ECG readings
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
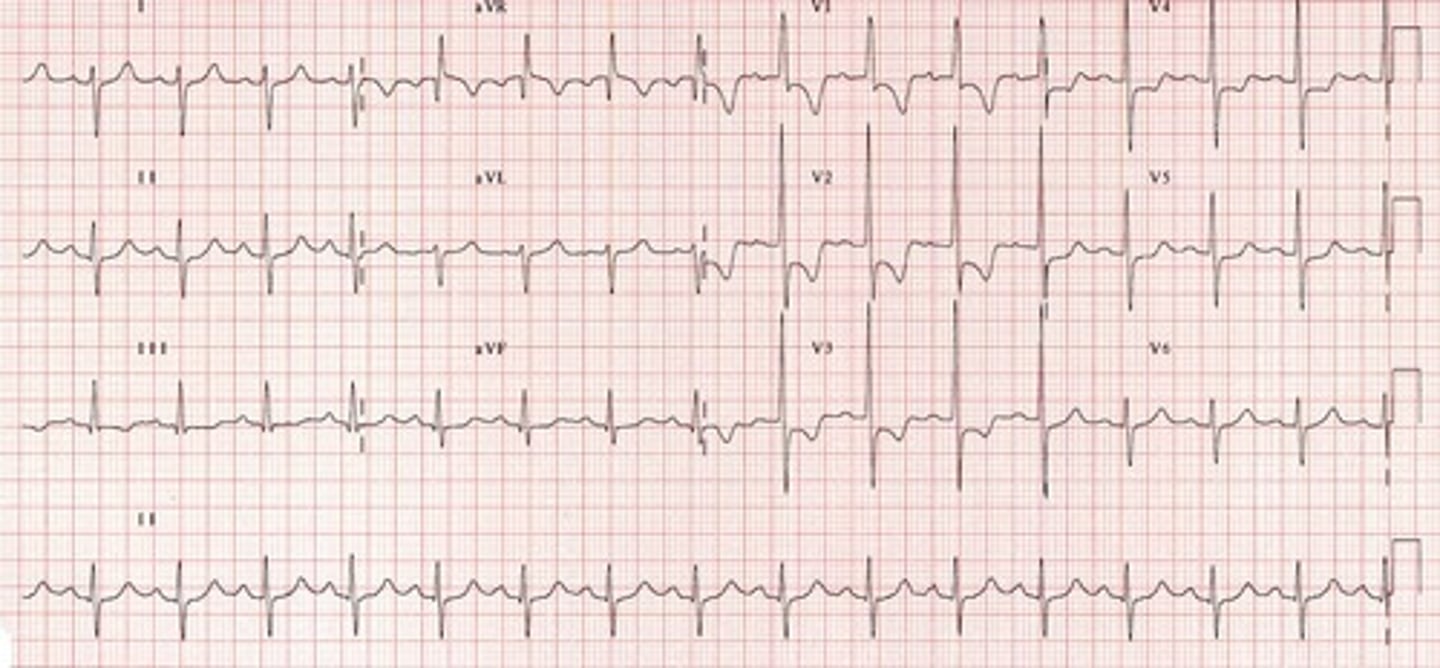
normal sinus rhythm
Originate: SA node
QRS complex: narrow
P wave: before QRS, same
Heart rate: 60-100 bpm
R-R intervals: regular

sinus bradycardia
Originate: SA node
QRS complex: narrow/wide
P wave: before QRS, same
Heart rate: <60 bpm
R-R intervals: regular

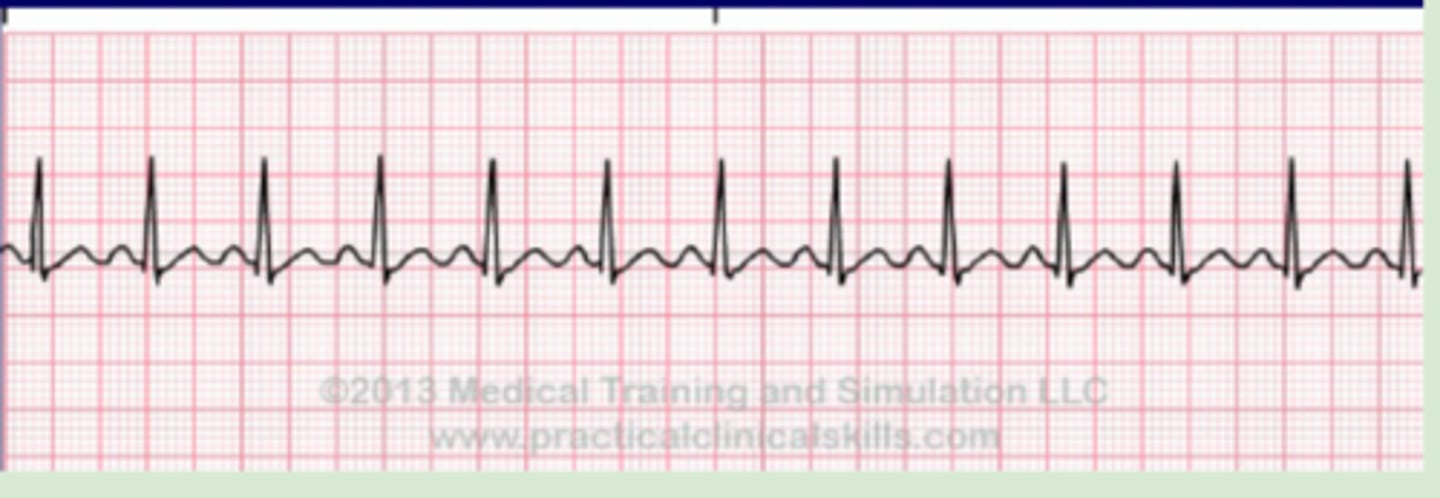
sinus tachycardia
Originate: SA node
QRS complex: narrow
P wave: before QRS, same
Heart rate: >100 bpm
R-R intervals: regular
sinus arrhythmia
Originate: SA node
QRS complex: narrow
P wave: same
Heart rate: 60-100 bpm
R-R intervals: irregular
wandering atrial pacemaker
Originate: AV node
QRS complex: narrow
P wave: at least 3 different waves
Heart rate: <100 bpm
R-R intervals: regular
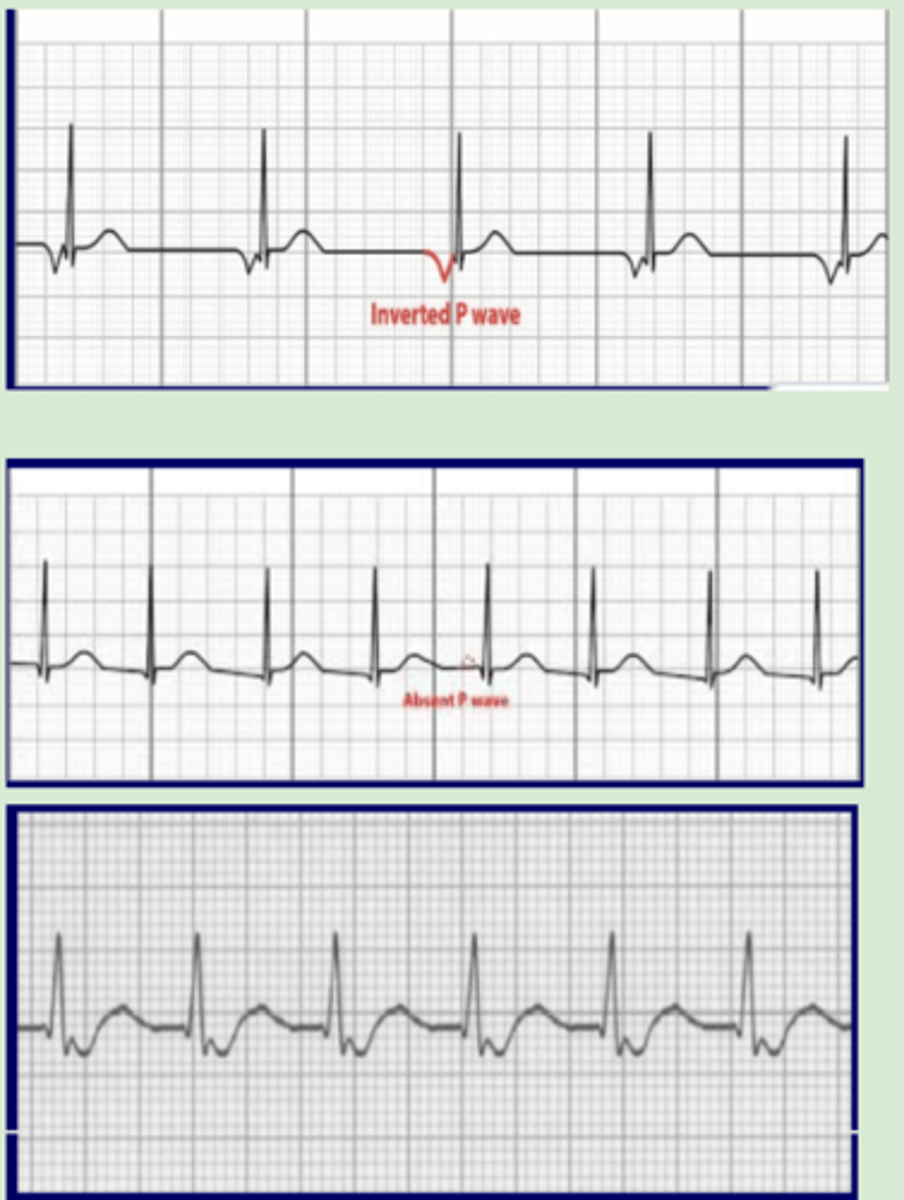
AV nodal junctional rhythm
Originate: AV node
QRS complex: narrow
P wave:
-Top of AV node = inverted, prior to QRS
-Middle of AV node = hidden in QRS
-Bottom of AV node = inverted, after QRS
Heart rate: 40-60 bpm
R-R intervals: regular
-Accelerated junctional rhythm: >60-100 bpm
-Junctional tachycardia: >100 bpm
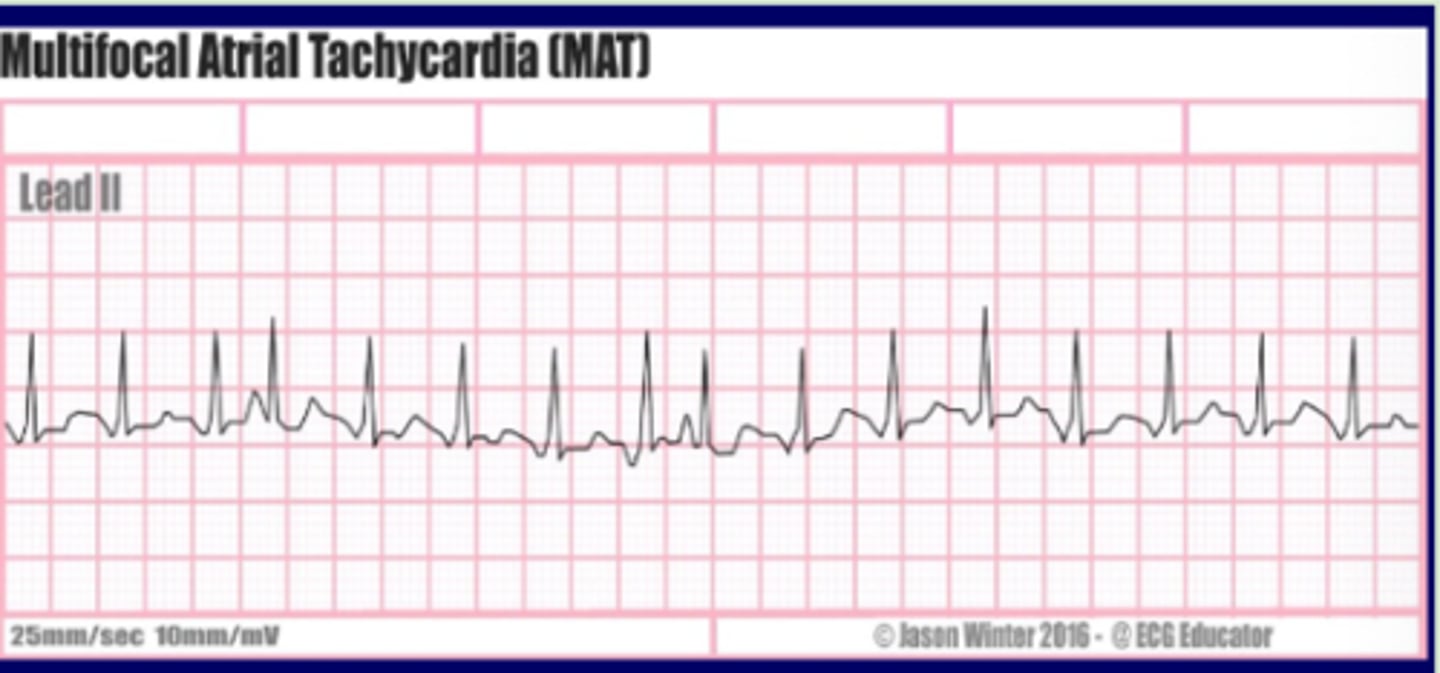
multifocal atrial tachycardia
Originate: multiple rapidly firing atrial impulses
QRS complex: narrow
P wave: different
Heart rate: >100 bpm
R-R intervals: irregularly irregular
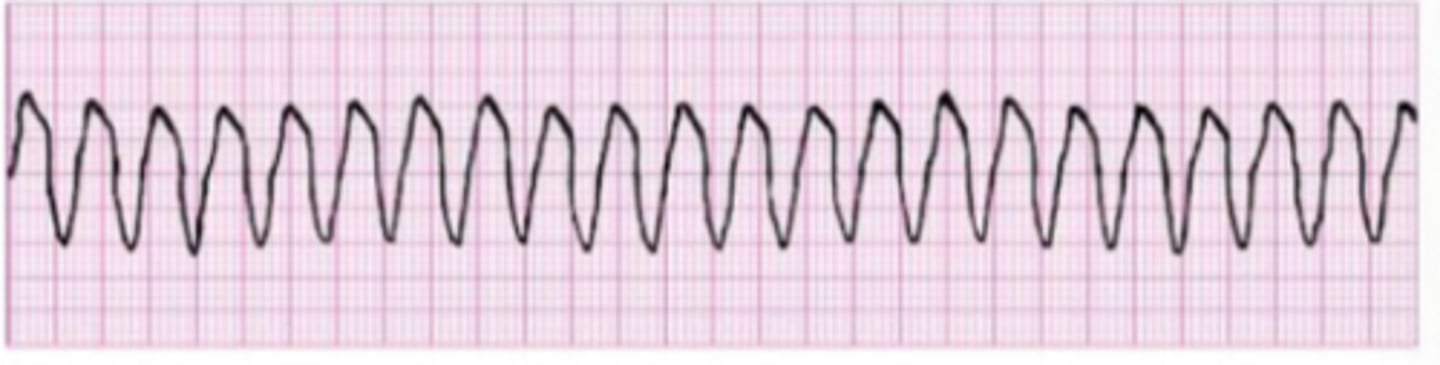
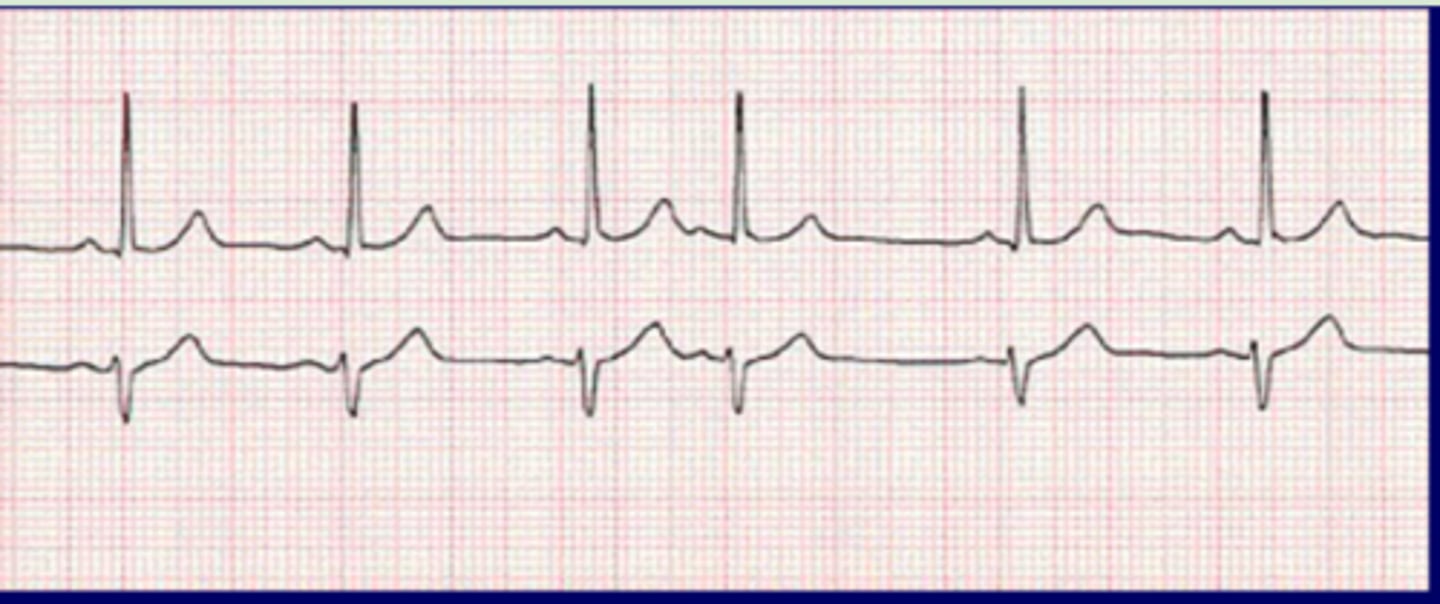
atrial flutter
Originate: atrial automaticity focus in self-perpetuating loop
QRS complex: narrow
P wave: saw tooth pattern
Heart rate: 250-400 bpm
R-R intervals: regular

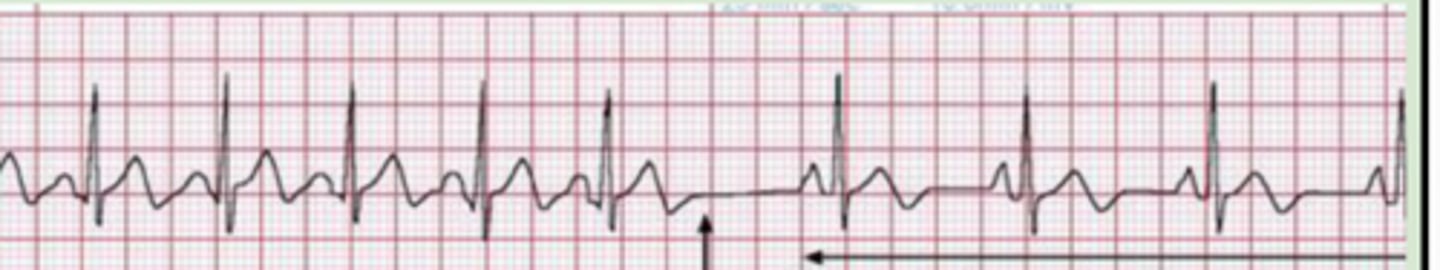
atrial fibrillation
Originate: atrial is fibrillating and not contributing to ventricular filling
QRS complex: narrow
P wave: none
Heart rate: variable
R-R intervals: irregular
Unsynchronized and chaotic

supraventricular tachycardia (SVT)
Originate: atrial or AV nodal focus
QRS complex: narrow
P wave: may not be identifiable
Heart rate: 140-280 bpm
R-R intervals: regular

paroxysmal SVT
Abrupt onset
Abrupt offset

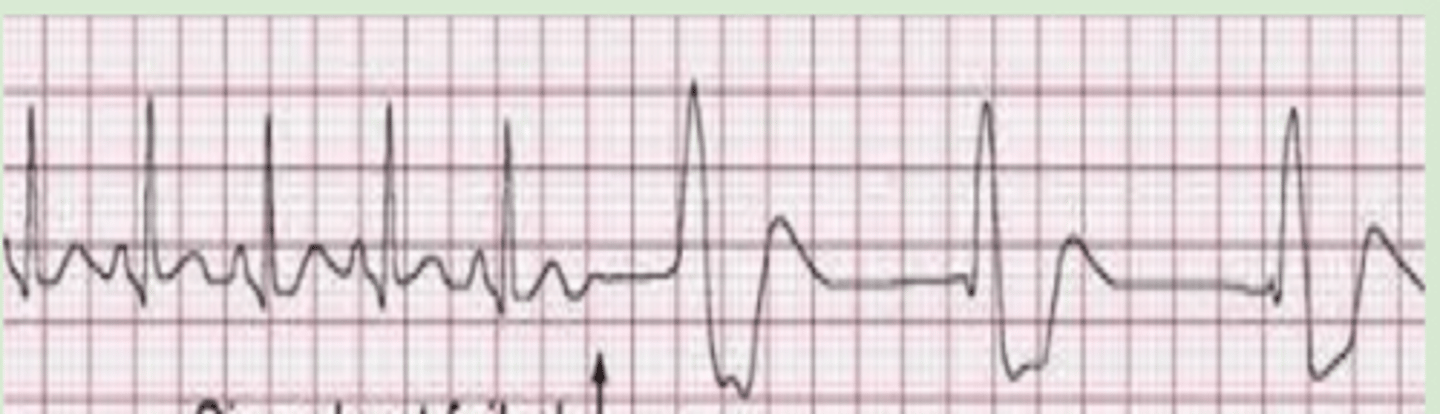
monomorphic ventricular tachycardia
Originate: ventricular automaticity focus
QRS complex: wide
P wave: none
Heart rate: very rapid
R-R intervals: regular
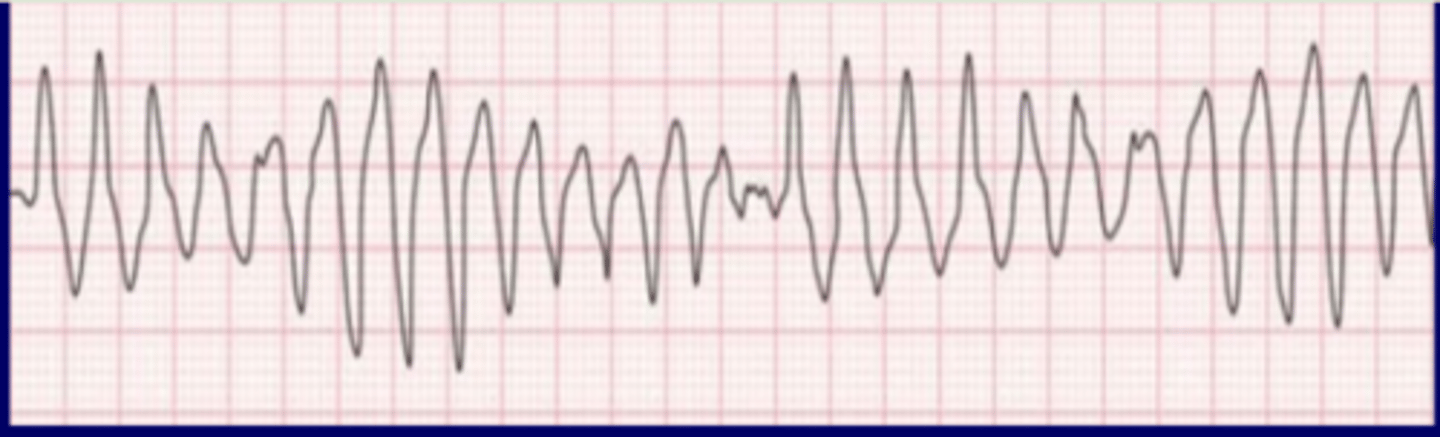
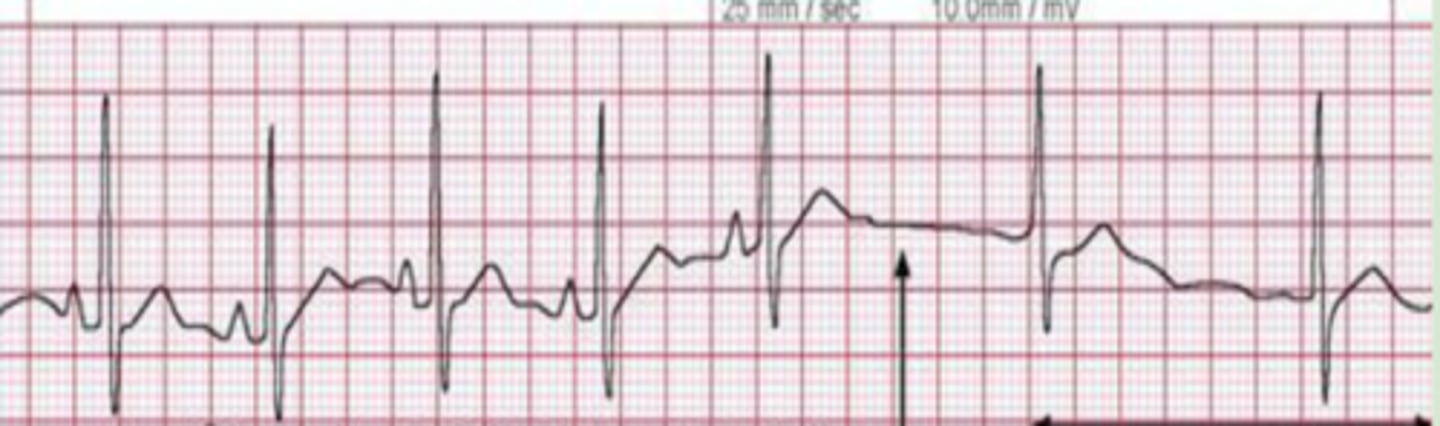
torsades de pointes
Originate: ventricular automaticity focus
QRS complex: twist
P wave: none
Heart rate: very rapid
R-R intervals: irregular
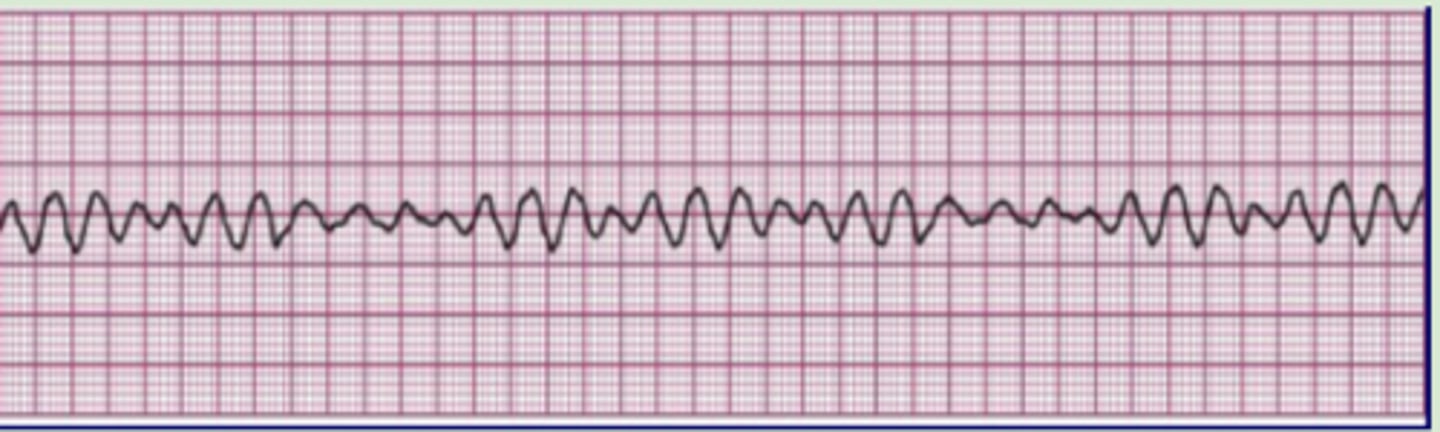
ventricular fibrillation
Originate: multiple weak ectopic ventricular foci
QRS complex: none
P wave: none
Heart rate: none
R-R intervals: irregular
Ventricle quivers
No cardiac output, no perfusion, no pulse
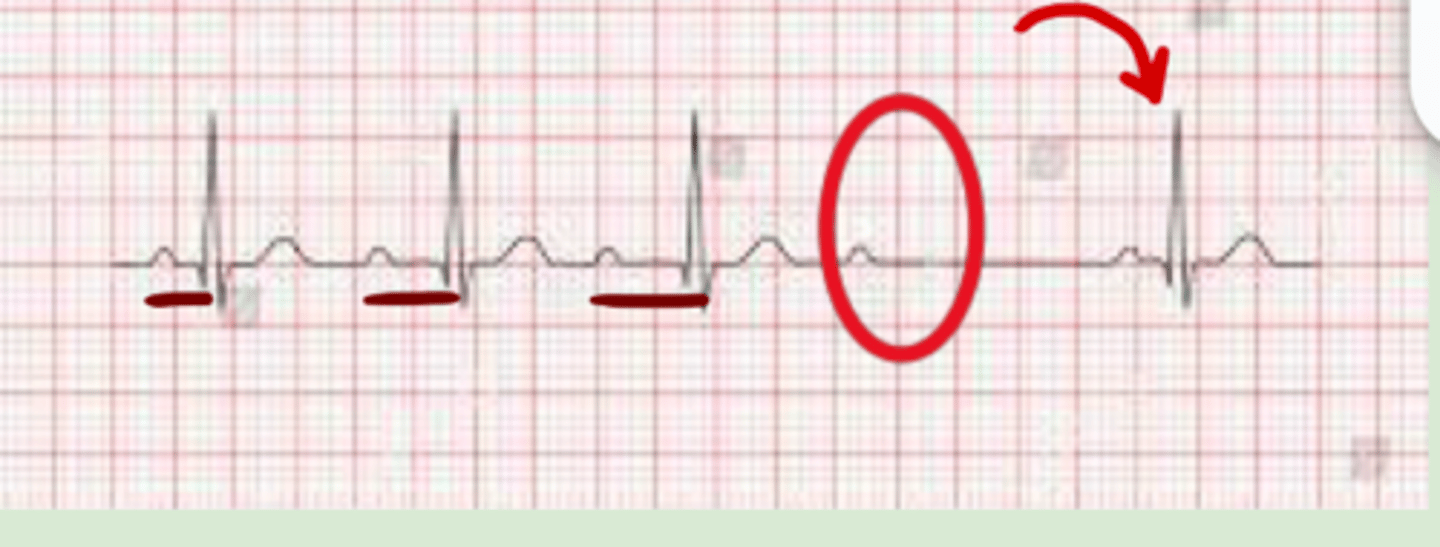
premature atrial contraction (PAC)
Originate: ectopic atrial focus fires impulse within SR
QRS complex: narrow
P wave: different
Heart rate: 60-100 bpm until PAC
R-R intervals: regular until premature beat causes interval to come earlier than expected
Pause after premature beat
premature junctional contraction (PJC)
Originate: AV node
QRS complex: narrow
P wave:
-None
-inverted before
-inverted after
Heart rate: 60-100 bpm until PJC
R-R intervals: regular until PJC

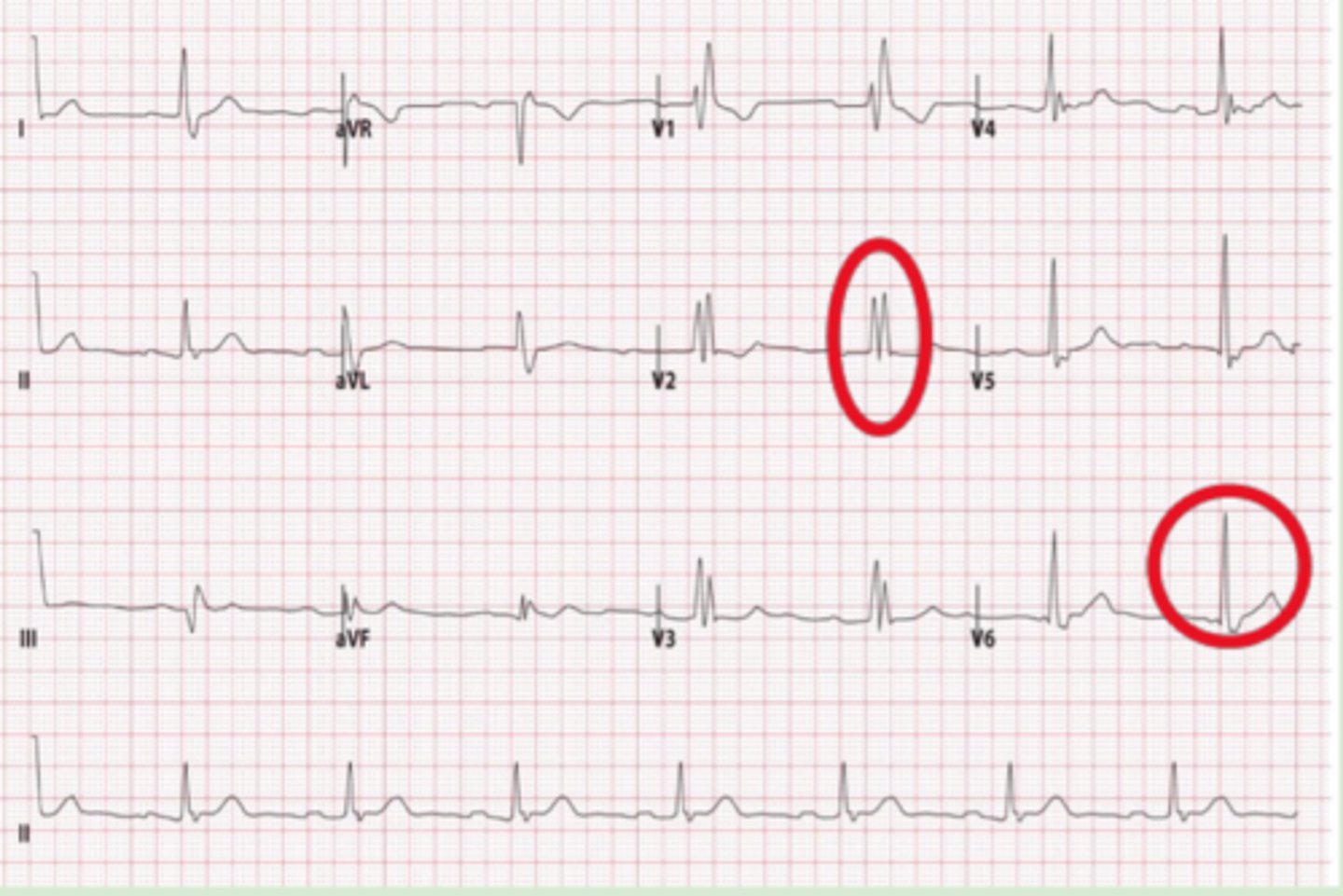
premature ventricular contraction (PVC)
Originate: irritable ventricular focus
QRS complex: wide
P wave: same until PVC
Heart rate: 60-100 bpm until PVC
R-R intervals: regular until PVC
Regularity:
-Isolated
-Bigeminy (every other beat)
-Trigeminy (every 3rd beat)
Series:
-Couplet (2 in row)
-Triplet (3 in row)
Morphology:
-Unifocal (same morphology)
-Multifocal (different morphology)

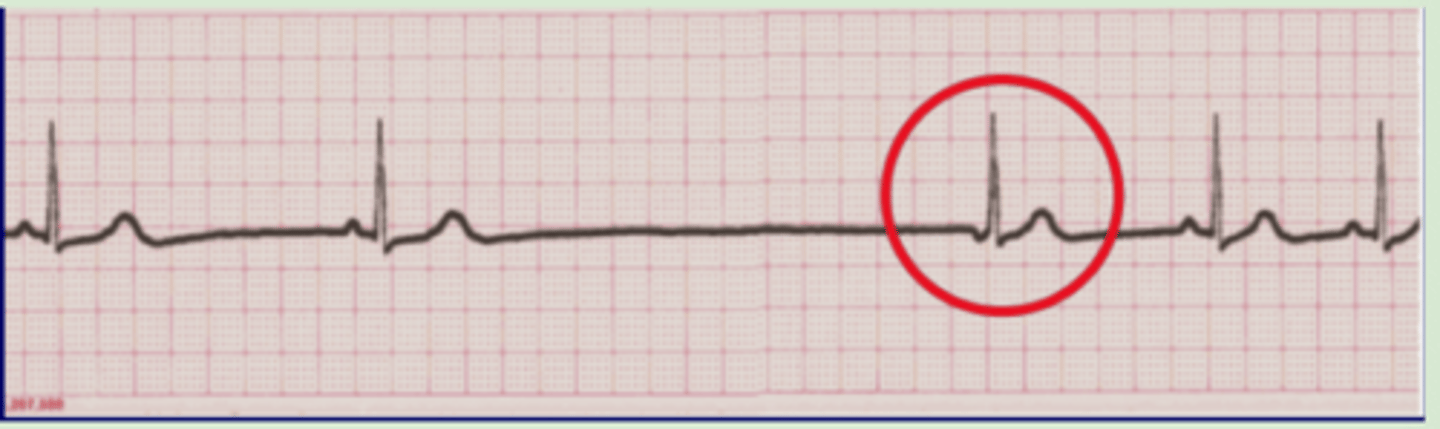
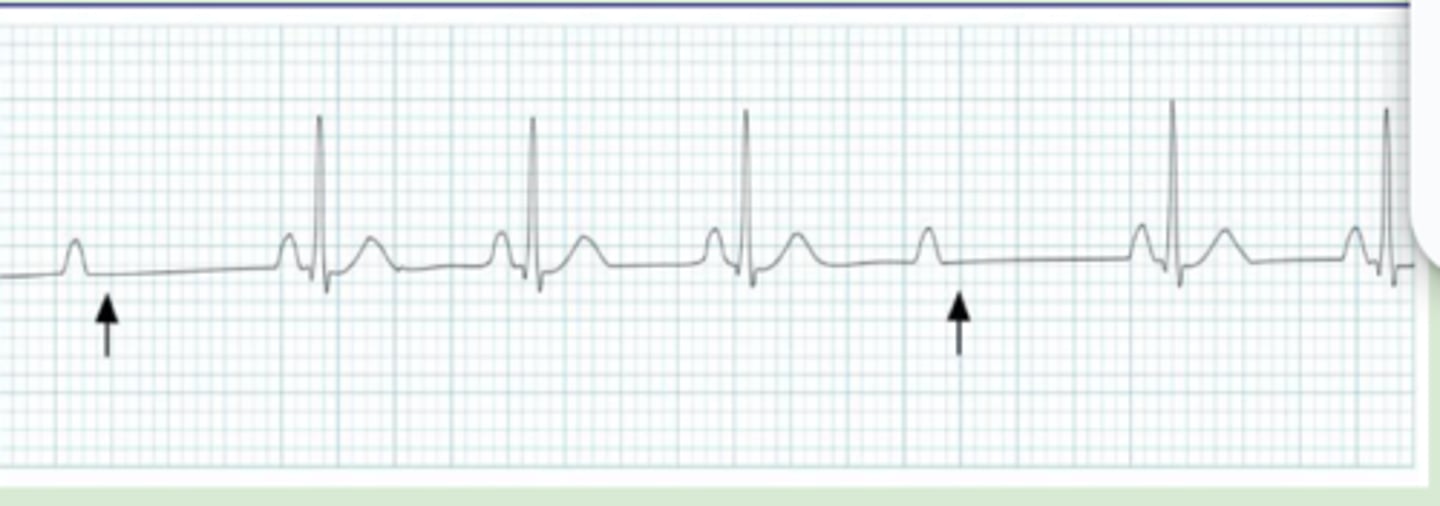
junctional escape beat
Regular sinus rhythm with a long pause followed by a singular junctional beat and return to normal sinus
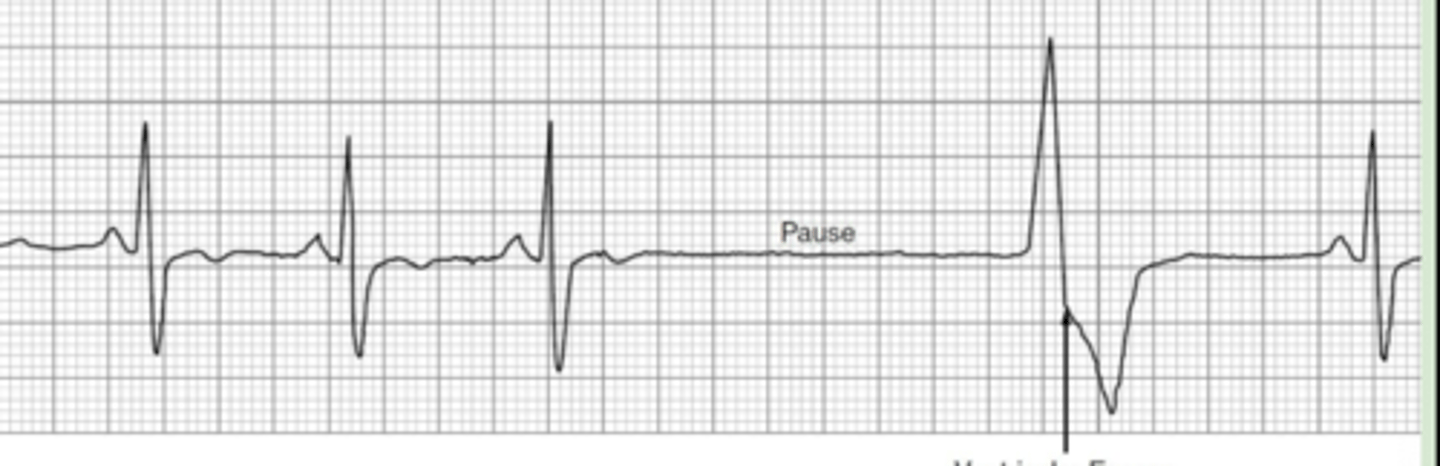
ventricular escape beat
Sinus rhythm → long pause → singular ventricular beat → return to normal rhythm
atrial escape rhythm
Failure of the sinus node → brief pause → takeover of rhythm by another atrial impulse
-P wave will differ following pause
junctional escape rhythm
Failure of the sinus node → brief pause → takeover of rhythm by the AV node
-inversion or absence of P wave will present in new rhythm
ventricular escape rhythm
Failure of the sinus node → brief pause → takeover of rhythm by focus in the ventricle
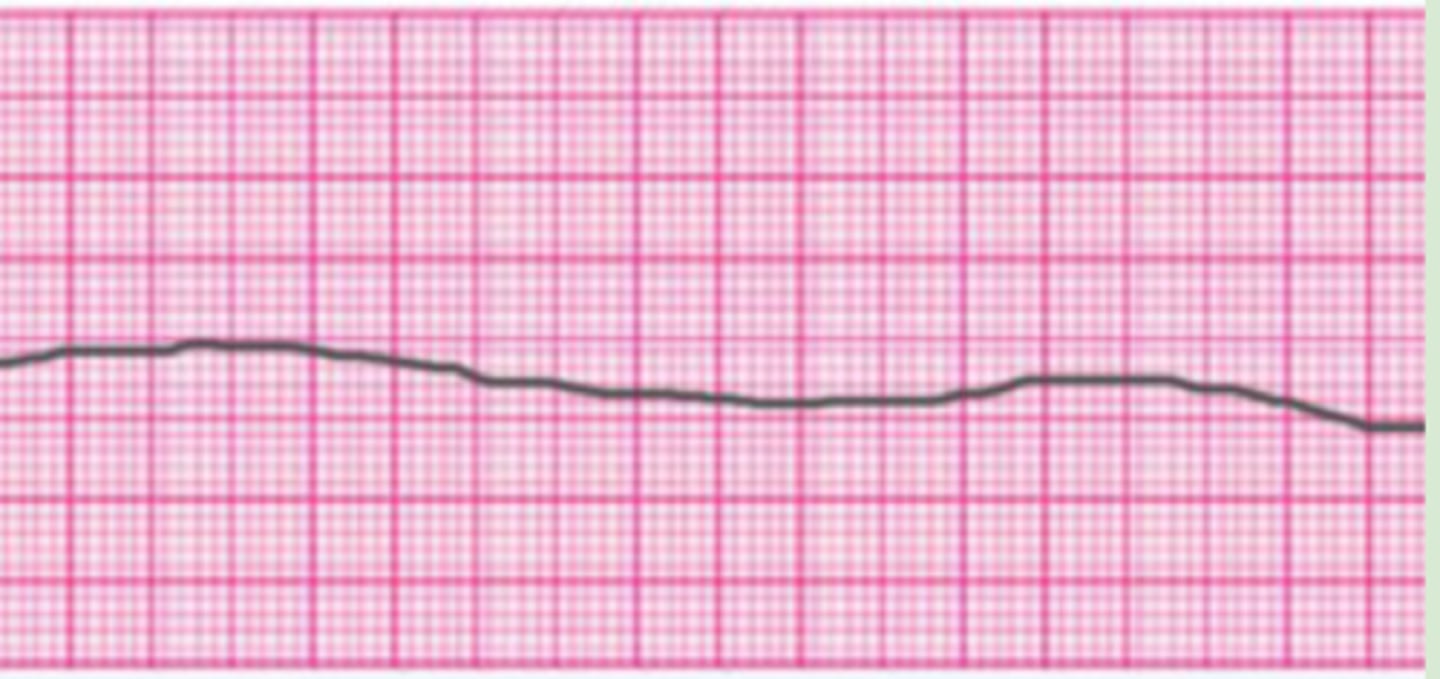
asystole
Failure of the sinus node → no assumption of pacemaker activity by other areas → no cardiac output, no perfusion, and no pulse
first degree AV block
Delayed impulse from SA to AV node → prolonged PR interval with each beat
-1 box large
-rest will look normal

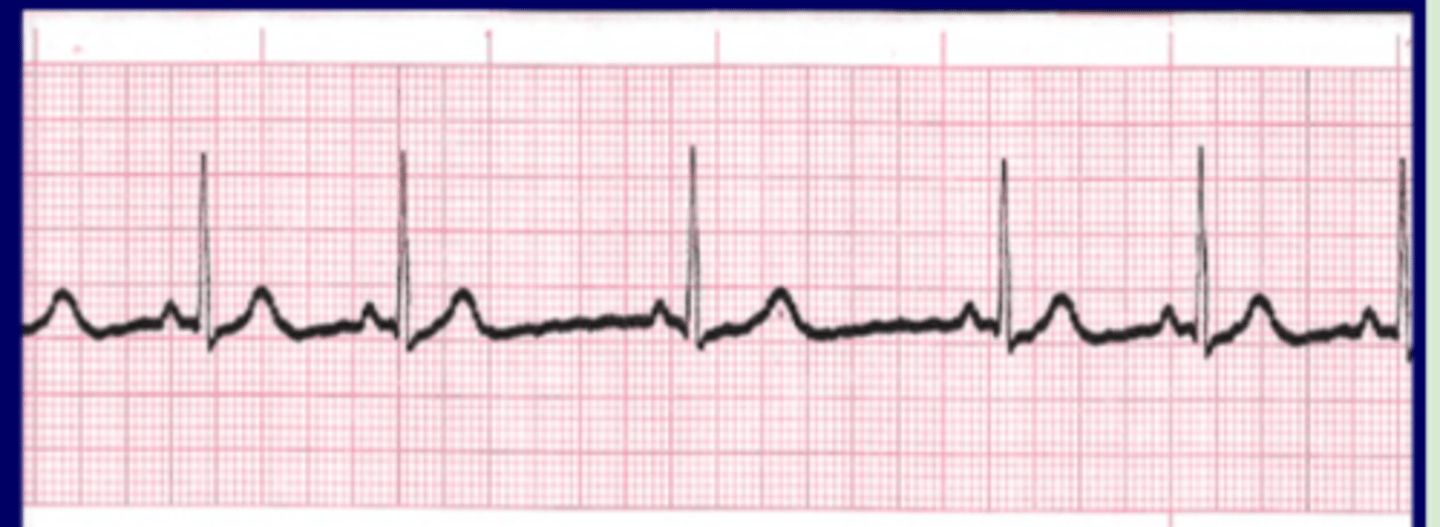
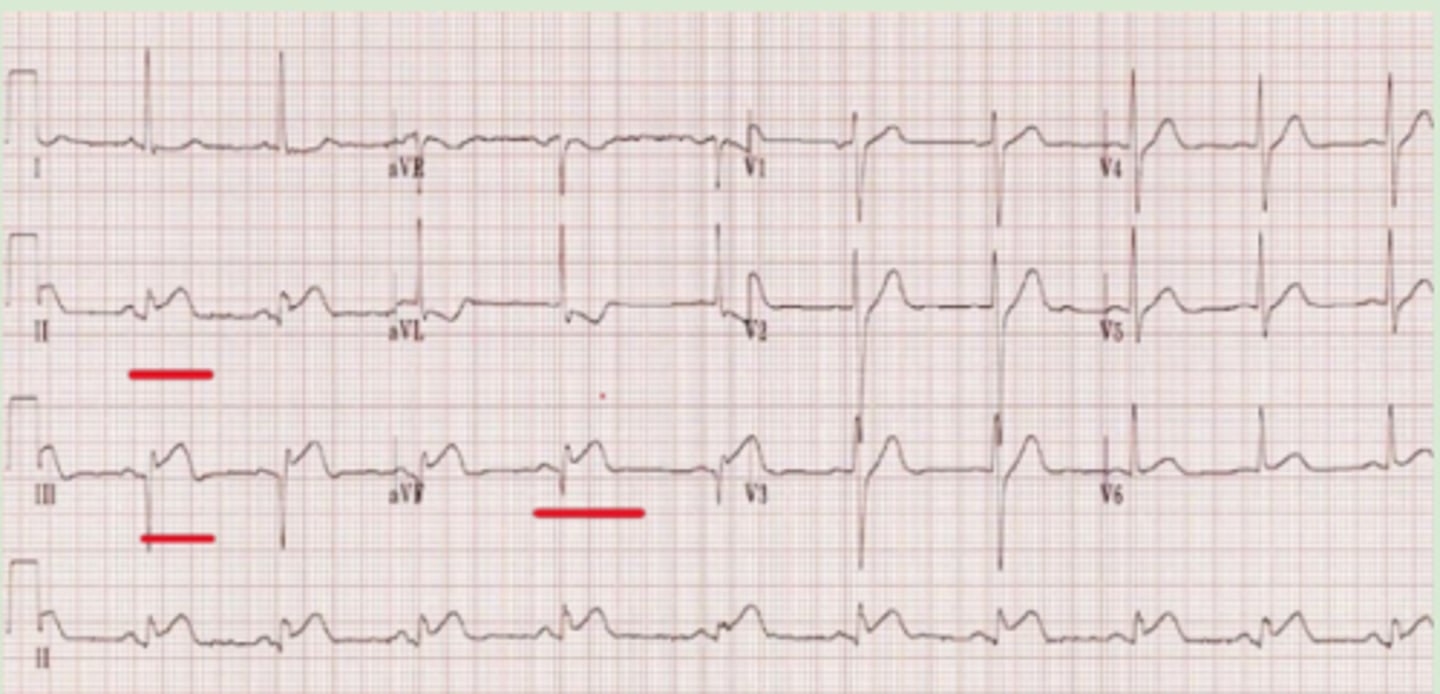
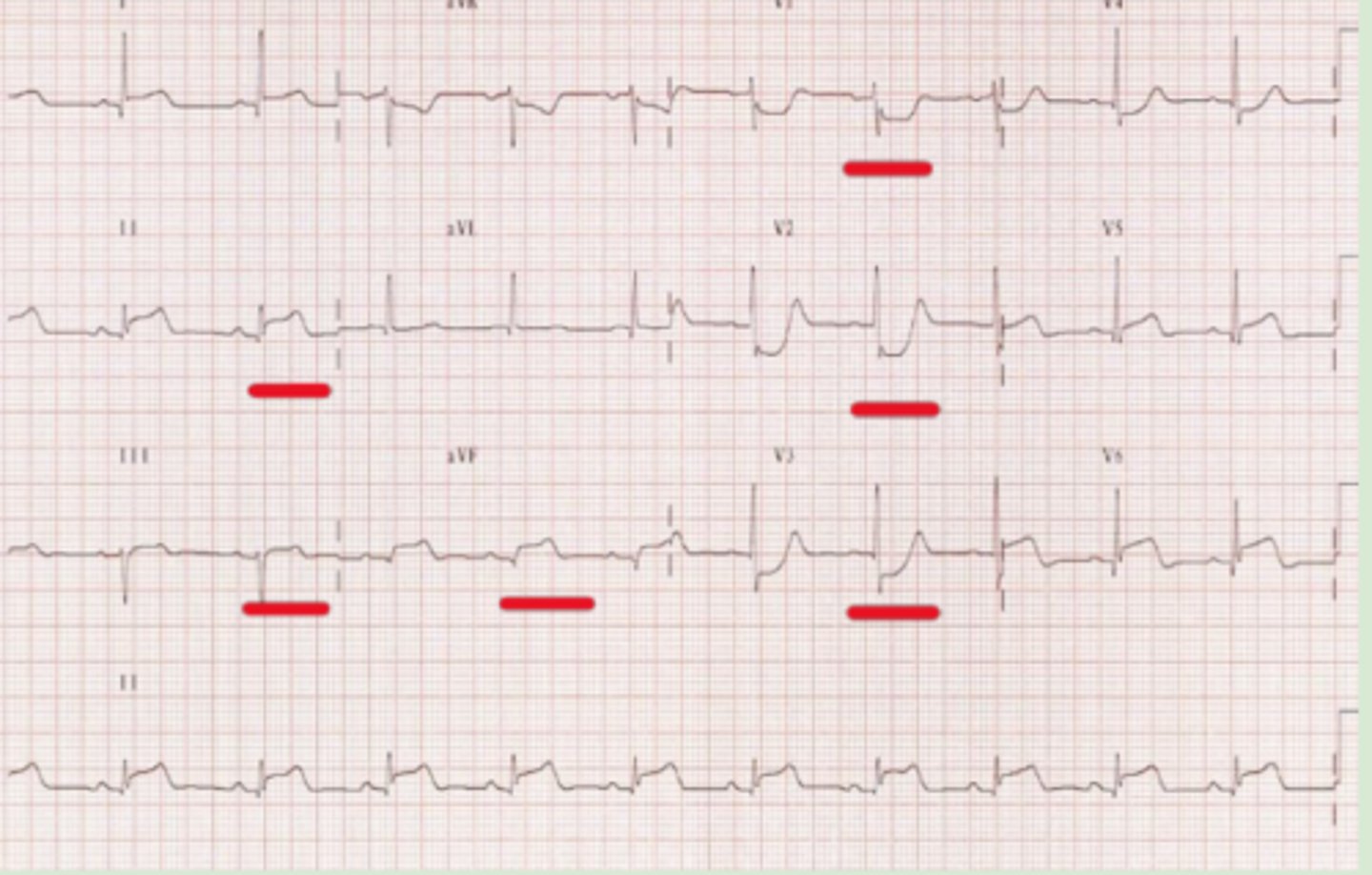
second degree type I AV block (wenckebach)
Impulses through the AV node take progressively longer showing then are completely blocked
-PR interval will slowly become more prolonged → P wave with no present QRS complex to follow → rhythm picks back up
second degree type II AV block
Atrial impulses are locked sporadically
-NO prolongation prior to dropping of the QRS complex → PR interval will be constant
third degree
Sinus beats are independent from the beat originating in the AV node or ventricle
-There will be zero relation of P waves to the QRS complex

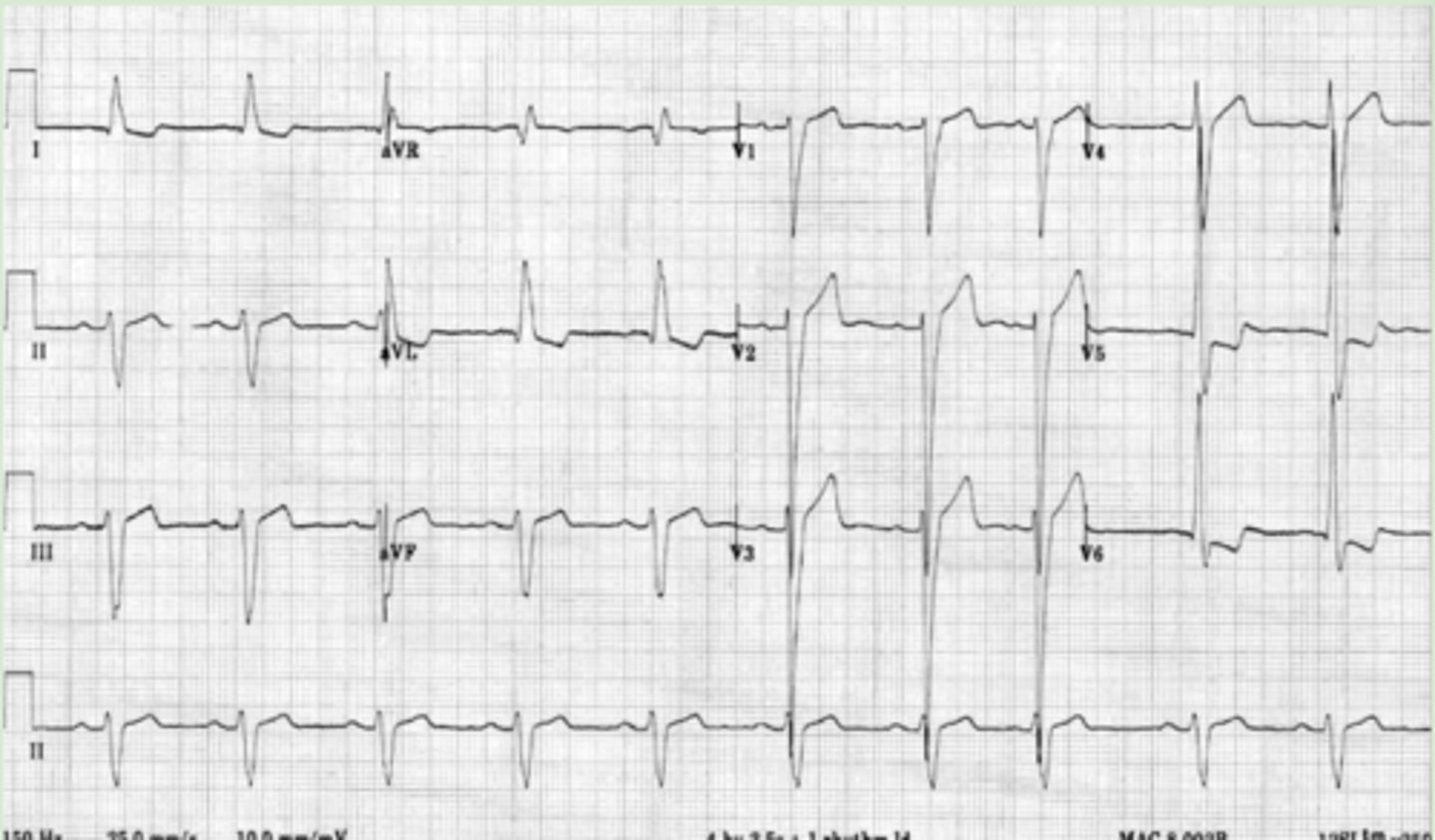
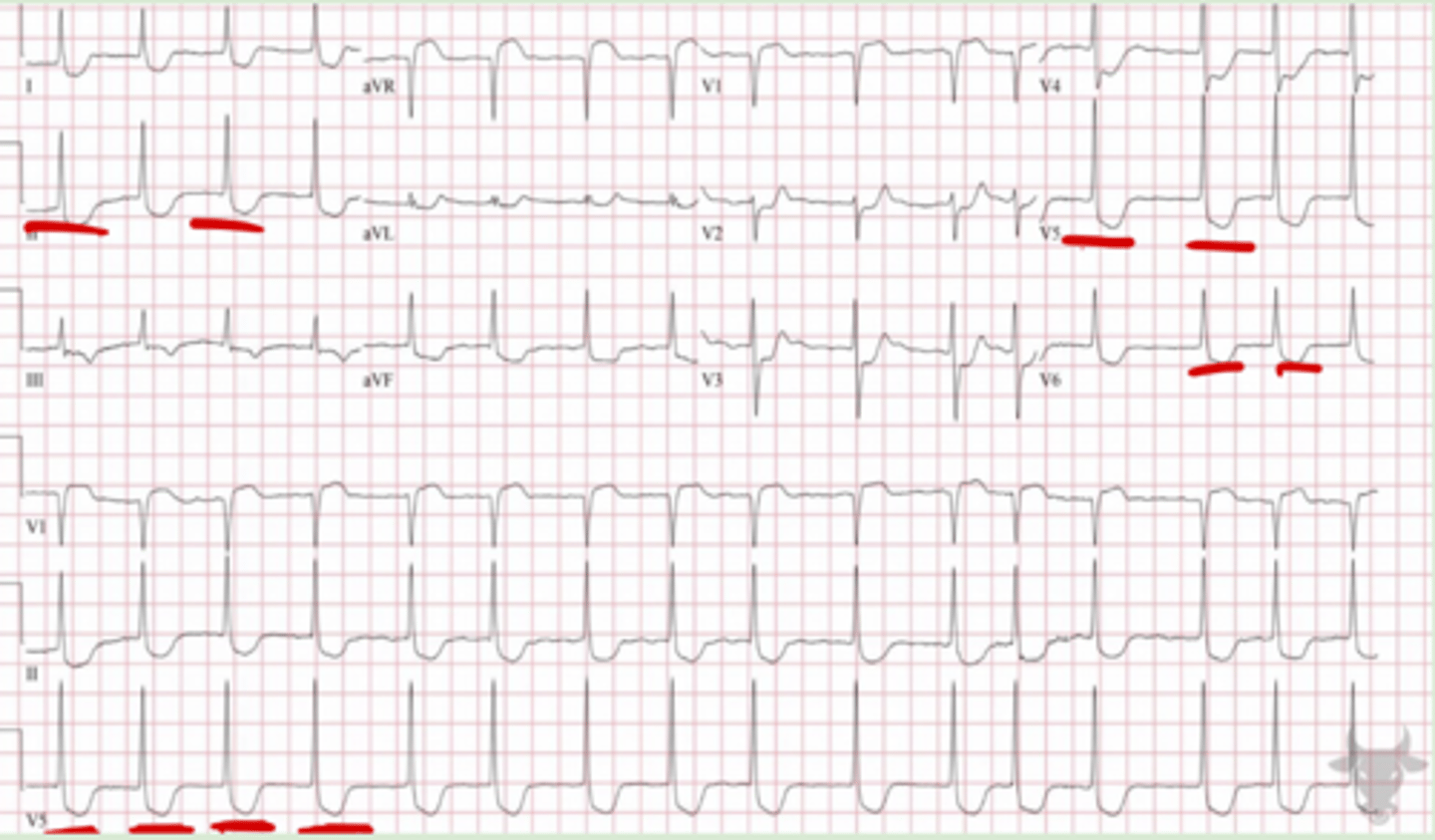
left bundle branch block
QRS = >0.12 seconds
Primarily V1 but also V2-V3
-Deep S waves
V5-V6
-Tall R waves
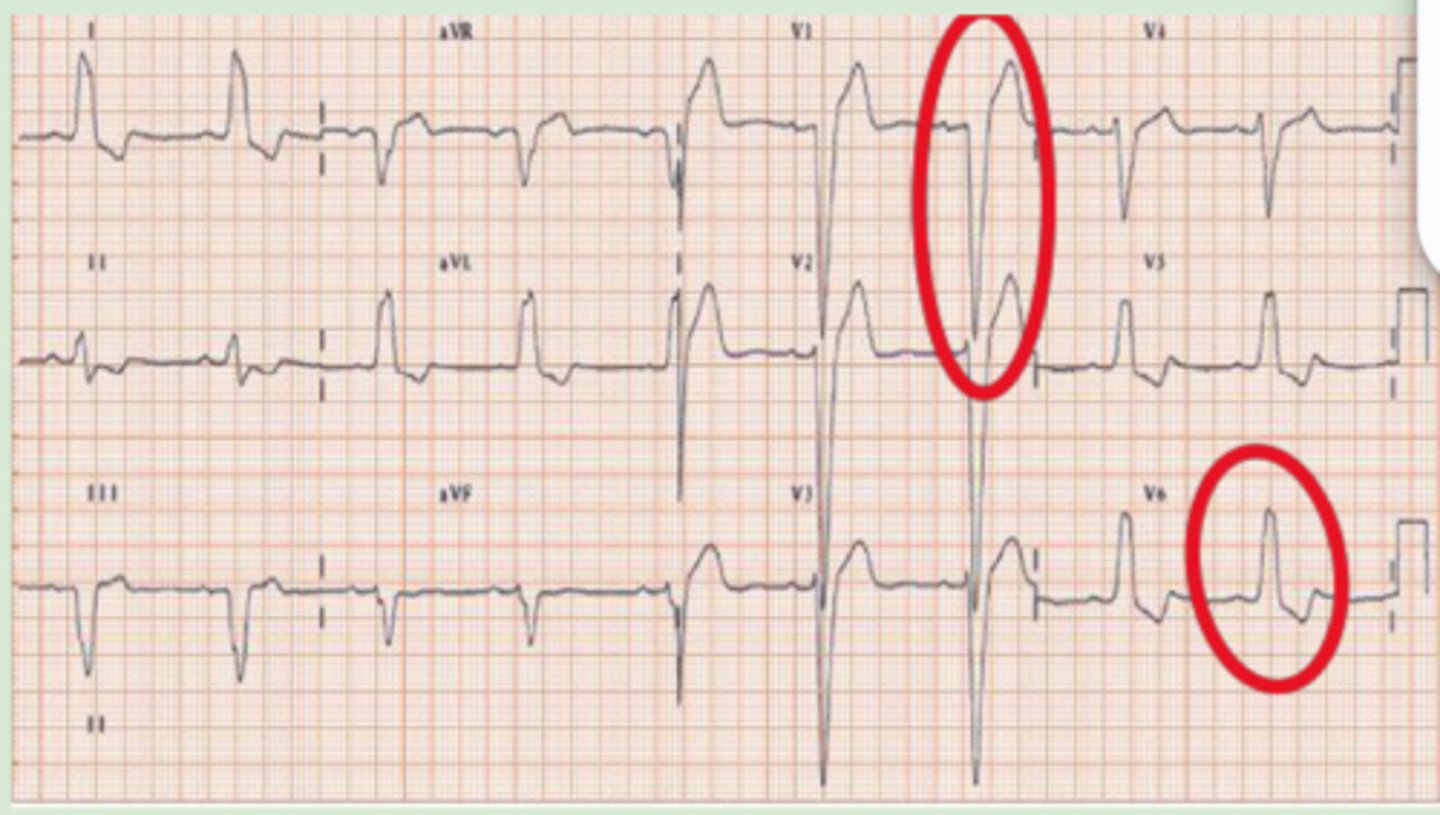
right bundle branch block
QRS = >0.12 seconds
Primarily V1 but also V2-V3
-RSR appearance (M wave)
V5-V6
-Wide, slurred s wave
right ventricular hypertrophy
V1 = Dominant R wave
-Larger than S wave or > 7 mm tall
-May also see T wave inversions
V5&6 = Dominant S wave
-Larger than R wave or > 7 mm tall
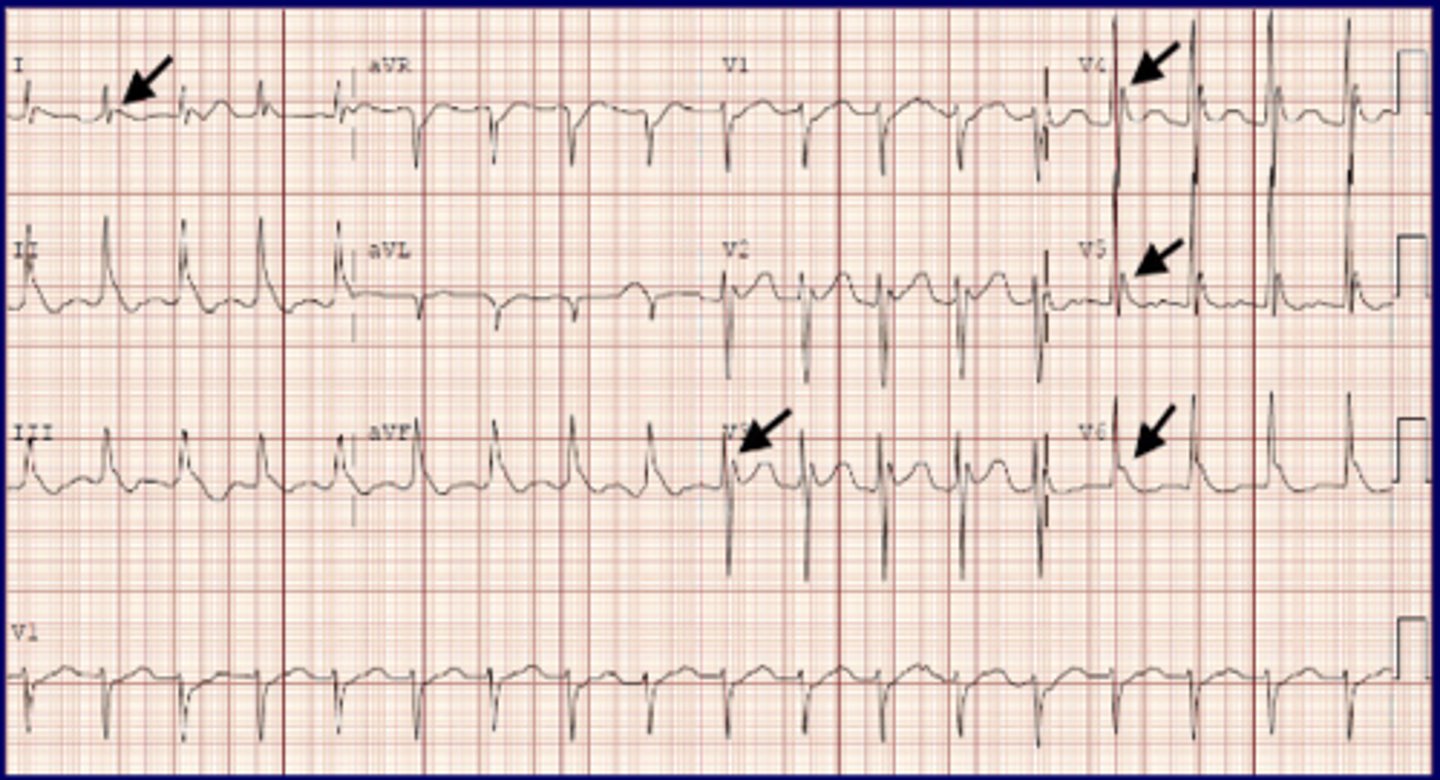
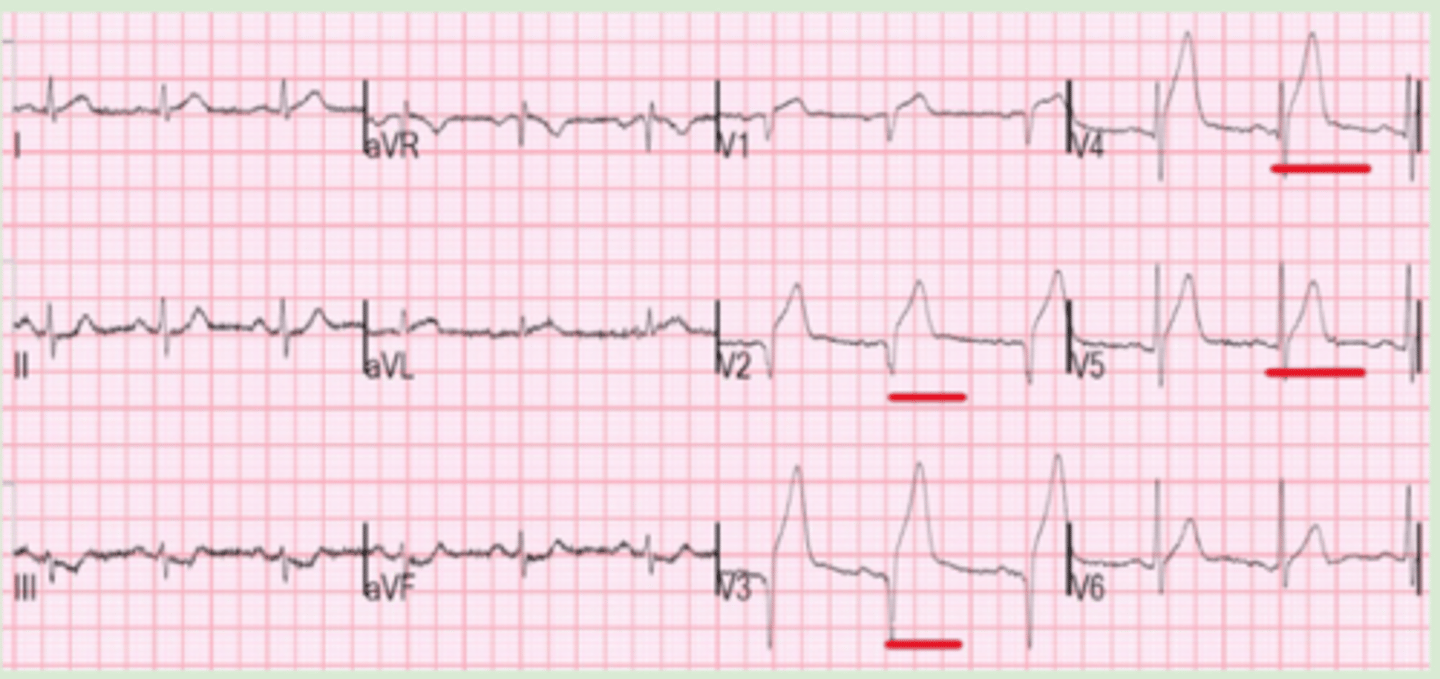
left ventricular hypertrophy
I, aVL = Increased amplitude of R waves
III, aVR, V1-V3 = Increased depth of S waves
V5-V6 = Tall R waves
-Will also see ST & T wave abnormalities consistent w/ LV strain
inferior myocardial infarction
ST elevations in leads II, III, aVF
lateral myocardial infarction
ST elevations in leads I, aVL, V5, V6
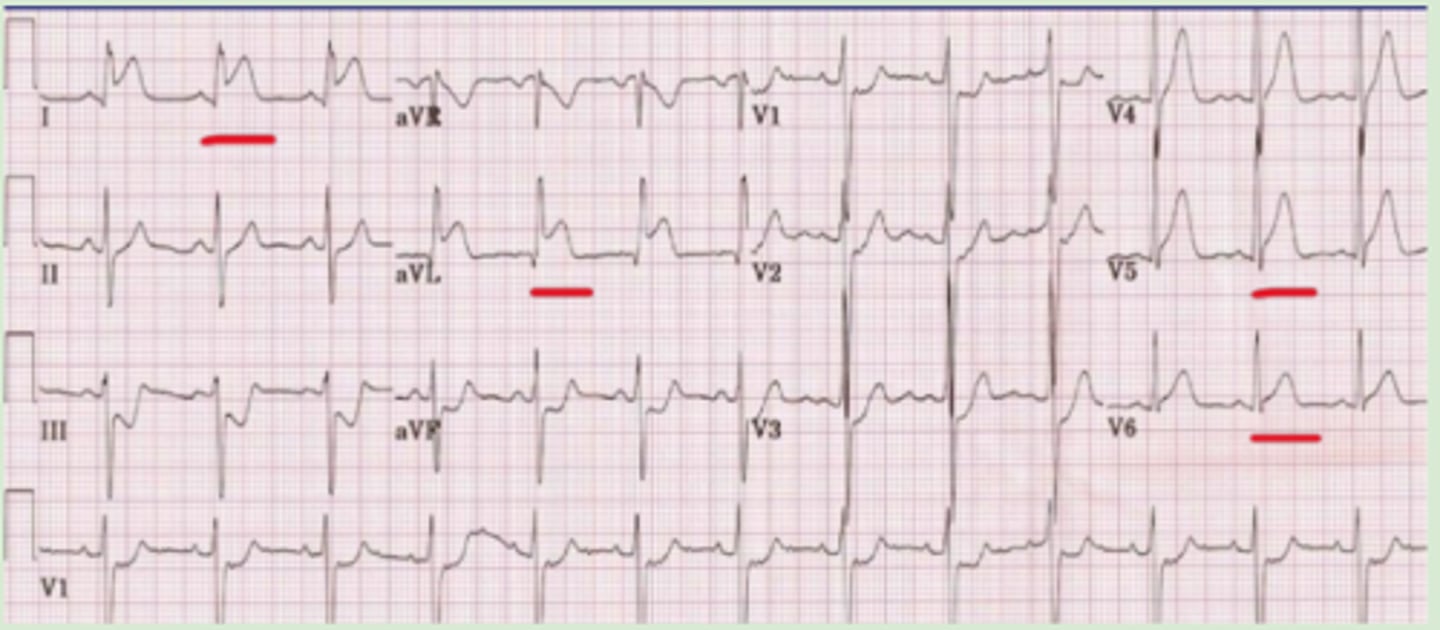
anterior myocardial infarction
ST elevation in leads V3 and V4
inferior + posterior myocardial infarction
ST elevation in leads II, III, aVF + ST depression in leads V1-V3
myocardial ischemia
ST depression consistent across leads with no presence of elevation
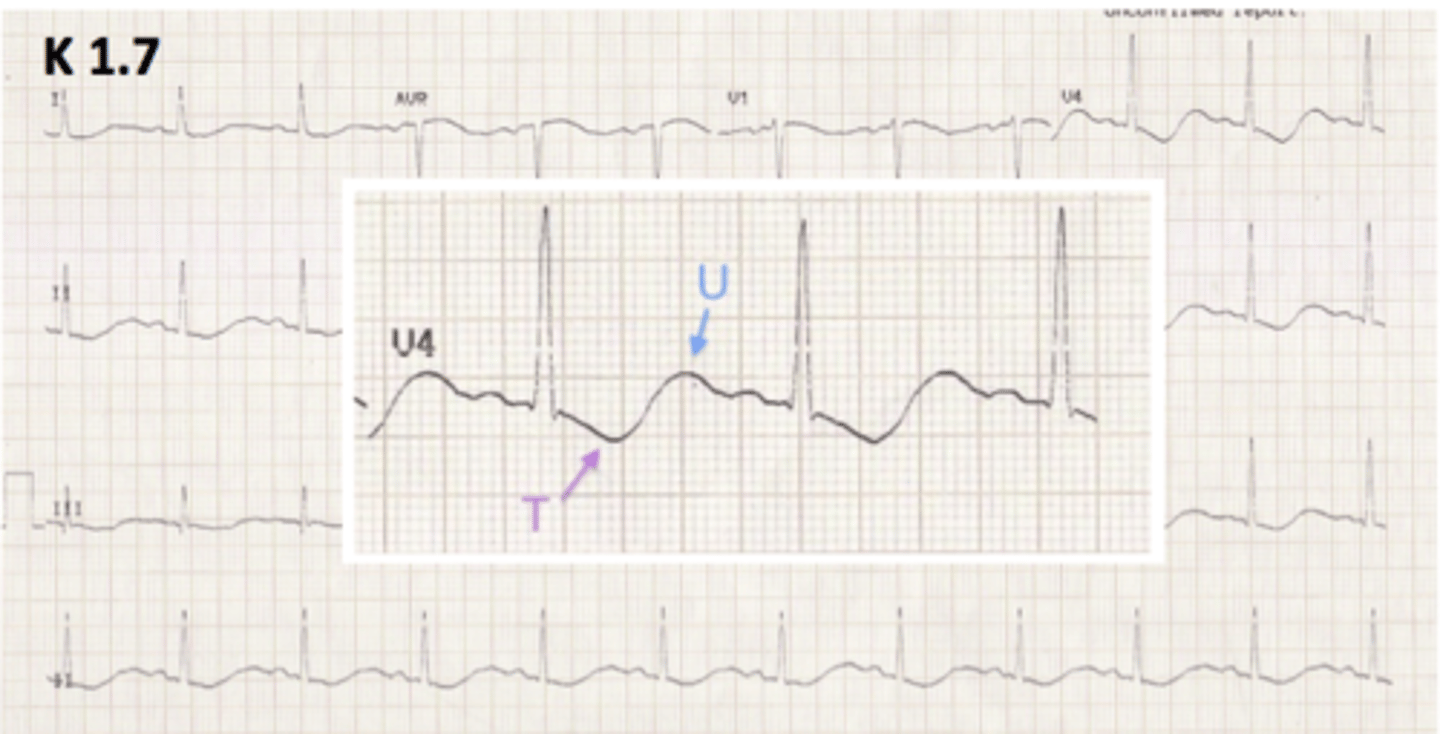
moderate hypokalemia
prominent U wave
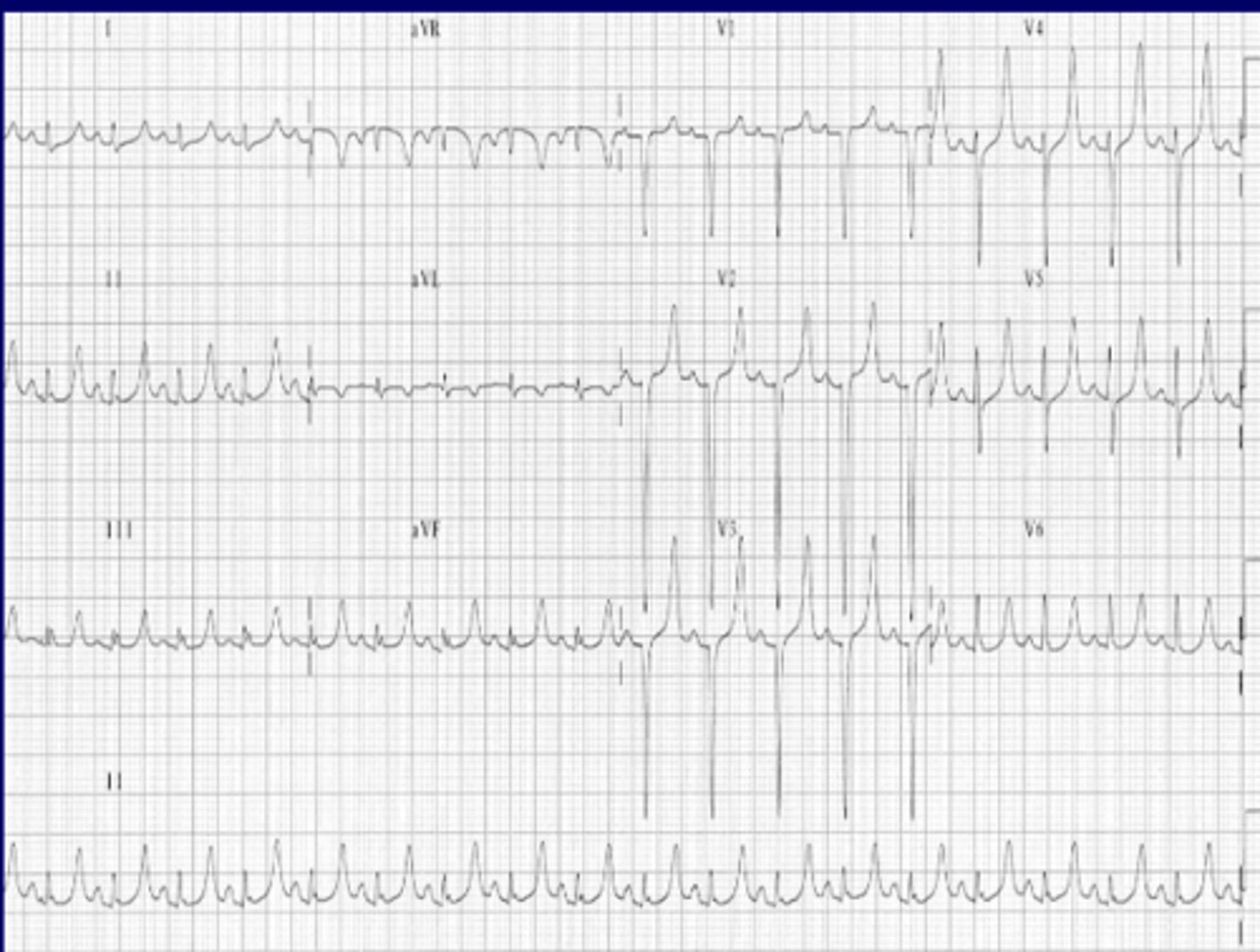
severe hypokalemia
hyperkalemia
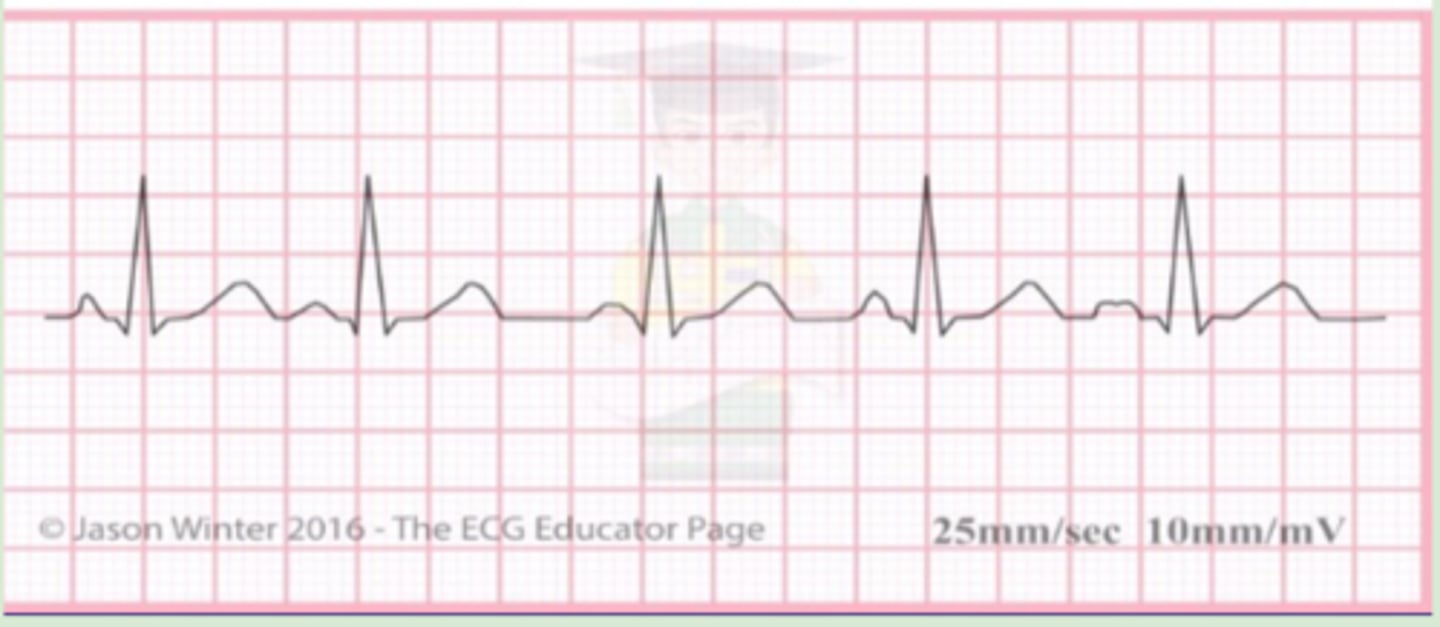
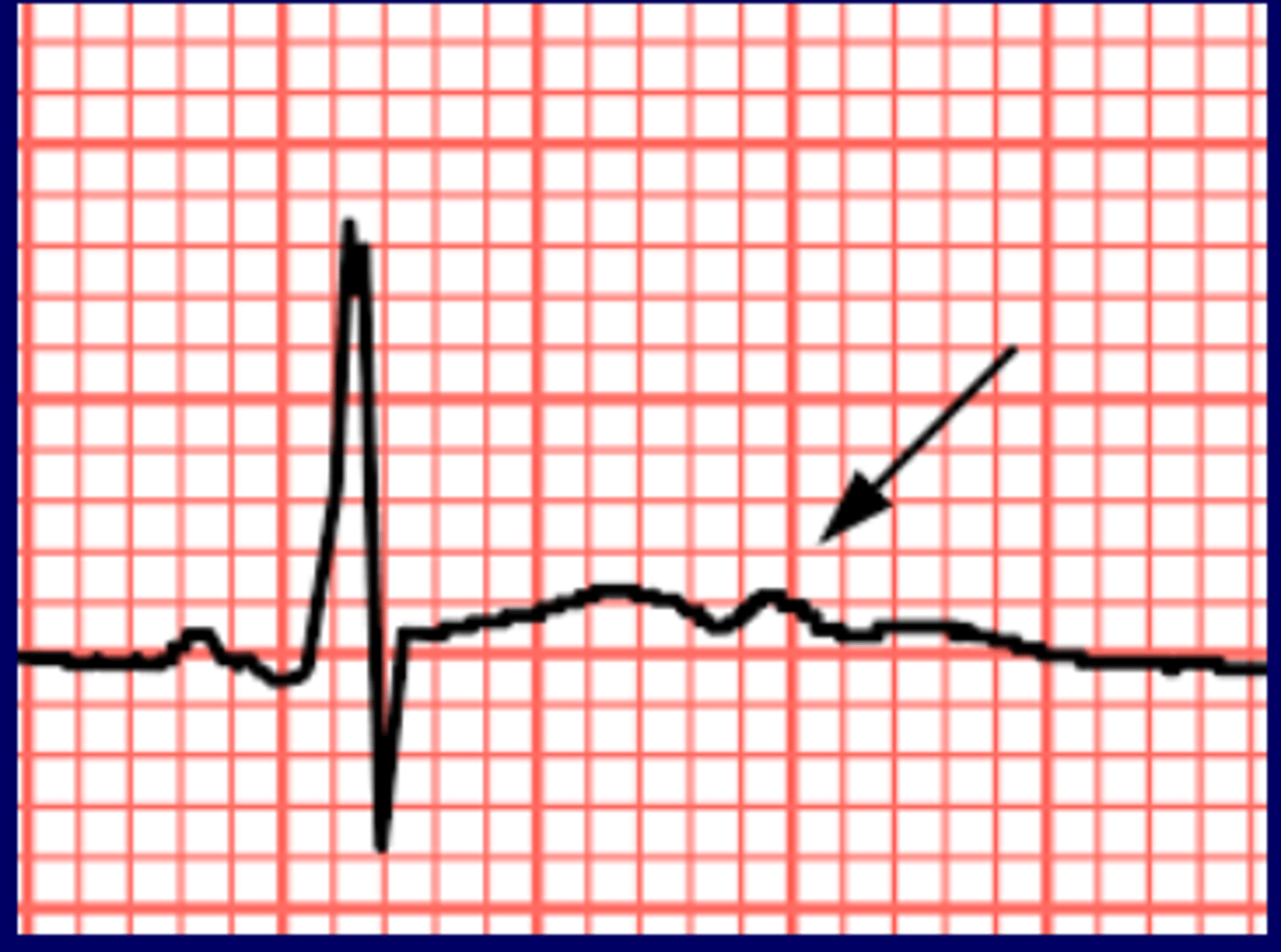
hypothermia
Osborne J-wave
-occurs near J-point on the S wave and ST junction