Male Reproductive System
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
25 Terms
Testes
Male gonads - male reproductive organs. They produce sperm and androgens like testosterone that are active throughout the reproductive lifespan of the male.
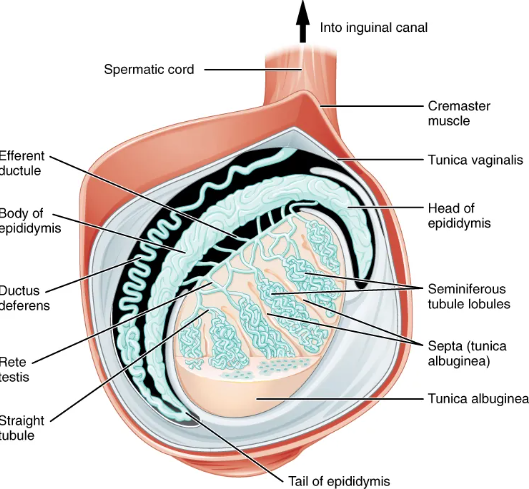
Testes structure
Testes are housed within the scrotum. Surrounded by two layers of connective tissue. The outer tunica vaginalis is a serous membrane that has a parietal and a thin visceral layer.
Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue covering the testis itself. It invaginates to form septa that divide the testis into 300-400 lobules.
Within lobules, sperm develop in seminiferous tubules.
Descent of the testis
During the seventh month of male fetus development, each testis moves through the abdominal musculature to descend into the scrotal cavity.
Cryptorchidism
One or both testes fail to descend into the scrotum prior to birth.
Seminiferous tubule structure
Composed of developing sperm cells surrounding a lumen, the hollow center of the tubule, where formed sperm are released into the duct system of the testis. Lumen → straight tubules → meshwork of tubules called rete testes.
Sperm leave rete testes and testis through 15 to 20 efferent ductules crossing the tunica albuginea.
Sertoli cells
Surrounding all stages of developing sperm cells are elongate, branching Sertoli cells.
A type of supporting cell called a sustentacular cell (sustentocyte) typically found in epithelial tissue.
Sertoli cells secrete signaling molecules that promote sperm production and can control whether germ cells live or die.
Blood-testis barrier
Tight junctions between these sustentacular cells create the blood-testis barrier, which keeps bloodborne substances from reaching germ cells and keeps surface antigens on developing germ cells from escaping into the bloodstream and prompting an autoimmune response.
Spermatogonia
Least mature cells line the basement membrane inside the tubule.
Spermatogonia are the stem cells of the testis and are able to differentiate into different cell types throughout adulthood.
Spermatogonia divide to produce primary and secondary spermatocytes, then spermatids, then formed sperm.
Spermatogenesis
The process that begins with spermatogonia and concludes with the production of sperm.
Length of spermatogenesis
One production cycle, from spermatogonia through formed sperm, takes 64 days.
A new cycle starts every 16 days.
When do sperm counts begin to decline
After age 35.
Spermatogenesis process
Two identical diploid cells result from spermatogonia mitosis. One of these cells remains a spermatogonium and the other becomes a primary spermatocyte.
The result after meiosis I is two cells, called secondary spermatocytes, each with only half the number of chromosomes.
The second meiotic division results in a total of four cells with only half of the number of chromosomes. Each of these new cells is called a spermatid.
Spermiogenesis transforms early spermatids, reducing the cytoplasm, and beginning the formation of a true sperm. This occurs in the portion of the tubule nearest the lumen.
Sperm are released into the lumen and move along ducts in the testis toward the epididymis.
Structure of a sperm
Sperm have a distinctive head, mid-piece and tail region.
The head of the sperm contains an extremely compact haploid nucleus with very little cytoplasm.
The acrosome covers most of the head of the sperm cell as a cap filled with lysosomal enzymes important for fertilization.
Tightly packed mitochondria fill the mid-piece of the sperm. ATP produced by these mitochondria power the flagellum, which extends from the neck and mid-piece through the tail, enabling movement.
The central strand of the flagellum is called the axial filament.

How many sperm are produced daily?
100 - 300 million sperm.
Role of Epididymis + transport of sperm through
From the lumen to the seminiferous tubules, sperm are surrounded by testicular fluid and moved to the epididymis.
The epididymis is a coiled tube attached to the testis where new sperm continue to mature.
Sperm are moved along by contraction of smooth muscle lining epididymal tubes. As they move along, they continue to mature and acquire their ability to move on their own.
More mature sperm are stored in the tail of the epididymis until ejaculation occurs.
How long does it take for sperm to move through the coils of the epididymis?
12 days
Ejaculation
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle to the ductus deferens (vas deferens).
Ductus deferens
Thick muscular tube bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord.
Each ductus deferens extends superiorly into the abdominal cavity though the inguinal canal in the abdominal wall.
Ductus deferens continues posteriorly into the pelvic cavity, ending posterior to the bladder where it dilates in a region called the ampulla.
Vasectomy
Surgical sterilization to interrupt sperm delivery- performed by cutting and sealing a small section of the ductus deferens.
Semen
Thick milky fluid that ejaculates. Sperm make up only 5% of the final volume.
Semen is produced by the seminal vesicles, the prostate, and the bulbourethral glands.
Seminal Vesicles
As sperm pass through the ampulla at ejaculation, they mix with fluid from the associated seminal vesicle.
The seminal vesicles are glands that contribute ~60% of semen volume. Seminal vesicle fluid contains lots of fructose which is used by sperm mitochondria to generate ATP when traveling through female reproductive tract.
Ejaculatory Duct
When the fluid contains both sperm and seminal vesicle secretions, it moves into the ejaculatory duct, a short structure formed from the ampulla of the ductus deferens and duct of the seminal vesicle.
The paired ejaculatory ducts transport seminal fluid into the prostate gland.
Prostate Gland
Sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra. Size of a walnut, formed of both muscular and glandular tissue.
Secretes an alkaline milky fluid to passing seminal fluid (semen), to coagulate then decoagulate the semen following ejaculation.
Why does semen coagulate?
So it is retained within the female reproductive tract.
Benign prostatic hyperplasia
Abnormal growth of the prostate - leads to number of lower urinary tract symptoms such as frequent and intense urges to urinate, weak streams.