Renal L3 - Mechanisms which control glomerular filtration rate
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
Autoregulation
Mechanisms within the kidney act to ensure that GFR remains relatively constant when blood pressure changes
what does Autoregulation of GFR involve?
Controlled regulation of GFR usually involves changes in glomerular capillary pressure.
An increase in glomerular capillary pressure will increase GFR (assuming no other alterations) if there was no autoregulation.
GFR is highly autoregulated; GFR remains relatively constant over a wide range of mean arterial pressures.
Why is the autoregulation of GFR so important? Consider what determines GFR, as well as the consequences if GFR is perturbed.
Mean arterial pressure is a critical determinant of GFR; many daily activities change mean arterial pressure (eg exercise).
Autoregulation of GFR avoids imbalances in fluid, electrolyte and waste excretion due to changes in mean arterial pressure
Autoregulation of GFR also prevents damage to the filtration barriers by high blood pressures.
How else can Gloemerular capillary pressure be altered?
Glomerular capillary pressure can also be altered by the resistance of afferent and efferent arterioles
What mechanisms contribute to auto regulation
Mechanisms contributing to autoregulation include the myogenic mechanism and tubuloglomerular feedback
Explain Vasoconstriction
of afferent arterioles decreases blood flow into the glomeruli, thereby reducing glomerular capillary pressure and GFR, while vasoconstriction of efferent arterioles increases pressure in the glomeruli, potentially increasing GFR.
Explain Vasodilation
of afferent arterioles increases blood flow into the glomeruli, thereby raising glomerular capillary pressure and GFR, while vasodilation of efferent arterioles decreases pressure in the glomeruli, potentially reducing GFR.
Explain Myogenic mechanism
Myogenic tone is a property of arteriolar smooth muscle; it involves contraction of the muscle in response to stretch.
Thus, an increase in MAP will reduce the diameter of the afferent arteriole and limit the increase in glomerular capillary pressure.
what would happen if there was no auto regulation then ?
increase in blood pressure →
Increase in glomerular capillary pressure →
Increase in GFR
However with auto regulation?
increase in blood pressure → Myogenic response: Reduction in afferent arteriolar diameter → keeps glomerular capillary pressure constant → No change in GFR
What is the macula densa?
A collection of specialized epithelial cells in the distal convoluted tubule that detect sodium (NaCl) concentration in the tubular fluid.
How does an increase in GFR affect the macula densa?
It increases the amount of NaCl reaching the macula densa cells.
What happens when the macula densa senses increased NaCl?
It sends a signal to the afferent arteriole to constrict, which reduces GFR.
What is the feedback loop involving the macula densa called?
Tubuloglomerular feedback. This mechanism enables the kidneys to regulate GFR by adjusting the diameter of the afferent arteriole based on sodium chloride concentration.
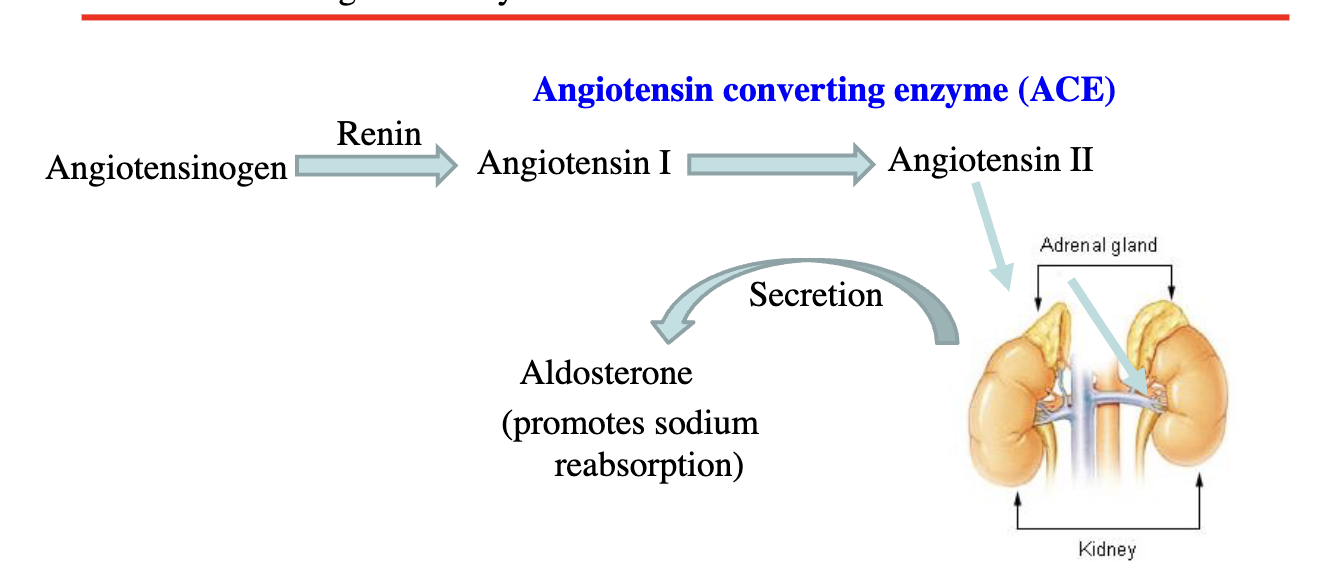
What is the role of juxtaglomerular (JG) cells?
JG cells (also called granular cells) release renin and indirectly regulate GFR via the renin-angiotensin system.
What is the overall effect of tubuloglomerular feedback?
To stabilize GFR by adjusting afferent arteriole resistance in response to changes in NaCl concentration detected by the macula densa.
Why does increased GFR lead to more NaCl at the macula densa?
Because more fluid is filtered into the tubule, carrying more NaCl past the macula densa cells.
What happens to GFR when the afferent arteriole constricts?
GFR decreases due to reduced blood flow to the glomerulus, leading to lower filtration pressure.
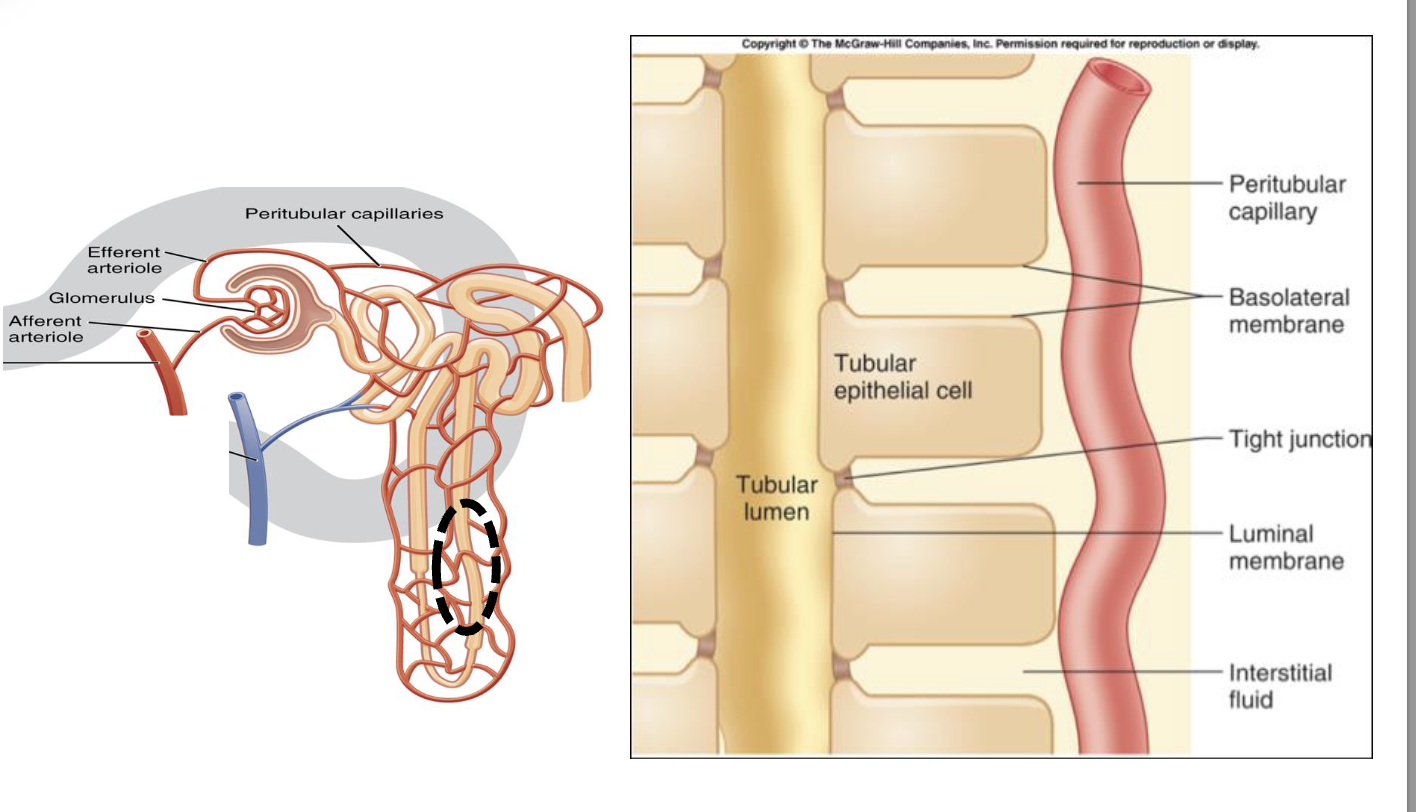
Tubular lumen and interstitial fluid - terminology
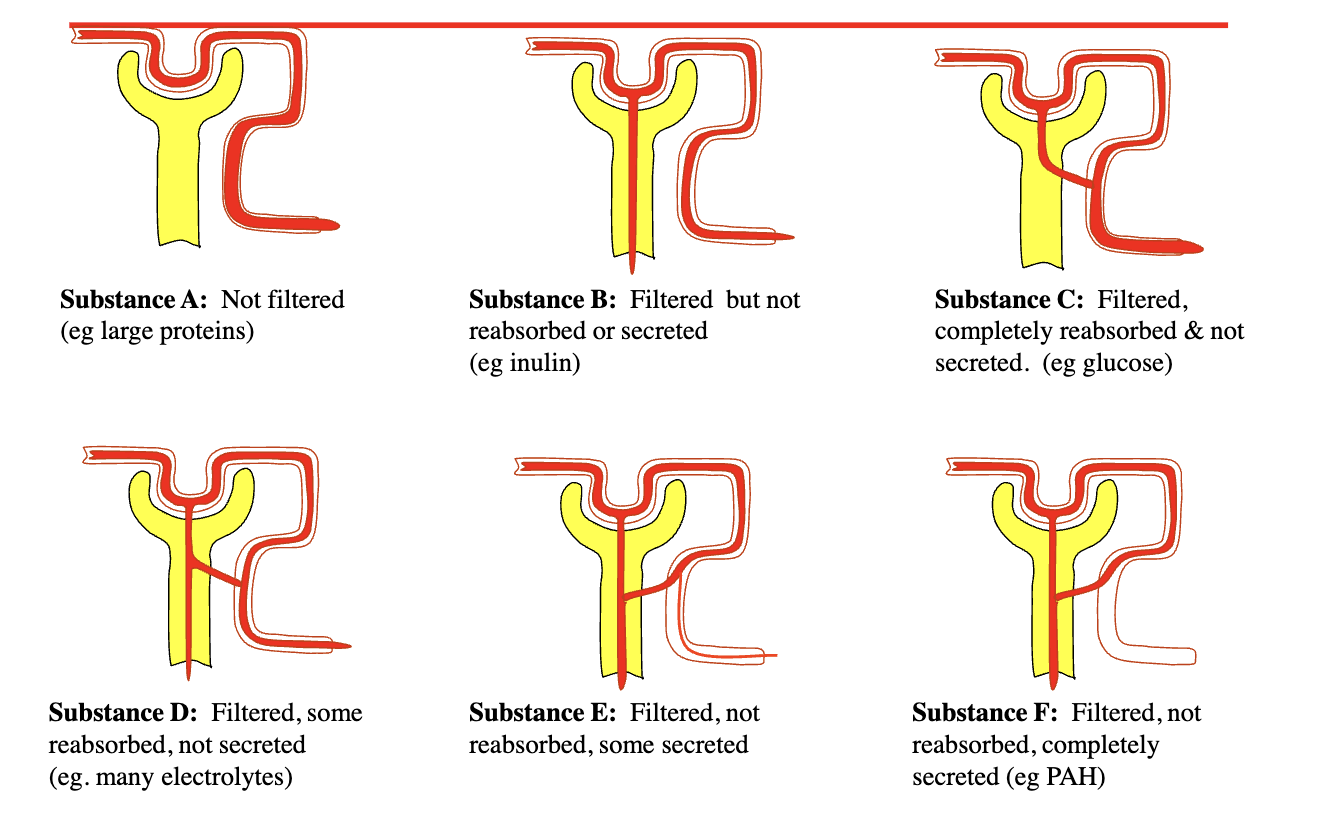
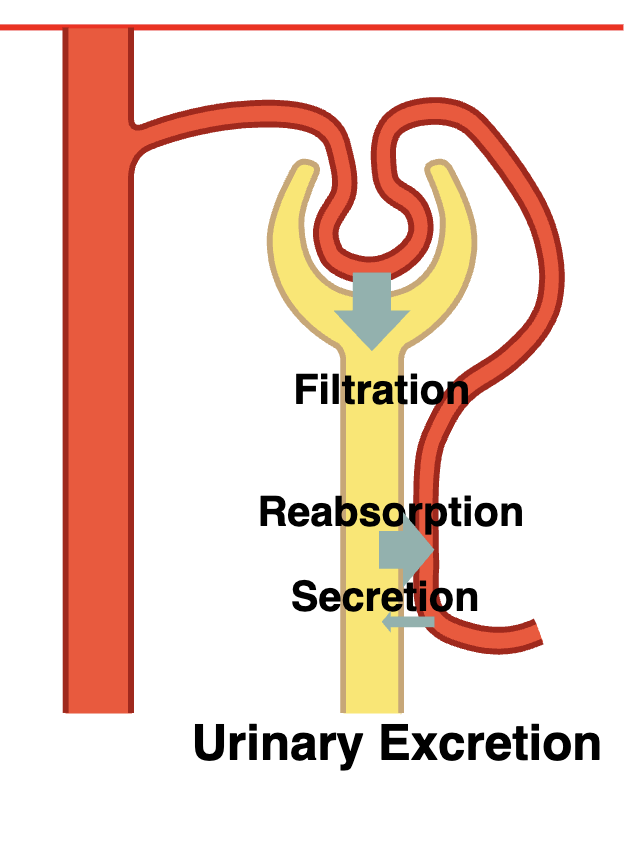
describe Glomerular filtration
the movement of fluid and solutes from the glomerular capillaries into Bowman’s space.
Describe Tubular reabsorption
– the movement of materials from the filtrate in the tubules into the peritubular capillaries.
– Taking fluid back into the body!
Describe Tubular secretion
the movement of solutes from the peritubular capillaries into the tubules
Removing fluid from the body
How does urinary excretion work through the nephron
How is reabsorption selective ?
some substances almost completely reabsorbed
many ions highly reabsorbed
Waste products poorly reabsorbed
Descending Limb Permeability?
Impermeable to sodium
Permeable to water
Ascending Limb Permeability?
Permeable to sodium
Impermeable to water
Where is sodium reabsorbed
Proximal tubules – 64%
Loop of Henle – 28%
Descending - impermeable
Ascending- Active transport
Distal tubule & Collecting Duct – 7%
Fine control
aldosterone
Excreted – 1%
Where is water reabsorbed?
Water follows sodium so more sodium means more water will enter that compartment
Proximal tubules - 67%
Osmosis
Loop of Henle – 10%
Descending- osmosis
Ascending- impermeable
Distal tubule & Collecting Duct – 9%
Fine control ADH (Anti-diuretic hormone)
Excreted – <1%
Explain the Renin Angiotensin Aldosterone System
How does water move from the hypo-osmotic compartment (less sodium) into the hyperosmotic (more sodium) compartment

Describe Vasopressin
antidiuretic hormone
Vasopressin (another name antidiuretic hormone (ADH)) increases the tubular permeability in the collecting duct.
Thus, the presence or the absence of vasopressin can influence the osmolarity of urine.
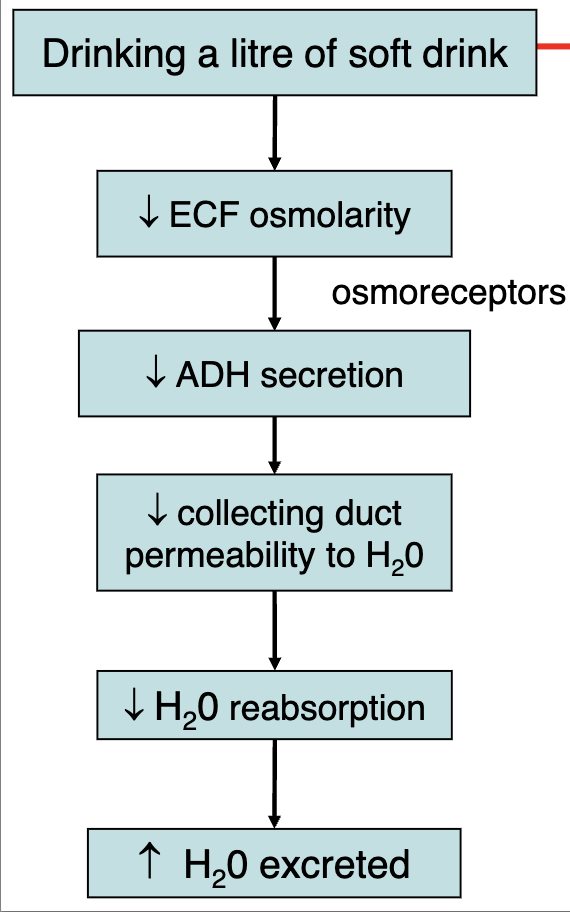
What is the pathway by which ADH secretion is lowered upon drinking a litre of soft drink and water excretion raised
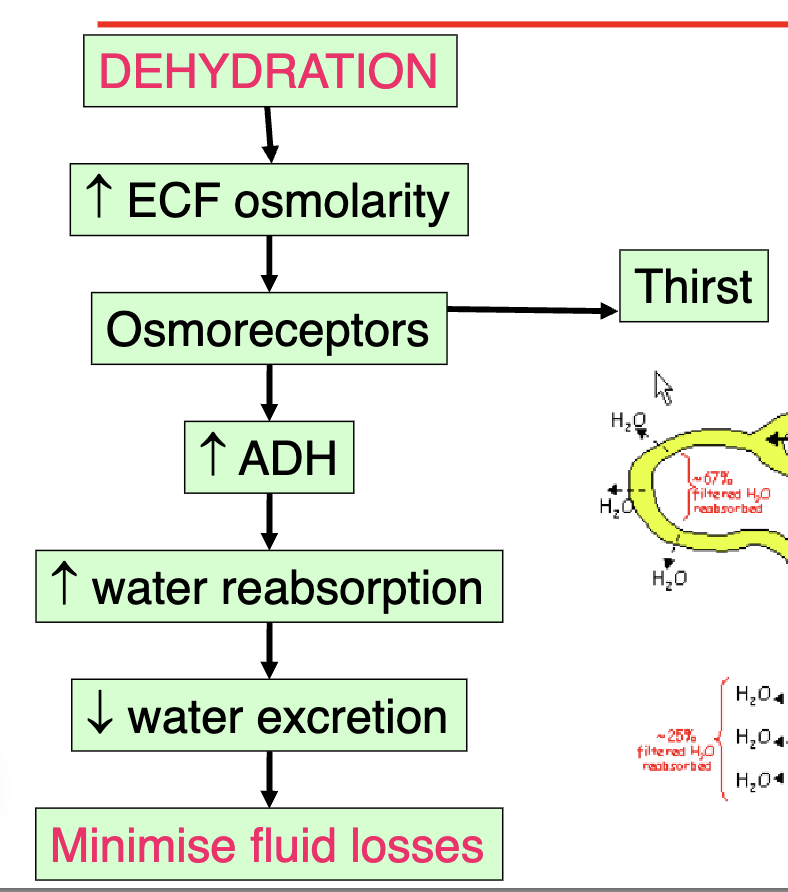
Whats the problem and solution for Dehydration ?
Problem
No water intake
sweating
Remember the kidney must make some urine.
1200 mOsm/l maximum concentrating ability of the kidney
Solution
retain sodium and water to minimise ECF osmolarity and volume loss
intake fluid
What is the bodies response to dehydration
What is Transport Maximum (Tm)?
The maximum rate at which a substance can be actively reabsorbed or secreted by the kidneys (measured in mg/min), due to saturation of carrier proteins1568
What causes the transport maximum (Tm) to be reached?
Saturation of all available carrier proteins for that substance156
What happens when the filtered load of a substance exceeds its Tm?
The excess amount cannot be reabsorbed (or secreted) and is excreted in the urine
Give an example of a substance with a well-known Tm in the kidney.
Glucose, About 320 mg/min (varies slightly by source; some list 375 mg/min for healthy adults
What is the normal filtered load of glucose?
About 125 mg/min
Is glucose normally found in the urine? Why or why not?
No, because the normal filtered load is well below the Tm, so all glucose is reabsorbed16
Why does glucose appear in the urine of patients with uncontrolled diabetes mellitus?
Their filtered load of glucose exceeds the Tm, so not all glucose can be reabsorbed, resulting in glucose in the urine (glycosuria
What is the renal threshold for glucose?
The plasma concentration at which glucose first begins to appear in the urine, typically around 180 mg/dL
What is the difference between Tm and renal threshold?
Tm is the maximum rate of transport (mg/min), while renal threshold is the plasma concentration at which a substance starts to appear in urine
What is secretion important for
secretion Transport processes similar to tubular reabsorption but in reverse direction
Important for
Disposing of substances not in filtrate such as drugs (penicillin)
Eliminating undesirable substances that have been reabsorbed by passive processes such as urea
Ridding body of excessive K+
Controlling blood pH
For each substance in plasma, a particular combination of filtration, reabsorption & secretion occurs.