OSCE Preparation
1/343
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
344 Terms
How to assess peri-implant tissues
- Visually assess the soft tissue health and the presence or absence of inflammation around the implant
- Gentle probing pressure with a plastic probe
- Measure and record peri-implant probing depths, at 4-6 sites around the implant where possible, using fixed landmarks (BPE is NOT appropriate for the assessment of implants)
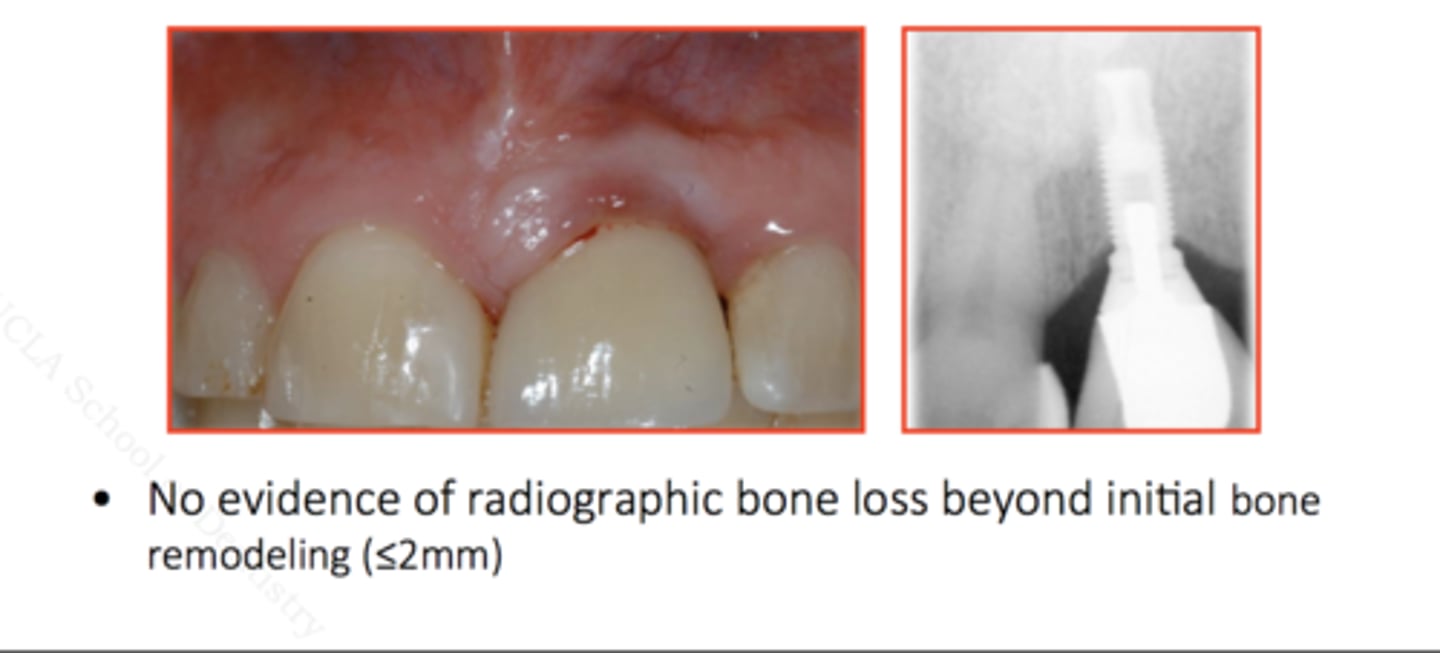
Peri-implant tissues: early signs of failure
- Marked increase in probing depth from baseline fixed points
- Bleeding on probing and/or suppuration
- Excess residual cement
- Submucosal plaque and calculus deposits
- If progressive bone loss is present, diagnosis of peri-implantitis can be made
Peri-Implantitis
- Infection with suppuration and inflammation of the soft tissues surrounding an implant, with clinically significant loss of peri-implant crestal bone after the adaptive phase
- Tissues will appear red and swollen, bleed on gentle palpation or probing, with suppuration
- May be an increase in probing depth around the implant and the implant threads may be detectable
- Recession of the surrounding mucosa can occur, exposing the threads
- May also experience pain around the implant (usually only occurs during episodes of acute infection)

Peri-implantitis treatment (SDCEP)
1. Radiographic examination of the implant using peri-apical radiographs to evaluate peri-implant bone levels compared
with the baseline radiograph; If clinically significant progressing crestal bone loss is detected, refer back to the clinician, who placed the implant. If this is not possible, carry out the following treatment:
2. Use the Oral Hygiene TIPPS behaviour change strategy to highlight the importance of effective plaque removal and to show the patient how he/she can achieve this. Encourage the use of oral hygiene aids such as implant floss and interdental brushes. Where applicable, give smoking cessation advice
3. Remove supra-mucosal and sub-mucosal plaque and calculus using an appropriate method. Remove sub-mucosal excess residual cement if this is detected. LA may be required. Highlight to the patient the areas where supra-mucosal deposits are detected.
4. Arrange a follow-up appointment after 1-2 months to assess the outcome of treatment. Re-examine the peri-implant tissues. Where there is no improvement or in the presence of
acute pain and infection, seek advice from secondary care. If the inflammation has settled and a stable situation has been achieved, arrange radiographic follow-up in 6-12 months

In patients with peri-implantitis, is there evidence to support a specific intervention to recover soft tissue health?
- There is currently very little evidence on which to base a recommendation for the treatment of peri-implantitis
- However, there is no evidence that currently used treatment regimes are ineffective. These may include oral hygiene demonstration and professional instrumentation.
- The guidance development group recommends that patients with suspected peri-implantitis should ideally be referred back to the clinician who placed the implant.
- If this is not possible, the guidance development group recommends supra-mucosal debridement and sub-mucosal instrumentation of the implant surface plus the Oral Hygiene TIPPS behaviour change strategy to address inadequate oral hygiene.
- The condition should be monitored by the primary care dentist and if no improvement is observed then secondary care should be consulted for advice.
Peri-Implant Mucositis (implant gingivitis)
- Inflammation of the peri-implant mucosa with no evidence of
progressing crestal bone loss
- Plaque-induced gingivitis with oedema
- Tissues will appear red and swollen and may bleed on gentle
palpation or probing; suppuration may also be visible
- Probing depths of 4mm or greater
Peri-Implant Mucositis treatment (SDCEP)
- Current evidence regarding the most effective interventions to recover soft tissue health in patients with peri-implant mucositis is inconclusive. However, the removal of plaque and
calculus deposits and the re-establishment of effective personal oral hygiene are likely to be important elements of effective treatment
1. Exclude the presence of peri-implantitis by carrying out peri-apical radiographs to assess peri-implant bone levels compared with the baseline radiograph
2. Use the Oral Hygiene TIPPS behaviour change strategy to highlight the importance of effective plaque removal and to show the patient how they can achieve this. Encourage the use of oral hygiene aids such as implant floss and interdental brushes. Where applicable, give smoking cessation advice
3. Remove supra-mucosal and sub-mucosal plaque and calculus deposits using an appropriate
method. Remove sub-mucosal excess residual cement if this is detected. LA may be required. Highlight to the patient the areas where supra-mucosal deposits are detected.
4. Re-assess at a future visit to ensure that the inflammation has settled and a stable situation has been achieved.

In patients with peri-implant mucositis, is there evidence to support a specific
intervention to recover soft tissue health?
- Currently very little evidence on which to base a recommendation for the treatment of peri-implant mucositis. However, there is no evidence that self-performed oral hygiene measures plus professional instrumentation to remove plaque and calculus deposits do not improve the health of peri-implant soft tissues
- The guidance development group recommends supra-mucosal debridement and unscrewing of the abutment for cleaning or, if this is not possible, sub-mucosal instrumentation of the abutment surface
- The Oral Hygiene TIPPS behaviour change strategy should be used to address inadequate oral hygiene
- The guidance development group do not recommend the use of mouthwash or irrigation to treat peri-implant mucositis
Oral hygienes TIPPS (SDCEP)
- Talk with the patient about the causes of periodontal disease and discuss any barriers to effective plaque removal
- Instruct the patient on the best ways to perform effective plaque removal
- Ask the patient to practise cleaning his/her teeth and to use the interdental cleaning aids whilst in the dental surgery
- Put in place a plan which specifies how the patient will incorporate oral hygiene into daily life
- Provide support to the patient by following up at subsequent visits
Oral hygienes TIPPS (SDCEP): talk
- Talk with the patient about the causes of periodontal
disease and why good oral hygiene is important
- Use of a visual aid may help patients understand the disease process and the effects of plaque on the periodontal tissues
- Brush regularly using an effective technique.
- Brushing twice a day for at least 2 minutes will ensure that all tooth surfaces are adequately cleaned
- Both manual and rechargeable powered toothbrushes are effective for plaque removal when used correctly
- Manual and rechargeable powered toothbrush heads should be small and of a medium texture and should be changed when obvious signs of wear appear
- Use a fluoride-containing toothpaste and 'spit don't rinse'
- Evidence suggests that fluoride toothpastes which also contain triclosan and a copolymer are more effective at reducing plaque and gingivitis indices but the clinical
relevance of these reductions is unclear
- Clean interdentally once a day
- To be effective, the brush should fit snugly into the interdental space without the wire rubbing against the tooth.
Oral hygienes TIPPS (SDCEP): instruct
- Instruct the patient in the use of the oral hygiene tools
- Demonstrate, in the patient's mouth while he/she holds a mirror, how to systematically clean each tooth using a toothbrush (manual or rechargeable powered) as well as how to use floss and/or interdental brushes. If appropriate, advise the patient to wear their glasses while cleaning their teeth
- Confirm that the patient knows what to do. If they do not, show the patient again.
Oral hygienes TIPPS (SDCEP): plan
- Help the patient plan how to make effective plaque removal a habit.
- Ask the patient when would be the best time
for them to brush and clean interdentally
- Suggest using another regular activity as a reminder such as immediately before going to bed and after getting up
- To act as an incentive for the patient, tell them that you will ask at the next visit, for example: "Have you tried using interdental cleaning aids?", "How did your action plan work?"
Oral hygienes TIPPS (SDCEP): practise
- Ask the patient to practise i.e. to clean their teeth in front of you.
- Correct the patient's technique if required and ensure that the patient has really understood what they need to do
- Confirming that the patient is doing the task well will boost confidence and also help them to remember when at home
- Ask the patient for some feedback: how their teeth feel, as clean teeth should feel smooth to the tongue
- Address any concerns the patient has if there is bleeding after brushing or interdental cleaning: gums may bleed more than normal in the first few days of using the correct oral hygiene technique and in patients who have recently stopped smoking
Oral hygienes TIPPS (SDCEP): support
Ensure you support the patient to achieve effective plaque removal by following-up on the advice at subsequent appointments
Periodontitis Classification and Diagnosis
Stage: interproximal bone loss at worst site (periodontitis related)
- Stage 1: <15% or <2mm attachment loss from CEJ – early, mild
- Stage 2: coronal third of root - moderate
- Stage 3: mid third of root - severe
- Stage 4: apical third of root – very severe
Grade: bone loss to age ratio
- Grade A: <0.5, slow rate of progression
- Grade B: 0.5 – 1.0, moderate rate progression
- Grade C: >1.0 rapid rate of progression
Extent: bone loss distribution
- Localised (<30% of teeth)
- Generalised (>30% of teeth)
- Molar/incisor pattern
Stability
- Stable: Pockets ≤ 4mm, BoP <10%, No BoP at 4mm sites
- In remission: Pockets ≤ 4mm, BoP >10%, No BoP at 4mm sites
- Unstable: pockets ≥ 4mm with BoP, BoP present at 4mm sites
or greater
Risk factors
- Smoking (cigarettes/day)
- Diabetes (optimal or suboptimal control, HbA1c levels)
Gingivitis classification and diagnosis
- Code 0,1,2 with no obvious evidence of interdental recession
- Clinical gingival health: <10% BOP
- Localised gingivitis: 10-30% BOP
- Generalised gingivitis: >30% BOP
Symptoms of Reversible Pulpitis
- Pain provoked by stimulus e.g. cold, sweet
- Pain relieved when stimulus removed
- Intermittent pain that doesn't disturb sleep
- Vital pulp
- Not TTP
Aims of treating reversible pulpitis
- Remove pain
- Prevent disease progression to irreversible pulpitis
Reversible pulpitis treatment: primary teeth
- Hall technique PMC: if occlusal, selective caries removal avoiding pulp then restore with composite, RMGIC, GIC, or compomer
- Pulpotomy if radiograph shows no clear separation between the carious lesion and pulp
- If tooth close to exfoliation, consider dressing
Reversible pulpitis treatment: primary teeth
- What to do if there are symptoms of pain that may be due to food packing or pulpitis with reversible symptoms but diagnosis is uncertain
- Place temporary dressing into cavity
- Review 3-7 days later to check symptoms
- Resolution of symptoms at review will indicate that the pulpitis was reversible; Hall crown or suitable restoration can be place
- If symptoms do not resolve or worsen, extraction or pulpotomy indicated
Symptoms of Irreversible Pulpitis
- Pain can occur spontaneously
- Pain is typically not relieved when stimulus is removed worsened by heat
- Pain relieved by cold
- May last for several hours and keep child awake at night
- Dull, throbbing
- Vital pulp although inflamed
- Not TTP
Aims of treating irreversible pulpitis
To relieve pain
Irreversible pulpitis treatment: primary teeth
- If uncooperative, gently remove gross debris from cavity and apply corticosteroid antibiotic paste under a temporary dressing; OR open pulp chamber under LA and apply corticosteroid paste directly to pulp then place dressing then prescribe pain relief then pulpotomy or extraction at later date
- If cooperative, pulpotomy or extraction
Symptoms of dental abscess/periradicular periodontitis (primary teeth)
- Pain, if present, may be spontaneous and keeps awake at night
- Pain is easily localised
- Increased mobility
- TTP
- May be clinical evidence of sinus, abscess, swelling
- May be radiographic evidence of interradicular pathology
Aims of treating dental abscess/periradicular periodontitis
- Remove source of infection
- Avoid or relieve pain
Dental abscess/periradicular periodontitis treatment: primary teeth
- If cooperative, extraction even if asymptomatic
- If restorable, consider pulpectomy which may need referral
- If uncooperative, refer to specialist
Yellow bin
Infectious waste that must be incinerated or sharps
Orange bin
Infectious waste that can be treated to render safe prior to disposal
Purple bin
Cytotoxic/cytostatic waste that must be incinerated by a licensed facility
Yellow and black bin
Offensive/hygiene waste that can be landfilled on a licensed site
Black bin
General domestic waste that may be landfilled or recycled
Grey bin
Glass, aerosol cans, food tins, and crockery
Green bin
Recyclable waste
Clinical waste
Orange bin
3 multiple choice options
Medicinal waste (pathological)
Blue bin
3 multiple choice options
Mixed municipal waste
Black bin
Offensive waste from humans with animals
Yellow bin with black stripe
3 multiple choice options
Anatomical waste
Red bin
3 multiple choice options
Amalgam waste
White bin
3 multiple choice options
How to write a referral to oral med
- Pt details
Dear Dr _____. I am writing to refer the above mentioned patient for a biopsy/assessment. The lesion in question is:
- Size
- Site
- Distribution: margins, raised, flat, slough
- Colour
- Texture: flat, smooth
- Consistency: hard/soft
- Onset
I have enclosed a copy of the patients medical history and clinical photographs related to the case.
Name
Signature
Title
When to refer - white patches
Lesion has been there for > 2 weeks
When to refer - red/white patches
Refer patient straight away
Emergency treatment on a child - parent not present
Do not delay emergency treatment that is required to save a life/prevent serious harm if authority cannot be sought from someone on a PR form
What to consider before paediatric extraction of primary first molars
Check radiograph for presence, position, normal formation of developing permanent dentition
Paediatric extraction of primary first molars: reasons
- Extensive decay that cannot be effectively treated with dental fillings or other restorative measures may necessitate extraction to prevent the spread of infection.
- Infections or abscesses around primary molars can cause pain, swelling, and risk spreading to other teeth or tissues, requiring extraction.
- Sometimes, primary molar extraction is part of orthodontic treatment plans to create space for permanent teeth or to correct bite alignment issues.
- Severe trauma or injury to a primary molar might require extraction if it cannot be adequately restored.
- Impacted or Ectopic Teeth: Teeth that are not erupting properly, are impacted, or are in abnormal positions might need to be extracted to prevent future complications.
- Deciduous Teeth Retention: In cases where primary teeth fail to exfoliate naturally and cause interference with permanent tooth eruption, extraction may be required.
- Crowding: Extraction might be recommended if there's overcrowding or lack of space for proper eruption of permanent teeth.
Paediatric extraction of primary first molars: risks
- Pain or Discomfort: The extraction site may be sore or uncomfortable for a few days after the procedure. This can typically be managed with over-the-counter pain relievers and proper oral care.
- Bleeding: Some bleeding is normal after extraction. Gauze is usually provided to control bleeding, and applying pressure helps stop the bleeding.
- Infection: There's a risk of infection at the extraction site. Following post-operative care instructions, including proper oral hygiene and avoiding certain foods, can help minimise this risk.
- Dry Socket: In rare cases, a blood clot may not properly form or may dislodge from the extraction site, leading to a condition called dry socket. This can be painful and may require additional treatment from the dentist.
- Damage to Surrounding Structures: In rare instances, neighbouring teeth, nerves, or the sinus cavity might sustain damage during the extraction process.
- Shift in Tooth Alignment: Premature loss of primary teeth can sometimes affect the alignment of permanent teeth, potentially leading to crowding or misalignment.
Who has parental responsibility?
- Birth mother
- Biological father, if married to birth mother (even if now separated or divorced)
- Father, named on birth certificate and child born/birth registered after 01/12/03
- Named as parent on birth certificate if child conceived on or after 06/04/09 via embryo transfer or artificial insemination as per the Human Fertilisation and Embryology Act 2008
- Holder of an Adoption Order
- Holder of a Parental Responsibility Agreement
- Holder of a Parental Responsibility Order
- Holder of a Residence Order
- Holder of a Child Arrangements Order with a Parental Responsibility Order
- Holder of a Special Guardianship Order
- An appointed Legal Guardian
- Holder of a Parental Order
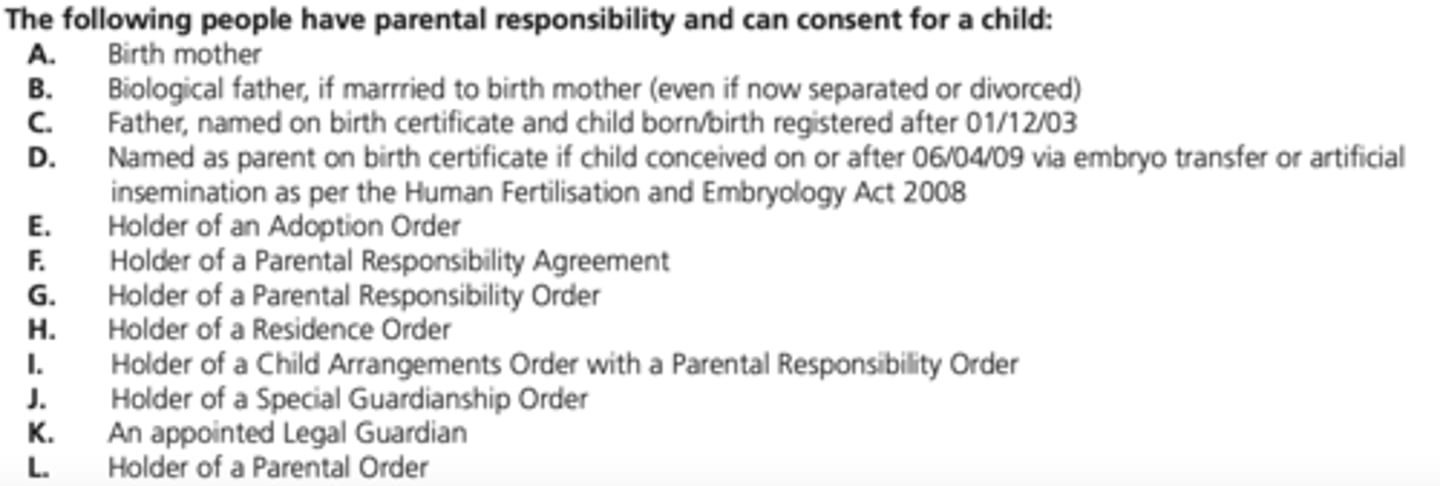
Parental responsibility
- If a child isn't Gillick competent, authority to treat can be given by someone with parental responsibility under the Children Act 1989
- If one person with parental responsibility authorises treatment, it's not usually necessary to get authority from another person with such responsibility
- In non-urgent cases where there is a dispute, it would be wise to seek a resolution that's in the child's best interests
Gillick Competence
- Children's Act 1989
- Used in medical law to decide whether a child under 16 years of age is able to consent to their own medical treatment without the need for parental permission
- Helps assess whether a child has the maturity to make their own decisions and to understand the implications of those decisions
What things do we consider when deciding if a patient is Gillick competent?
- Child's age, maturity, and mental capacity
- Understanding of the issue and what it involves
- Understanding of the risks implications and consequences
- How will they understand any advice or information they have been given
- Understanding of any alternative options
Mental Capacity Act 2005
- It is assumed that someone has capacity unless it is established that they lack capacity
- A person is not to be treated as unable to make a decision unless all practicable steps to help them have been unsuccessful
- If they make an unwise decision, they cannot just be considered to not have capacity
What legislation were the Protected Characteristics published in?
Equality Act 2010
What to do if you have a paeds patient present without someone on the PR form
- No treatment to be carried out until the presence of someone on PR form is possible
- Acclimatisation/OHI can be carried out
Benefits of tooth extraction
- Relief from Pain
- Prevention of Infection
- Orthodontic Reasons
- Preparation for Dentures
- Preventive Measures e.g. impacted wisdom teeth
Risks of tooth extraction: common
- Pain
- Bleeding: normal oozing 6-12 hours post-op; maintain pressure with good packing; look for "liver-shaped clot"; remove with suction and apply pressure until haemostasis obtained
- Swelling: usually resolves 24-36 hours post-op; swelling after 36 hours may indicate infection
- Minor trauma to anaesthetised soft tissues: self- inflicted cheek, tongue or lip biting
Pulpotomy
- Procedure: Pulpotomy involves the partial removal of the diseased or infected pulp from the crown of the tooth, specifically in cases where the decay or infection has not extended into the tooth's root canals.
- Purpose: The main goal of a pulpotomy is to remove the infected portion of the pulp while preserving the healthy portion in the root canal to maintain the tooth's vitality and function.
- Indication: It's often used in paediatric dentistry for primary teeth when decay has reached the pulp but hasn't affected the tooth's roots extensively
Risks of tooth extraction: uncommon
- Minor infection: characterised by swelling that increases or does not resolve quickly after extraction; may be accompanied by draining pus, malaise and/or fever; needs to be seen by dentist
- Dry socket: loss/ lysis or failure of clot to form; more common in mandible because of reduced blood supply; increase in acute, localised pain after 48 hrs (2-5 days); refer to dentist

Treating dry socket (as a dentist)
- Radiograph
- Anaesthesia if necessary
- Irrigate to remove debris sterile saline
pack socket with dressing material e.g. Alveogyl
- Prescribe analgesia/antibiotics (metronidazole)
Risks of tooth extraction: rare
- Root displacement
- TMJ problems / trismus
- Haematoma formation
- Osteomyelitis
- Jaw fracture
What to check when patient arrives for extraction
- Check patient accompanied by appropriate person with PR
- Check paperwork
- Check how getting home
- Check empty bladder
Post-op extraction
- Take analgesia before LA wears off- eg Calpol; maintain analgesia regularly for 24 hours after extraction
- Don't let child play with socket with their tongue
- No spitting out or rinsing
- Swallow saliva otherwise clot is disturbed.
- If bleeding occurs, help child to bite on a gauze or cotton handkerchief for 10 minutes
- Don't let socket get disturbed
- Soft foods for 14 hours
- No excessive physical exertion for the rest of the day
Pulpectomy
- Procedure: Pulpectomy involves the complete removal of the entire pulp tissue from both the crown and the roots of the tooth, essentially treating the entire root canal system.
- Purpose: This procedure is typically performed when the infection or decay has spread extensively into the root canals or when dealing with an infected permanent tooth.
- Indication: Pulpectomies are more common in permanent teeth and are performed to eliminate infection, relieve pain, and save the tooth when the pulp is irreversibly damaged.
When to do a pulpotomy?
The decay or trauma is confined to the crown of the tooth, if the patient has bleeding disorders, too young i.e. potential occlusion issues, hypodontia i.e. no permanent successor
When to do a pulpectomy?
A pulpectomy is indicated in a primary tooth with irreversible pulpitis or necrosis or a tooth treatment planned for pulpotomy in which the radicular pulp exhibits clinical signs of irreversible pulpitis (e.g. excessive haemorrhage that is not controlled with a damp cotton pellet applied for several minutes) or pulp necrosis (eg, suppuration, purulence). The roots should exhibit minimal or no resorption.
When to do selective caries removal?
- Selective removal to firm dentine is recommended for shallow or moderately deep lesions
- For deep lesions (extending close to the pulp) in teeth with vital pulps, selective removal to soft dentine is recommended to avoid pulpal exposure and to preserve the health of the pulp.
Which piece of legislation protects workers who 'blow the whistle' from being subjected to detriment?
Public interest Disclosure Act 1998
Which piece of legislation states that safeguarding is everyone's responsibility?
Places duties on organisations and individuals to make arrangements for ensuring their functions are discharged with due regard to the need to safeguard and promote the welfare of children
Children's Act 2004
How to signpost someone in making a complaint?
1. Report to practice manager via telephone/verbal/written
2. If NHS: NHS choices (in England). If private: Dental Complaints Service
3. Other organisations: The Parliamentary and Health Service Ombudsman (England)
4. GDC
Which legislation provides guidance for adult safeguarding 16+?
Care Act 2014
Who are the local safeguarding partners?
- Local authorities
- Police
- Chief commissioning groups
- Safeguarding practice lead
Independent Medical Capacity Advocate service
There is a legal duty to refer vulnerable people who may lack the capacity to make critical decisions to this service
Lasting Power of Attorney
- A means by which a person can give another person the legal power to make certain decisions for them when they lose capacity
- Must have capacity when they appoint an LPA and no-one else can appoint an LPA on their behalf
What is a provisional diagnosis?
When a definitive diagnosis can not be made, but high index of suspicion of cause
Giving OHI to children (DBOH)
- brush twice a day with a pea sized amount of fluoride toothpaste (smear for < 3 yo): 1350-1500ppm recommended, although in very young children, where the ability to control swallowing is limited, at least 1000ppm is fine
- sugar, no more than 19g in 4-6/24g in 7-10/30g in 11+
- no supervision required after 6 years old
- balanced diet following eat well plate, x5 fruit and veg daily, carbohydrates, protein, dairy, fats
- 6-8 cups of water per day
- no more than x4 sugar attacks per day
Process of safeguarding
- Ask questions relating to potential injuries; be attentive to body language and tone of voice, dentists job is to recognise and refer - nothing else.
- Record in the notes, speak to a colleague and if you still have concerns refer to the local authorities i.e. safeguarding organisation or the police
How many verifiable CPD hours to complete
- dentists need to do a minimum of 100 hours
- dental therapists, dental hygienists, orthodontic therapists and clinical dental technicians need to do 75 hours
- dental nurses and dental technicians need to do 50 hours
- temporary registrants (dentists) need to do 20 hours
Safeguarding CPD
Regular training: whole team, level 2 (minimum 3 hours), 3-yearly update)
Medical emergencies CPD
Recommended at least 10 hours in each CPD cycle, and at least two hours of this type of activity every year.
Disinfection and decontamination CPD
Recommended at least five hours in each cycle.
Radiography and radiation protection CPD
If you undertake radiography, recommended at least five hours in each cycle.
For dental technicians, recommended materials and equipment, instead of radiography and radiation protection at least five hours in each cycle.
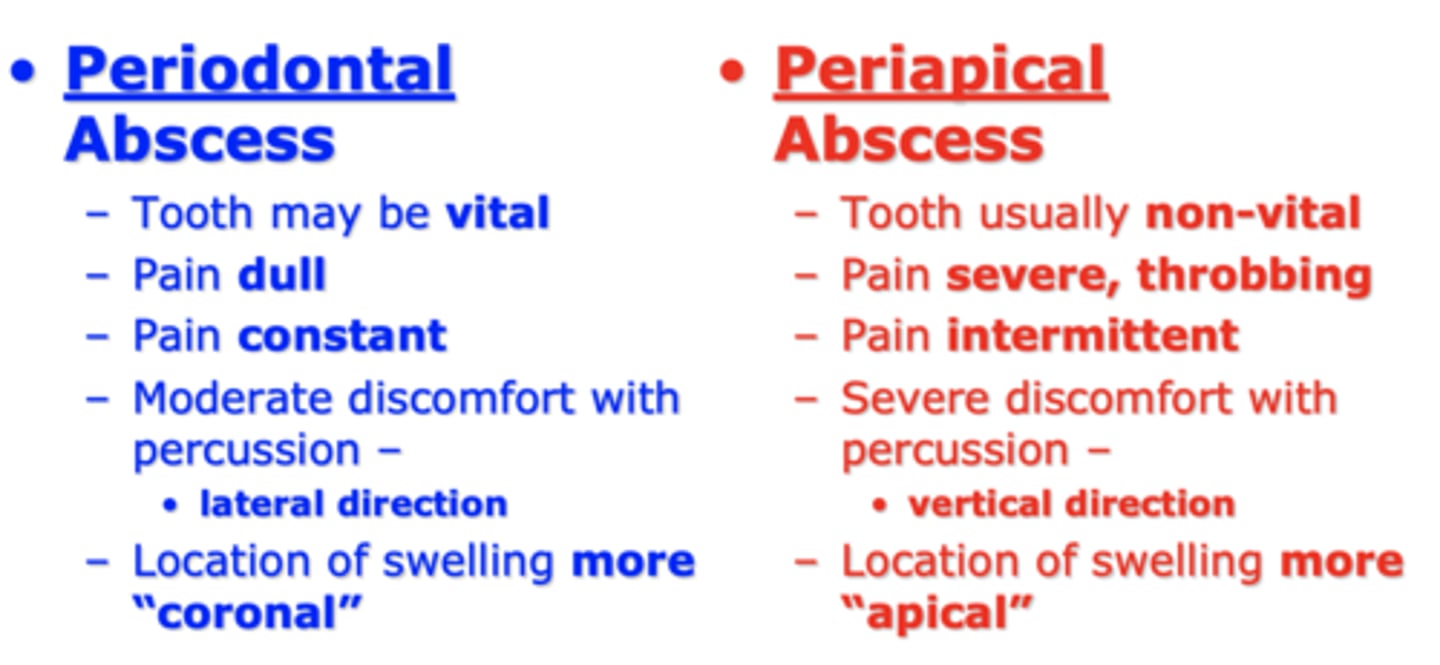
Periapical abscess
- Location: Arises at the tip of the tooth's root (apex), typically due to an infection that originates within the dental pulp (inside the tooth) and spreads to the surrounding tissues.
- Cause: Often results from untreated dental decay, deep cavities, or dental trauma that allows bacteria to enter the pulp chamber, leading to pulpitis (inflammation of the pulp) and eventual infection of the periapical area.
- Symptoms: Symptoms include severe, throbbing tooth pain, swelling, and the formation of a localised pus-filled swelling (abscess) near the affected tooth. The tooth may be sensitive to touch or pressure.
- Treatment: Treatment usually involves root canal therapy or extraction to eliminate the infected pulp and drain the abscess

Periodontal abscess
- Location: Originates in the supporting structures of the tooth, specifically the periodontal tissues (gums, periodontal ligament, and bone) rather than within the tooth itself.
- Cause: Typically occurs due to gum disease (periodontitis), where bacteria accumulate in periodontal pockets around the tooth, leading to infection, inflammation, and the formation of an abscess.
- Symptoms: Symptoms may include localised swelling, redness, pain, and tenderness in the affected gum area. Sometimes, there might be pus drainage from the gum pocket.
- Treatment: Treatment involves drainage of the abscess, deep cleaning (scaling and root planing) to remove bacterial deposits and infected tissue, and sometimes surgical intervention to access and clean the affected area.
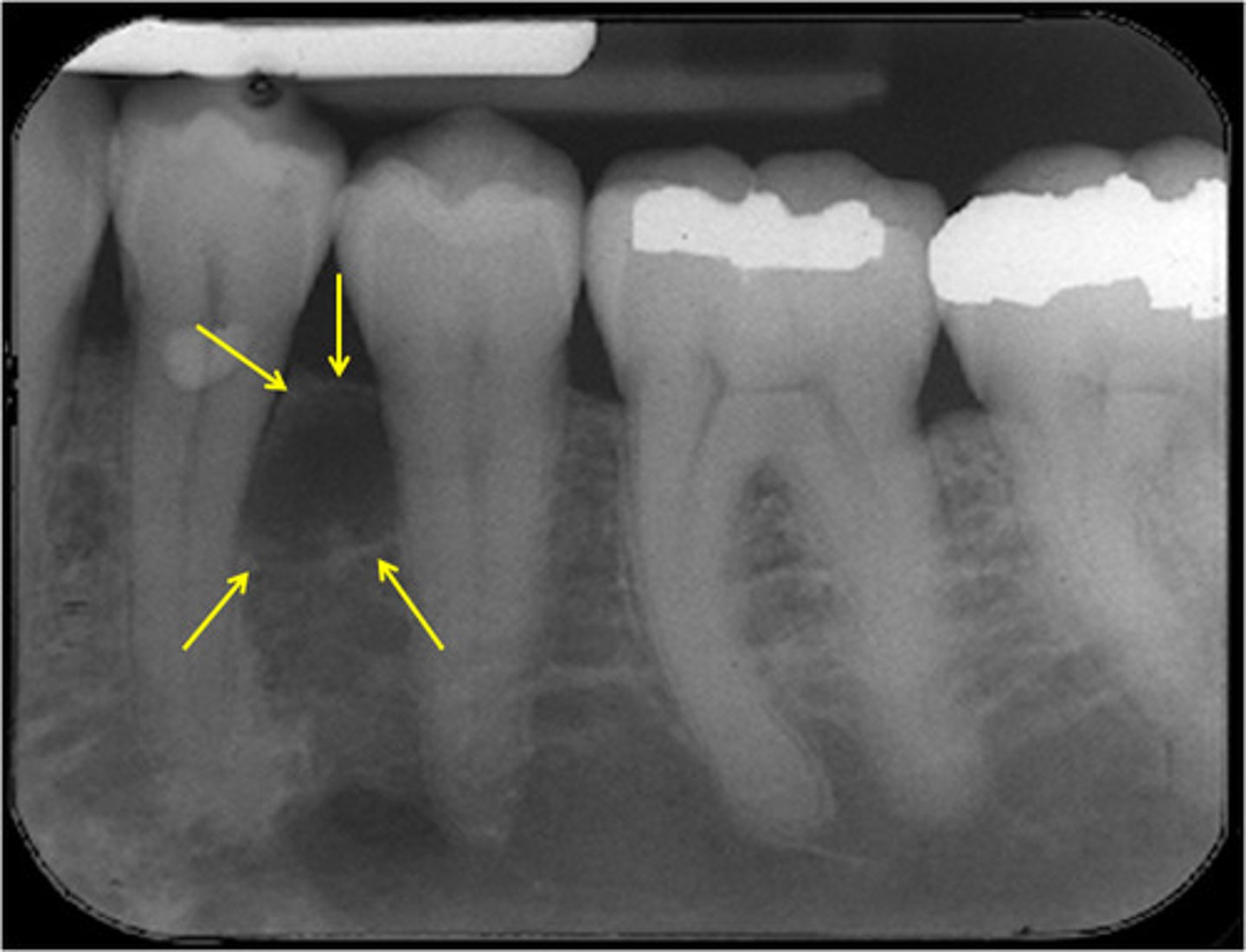
Difference between periapical and periodontal abscess
- Periapical abscesses stem from infections within the tooth pulp and occur at the tooth's root
- Periodontal abscesses originate from infections in the gums and supporting structures surrounding the tooth
Antibiotics for dental abscess
1. Amoxicillin: This is often the first choice for dental infections due to its efficacy against oral bacteria. The typical adult dose is 500 mg to 1 gram three times a day for five to seven days.
2. Clindamycin: Sometimes used as an alternative for patients allergic to penicillin or those who cannot tolerate amoxicillin. The usual adult dose is 150-300 mg every six hours for five to seven days.
3. Metronidazole: Used as an alternative in specific cases or in combination with other antibiotics. The usual adult dose is 200-400 mg three times a day for five to seven days.
Treatment options for fractured tooth
- For minor chips or fractures, dental bonding can be used. A tooth-coloured resin is applied and shaped to restore the tooth's appearance.
- A dental crown may be recommended for more significant fractures that involve a larger portion of the tooth. The crown covers the damaged tooth, restoring its shape, strength, and appearance.
- f the fracture extends into the tooth's pulp, causing pain or infection, a root canal might be needed. This involves removing the damaged pulp and sealing the tooth.
- In cases of severe fractures that cannot be restored, extraction might be necessary, followed by replacement options like dental implants, bridges, or dentures.
- For front teeth with minor fractures, veneers (thin shells of porcelain or composite) can be bonded to the tooth's front surface to improve its appearance.
- If the fractured tooth needs to be extracted, a dental implant might be considered as a replacement option. This involves placing a titanium post into the jawbone, topped with an artificial tooth.
Managing bruxism
- Mouthguard/biteguard/splint to protect the teeth from grinding during sleep. These custom-fitted oral appliances create a barrier between the upper and lower teeth, reducing the impact of grinding and preventing tooth wear.
- Since stress and anxiety often exacerbate bruxism, stress-reduction techniques like meditation, yoga, counselling, or relaxation exercises can be helpful in managing the condition.
- Cognitive-behavioral therapies (CBT) can be beneficial in addressing underlying stress or anxiety triggers associated with bruxism.
- Muscle Relaxation Exercises: Techniques such as applying moist heat to the jaw, gently massaging facial muscles, or doing jaw exercises can help relax the muscles involved in bruxism.
- Dental treatments may be necessary to correct misaligned teeth or bite issues that contribute to bruxism.
- In certain cases, muscle relaxants or medications to manage stress or anxiety might be prescribed by a healthcare professional to alleviate bruxism symptoms.
- Lifestyle Changes: Avoiding or reducing caffeine intake, alcohol consumption, and tobacco use might help alleviate symptoms.
Non-pharmacological behavioural techniques
- Preparatory information
- Non-verbal communication
- Verbal communication
- Voice control
- Enhancing control
- Tell-show-do
- Positive reinforcement
- Behaviour shaping
- Modelling
- Distraction
- Systematic desensitisation
- Cognitive Behavioural Therapy
SOP of dentist, not of therapist
- diagnose disease
- prepare comprehensive treatment plans
- prescribe and provide endodontic treatment on adult teeth
- prescribe and provide fixed orthodontic treatment
- prescribe and provide fixed and removable prostheses
- carry out oral surgery
- carry out periodontal surgery
- extract permanent teeth
- prescribe and provide crowns and bridges
- provide conscious sedation
- carry out treatment on patients who are under general anaesthesia
- prescribe medicines as part of dental
treatment
- prescribe and interpret radiographs
Additional skills which a dentist could
develop:
- providing implants
- providing non-surgical cosmetic
injectables
Treatments therapists can deliver under prescription of a dentist
- Tooth whitening
- Inhalation sedation
- Non-surgical cosmetic injectables
Safeguarding: dental neglect
- Willful failure of parent or guardian to seek and follow through with treatment necessary to ensure a level of oral health essential for adequate function and freedom from pain and infection
- Poor oral hygiene
- Halitosis
- Early Childhood Caries (ECC)
- Odontogenic infections: recurrent and previous abscesses
- Periodontal disease
- Aptha lesions because of a nutritional deficiency status
Signs of neglect in adults
- Patient disclosure
- Patient has an unkempt appearance
- Medication not administered
- Inappropriate clothing
- Personal care not been carried out
- Soiled clothing
- Malnourished
- Dehydrated
- Persistent infection
- Not taken to healthcare appointment (regular occurrence)
Safeguarding: attending with 16 year old sibling
inappropriate caring responsibility
How to raise safeguarding issue
- Inform tutor of concerns appropriately
- Documentation of facts in a contemporaneous way; if disclosure, then important that patient's own words used where possible
- Speak to parents
- Raise concern with safeguarding team: ICE and telephone call
- Completion of Datix
- Logbook for safeguarding incidents
- Debrief
Main categories of abuse
- Physical
- Emotional
- Sexual
- Neglect
How can we recognise abuse?
- Difficult relationships
- Non-accidental injury
- Change in behaviour: clingy, withdrawn, anxious
- Inappropriate behaviours with others
- Dirty clothing/equipment
- Non-attendance at appointments
What are some oral signs of physical abuse that you might notice in the individuals attending a dental practice?
- Damage to the mouth such as burnt, bruised, or cut lips
- Torn or bruised skin where the upper lip joins the mouth
- Fractured incisors
- Injuries at different stages of healing
- Object marks, clear outlines of objects
What are some oral and facial signs of domestic violence that you might notice in the individuals attending a dental practice?
- Facial or intraoral bruising or laceration
- Teeth lost due to trauma
- Fractures to nose, cheek, or jaw
- Torn frenum
- Bite marks
- Hair loss
What are some oral signs of neglect that you might notice in the individuals attending a dental practice?
- Poor oral hygiene
- Halitosis
- Early Childhood Caries (ECC)
- Odontogenic infections: recurrent and previous abscesses
- Periodontal disease
- Aptha lesions because of a nutritional deficiency status
What is the triangle of safety?
- Extraoral areas where accidental injuries are unusual
- Ears, side of face, neck, and top of shoulders
Safeguarding in practice
- Safeguarding policy: made aware of at induction
- Named safeguarding lead
- Regular training: whole team, level 2 (minimum 3 hours), 3-yearly update)