Pathology 3: Neutrophils, eosinophils and immune complex-mediated disease
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
What are some causes of neutrophil-rich inflammation?
Trauma, foreign material, thrombosis, burns, necrosis, immune complexes
Words for neutrophil dominated lesion
Purulent, suppurative, neutrophilic
How long does it take neutrophils to enter the tissue?
Within hours
How long does pus take to form?
Days, almost always from bacterial infection

Morphologic diagnosis
mesenteric abscess, severe chronic focal neutrophilic/suppurative mesenteric lymphadenitis (began in mesenteric lymph node)

Morphologic diagnosis
localized subcutaneous creamy abscess
Morphologic diagnosis
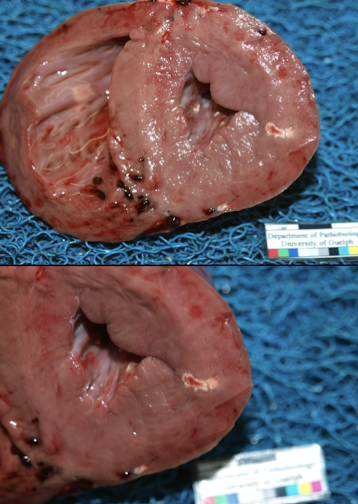
Inter-ventricular septum and into the R ventricle of the heart is multifocal suppurative and necrotizing myocarditis
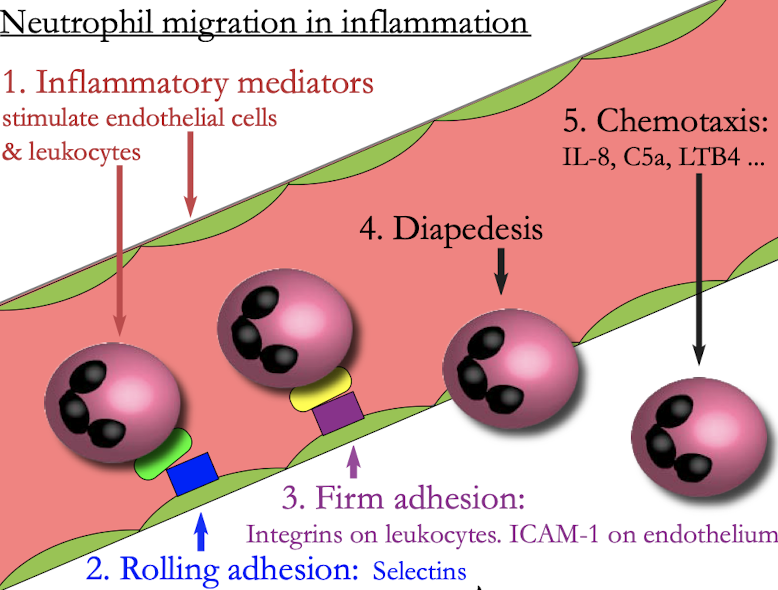
How does a neutrophil get to the site of infection?
neutrophil migration from the blood into issues is a carefully controlled process, that includes selectin mediated rolling adhesion to endothelium, integrin mediated firm adhesion to endothelium, trans-endothelial migration, and directed migration or chemotaxis toward the inflammatory stimulus.
How long does an abscess take for form?
At least a Week
What are some terms we can use to describe inflammation dominated by neutrophils ± mucus?
suppurative, purulent, mucopurulent, catarrhal

Tarsus from a dairy cow
Pathologic process
Acute or chronic
Benefits of the reaction
Harm of the reaction
Suppurative inflammation & fibrosis
Chronic (thick white fibrous tissue)
contain and wall off the bacterial infection
reduced mobility, pain
What are some outcomes of neutrophilic/suppurative inflammation?
resolution
Chronic suppurative inflammation
Stimulation of fibrosis
Containment abscess formation

What is this an example of?
Neutrophilic/suppurative inflammation
What’s the mechanism for neutrophil response to inflammation?
bacteria come in
Recognized by phagocytes, complement, antibody
Inflammatory mediators stimulate endothelial cells and leukocytes
Rolling adhesion: selections
Firm adhesion: interns on leukocytes. ICAM-1 on endothelium
Diapedesis
Chemotaxis: IL-8, C5a, LTB4
What is neutrophil chemotaxis?
Directed migration toward a stimulus.
Neutrophils move toward higher concentrations of inflammatory mediators by extension of lamellipodia that adhere to tissue matrix
Steps for phagocytosis
Opsonins enhance the recognition of bacteria by leukocytes
IgG → FcγR (acquired), C3b → CR3 (Innate & acquired), SP-A MBL(innate)
What do Toll-like receptors recognize?
the conserved structures on pathogen surfaces leading to cellular activation such as production of inflammatory mediators
What specificity does TLR 7, 8 trigger for?
single stranded RNA (RNA viruses)
What are some processes of killing bacteria?
Oxidative killing (peroxide H2O2)
Antimicrobial protein in neutrophil granules (lysozyme)
Proteolytic enzymes (collagenase)
How do leukocytes recognize bacterial infections?
Opsonization (antibody)
PAMPs (TLR)
Cytokines from other cells
How do leukocytes kill bacteria?
Oxidative killing
Proteolytic enzymes
Bactericidal proteins
NETs
What are the roles of neutrophils?
contain or eliminate infection
from impaired organ function
injury to host tissue
stimulation of fibrosis
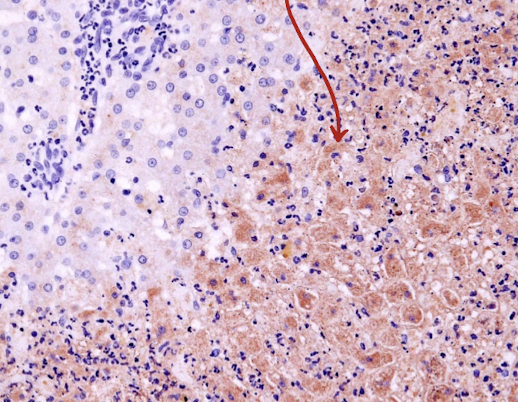
What does malondialdehyde indicate?
Oxidative stress (brown immunohistochemical staining)
Where do we find neutrophils in healthy animals in the absence of inflammation?
blood and lymph nodes
What calls neutrophils to site of infection?
TNF, Type 1 and 2 interferons
How do neutrophils recognize that infection is present?
IgG and complement
What are 2-4 ways neutrophils kill bacteria?
NETs, cytotoxic granules
What happens to neutrophils when the infection is resolved?
they die, phagocytosed by macrophages
What role do eosinophils play in inflammation?
Stimulated by parasites and allergies. Play similar roles of neutrophils but they are not phagocytic cells, involved in oxidative injury, the proteins in granules injure cell membranes
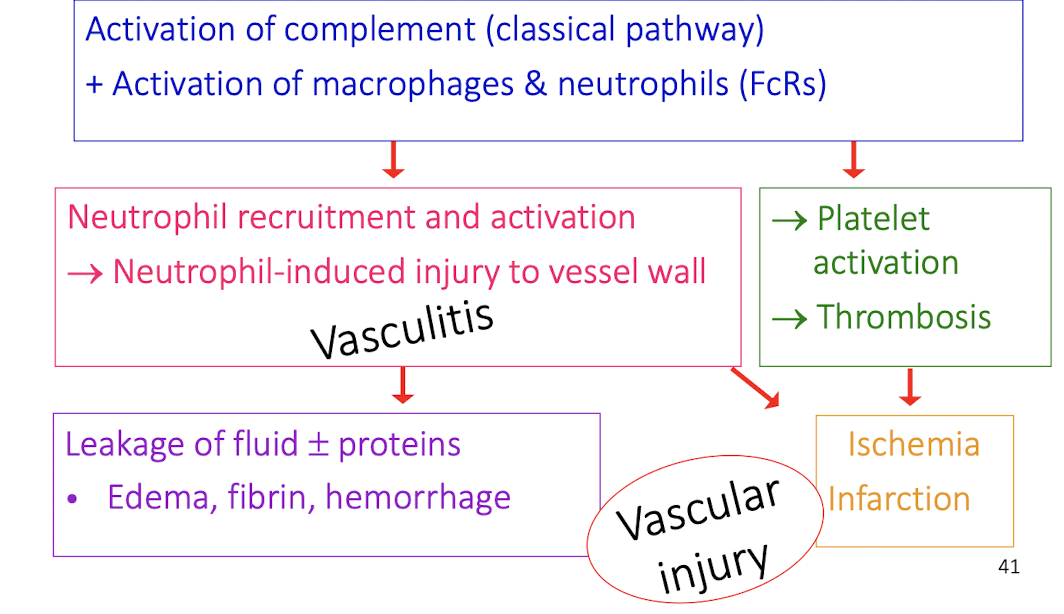
What is Type 3 hypersensitivity?
Immune complexes: antibody + antigen
Systemic reactions. Circulating immune complexes deposit in vessel walls, synovium, glomeruli, skin
Antigen localized in vessel walls may react with circulating antibody
Type 3 hypersensitivity: Sequelae to immune complex deposition
activation of complement (classical) and activation of macrophages and neutrophils (FcRs)
neutrophil recruitment and activation from injury to vessel wall
leakage of fluid and proteins which causes edema, fibrin, hemorrhage
platelet activation, thrombosis
ischemia infarction
vascular injury
Where in the body do type 3 hypersensitivity reactions occur?
Disease manifestation depends on the site of immune complex deposition
Joints, glomeruli, skin, uveitis, many tissues at once
What would happen if an animal did not have any of β-integrin / CD18?
genetic defect in the gene encoding CD18 and causes impaired neutrophil migration to site of infection
What ways do antibodies protect against bacterial infection?
bind to bacteria and activate complement mediated lysis
opsonizes the bacteria to promote killing by neutrophils and macrophages
binds bacterial cell adhesion proteins to block colonization of surfaces
binds and neutralizes bacterial toxins
Vasculitis
Inflammation that specifically targets blood vessel walls
What main cells are recruited during allergy and parasitism stimuli?
Eosinophils
When do neutrophils phagocytose bacteria?
when opsonized by immunoglobulin , C3b, or other opsonins
How are ingested bacteria killed?
Proteolytic enzymes, bactericides proteins in neutrophil granules, and oxygen radicals like hypothalamus acid
What can kill extracellular bacteria?
Neutrophil traps
How can neutrophil accumulation cause harm?
Space occupying lesion, inducing proteolytic or oxidative injury to host tissues, trigger thrombosis, scarring of tissues
What triggers formation of immune complexes?
Persistent antigenic stimuli, neoplasia, virus, immune mediated drug reaction, autoimmune reaction
What incite a neutrophil inflammatory response?
Aggregates of antigen and antibody deposited in the wall of blood vessels
Where are immune complex diseases most apparent
In well vascularized tissues such as synovium, renal glomeruli, skin
Causes vasculitis
How do eosinophils kill parasites?
Synthesis of oxygen radicals and secretion of basic proteins from their granules (can also damage tissue)