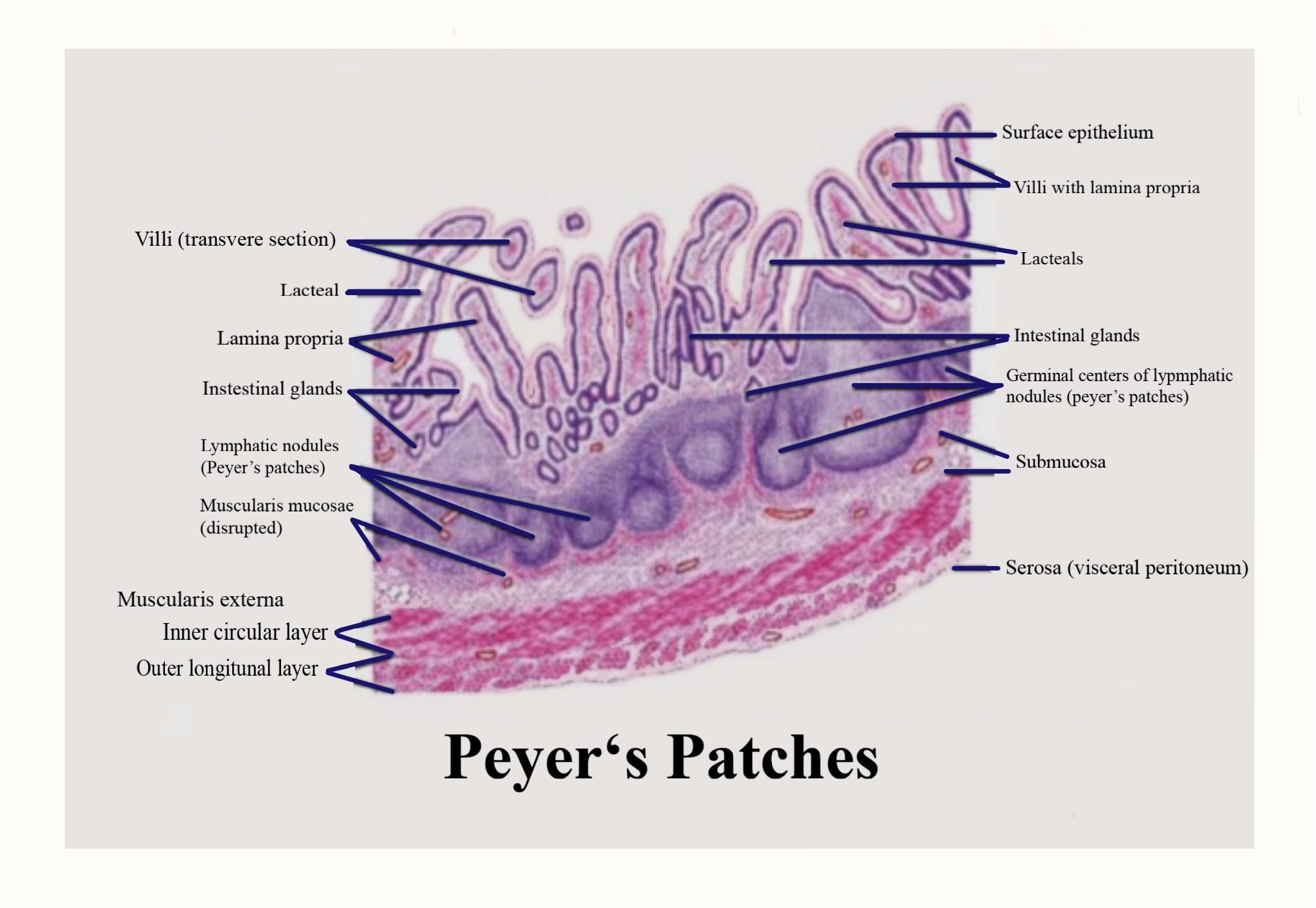
what is the function of Peyer’s patch in relation to M cells?
group of well-organised lymphoid follicles located in the lamina propria and submucosa of the distal portion of the small intestine
Antigen sampling: M cells in the follicle-associated epithelium, a specialised layer of cells covering the Peyer's patch, capture antigens from the intestinal lumen.
Immune cell activation: These antigens are then passed to immune cells like dendritic cells and macrophages, which are positioned just beneath the M cells.
Immune response initiation: These antigen-presenting cells activate lymphocytes (B cells and T cells), which are crucial for mounting an immune response.
Define MALT and its significance in mucosal immune defence
Mucosal-associated lymphoid tissue;
Immune structures near mucosal surfaces containing antigen-presenting cells i.e DC and MP as well as B and T lymphocytes
M Cells allow the controlled pass of microbial components from the exterior into MALT.
• APCs capture these and present them in their surface.
• Lymphocytes recognise these to learn about potential threats
Where are examples of where MALTs are located?
In the intestinal tract (Peyer's patches)
Pharynx (tonsils), and bronchial-associated lymphoid tissue (BALT), among others.
What is the relationship between M cells and MALT?
M cells shuttle antigens in a controlled manner to MALT where antigen-presenting cells like lymphocytes can THEN capture and present them to lymphocytes;
*M cells do not present antigens themselves.
What immune cells are typically present in MALT?
Antigen-presenting mononuclear phagocytes (APC) (dendritic cells and macrophages) and B and T lymphocytes.
What is the first line of defence described in the lecture
Prevention through barrier formation to prevent injury and pathogen entry at the skin, gastrointestinal tract, and lungs.
How do barrier functions vary by tissue location regarding absorption and defence?
Intestinal barrier is a single layer of cells and more permeable for absorption
Lung epithelium is pseudostratified (various cell layers i.e large airways) , absorption of oxygen and for gas exchange (release CO2)
Skin is multi-stratified and tightly closed, prioritising defense over absorption.
What happens when barrier function is compromised?
Infections by pathogens (e.g., S. aureus exploiting skin barrier defects) and associations with chronic inflammatory diseases like Crohn's disease, ulcerative colitis, psoriasis, asthma, and eosinophilic esophagitis.
Examples of pathogens exploiting barrier defects mentioned?
Staphylococcus aureus exploits skin barrier defects; Salmonella Typhi can swim through mucus to invade epithelial cells and replicate.
What are the two main signals Paneth cells provide to maintain the intestinal stem cell niche?
Bactericidal mediators (lysozyme and defensins) and stem cell–stimulating factors that promote proliferation and differentiation.
How often does intestinal epithelium renew itself and what cells drive renewal?
Approximately every 48 hours; renewal driven by intestinal epithelial stem cells and progenitors.
Where are basal progenitors located and what is their role?
Located in the airway epithelium; they differentiate into various epithelial cell types to renew the barrier.
What is a cornified envelope and which tissue has it?
A keratinised outer layer found in the skin; the skin has no mucus due to this cornified envelope.
Which tissues contain goblet cells and mucus-producing capacity?
Goblet cells are abundant in the intestine and lung; the skin lacks mucus and relies on a cornified envelope.