Week 10 - Pain Pt 2, Complications, Euthanasia
1/172
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
173 Terms
Pain is ______________.
- A subjective experience
3 multiple choice options
How do our treatments for pain differ from patient to patient?
- Since patients vary widely in response to pain you must individualize treatment
How do we determine/assess pain in our veterinary patients?
- Subjective behavioral observations (species specific pain related behaviors)
- Predicting pain by experience and anticipated level of pain associated with a condition or procedure
- Physiologic response (HR, RR, BP, etc)
- Patient response to palpation/movement
- Patient response to therapy
What is the 4th vital sign?
- Pain
In a canine or feline patient in pain, what might you visually observe? (behavior, PE findings, etc)
- Reluctance to move
- Reluctance to lie down
- Constantly shifting positions
- Licking lips
- Submissive/guarding position
- Aggression
- Vocalization
- Hair coat changes/grooming
- Postural changes
- Facial expressions
- Trembling or shaking
- Tachypnea or panting
- Depression
- Myofascial/gait/posture changes
In horses or cattle who are in pain, what might you visually observe? (behavior, PE findings, etc)
- Facial expressions (equine grimace scale - stiff backward ears, orbital tightening, tension above eye area, prominent strained chewing or clenched teeth, mouth strained and pronounced chin, strained nostrils with flattening of profile)
- Reluctance to move
- Vocalization
- Stomping feet
- Decreased appetite
- MSK (weight bearing changes)
- Sweating (horses)
- Head low position
- Recumbency
What is an important, common sequelae of chronic pain in horses?
- TMJ
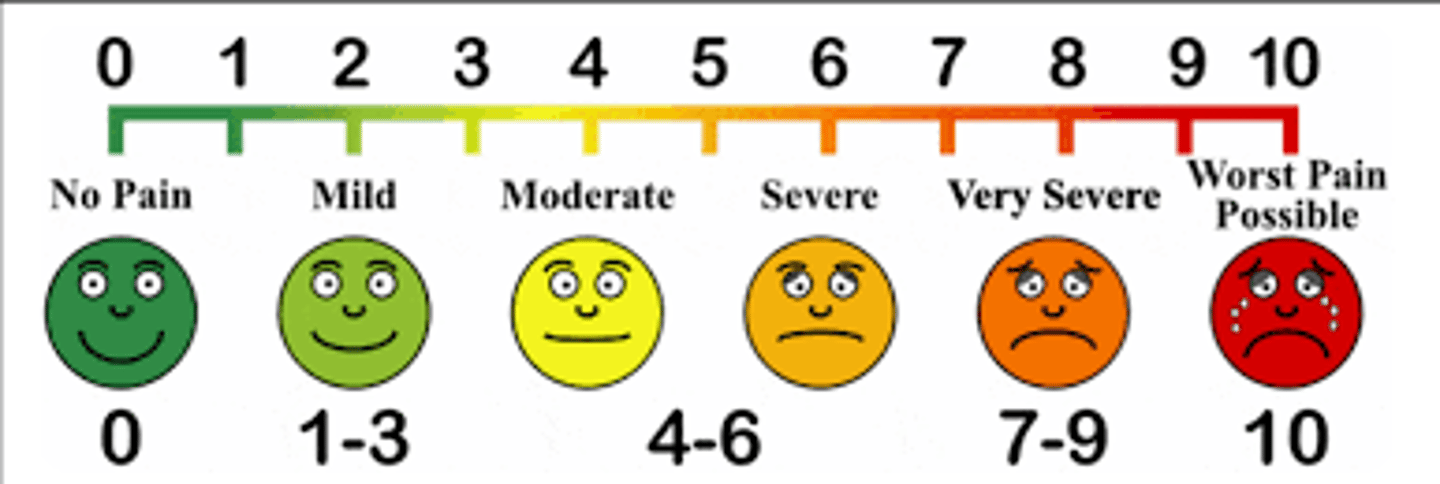
What are pain scoring visual analog scales? Are they applied well in veterinary patients?
- Scales of 1-100 (1-10) orally or pictures to attempt to objectively report pain - used in humans!
- Not very applicable to veterinary patients because our patients cannot talk to us and there are many interobserver variations and inconsistencies
What objective pain assessment tools are better applied in veterinary medicine?
- Glasgow Composite Pain Scale
- CSU Acute Pain (dog, cat, horse)
- Grimace Scales (mouse, rat, rabbit, equine)
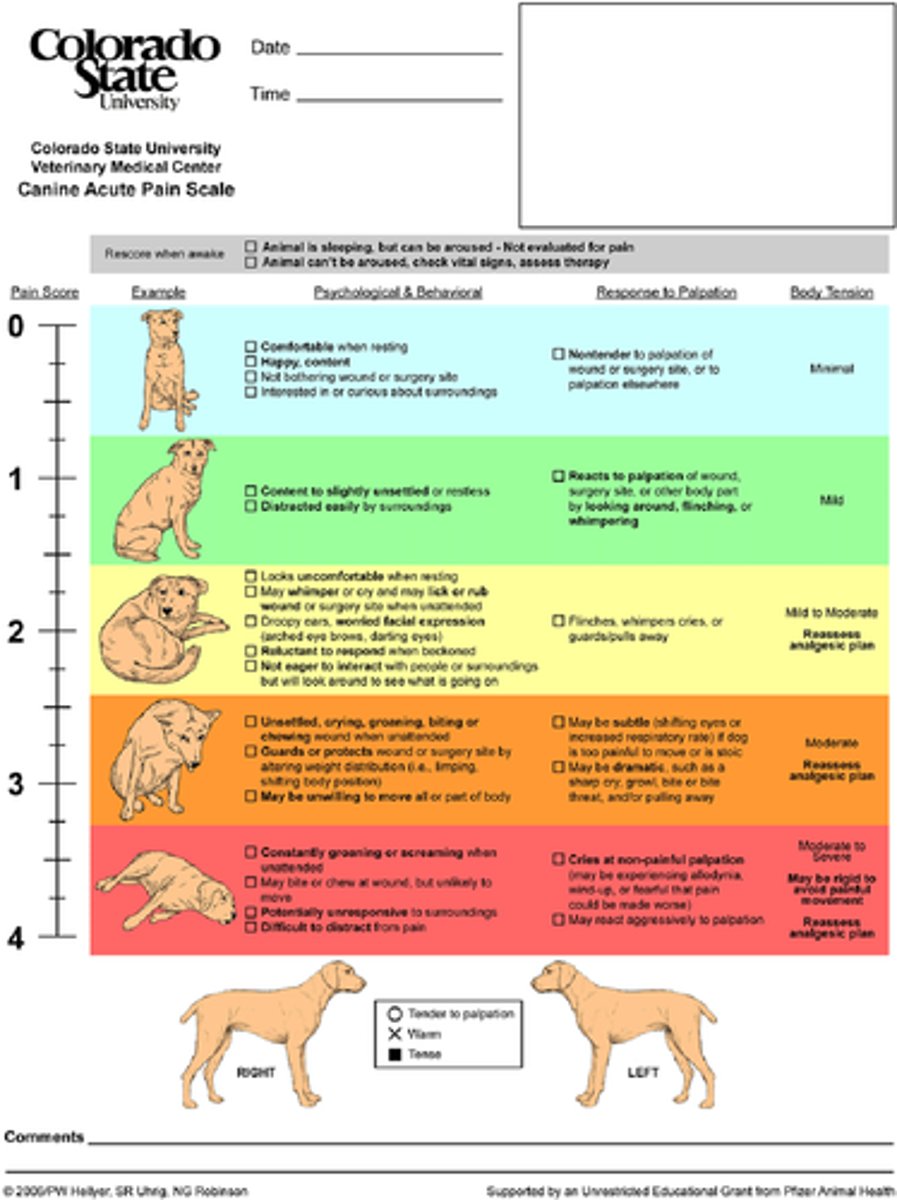
In order to use the Glasgow Composite Pain Scale, what must you do? How does this help you?
- Get a baseline assessment when the patient arrives in the clinic
- This provides a comparison for post operative pain
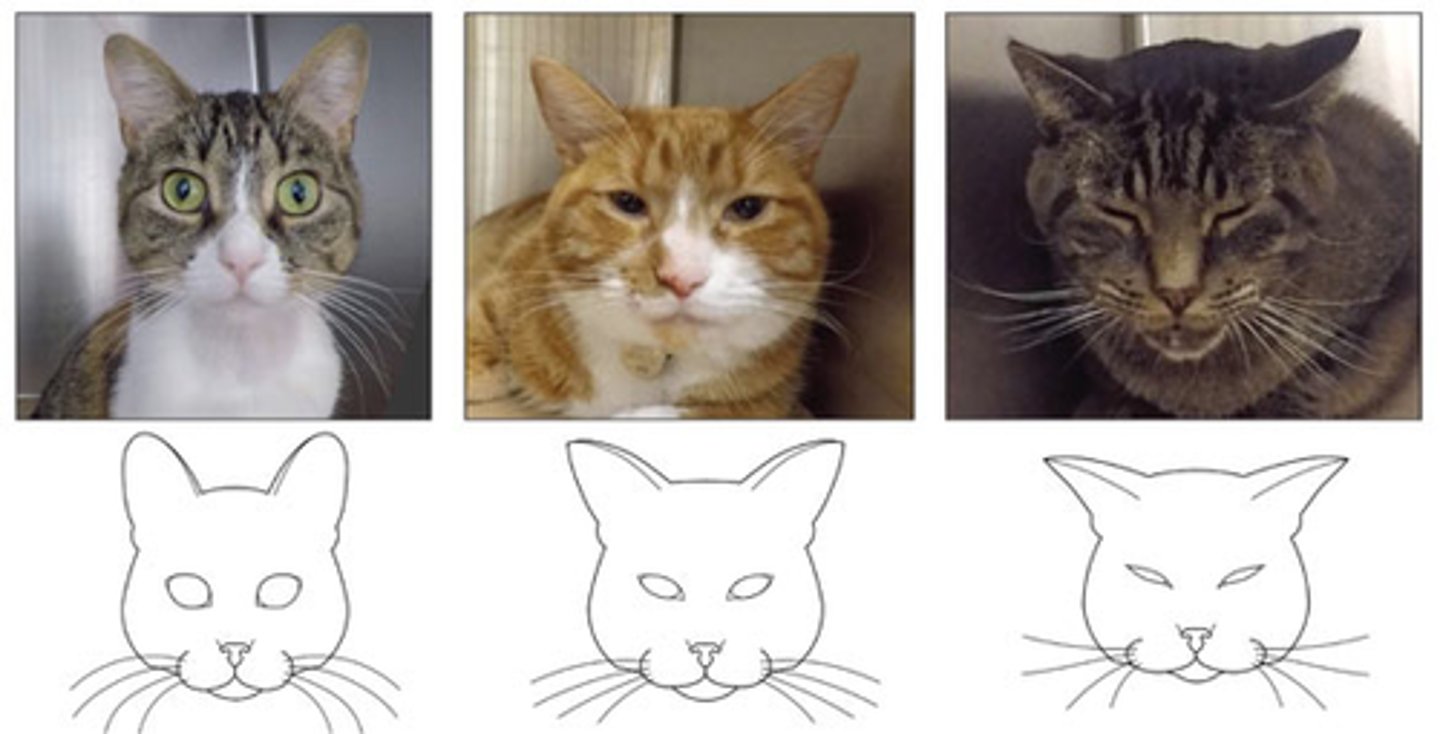
In reference to the feline grimace scale, what are the '5 action units'?
- Eyes, ears, muscles, whiskers, head position
In reference to the equine grimace scale, what are the '5 action units'?
- Ears, orbital position, tension above eyes, chewing muscles, mouth position/straining, nostril flare or flat
What is the ultimate test of proper pain assessment?
- Patient response to therapy
What is the goal of long term pain therapy?
- Titration of therapy to lowest possible dose
What are the 3 major times for a surgical/anesthetic patient that pain control should be considered?
- Preemptive
- Intra-op
- Post-op
What is multimodal analgesia?
- Use of multiple drugs and techniques with different MOAs to produce optimal analgesia
How do we provide multimodal analgesia to our patients/
- Interrupt/modulate pain at various sites in the pain pathway
- Activate/inhibit different receptors
What is pre-emptive pain control?
- Before the painful event is occurring, stop the process before it happens and eliminate the possibility of hypersensitization or wind up pain
What is involved in pre-emptive pain control?
- Pain scoring
- Pre-emptive analgesia (pre-med opioid/NSAID or local anesthesia)
- Local/regional anesthesia
What is intra-operative pain control?
- Pain control management during a procedure
How is pain controlled intraoperatively?
- CRIs ((FLK, HLK, MLK, DLK, LK)
- Lidocaine/Ketamine with Fentanyl, Hydro, Methanone, or Dexmedetomidine)
- Continued local/regional anesthesia
What is post operative pain control?
- Immediate post-op analgesia (up to 2 weeks post-operatively)
- Long term (patient no longer needs analgesia, but provide rehabilitation)
Name 5 goals of pain therapy
- Eliminate/reduce pain
- Manage/treat inciting cause of pain
- Improve patient comfort (non-pharmacological methods... nursing care!)
- Eliminate/suppress pain behaviors (promote normal behavior patterns)
- Remove/reduce stress/distress (sedative/anxiolytics)
What are the 5 major therapeutics we use to control pain?
- Opioids
- Alpha 2 adrenergic agonists
- NMDA receptor agonists
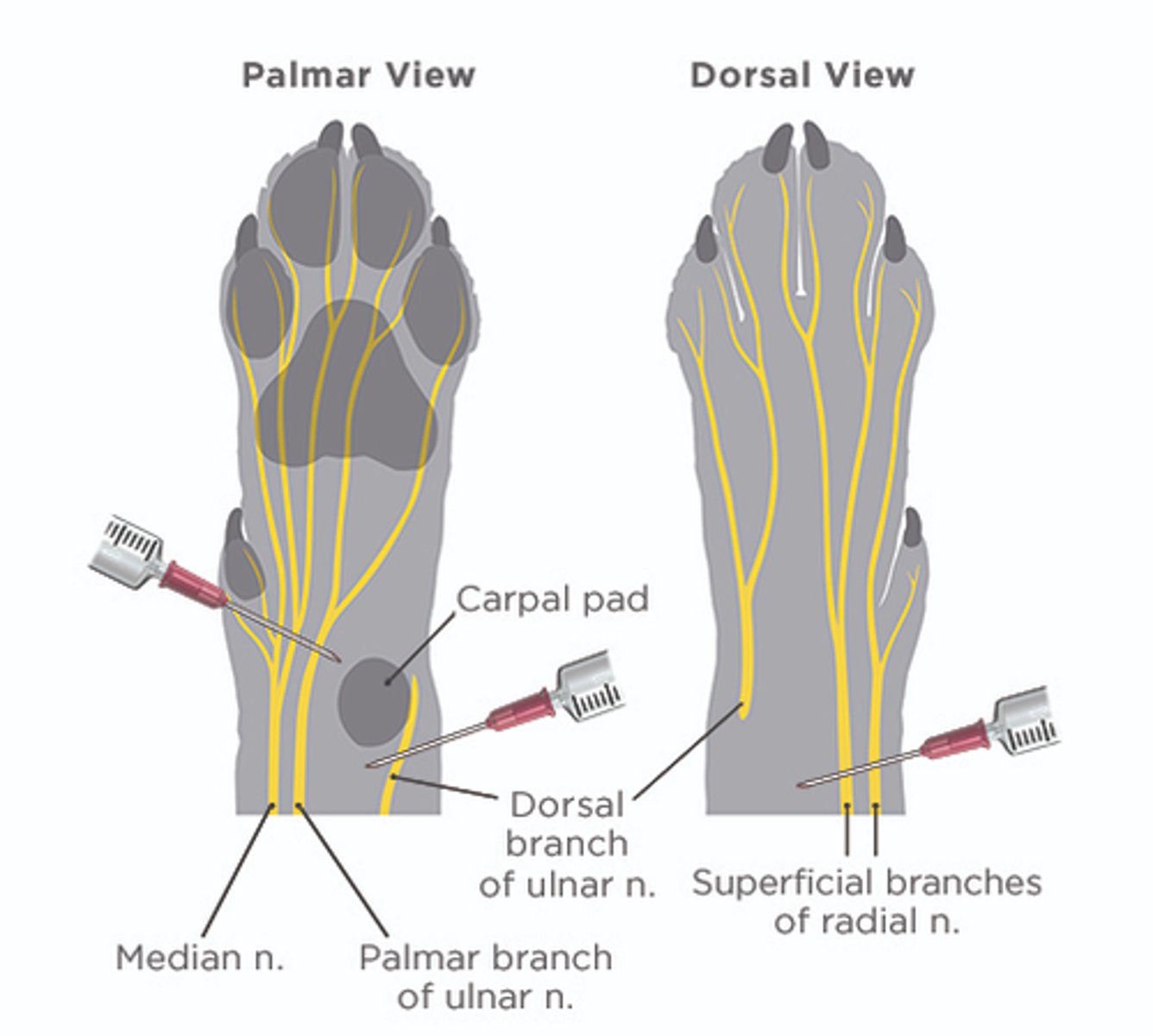
- Local anesthetics
- NSAIDs

How do opioids work? Where does it have its main effects? What effects does it have?
- Work by inhibiting glutamate release at dorsal horn of spinal cord
- Effects in brain
- Decrease sympathetic tone
Describe the mechanism of action of alpha-2 adrenergic agonists. Where does it have its main effects? What effects does it have?
- Like opioids
- Profound effects in brain
- Muscle relaxation
Where do NMDA receptor antagonists work?
- Dorsal horn of the spinal cord
- Some affect the brain
Where do local anesthetics block?
- At fast sodium channels
Describe the mechanism of action of NSAIDs
- Inhibit COX pathway
- Prevent production of inflammatory mediators
Do benzodiazepines provide analgesia?
- NOPE
What do benzodiazepines do for the patient?
- Muscle relaxation
What non-pharmacological interventions might you consider to help manage pain?
- Physiotherapy
- Acupuncture
- Massage
- Heat/cold therapy
- Laser therapy
- Electromagnetic therapy

Describe the mechanism of action of opioids
- Work at many levels
- Inhibit somatosensory afferents at supraspinal levels
- Activate descending inhibitory pathways
- Inhibit pain transmission in dorsal horn of spinal cord (bind to receptors on nociceptive neurons; inhibit activity of nociceptors)
- Peripheral actions too (opioid receptors found on inflammatory cells; may suppress release of cytokines and other sensitizing compounds)
Opioids are best used for what level of pain?
- Mild to severe
- Ex. trauma or surgical pain
Opioids have a lesser efficacy in what kind of pain?
- Chronic pain states and neuropathic pain
What side effects are seen with opioid use?
- Minimal to moderate side effects
- Behavioral side effects are species and dose dependent
- Possible hyperthermia in cats
- Possible respiratory depression
What considerations should be made when choosing an opioid?
- Onset of action of the opioid
- Duration of action of the opioid
- Opioid receptor activity (agonist v agonist antagonist)
- Route of administration
- Pain severity of the patient
What are the different routes of administration of opioids?
- Systemic (IV, IM, SQ)
- Orally
- Sublingual/transmucosal
- Epidural
- Transdermal
- Intra-articular
What opioids can be given orally?
- Morphine, codeine
What pharmacokinetic mechanism should you be aware about in regards to oral administration of opioids?
- Significant first pass hepatic metabolism of most opioids
Which opioid can be given sublingual/transmucosal?
- Buprenoprhine
How can opioids be given as an epidural?
- Combine morphine with local anesthetic (commonly lidocaine or bupivicaine) for an epidural
(note: we do more local/regional blocks as opposed to epidurals)
Why might you consider doing an epidural?
- Duration of effect - 12-24 hours!
- Lower dose - decreased sedation/other side effects
What are 3 potential side effects of epidural opioids?
- Urinary retention
- Pruritis (?)
- Delayed respiratory depression (?)
What are the supraspinal effects of alpha 2 adrenergic agonists?
- Sedation
- Analgesia
- Muscle relaxation
Describe the mechanism of action of alpha 2 adrenergic agonists
- Modulate descending noradrenergic pathways
- Inhibit pain transmission in dorsal horn of spinal cord
- Interrupt nerve transmission (?)
Alpha 2 adrenergic agonists are commonly used in large or small animals? Why?
- Large animals
- Well known efficacy and potentially lesser side effects
How are alpha 2 adrenergic agonists utilized in small animal patients? What side effects should you watch for?
- At lower doses
- Cardiovascular side effects
What clinical effect do alpha 2 adrenergic agonists have?
- Moderate-marked sedation and analgesia
What route of administration can alpha 2 adrenergic agonists be given?
- Systemic and epidural
Name 4 drugs that are NMDA receptor antagonists
- Ketamine
- Tiletamine
- Amantadine
- Methadone
What is the clinical use for NMDA receptor antagonists?
- Chronic pain
- Pain associated with wind up/central sensitization
- As a component of pre-emptive analgesia
- As a component of multimodal analgesia
Where are NMDA receptors found?
- Centrally AND peripherally
NMDA receptors in the brain are involved in what?
- Learning, memory, behavior, motor coordination
- Wind up, central sensitization, neuronal plasticity, neuronal degeneration
NMDA receptors in the spinal cord are involved in what?
- Wind up, central sensitization, neuronal plasticity, neuronal degeneration (?)
Overall, NMDA receptors play an important role in what kind of pain states?
- Chronic pain states
What does local anesthesia result in?
- Temporary loss of sensation to a region of the body W/O loss of consciousness
How are local anesthetics administered? How do they work?
- Administer the drug in region of peripheral nerve you would like the block
- Blocks nerve conduction by blocking neuronal sodium channels
- This prevents transmission of nociceptive information
True or False: You should always consider the use of a local anesthetic technique
- True
How does COX activity change in response to inflammation?
- Increases
- Part of the inflammatory response to tissue injury
How does COX activity contribute to pain and inflammation?
- Produces prostanoids (prostaglangings, prostacyclin, thromboxanes)
- Potent mediators of inflammation and amplifiers of nociception (produces hyperalgesia)
How does NSAIDs work?
- By inhibiting cyclooxygenase enzymes
- This decreases inflammation, improves mobility and QOL
What factors should you consider when selecting an NSAID for pain management?
- Clinical experience/comfort
- Safety/efficacy
- Pharmacology of the drug
- Convenience (route and frequency)
- Price
Why may NSAID usage and anesthetic induced hypotension result in adverse renal effects?
- Renal hypoperfusion and nephrotoxicity due to certain NSAIDs
What should you be concerned about in regards to using NSAIDs during a surgical procedure?
- Potential increase in bleeding tendencies
- More attention during procedures associated with areas of non-compressible hemorrhage (i.e. spinal lesions, hepatic biopsies, dobermans)
Are preemptive NSAIDs an appropriate method of pain management?
- Clinician dependent
What should you consider before prescribing NSAIDs to a patient?
- Hydration status
- Age
- Concurrent medications (ex. steroids)
- Procedure
- Co existing diseases
- Cost/benefit ratio
Does movement during an anesthetic procedure mean that the patient is awake? Why or why not?
- No
- Not all movement during general anesthesia is the same
- Purposeful movement indicates that the patient is awake
- Reflexive movement is not a conscious movement
If it is necessary to run iso over ______% and sevo over ________% you need to consider better analgesic options
- Iso > 2%
- Sevo > 2.5%
What happens if you routinely administer high levels of inhalant anesthetic without considering nociception and pain?
-
What complications may you run into during the pre-med phase of anesthesia?
- Having the correct drug
- Errors in drawing up the drugs
- Mislabeling
- Not reading the label
- Wrong dose (decimals, kgs vs lbs)
- Incompatible drugs
- Drug efficacy issues
What could go wrong in regards to drug efficacy issues?
- Although anesthetic drugs tend to work as expected, they can vary a great deal unexpectedly
(ex. apnea, excitement, muscle rigidity, fasciculations, little to no effect, etc)
What issues/complications might you run into during the induction phase?
- Drug administration (perivascular instead of IV, too fast or slow, wrong drug or amount, unexpected response)
- Apnea
- Excitement
- Intubation (impaired visualization, secretions, regurgitated material, etc)
How does off the needle induction compare to IV induction?
- Does not compare :(
What should you do to try and mitigate complications during intubation?
- Be prepapred!
- Stylets, suction, swabs, capnography, endoscopy, tracheostomy kit, topical lidocaine
In what species is laryngospasm more of an issue?
- Cats, pigs, sheep, goat

What should do to avoid laryngospasm during intubation?
- Topical lidocaine!
- Wait and give the drug time to work after spraying (15-30 seconds)
Aside from laryngospasm, what other complications might you run into when trying to intubate a patient?
- Laryngeal hemiplegia
- Regurgitation
What are the different ways that you can diagnose accidental esophageal intubation? What is the gold standard way to make sure that your ET tube is in trachea?
- Can you visualize the tube between the arytenoid cartilages?
- Can you seal the airway (cuff inflation)?
- Is the patient staying asleep?
- Problems with hypoxia?
- Is the stomach dilating?
- Does the reservoir bag move synchronously with ventilation efforts?
- Gold standard = normal capnograph
An overinflated ET cuff can lead to what 2 things?
- Tracheal injury
- Tracheal rupture (Cats)

In cats, if you need to inflate a cuff with more than 2-3 mLs, what should you do?
- Get a bigger tube
If you intubate a patient with an ET tube that is too long, what might occur?
- ET tube will be pushed against the wall
- May end up with one lung intubation
- Most common in pigs
What feature of certain ET tubes helps to prevent blocked airflow in the case that the tube is pushed up against a wall?
- Murphy eye

What happens if you fill a sevoflurane vaporizer with isoflurane?
- You will be accidentally administering a higher amount of inhalant anesthesia
- Isoflurane has a much higher vapor pressure
- Ex. If you have the sevoflurane vaporizer set to 3%, 4.5% isoflurane will be administered to the patient
What happens if you fill an isoflurane vaporizer with sevoflurane?
- You will be accidentally administering a lower amount of inhalant anesthesia
- Ex. If you have the isoflurane vaporizer set to 3%, 1.8% sevoflurane will flow out
What color is associated with isoflurane?
- Purple
What color is associated with sevoflurane?
- Yellow
What is the 'lock out' mechanism?
- If you cannot get the vaporizer to open, there may be a 'lock out' and you may have to turn a knob to release it
If an anesthetic machine falls on its side, is it okay to pick it up and continue to use it?
- No - they have a wick to calibrate flow and this will become over saturated if the machine falls over
- Your machine will not work properly
What is the maximum number (in mmH2O ) on the manometer that should be reached? What is the exception?
- 20 mmHg
- Except in horses
What will occur if a pop-off valve remains closed?
- Increase intrathoracic pressure
- Collapse of caudal and cranial vena cava
- Cardiovascular collapse
- Death
When is the only time you should really have the pop-off valve closed?
- For leak checking
What are some other issues you may run into in regards to 'machine mishaps'?
- Oxygen is not on
- Vaporizer is not on
- Gas in the tank?
- Compressed gas cylinders
What is the second most common anesthetic complication?
- Hypotension

What are the systolic and MAP values for defining hypotension?
- Systolic < 90 mmHg
- MAP < 70 mmHg
What is the equation for blood pressure? BP = ....
- BP = CO x SV
What is the equation for cardiac output? CO = ....
- CO = SV x HR
What are the 4 steps to addressing hypotension under anesthesia?
- Assess anesthetic depth and reduce inhalant dose if possible
- Normalize heart rate and rhythm
- Fluid bolus
- Inotropes/vasopressors
To effectively recognize bradycardia, what must you first do?
- Get a baseline HR for comparison
In general, at what bpm are the following species considered bradycardic?
- Horses
- Large breed dogs
- Toy breed dogs
- Cats
- Ruminants
- Horses: < 25 bpm
- Large Breed dogs: < 60 bpm
- Toy breed dogs: < 90 bpm
- Cats: < 100 bpm
- Ruminants: < 80 bpm