chapter 13, Antimicrobials and Resistance
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
alexander flemings findings (1928)
there were zones of inhibitions around mold, and staph aureus did not grow. the mold juice was antibiotics
where do antibiotics come from (2)
in the wild: antibiotics produced by some bacteria and fungi
Though something has antibiotic properties it doesn't mean we call that material an antibiotic (tree bark)
in the lab: man- made derivatives of natural compounds
Synthetic cmps need to be approved to be used.
how do antibiotics work?
Antibiotics inhibit bacterial growth/ reproduction or survival
Can prevent growth without killing the cell
Either inhibit growth (accessory) or inhibit survival (required)
ex//
DNA gyrase is accessory
Cell wall synthesis is necessary
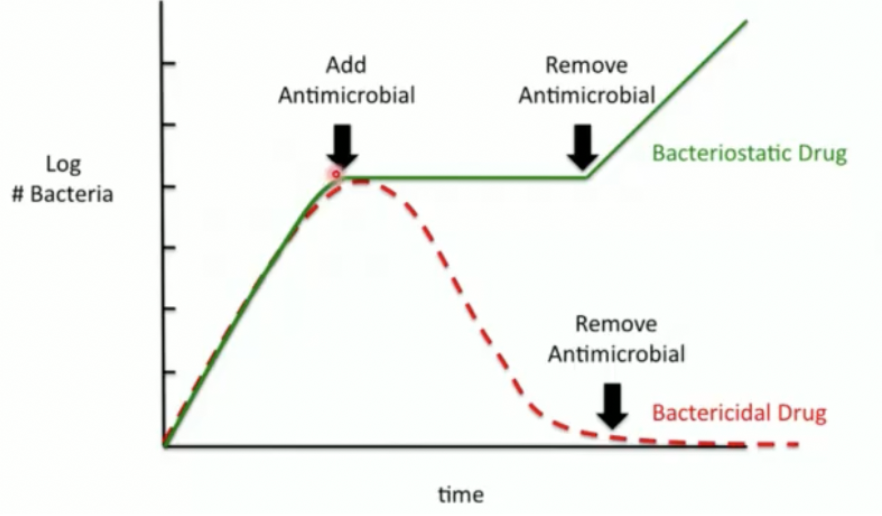
bacteriostatic
describing action of antibiotics.
prevent bacterial growth/ reproduction, but DOESNT KILL BACTERIA
ex// blocking protein synthesis, inhibiting DNA replication
Added antimicrobial, bacteria doesnt change
Removed antimicrobial, bacteria continues growing
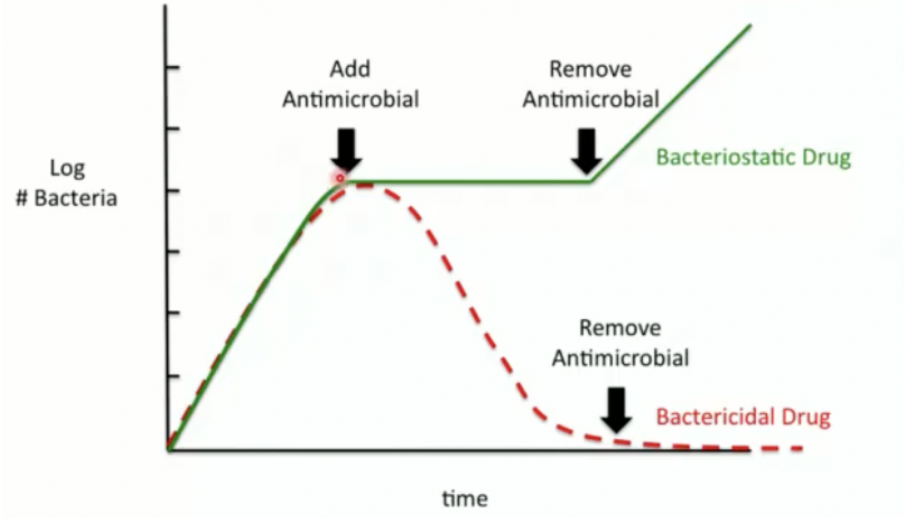
bactericidal
describing action of antibiotics
antibiotics KILLS BACTERIA
ex// destroying cell walls, disrupting membranes
Added antimicrobial, kills bacteria
Removed antimicrobial, bacteria is still dead
antibiotic resistance
if a microbe gains ability to resist effects of an antibiotic
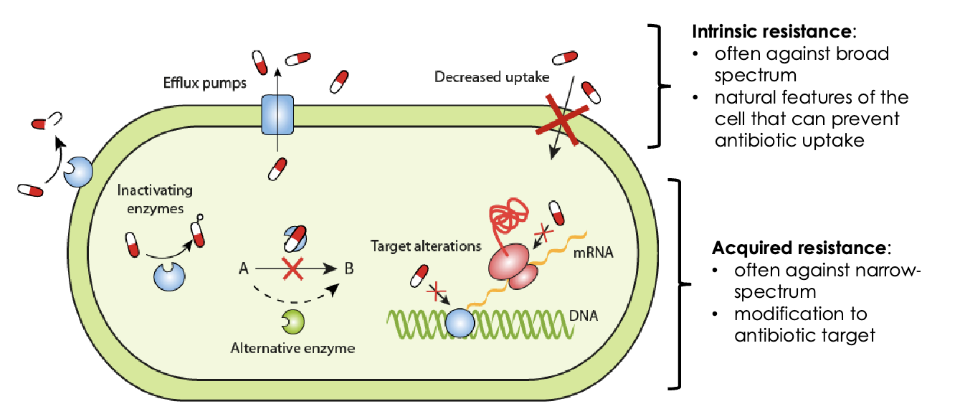
types of (antibiotic) resistance (2)
intrinsic resistance
acquired resistance
intrinsic resistance (peniciliin ex// w gram -ve +ve)
Some bacteria are naturally resistant to antibiotics
Don't need to evolve to resist the activity of an antibiotic
ex// gram -ve bacteria are more resistant to penicilin than gram +ve bacteria
Penicillin targets peptidoglycan
gram +ve bacteria PG are more exposed than gram -ve
gram -ve bacteria have an outer membrane barrier & thin PG layer
Decrease uptake, increased efflux
Broad range, not specific to one type of antibiotic (targets outer layer of cell)
Works against have activity across a range of species
Gram -ve and +ve
Antimicrobials that attack intracellularly are more specific than the ones that attack peptidoglycan. PG is more conserved across all species whereas intracellularly there can be different things inside
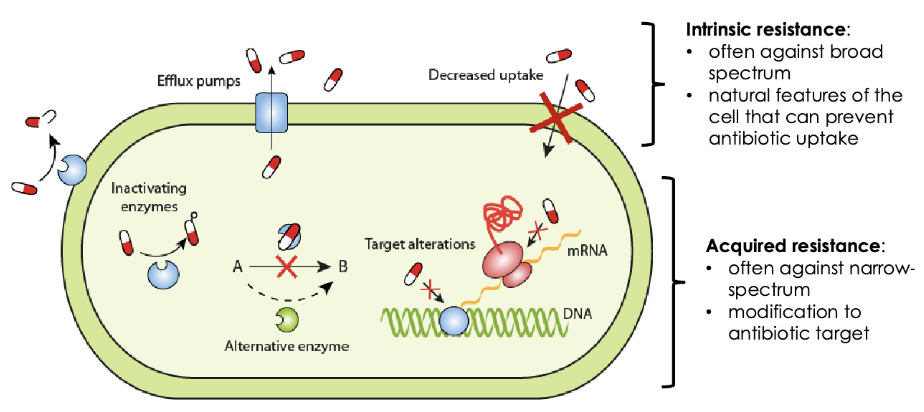
acquired resistance
Some bacteria become resistant through mutation/evolution and natural selection for features that are less susceptible to antibiotics
Happens over generations
ex// Antibiotic erythromycin targets the ribosome → inhibits protein synthesis
Bacterial ribosome evolves over 1000s of years so that erythromycin can no longer bind to the ribosome
Bacteria become resistant to antibiotic
Mutation for something more targeted (narrow spectrum of activity)
Target alterations, inactivating enzymes from inside the cell
Gram -ve or +ve
Antimicrobials that attack intracellularly are more specific than the ones that attack peptidoglycan. PG is more conserved across all species whereas intracellularly there can be different things inside
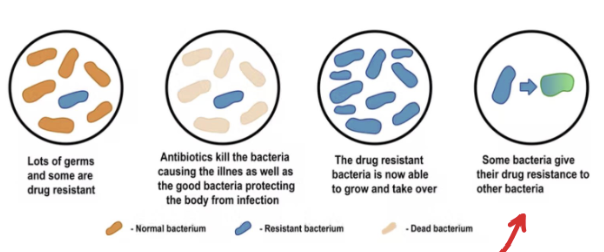
how do bacteria become drug resistant?
population has some bacteria that are drug resistant
Antibiotics added, the non-resistant bacteria is knocked out
The niche at the infection is colonized by the drug resistant bacteria and is taken over. Selecting microbes. Speeding up natural selection
where does resistance come from
mutation —> evolution
Change target of the antibiotic in bacteria
Alter metabolic pathways
Change in membrane permeability
ex//
change enzyme in cell to catalyze better
modifying protein for DNA binding protein (transcription)
changing membrane permeability: (stop expressing transporter proteins and start producing efflux pumps that pump antimicrobials outside of the cell)
express inactivating enzymes that are embedded in the structures in the cell wall
ways of testing antibiotic sensitivity (2)
disk diffusion assay
minimum inhibitory concentration (MIC)
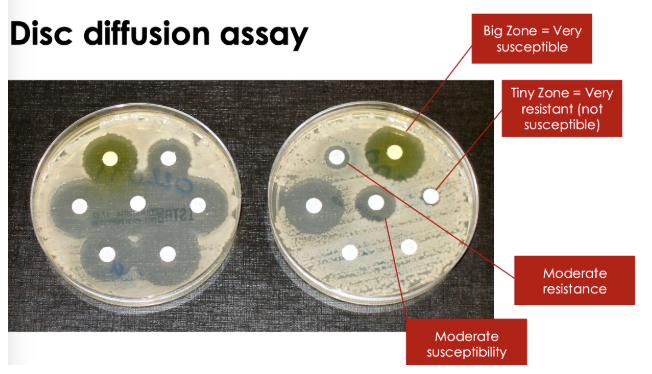
disc diffustion assay
Plate-based assay to test for antibiotic susceptibility
Steps:
Take isolated pathogen from patient
Grow pathogen in pure culture after 48h
Inoculate agar plate with bacteria
Spread bacteria around evenly
Place disc impregnated with known concentration of antibiotic you are testing onto agar (each number is a different antibiotic)
Antibiotics diffuse into agar, preventing growth of susceptible bacteria. This is incubated for 24-48h
Measure zone of inhibition: the area around the antibiotic disc in which bacteria cannot grow. Observe how well antibiotic inhibited growth. measure in cm or mm
Bigger zone of inhibition, better antibiotic, more susceptible to antibiotic
No zone, microbe is completely resistant to that antibiotic
Closer bacteria can get to disk, more resistant the bacteria is to that antibiotic. If a bacterium cannot get close to the disk, then the antibiotic kills/hurts that bacterium that means the bacterium is susceptible to that antibiotic
Resistant: smaller than threshold (smaller disk)
Susceptible: higher than threshold (bigger disk)
minimum inhibitory concentration (MIC)
Liquid medium-based assay to test for antibiotic susceptibility. In lab
Steps:
1. Dispense antibiotics, in gradient, into 96 well plate
• Each row = different antibiotic
• Each column = different Concentration
One side is only bacterial growth medium
One side is only growth control, 0 antimicrobial
All rows should have bacterial growth
Lowest conc that inhibited bacterial growth is the minimal inhibitory concentration MIC
Liquid assay to test for antibiotic
susceptibility
Steps:
2. Inoculate each well with same volume of bacterial culture
3. Incubate plate to allow bacteria to grow
4. MIC is lowest concentration of antibiotic where you see NO bacterial growth
lower MIC= more susceptible, weaker resistance
higher MIC= more resistant (stronger resistance)