Reproductive Physiology - Lecture 3
1/66
Earn XP
Description and Tags
Fertilization and Pregnancy
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
what is fertilization?
the fusion of male and female gametes to form a zygote
what is fertilized egg called for the first two months
embryo
what is the fertilized egg called for the next 7 months
fetus
how long does the gestational period
40 weeks
what is the site of fertilization
female oviduct
how long is sperm viable for
5 days
how long is the oocyte viable for
12-24 hours
is the sperm initially capable of fertilization
no, it requires it capacitation
what is the survival time of sperm in the reproductive track
5 days
what are the two reaons only a few hundred sperm make it to the uterine tubes
damage due to acidic pH in the female tract
some sperm are lost due to leakage from cervix
what is capacitation
Capacitation is a process that sperm undergo in the female reproductive tract, which enhances their motility and ability to fertilize an egg. This prepares the sperm to successfully penetrate the zona pellucida of the oocyte.
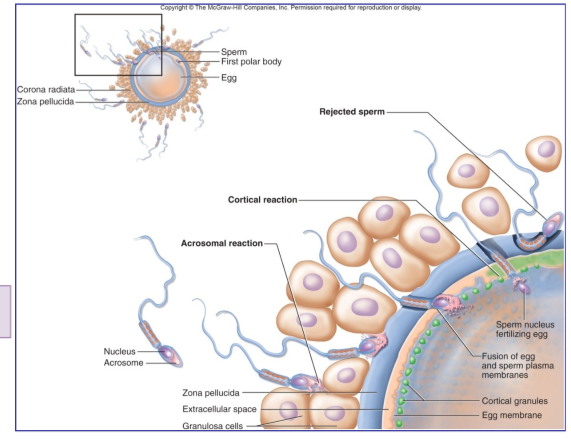
what is the acrosome reaction
The acrosome reaction is a vital process during fertilization where the sperm's acrosome releases enzymes that digest the zona pellucida, facilitating the sperm's entry into the oocyte.
enzymes poke hole into the zona pellucida so the nuclear male parts can get to female nuclear parts
why is polyspermy not favoured in fertilization
Polyspermy is not favored in fertilization because it can lead to an abnormal number of chromosomes, resulting in failed embryo development.
how is polyspermy prevented during fertilization
polyspermy is prevented by block
describe the polyspermy block mechanism
when sperm make contact with the egg membrane, a change in membrane potential occurs
corticle granulles surrounding the egg release its enzymes to harden the zona pellucida
since hardended, the proteins in the zona pellucida are inactivated, so sperm cannot bind to the zona pellucida
describe the pathway of fertilization
Fertilization begins with sperm traveling through the female reproductive tract, meeting the egg in the fallopian tube. The sperm then penetrates the zona pellucida, triggering the cortical granule release and fusion with the egg, culminating in the formation of a zygote.
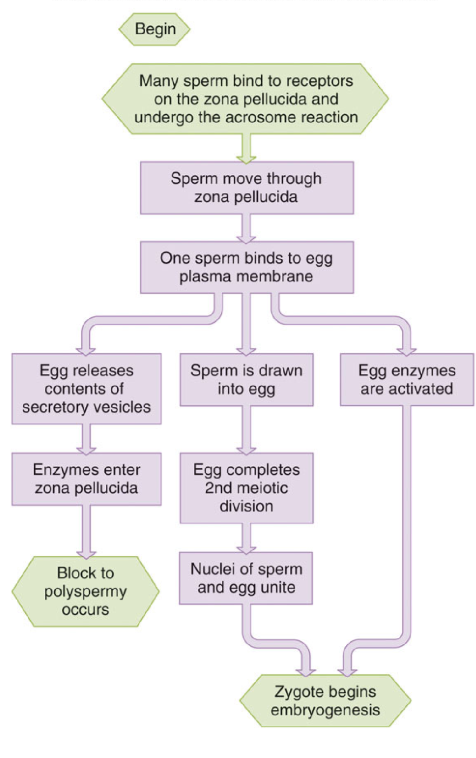
what stimulates the 2nd meiotic division of the oocyte
fusion of sperm with the oocyte, causes it to become the ovum
what occurs after the second meiotic division
the sperm plasma membrane disintegrates, chromome somes from sperm and ovum migrate to center resulting in DNA replication leading to a zygote
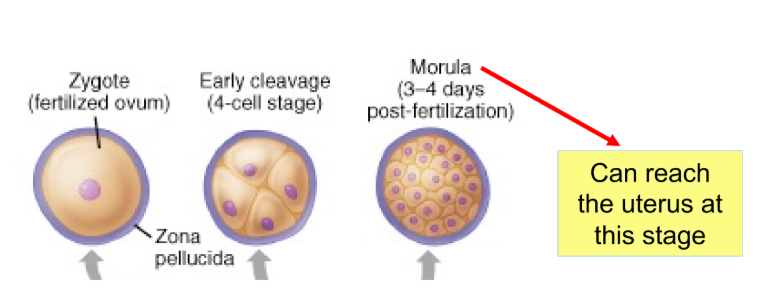
what do the mitotic division after fertilized ovum result in?
the formation of the morula
same size as zygote
can now reach the uterus and begin implantation
the morula is totipotnet at the 16-32 cell stage. what does totipotent mean?
Totipotent refers to the ability of a cell to differentiate into any cell type, including all embryonic and extraembryonic cell types.
each cell has the capacity to grow into the individual
division of the totipotent morula cells results in _____
identical twins
‘egg splits into two’
fertilization of two oocytes released during the same cycle result in ….
fraternal twins
what forms after the morula phase?
blastocyst stage
what is the outer layer of the blastocyst
the trophoblast
which will become the fetal placenta
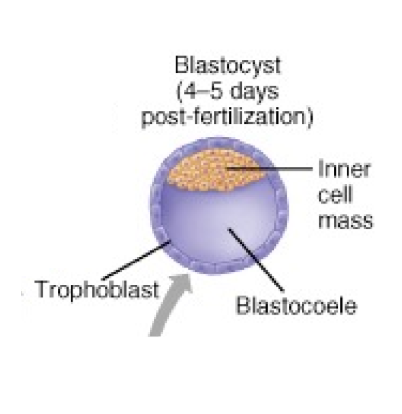
what is the inner layer of the blastocyst
the inner cell mass that floats within the blasocoele cavity
will become the embryo
does a blastocyst have a zona pellucida?
no, it is replaced by a trophoblast
are cells still totipotent in the blastocyst stage?
no, they become pluripotent
each cell will differentiate into specific cell types to make the organs
what hormone is high in the uterus during the blastocyst stage
progesterone is high to allow for implantation
when does implantation occur
6-7 days after fertilization
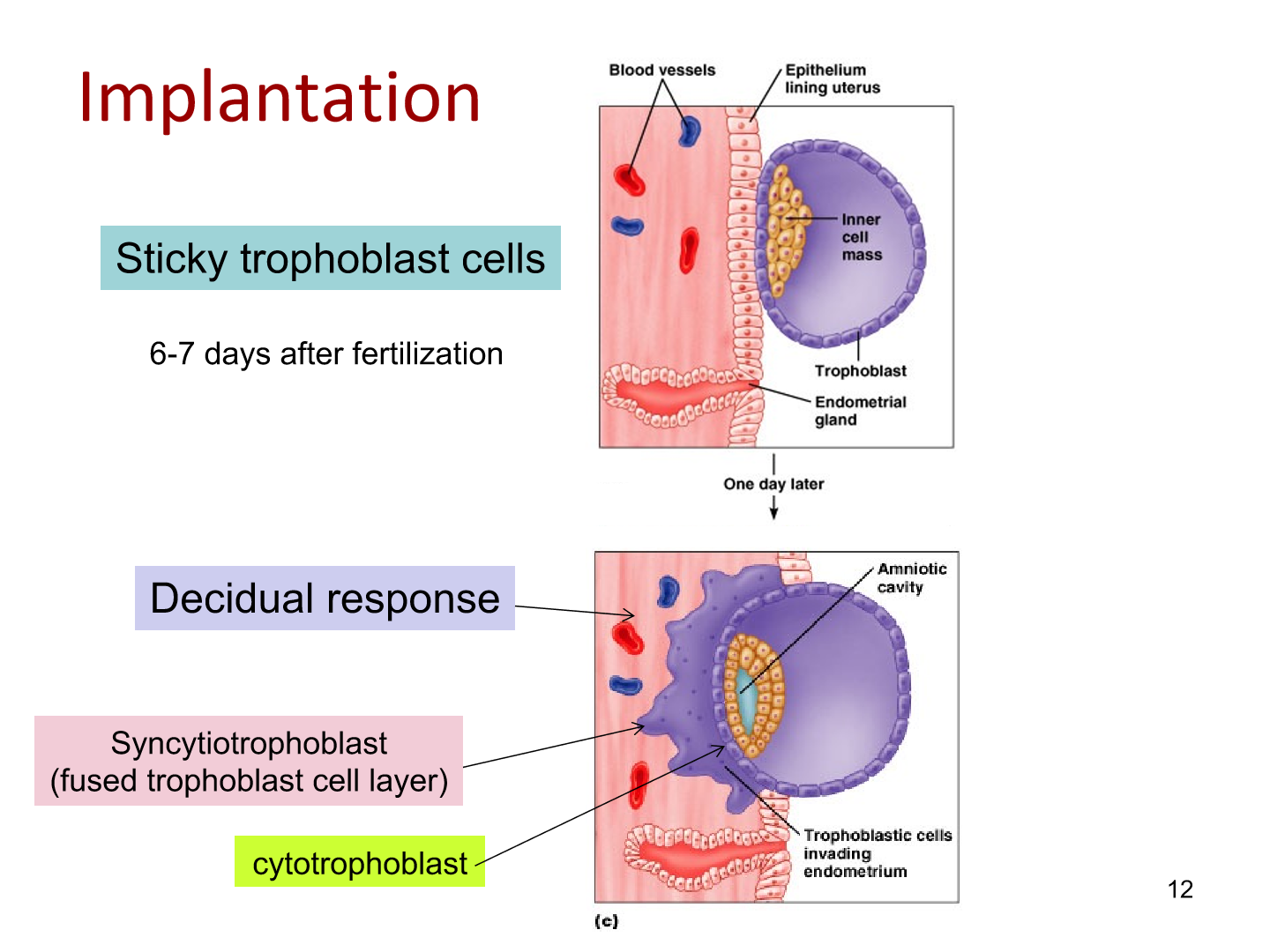
describe the process of implantation
trophoblast layer has enzymes that can dig itself into endometrial layer by eating through endometrial layer
syncytiotrophoblast are the fused trophoblasts that attach to endometrium
cytotropblasts are differentiated trophoblasts
amniotic cavity forms during implantation as blastocyst burrows
what is the decidual response
The decidual response refers to the changes in the endometrium (uterine lining) that prepare it for and support pregnancy, specifically in response to implantation of an embryo.
after how many weeks is the placenta completely functioning and the embryo has a heart beat
5 weeks
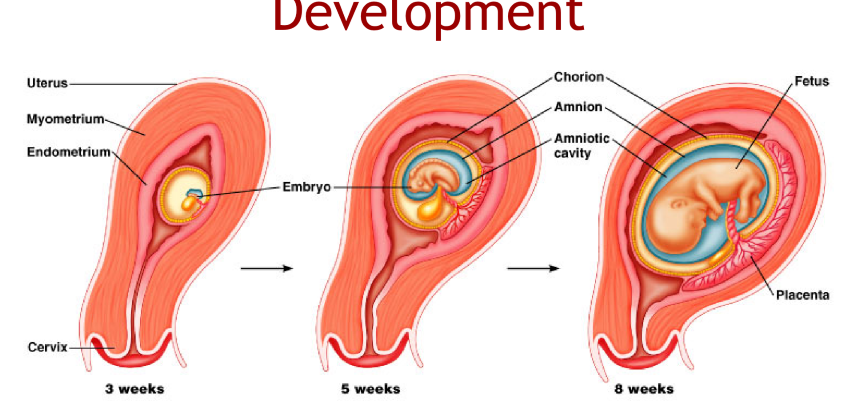
what is the function of the amniotic cavity
a cavity made of fluid that cushions the fetus and avoid bugs and germs from mother’s body
where does all the food from the mother enter the embryo, and where does the embryo’s waste leave?
from the umbilical cord
all waste is then excreted via mother’s kidneys or GI system
what are the three functions of the placenta
endocrine organ
secrete hCG and three other hormones
exchange tissue
respiratory gases, nutrients and waste products
filter/immunological protection
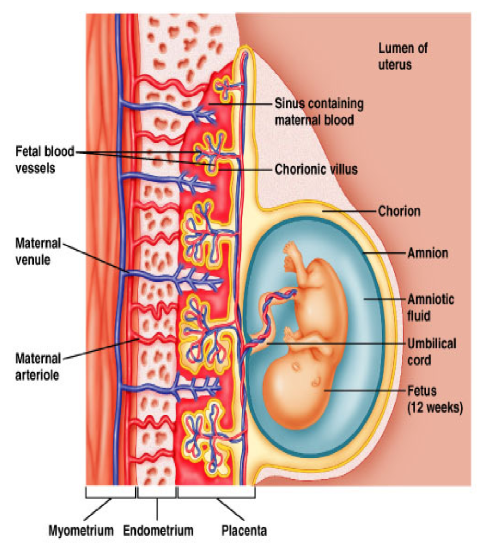
what is the function of chorionic villus
area of exhange with the placental capillaries to exhance nutrients with the baby
do maternal and baby blood ever come in direct contact?
no never. chorion creates a seperation
oxygen and gas can diffuse, but not blood itself
what are the four major hormones of the placenta
human chorionic gonadotropin (glycoprotein)
human placental lactogen (protein)
Progesterone
Estrogen
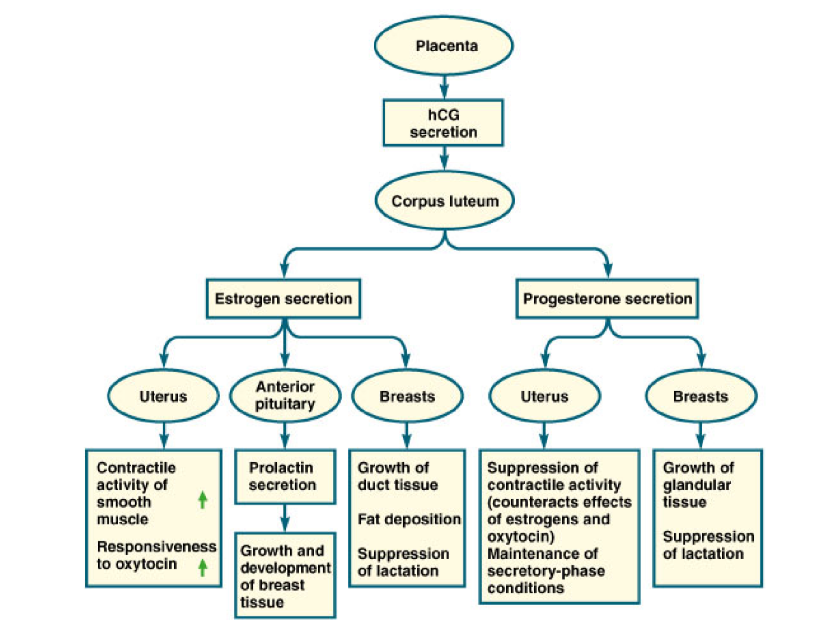
function of hCG
maintains corpus luteum in early pregnancy
function of hPL
Growth hormone and anti-insulin action in mother
prevents mother from taking up sugars so they can be transfered to the embryo at placenta
4 functions of placental progesterone
decreases uterine contraction (no labor)
inhibition of LH and FSH
growth of mammary glands
secrete sperm unfriently mucus
3 functions of placental estrogen
growth of myometrium
growth of mammary ducts
inhibition of LH and FSH
when the trophoblast layer attaches to uterine wall, what hormone is secreted
hCG
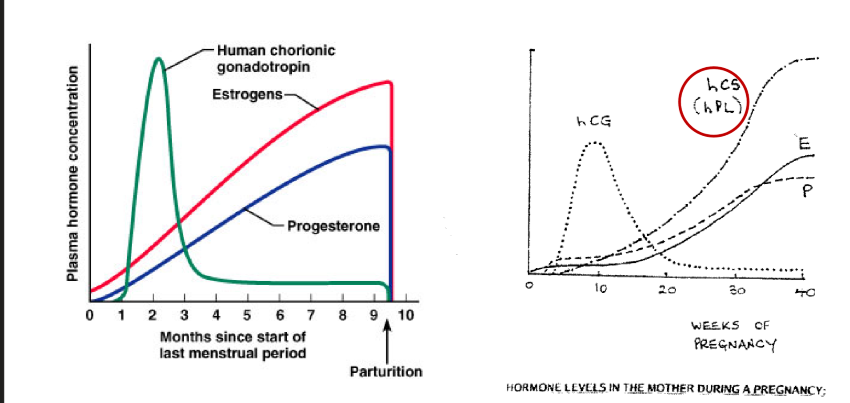
why does hCG drop off after 2.5 months
hCG is essential to maintain the corpus luteum for estrogen and progesterone secretion for first trimester, however second trimester and onward, the placenta increases estrogen and progesterone levels
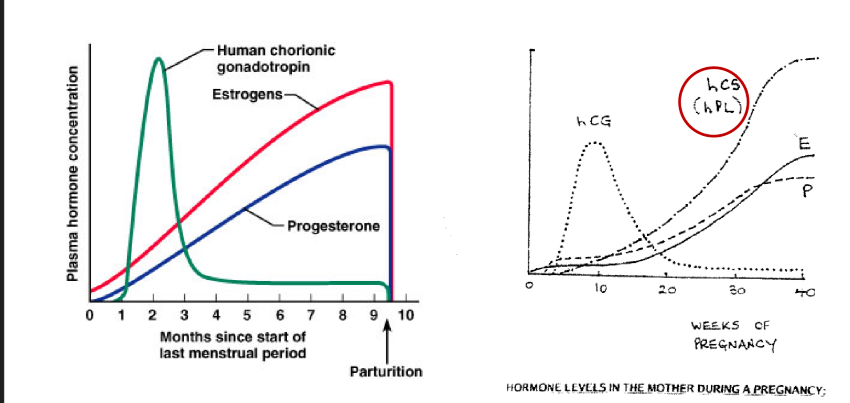
why does hPL increase over term of pregnancy
to increase glucose available for fetus
theoretically, how could you abort an embryo in the first trimester
damage/destroy the corpus luteum
Effects of estrogen and progesterone on uterus, anterior pituitary, and breasts
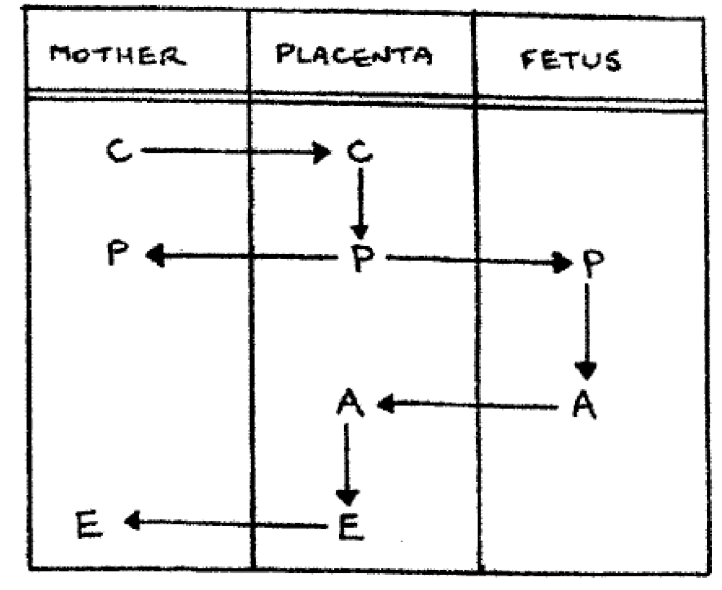
Describe the production of estrogen and progesterone by the placenta
the mother transfers cholesterol to the placenta, where it is coverted into the progesterone
the progesterone can either be given back to the mother, or:
progesterone is delivered to the fetus and converted into androgens which are then given back to the placenta
the placenta then takes the androgens and converts it to estrogen with P450 aromatase and gives it to mother
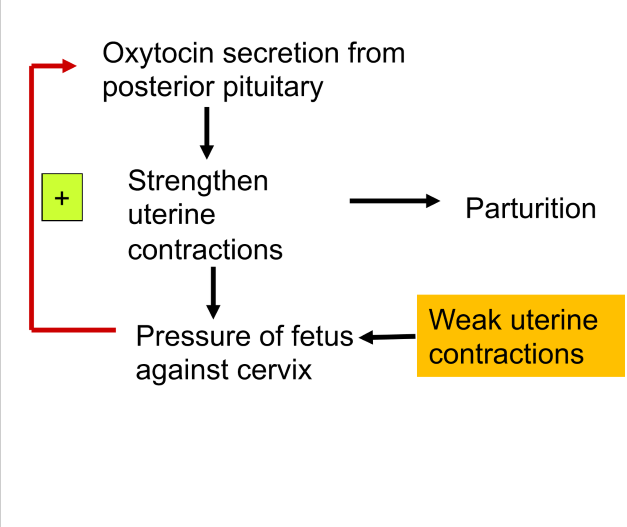
describe the positive feedback loop of parturition
oxytocin is secreted from the posterior pituitary gland which strengthends uterine contractions
pressure of the fetus against the cervix causes a positive feedback loop on to the posterior pituitary to release more oxytocin. This increased oxytocin amplifies contractions, facilitating labor and delivery.
what 4 hormones increase myometrial contractions
estrogen
oxytocin
prostaglandins
stretch
what two hormones inhibit myometrial contractions
progesterone
relaxin
what two hormones increase cervical ripening
prostaglandins
relaxin
what hormone inhibits cervical ripening
progesterone
what are the two sources of relaxin in a human
corpus luteum
placenta
What other organ does relaxin act on, and what does it do?
Relaxin will also work on the kidneys to reduce eGFR increase renal vasodilation to reduce workload of mother as she is filtering blood for both herself and baby
4 steps of partuition
end of pregnancy
cervix ripens
beginning of partuition
cervix dilates and labor is induced
birth
baby’s head wedges cervix open and his born head first
afterbirth
expulsion of placenta
what is afterbirth
The expulsion of the placenta following the birth of the baby. This process occurs after delivery and is crucial for maternal recovery.
what do the mammary glands look like from birth to puberty
ruidmentary ducts with very few alveoli
what does estrogen do to the mammary glands at puberty
causes ducts to grow and branch out
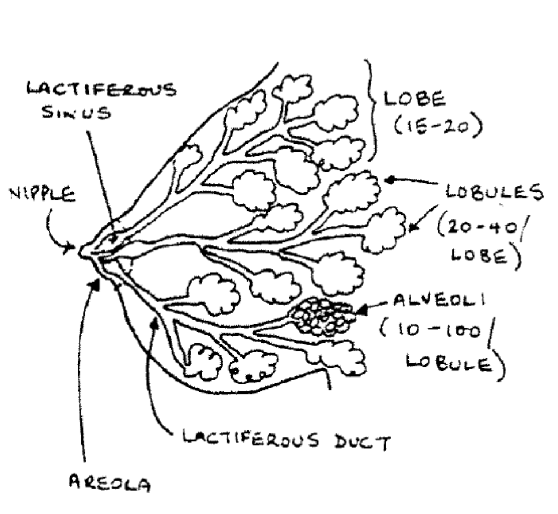
what does progesterone do to mammary glands at puberty
causes alveoli to develop and mature
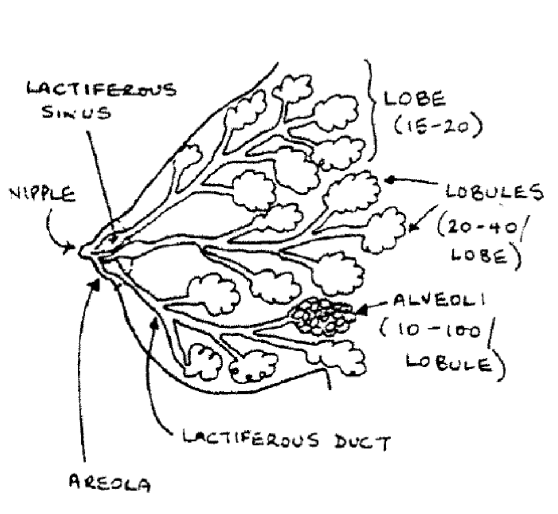
what else occurs to mammary glands in puberty, not controlled by hormone regulation
deposition of fat and alveolar tissue
what does prolactin do to mammary glands during pregnancy
lactogenesis: initiation of milk synthesis
low E and P
what does oxytocin do to mammary glands during pregnancy
required for milk ejection
what hormone is needed for galactopoesis (maintenance of lactation)
prolactin
Describe how milk is released from the mammary gland
Milk release is stimulated by oxytocin, which contracts the myoepithelial cells surrounding the mammary glands, pushing milk into the ducts and out of the nipple for breastfeeding.
the milk itself is made by the alveolar cells
myoepithelial cells contract to push milk out of gland
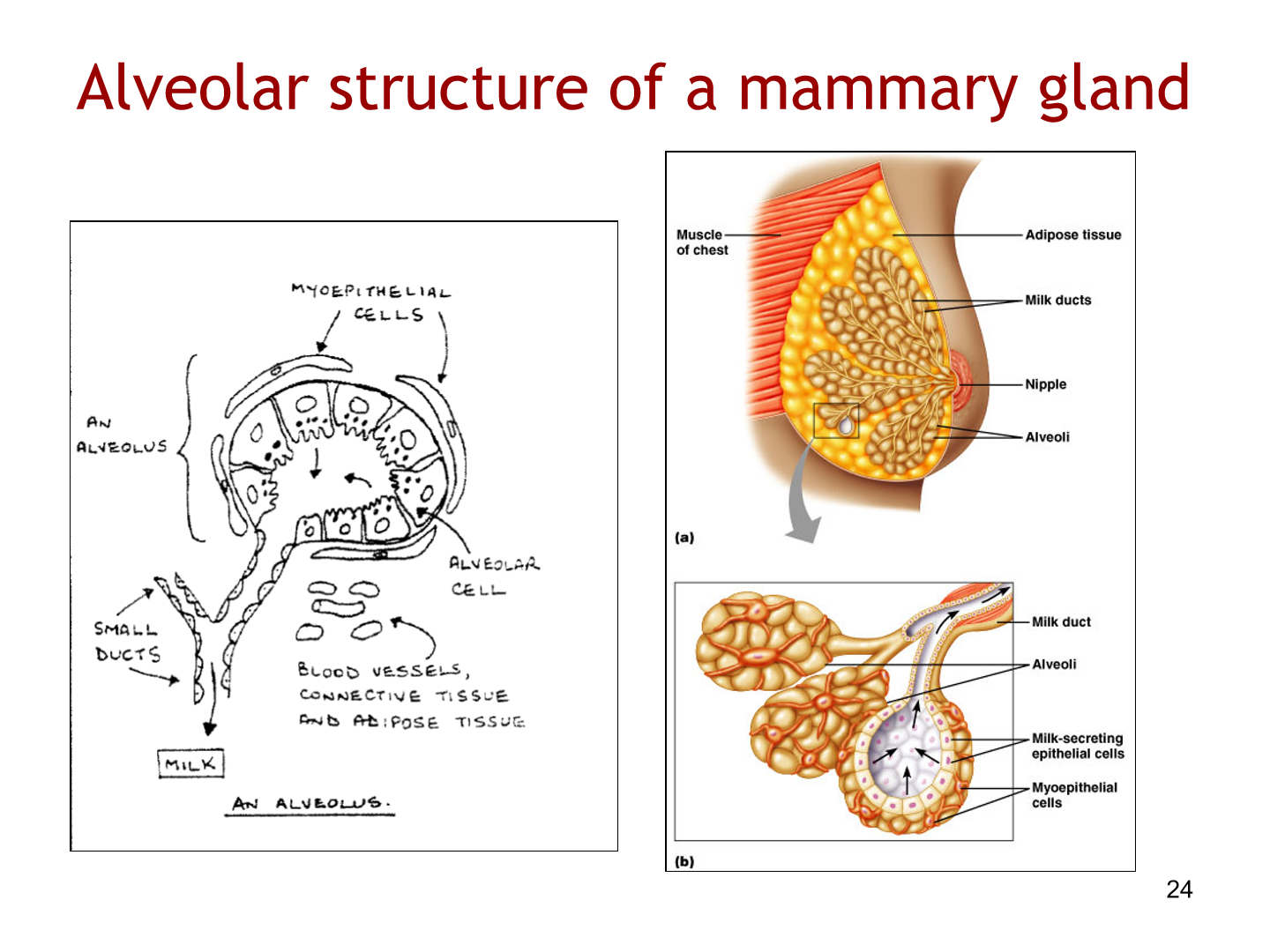
what type of secretions are milk?
apocrine secretions: partial loss of apical cytoplasm
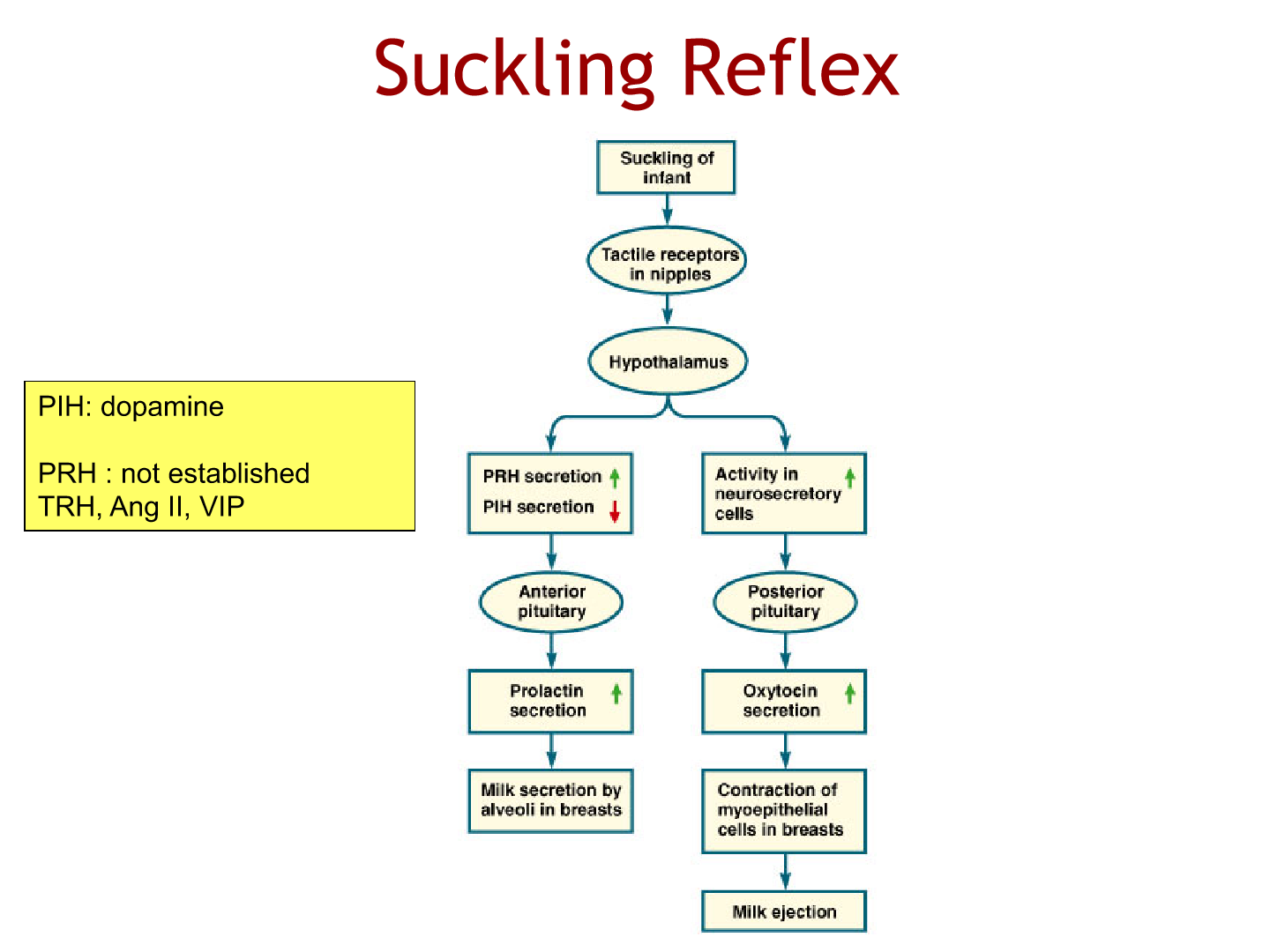
describe the suckling reflex
tactile receptors of nipples stimulate the hypothalamus to decrease dopamine in the anterior pituitary to secrete prolactin to cause milk secretion
dopamine = prolactin inhibiting hormone
thyroid releasing hormone, ANG II may help prolactin secretion (but we don’t know)
hypothalamus also increases neurosecretory cells in posterior pituitary to increase oxytocin to cause milk ejection