3.2 Coughing in Horses 1
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
URT disease: clinical signs
fever, nasal discharge, coughing, enlarged submandibular lymph nodes
LRT disease: clinical signs
+/- fever, +/- nasal discharge, coughing, mucoid tracheal secretion, poor performance, may be subclinical
URT & LRT: equine influenza virus
2-3 year old racehorses
H3N8 and (H7N7)
reservoir between epizootics unknown
world-wide occurrence
antigenic drift
most common cause of URTI
spread by aerosol & direct contact
vaccinated animals susceptible after 2-3 months
partial immunity may suppress clinical signs but allow virus shedding
equine influenza: pathogenesis
-inhalation
-incubation 1-3 days
-infects epithelial cells of upper & lower airways
-loss of ciliated epithelium, compromise of mucociliary mechanism
-URT +/- LRT signs
-may be associated with secondary bacterial infection
-no viremia
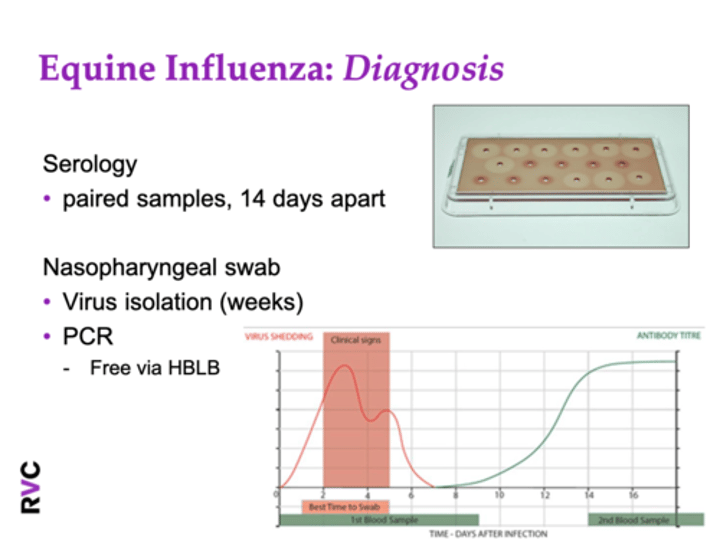
equine influenza: diagnosis
serology
-paired samples, 14 days apart (antibody titer)
nasopharyngeal swab
-virus isolation (weeks)
-PCR (free via HBLB)
equine influenza: treatment
-isolate
-symptomatic & supportive
-limit stress
-hydration
-NSAIDs to limit pyrexia & improve appetite
-rest
-specific anti-viral therapy (acyclovir, interferon)
-monitor for secondary infection
equine influenza: vaccination
-present-day threat from H3N8 equi-2 Florida strains, divided into clades 1 & 2
-vaccines effective against H7N7 & some H3N8 strains (10-20 years out of date)
-2003 advised vaccines changed to include Florida clade 1 strain
-2010 advised to include Florida clade 2 strain
-2014 & 2019 recommendations unchanged
-significant effect of adjuvant, cross protection
-start course >6m due to maternal antibodies
equine influenza vaccination: jockey club rules
1st vaccination
2nd vaccination 21-60 days after 1st vaccination
3rd vaccination 120-280 days after 2nd vaccination
thereafter every 6 months
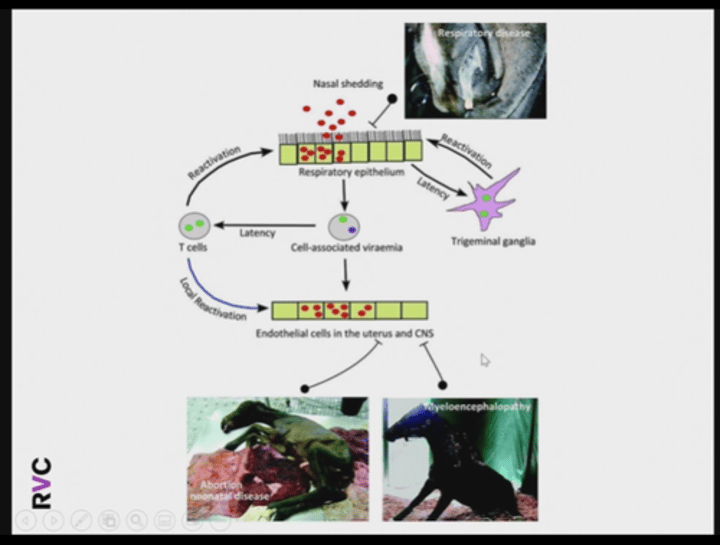
URT & LRT: equine herpes virus 1 & 4
-endemic in UK & worldwide
-75% of horses have latent infection acting as reservoir
-stress may activate latent infection-> transport, other illness, influenza, vaccinations
EHV 1 & 4: epidemiology
site of latency: bronchial LN, submandibular LN, trigeminal ganglia
EHV2 may be involved in reactivation
first exposure as foals & weanlings: infected from lactating mares, foal to foal spread
immunity short lived (3-5 months)
reinfected during breeding or racing careers: respiratory secretions, fetus/placenta, fomites
reinfection causes mild or inapparent infection, except broodmare (abortion last trimester or neonatal disease)
also get neurologic disease (strain variation)
EHV 1 & 4: pathogenesis
EHV1 & EHV4: inhalation of virus, incubation 3-7 days, replicates in URT epithelium then disseminates to LRT
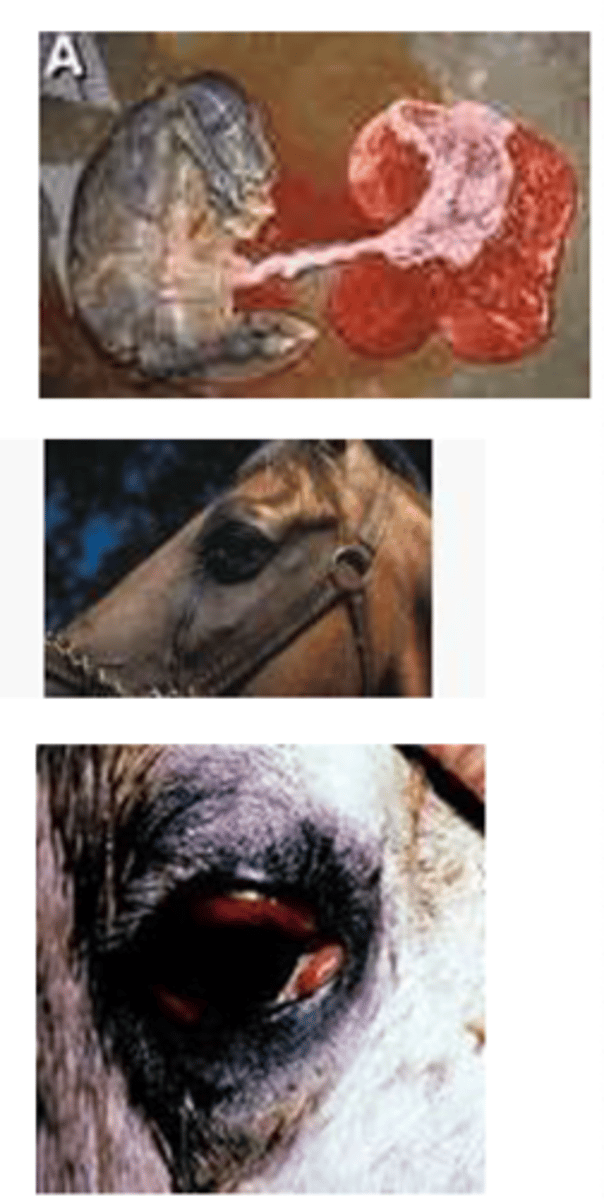
EHV1: transported to other organs in T lymphocytes, viremic for up to 3 weeks, vasculitis (neurological disease, abortion, chorioretinopathy) may be accompanied by secondary bacterial infection, may be subclinical
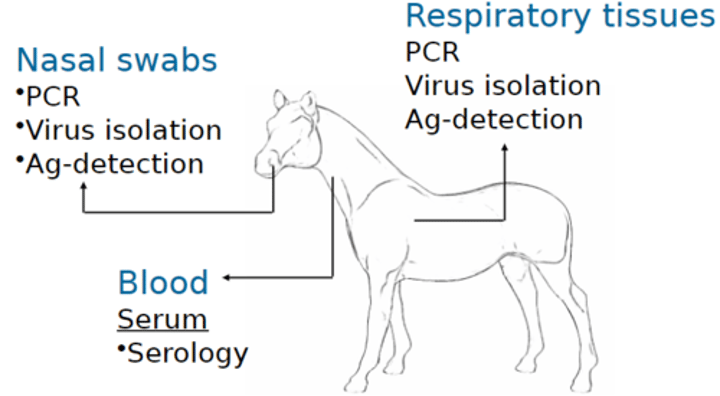
EHV 1 & 4: diagnosis & treatment
clinical signs
virus isolation
-blood-> 30 ml heparinized
-nasopharyngeal swab (+PCR)
serology
-paired samples
treatment same as equine influenza
EHV 1 & 4: vaccination
-can vaccinate from 4m
-natural immunity short-lived therefore unlikely to improve with vaccination
-reduce clinical disease, nasal shedding, & days of viremia, not complete protection
-two types-> inactivated, modified live
-two doses 4-6 weeks apart, booster every 6m
-pregnancy-> 5th, 7th, 9th month gestation inactivated vaccination
URT & LRT: equine viral arteritis
RNA arterivirus
notifiable
transmission by venereal infection of mares by stallions during mating, AI with semen from infectious stallions, contact with aborted fetuses & other products of parturition, direct contact in droplets (coughing/snorting)
stallions are chronic shedders
clinical disease in UK racing thoroughbreds not yet been reported
equine viral arteritis: pathogenesis
spread through respiratory, breeding, aborted fetus/placenta
incubation 3-14 days
variable pathogenicity of strains
macrophages-> LN-> leucocyte-associated viremia
localizes in endothelial cells (esp. smaller arterioles & epithelium of adrenals, seminiferous tubules, thyroid, & liver)
necrotizing arteritis-> edema & hemorrhage
equine viral arteritis: clinical signs
often no clinical signs
abortion & still birth (10-34 days following exposure, 3-10 months gestation)
fever, anorexia, edema (limb, prepuce, scrotum, ventral, periorbital), lacrimation, conjunctivitis, nasal discharge, coughing
equine viral arteritis: diagnosis & treatment
diagnosis:
blood samples, nasal swabs & semen can be used for isolation of virus or detection of viral RNA by PCR, serology
treatment:
symptomatic
equine viral arteritis: vaccination
vaccinate seronegative breeding stallions (pre-vaccination blood test)
modified live vaccine-> artevac
equine viral arteritis: HBLB code of practice
notifiable, stop all breeding, isolate & treat clinical cases, group in-contacts away from other horses on premises & obtain samples for virus isolation, screen all other horses in premises by serology, test semen from all stallions, clean & disinfect, repeat testing until freedom from active infection confirmed (declining antibody, no virus isolated), monitor semen positive stallions for persistence of shedding
URT & LRT: equine rhinitis virus
roles as pathogen controversial
can be isolated from asymptomatic horses as well
can induce experimental infection
young horses
60-80% have antibody titers by 5 years old
subclinical or mild URT & LRT signs
diagnosis-> virus isolation from NP swab or BALF, serology
treatment-> symptomatic
LRT bacterial infection
streptococcus zooepidemicus, streptococcus pneumoniae, pasteurella/actinobacillus most common, inhaled & overcome defense mechanisms, results in LRT only signs, may occur secondary to viral infection or non-infectious airway disease
LRT bacterial infection: identification
clinical signs/loss of performance
endoscopy & LRT samples (mucous, increased degenerate neutrophils & intracellular bacteria, C&S)
hematology (neutropenia/
neutrophilia, lymphopenia/
lymphocytosis, hyperfibrinogenemia/
increased SAA
LRT bacterial infection: treatment
antibiotics
rest
improve environment- dust free management
anti-pyretics
mucolytics
bronchodilators
non-infectious causes of coughing in adult horses
common: equine asthma (severe vs mild to moderate)
fairly common: aspiration pneumonia, pleuropneumonia, pulmonary abscesses, epiglottic entrapment, URT foreign body
uncommon: lungworm, tracheal stenosis/collapse, inhalation pneumonia, interstitial pneumonia, neoplasia, left heart failure
equine asthma: nomenclature
previously: COPD, "heaves", broken wind
RAO + summer pasture associated obstructive pulmonary disease + IAD
now: equine asthma syndrome, mild to moderate= IAD, severe= RAO or SPAOPD
mild-moderate equine asthma
young racehorses
20-65%, coincides with entering training, decreases with increasing age
also older national hunt, SB racehorses, & sports horses (no decrease with age)
excessive mucous in airways
cough and/or reduced performance
no increased respiratory rate/effort at rest
chronic signs (>4 weeks)
frequently subclinical
mild-moderate equine asthma: pathogenesis
implicated causes: inhaled dusts, LPS, ammonia
bacterial infection (inconclusive evidence)
viral infection (inconclusive evidence)
blood from EIPH (inflammation, secondary infection)
mild-moderate equine asthma: diagnosis & treatment
diagnosis: endoscopy (increased mucous), tracheal aspirate/BAL (increased mucous + neutrophils OR eosinophils/mast cells, culture bacteria?)
treatment: environment changes to reduce dust, antibiotics, interferon, corticosteroids (systemic or inhaled), bronchodilators (systemic or inhaled), sodium cromoglycate (mast cell stabilizer, preventative only), omega-3 polyunsaturated fatty acid supplementation
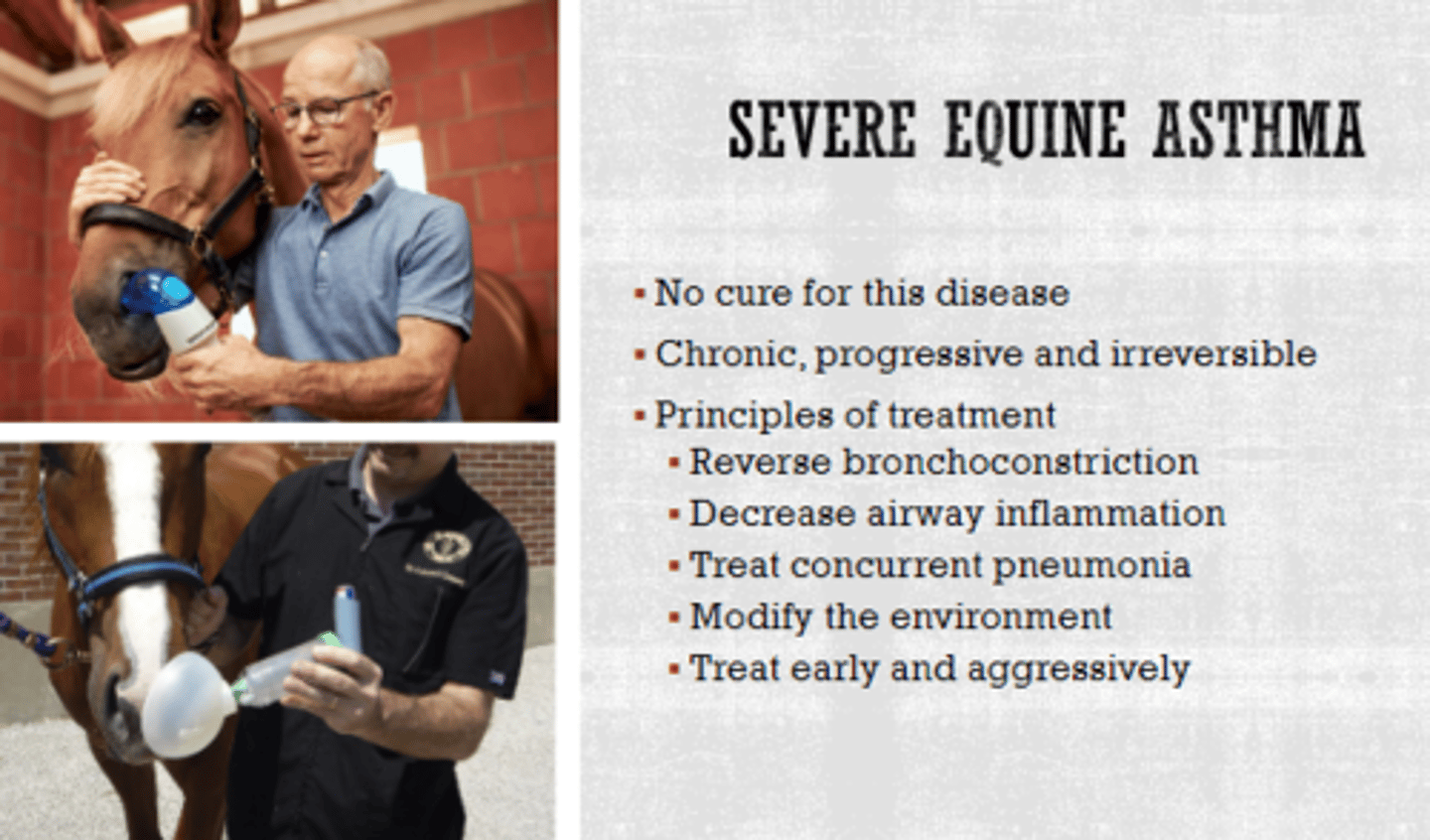
severe equine asthma
naturally occurring lower airway disease characterized by periods of reversible airway obstruction
neutrophil accumulation, mucous production, & bronchospasm
>7 years old
lifelong condition
genetic component to susceptibility
clinical signs may be seasonal
severe equine asthma: pathogenesis
spores & allergens deposit in bronchioles
immune reactions:
type 1 (mast cell degranulation), type 3 (immune-complex), type 4 (delayed)
bronchoconstriction, mucous production, airway inflammation
tissues are primed
can become hypersensitive
respond to non-specific allergens
severe equine asthma: clinical signs
acute & severe respiratory distress: increased respiratory effort, double expiratory effort/dyspnea
chronic: varies in severity from poor performance to overt signs of respiratory dysfunction with/without coughing & hypertrophy of abdominal muscles
severe equine asthma: diagnosis
determine likelihood of SEA
history & physical exam
assess airway inflammation (transtracheal wash, BAL)
rule out bacterial pneumonia
evaluate response to treatment
assess airway inflammation: endoscopy
-rule out pharyngeal disease
-airway inflammation->
hyperemia, corina blunting
-assess tracheal mucous
-obtain tracheal aspirate
-> cytology, culture
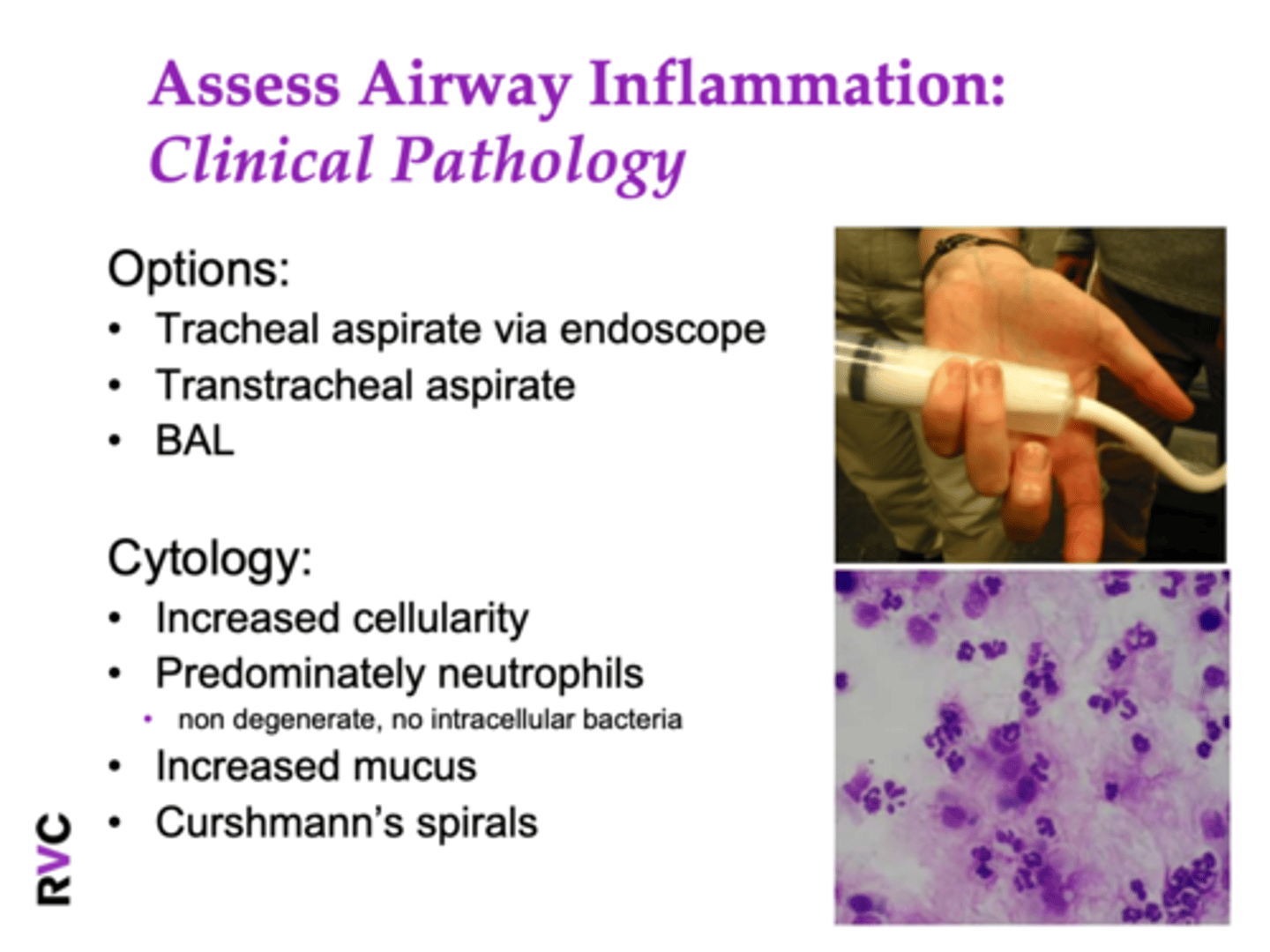
assess airway inflammation: clinical pathology
options: tracheal aspirate via endoscope, transtracheal wash, BAL
cytology: increased cellularity, predominately non-degenerate neutrophils, no intracellular bacteria, increased mucous, Curshmann's spirals
severe equine asthma: treatment
environmental management, reversal of bronchoconstriction, decrease pulmonary inflammation, decrease pulmonary mucous accumulation