CH. 22 - Respiratory System (Part 3)
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Systemic Gas Exchange
The unloading of O2 and loading of CO2 at the systemic capillaries
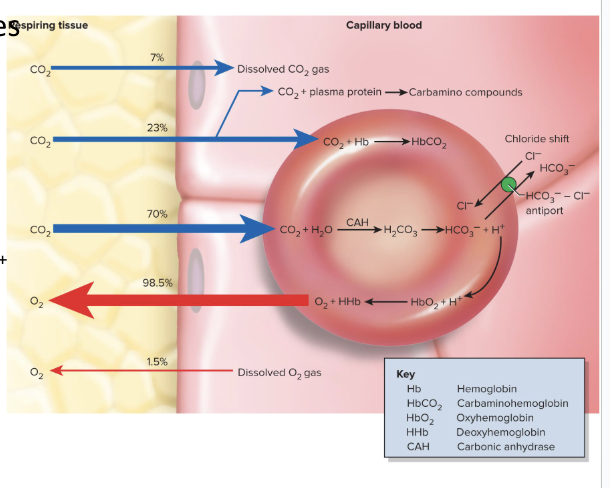
CO2 Loading in Systemic Gas Exchange
CO2 diffuses into the blood
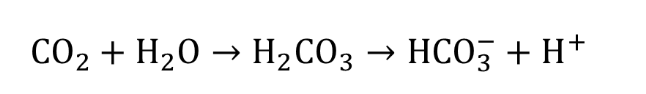
Carbonic anydrase in RBC catalyzes CO2 + H2O → H2CO3 → HCO3- + H+
Chloride shift happens
We put a bicarbonate ion into the plasma and put a Cl- ion into the rbc
Keeps reaction proceeding
H+ binds to hemoglobin
Oxygen Unloading in Systemic Gas Exchange:
As H+ ions bind to hemoglobin, we get less affinity for O2
as we lose O2, we are more likely to lose more O2 from that hemoglobin
hemoglobin arrives at the capillaries 97% saturated with O2, and leaves 75% saturated
difference is caused by the utilization coefficient:
we typically lose 22% of O2 in the capillaries
Venous reserve:
the O2 remaining in the blood after it passes through capillary beds
How do the reactions in the lungs for gas exchange compare to the reactions in systemic gas exchange?
Reactions that occur in the lungs are reverse of systemic gas exchange
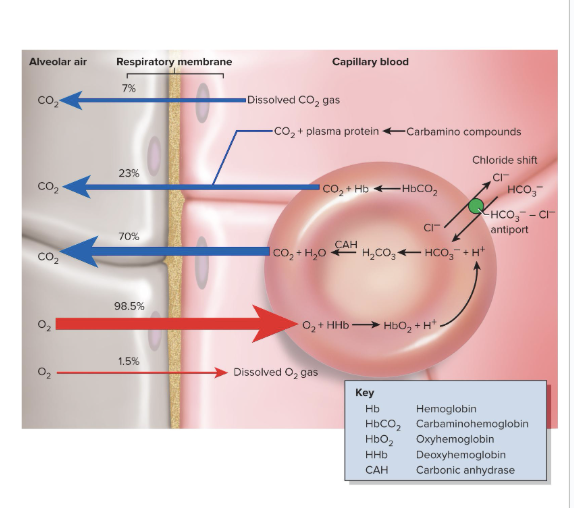
CO2 Unloading in Alveolar Gas Exchange
As hemoglobin loads O2 from the alveoli, its affinity for H+ decreases
Reverse chloride shift happens
bicarbonate diffuses back into the RBC in exchange for Cl-
H+ dissociates from hemoglobin and binds with bicarbonate in the RBC
carbonic anhydrase turns carbonic acid into CO2 and water
the CO2 diffuses into the alveoli to be exhaled
Hemoglobin unloads O2 to. . .
match the metabolic needs of different states of activity of the tissues
4 factors that adjust the rate of oxygen unloading to match metabolic need:
Ambient PO2
Ambient pH (Bohr effect)
Temperature
Biphosphoglycerate (BPG)
How ambient PO2 adjusts the rate of oxygen unloading:
active tissue has lower PO2
the lower the ambient partial pressure of oxygen, the more likely we are to release O2
How ambient pH adjusts the rate of oxygen unloading:
active tissue has higher levels of CO2
the more CO2 in blood, the more H ions, making pH lower and more acidic
the lower the blood pH, the more we unload O2
How temperature adjusts the rate of oxygen unloading:
Active tissue has a higher temperature
as body temp goes up, rate of unloading O2 goes up
as body temp goes down, the rate of O2 unloading goes down
How bisphosphoglycerate (BPG) adjusts the rate of oxygen unloading:
Erythrocytes produce BPG
can bind to hemoglobin
as it binds, it causes O2 to be unloaded
causes hemoglobin to change shape so it unloads O2
we get more BPG with increases in body temp, thyroxine, growth hormone, testosterone, and epinephrine
What are the set points for arterial blood pH, PCO2, and PO2?
pH: 7.35-7.45
PCO2: 40 mmHg
PO2: 95 mmHg
How do we maintain and monitor these arterial blood levels?
These arterial blood levels are maintained by adjustments to the rate and depth of breathing
to monitor these factors, we have chemoreceptors in the PNS and CNS that monitor chemistry of the blood and CSF
blood pH influences breathing/respiratory rhythm the most
least important is blood oxygen levels
What produces the respiratory response to pH changes?
Central Chemoreceptors
produce 75% of the change in respiration caused from the pH shift
CO2 crosses the BBB and reacts with water in the cerebrospinal fluid to produce carbonic acid
the H+ ions from carbonic acid strongly stimulates the chemoreceptors
Peripheral Chemoreceptors
produces 25% of the change in respiration in response to pH changes
H+ ions also stimulate these chemoreceptors
Acidosis Vs. Alkalosis
Acidosis: blood pH lower than 7.35
Alkalosis: blood pH higher than 7.45
Hypocapnia Vs. Hypercapnia
Hypocapnia: the pressure of CO2 is less than 37 mmHg
Most common cause of alkalosis
Hypercapnia: the pressure of CO2 is greater than 43 mmHg
most common cause of acidosis
Normal pressure of CO2: 37-43 mmHg
Respiratory Acidosis and Alkalosis
pH imbalances resulting from a mismatch between the rate of pulmonary ventilation and the rate of CO2 production
breathing in and out too much or too little relative to CO2 production
What is a corrective homeostatic response to acidosis?
hyperventilation
blowing off CO2 faster than the body can produce it
Pushes the CO2 reaction to the left
reduces H+ ions, raising pH back to normal
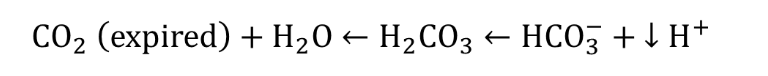
What is a corrective homeostatic response to alkalosis?
Hypoventilation
allows CO2 to accumulate in body fluids faster than we can exhale it
Shifts the CO2 reaction to the right
Raises number of H+ ions, lowering the pH back to normal
Ketoacidosis
Acidosis brought about by burning fat very quickly, releasing acidic ketone bodies
a classic symptom of type 1 diabetes
causes Kussmaul Respiration
hyperventilating to partially compensate for the fact that our metabolism is putting too many ketone bodies in our blood stream
high ketone bodies makes sweet urine
Effects of CO2 on Breathing (Direct and Indirect)
Direct:
increase of CO2 at the beginning of exercise can directly stimulate peripheral chemoreceptors and trigger an increase in ventilation faster than central chemoreceptors
Indirect:
through pH shifts
PO2 has ___ effect on respiration
little
Chronic Hypoxemia
chronically low O2
PO2 is less than 60 mmHg, which can significantly stimulate ventilation
Causes hypoxic drive:
respiration driven more by low O2
Can be triggered by emphysema, pneumonia, and high elevations
Causes of Increased Respiration During Exercise:
When the brain sends motor commands to the muscles, it also sends this information to the respiratory centers
these centers will increase ventilation in anticipation of the needs of the muscles
exercise stimulates propioreceptors of muscles and joints
they increase breathing when informed that muscles are moving
the increase in breathing keeps blood gas values at normal levels
Senescence of the Respiratory System
Declining pulmonary ventilation
Costal cartilages become less flexible
Lungs have less elastic tissue and fewer alveoli
Elderly are less able to clear lungs of irritants or pathogens
More susceptible to respiratory infection
their mucociliary escalator slows down, leading to pneumonia
pneumonia causes more deaths than any other infectious disease
Chronic obstructive pulmonary diseases
Emphysema and chronic bronchitis more common
Takes a lifetime of degenerative change for these diseases to happen
Contribute to hypoxemia and hypoxic degeneration of other organ systems
Hypoxia
oxygen deficiency in a tissue, or the inability to use oxygen
if not enough gas exchange, we get low blood O2, causing low tissue O2
cyanosis is a sign of hypoxia
Hypoxemic Hypoxia
state of low arterial PO2
usually due to inadequate pulmonary gas exchange
can also be due to oxygen deficiency at high elevations or impaired ventilation
drowning, aspiration, respiratory arrest, degenerative lung diseases
Ischemic Hypoxia
inadequate circulation of blood
not enough blood flow through the lungs
often caused by congestive heart failure and blockages of vessels
Anemic Hypoxia
due to anemia, resulting from the inability of the blood to carry adequate oxygen
Histotoxic Hypoxia
metabolic poisons such as cyanide prevent tissues from using oxygen
causes cyanosis
Oxygen Toxicity
develops when pure O2 is breathed at 2 ATM or higher for a short time
this generates free radicals and H2O2 (peroxide)
destroys enzymes
damages nervous tissue
Hyperbaric Oxygen
Formerly used to treat premature infants
were put in a chamber with elevated O2
it caused more harm than good, so it is not used anymore
Chronic obstructive pulmonary disease (COPD)
long-term obstruction of airflow and substantial reduction in pulmonary ventilation
Major COPDs are chronic bronchitis and emphysema
Almost always associated with smoking
Other risk factors: air pollution, occupational exposure to airborne irritants, hereditary defects
COPD reduces vital capacity
COPD causes: hypoxemia, hypercapnia, and respiratory acidosis
Hypoxemia stimulates erythropoietin release from kidneys, and leads to polycythemia
Chronic Bronchitis
Severe inflammation of the lower respiratory tract
Goblet cells enlarge and produce excess mucus
Immobilized cilia fail to remove mucus
Thick, stagnant mucus forms, which is ideal for bacterial growth
Smoke compromises alveolar macrophage function
Develop a chronic cough to bring up sputum (thick mucus and cellular debris)
Chronic bronchitis almost always lead to pneumonia
Symptoms include hypoxemia and cyanosis
Emphysema
Alveolar walls break down and merge together
Lung has fewer and larger spaces
Much less respiratory membrane for gas exchange
Lungs become fibrotic and less elastic
Lungs become flabby and form cavities with large spaces
Air passages collapse
Obstructs outflow of air
Air trapped in lungs, causing person becomes to be barrel-chested
Weakens thoracic muscles
Spend three to four times the amount of energy just to breathe
Cor Pulmonale
thickening of the right ventricle of the heart
happens when the blood entering the heart is more than the blood exiting due to an obstruction
Lung Cancer
Accounts for more deaths than any other form of cancer
Most important cause is smoking (at least 60 carcinogens)
Both tobacco and marijuana have these carcinogens and cause lung cancer
Squamous-Cell Carcinoma
Most common form of lung cancer
Begins with the transformation of the bronchial epithelium into stratified squamous from ciliated pseudostratified epithelium
Dividing cells invade the bronchial wall, cause bleeding lesions
Dense swirls of keratin replace the respiratory tissue
Adenocarcinoma
Originates in mucous glands of lamina propria of the lungs
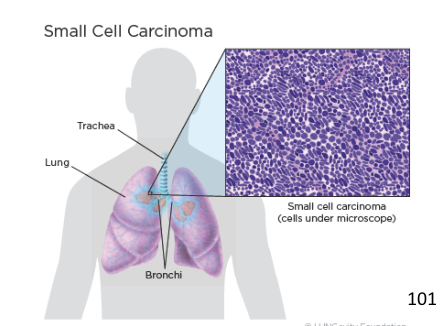
Small-Cell (oat cell) Carcinoma
Least common, most dangerous
Named for clusters of cells that resemble oat grains
Originates in primary bronchi, then invades the mediastinum, and metastasizes quickly to other organs