Exam 3 study guide
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
What are the types of neurons?
Motor Neurons (Efferent)
Sensory Neurons (Afferent)
Interneurons
Motor Neurons (Efferent)
Takes nerve impulses from the CNS to the muscles or glands
Multipolar because they have many dendrites and a single axon
They cause muscle fibers to contract or glands to secrete
Sensory Neurons (Afferent)
Neurons take nerve impulses form sensory receptors to the CNS
Unipolar
The sensory receptor is as simple as a naked nerve ending ( a pain receptor), or it may be a part of a highly complex organ, such as the eye or ear
Interneurons
Association neurons, occur entirely within the CNS
Multipolar, they convey nerve impulses between various parts of the CNS
Some lie between sensory neurons and motor neurons, and some take messages from one side of the spinal cord to the other or from the brrain to the cord, and vice versa
What are synapses?
Junction between the dendrites of one neuron and the axon of a second neuron
Nerves communicate by releasing chemical messenger at synapse
Important neurotransmitters:
Monoamines
Neuropeptides
Nitric oxide
Resting membrane potential:
Sodium in greater concentration outside
Potassium in greater concentration inside
Anions in greater concentration inside
Membrane permeability greater for potassium than sodium
Na+/K+ pump moves sodium out, potassium in
Utilizes ATP
Generating action potentials:
Voltage gated ion channels
Sodium channels open- sodium rushes in
Sodium channels close- stops inward flow of sodium
Potassium channels open- potassium rushes out
Net effect- Depolarization and then Repolarization
electrical flow created by ionic flow, not electron flow
Neuromuscular junction:
Motor neuron cell body and dendrites in gray matter of spinal cord
Axons extend to muscle
Axon’s terminal end contains a synaptic knob
Synaptic know has synaptic vesicles containing acetylcholine
Motor end plate:
Area beneath the terminal branches of the axons
Contains acetylcholine receptor complexes
Acetylcholine binding opens the receptor complex
Cholinesterase degrades acetylcholine into acetate and cholie
Proprioreceptors:
Muscle Spindles:
Encapsulated fibers within the muscle belly
Monitor changes in muscle length
Monitor the rate of change in muscle length
Respond by causing muscle contraction
Golgi Tendon Organs:
Encapsulated receptors
Located at the musculotendinous junction
Monitor tension within the tendon
Respond by causing the muscle to relax
Pacinian Corpuscles & Ruffini Endings:
Encapsulated receptors
Located near joints, in muscle, tendon, and bone
What are Chemical Synapses?
One way conduction mechanism that allows signals to directed toward specific goals. Allows the nervous system to perform its myriad function of sensation, motor control, memory etc.
What are Electrical Synapses?
An electrical synapse, also known as a gap junction, is a mechanical link between two neurons that allows for the conduction of electricity. Electrical synapses contain channels that allow charges (ions) to flow from one cell to another.
What is the Autonomic Nervous System?
Sympathetic and Parasympathetic Neurotransmitters and their regulatory organ system functions (excitatory and inhibitory)
Sympathetic:
Responsible for increasing activity (excitatory) in most systems (except GI)
Adrenergic fibers release epinephrine
Each sympathetic pathway from the cord to the stimulated tissue is composed of two neurons, a preganglionic neuron a postganglionic neuron, in contract to only a single neuron in the skeletal motor pathway
Sympathetic nerve fibers: T1-L2
T1: head
T2: neck
T3-T6: thorax
T7-T11: abdomen
T12-L2: legs
About 75% of all parasympathetic nerve fibers are in the vagus nerves (cranial nerve X), passing to the entire thoracic and abdominal regions of the body
Parasympathetic:
Responsible for slowing activity (inhibitory) in most systems (except GI)
Cholinergic fibers release acetylcholine
Somatic afferent (sensory):
Carries sensations from the periphery to the spinal cord. Includes exteroceptive (pain, temperature, touch) & proprioceptive.
Somatic efferent (motor):
Communicates from spinal cord to skeletal muscles.
What is the Central Nervous System composed of?
Brain (including retinas) and spinal cord
Which Organs are innervated by adrenergic (sympathetic) transmission?
Skeletal muscle → increases blood flow
Ventilation → increase
Sweat glands → increase perspiration
Heart → increase force and contraction rate
GI tract motility → Decrease
Eyes → dilate pupils
Secretion of digestive juices → decrease
Blood pressure → increase mean pressure
Airways → increase diameter
Which Organs are innervated by cholinergic (parasympathetic) transmission?
Skeletal muscle → decreases blood flow
Ventilation → decrease
Sweat glands → no effect
Heart → decrease force and contraction rate
GI tract motility → increase
Eyes → constrict pupils
Secretion of digestive juices → increase
Blood pressure → decrease mean pressure
Airways → decrease diameter
What is the Peripheral Nervous System composed of?
Spinal nerves and Cranial Nerves III-XII
Somatic Nervous System:
Afferent
Efferent
Autonomic Nervous System:
Sympathetic
Parasympathetic
What are the 3 major areas of the brain?
Cerebrum (telencephalon-(cerebral cortex), diencephalon)
Cerebellum
Brainstem (midbrain, pons, medulla oblongata)
What are the 2 major parts of the Diencephalon?
Thalamus
relays stimuli received from all sensory neurons to cortex for interpretation
relays signals from the cerebral cortex to the proper area for further processing
Hypothalamus
monitors many parameters
temperature, blood glucose levels, various hormone levels
helps maintain homeostasis
signals the pituitary via releasing factors
signals the lower neural centers
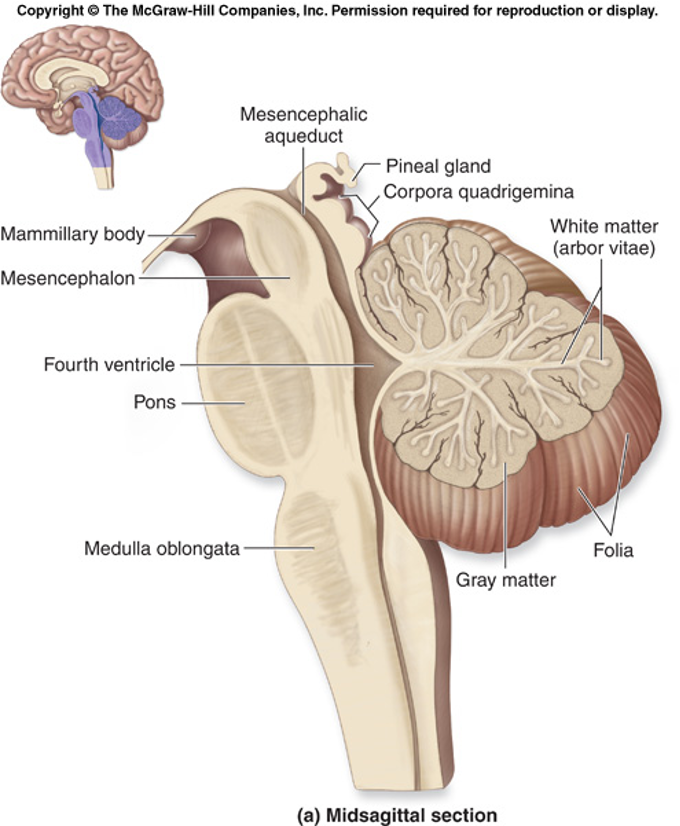
Cerebellum:
located behind the brainstem
helps monitor and regulate movement
integrates postural adjustments, maintenance of equilibrium, perception of speed, and other reflexes related to fine tuning of movement
Descending Nerve Tracts:
Ascending: dorsal
Descending: lateral, ventromedial tracts
What is Myelin?
Schwann cells wrapped around the axon of some neurons
appear as multiple lipid-protein layers
are a continuous cell
increase the speed of action potential production
White Matter:
Contains tracts or pathways made up of myelinated nerves
Carries ascending and descending signals
Brainstem:
Helps us with our reflexes
What are the Nodes of Ranvier?
Gaps between Schwann Cells
Impulse jumps from node to node
Saltatory conduction
What are Dendrites?
Receives stimuli and carry it to the cell body
What is the Cell body?
Site of cellular activity
Endocrine diseases can be classified either as diseases of ____ or ____ or as conditions involving the development of mass lesions- which themselves may be associated with underproduction or overproduction
underproduction or overproduction
Endocrine:
Produces internal secretions that are transported around the body by the bloodstream
Paracrine:
Describes a hormone or other secretion released from endocrine cells into the surrounding tissue rather than into the bloodstream. Insulin, secreted by pancreatic ß-cells affects secretion of glucagon by pancreatic a-cells
Exocrine:
Produces external secretions that are released through a duct
Negative feedback:
A system that prevents deviation from a mean value.
Ex. Blood sugar regulation
Positive feedback:
A system that promotes deviation from a mean value.
Ex. Childbirth, which the release of Oxytocin during labor triggers uterine contractions
Pituitary gland:
An endocrine gland, about the size of a pea, that sits in a small, bony cavity at the base of the brain whose secretions control the other endocrine glands and influence growth, metabolism, and maturation.
Hypothalamus:
A region of the forebrain located below the thalamus, forming the basal portion of the diencephalon, that regulates body temperature, some metabolic processes, and governs the autonomic nervous system.
Hypophyseal portal system:
The system of blood vessels that link the hypothalamus and the anterior pituitary in the brain.
Thyroid-stimulating hormone (TSH):
Produced by the anterior pituitary
Stimulates the release of thyroxine (T4) from the thyroid gland
It is regulated by thyrotropin-releasing hormone (TRH)
Thyrotropin-releasing hormone (TRH):
Produced by the hypothalamus
Stimulates cells in the anterior pituitary to secrete thyroid-stimulating hormone (TSH)
What is the term for an enlarged thyroid?
Goiter
A lack of thyroid hormone will lead to _____
decreased negative feedback on the pituitary, which in turn will lead to increased production of thyroid-stimulating hormone.
What are pancreatic islets?
They are small islands of cells that produce hormones that regulate blood glucose levels.
Insulin is produced by ____ in the pancreas and acts to lower blood sugar levels.
beta cells
Glucagon and insulin are _____ secreted by the pancreas that plays a key role in maintaining a stable blood glucose level.
peptide hormones
Glucagon is produced by ____ in the pancreas and acts to raise blood sugar levels.
alpha cells
Insulin:
A polypeptide hormone that regulates carbohydrate metabolism
Glycogen:
A polysaccharide that is the main form of carbohydrate storage in animals and also converts to glucose as needed
Glucagon:
A hormone, produced by the pancreas, that opposes the action of insulin by stimulating the production of sugar
Blood Sugar Chart:
Fasting for person without diabetes:
70-99 mg/dl (3.8-5.5 mmol/L)
Blood Sugar Chart:
Fasting for someone with diabetes:
80-130 mg/dl (4.4-7.2 mmol/L)
Blood Sugar Chart:
2 hours after meals for person without diabetes:
less than 140 mg/dl (7.8mmol/L)
Blood Sugar Chart:
2 hours after meals for someone with diabetes:
less than 180 mg/dl (10.0 mmol/L)
Blood Sugar Chart:
HBA1C for person without diabetes:
Less than 5.7%
Blood Sugar Chart:
HBA1C for someone with diabetes:
7.0% or less
Mechanical digestion:
Physical breakdown (chewing, churning, segmentation)
Chemical digestion:
To further degrade the molecular structure of the ingested compounds by digestive enzymes into a form that is absorbable into the bloodstream
Absorption:
Nutrients, water, and electrolytes are taken up into the bloodstream or lymph
Functions of the GIT organs?
Mouth: Chewing and initial breakdown of food with saliva containing enzymes, facilitating swallowing
Esophagus: Muscular tube that propels food to the stomach through peristalsis (muscle contractions)
Small intestine: Primary site of nutrient absorption, where food is mixed with digestive enzymes from the pancreas and bile from the liver, allowing for absorption of carbohydrates, proteins, fats and water
Liver: Produces bile, which helps with digestion of fats
Gallbladder: Stores and releases bile into the small intestine when needed
Pancreas: Secretes digestive enzymes into the small intestine to break down proteins, fats, and carbohydrates, as well as produces hormones like insulin to regulate blood sugar
Large intestine: Absorbs water from digested food, forming stool, and stores waste until defecation
What is the Neural Control of the Gut Wall?
The Enteric Nervous System (SNS)
What is the Neural regulation of the GIT?
Different types of reflexes
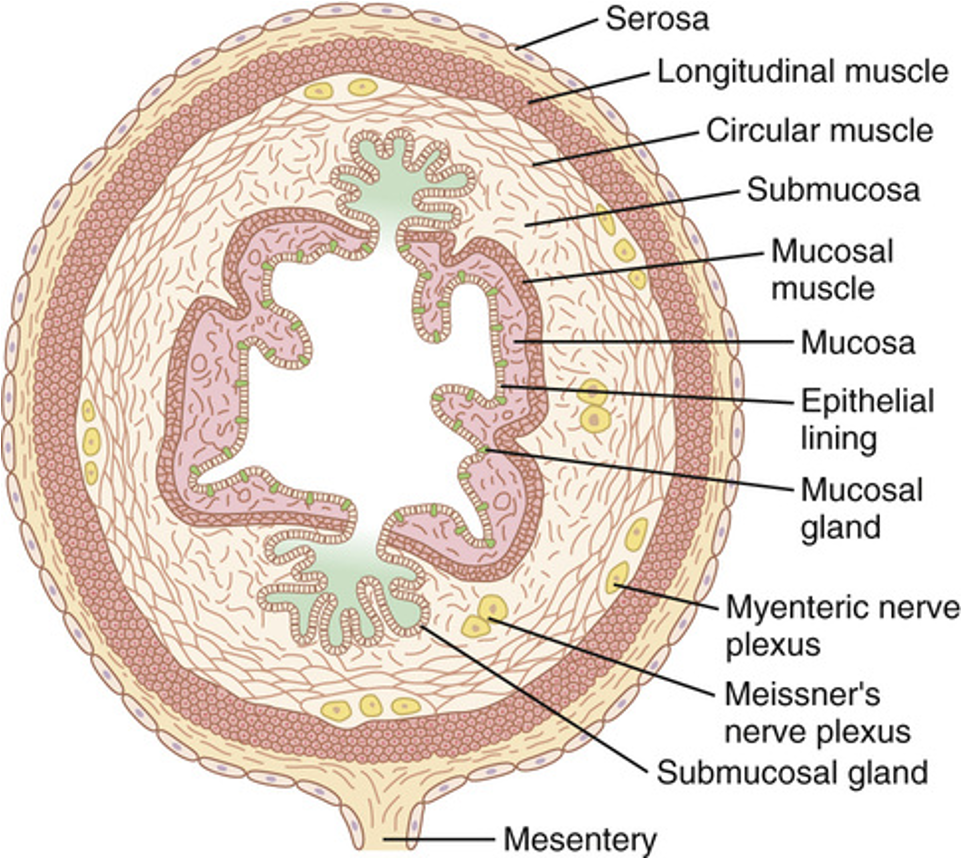
What is the Enteric Nervous System (ENS)?
Called the “gut brain” because it can control many aspects of digestion on its own, without input from the brain
Consists of 2 major plexuses (nerve networks) within the wall of the GI tract:
Myenteric Plexus (Auerbach’s plexus)
Submucosal Plexus (Meissner’s plexus)
Myenteric Plexus (Auerbach’s plexus):
Located between the muscle layers of the GI tract
Main function:
Controls GI movements (motility)- peristalsis (the wave-like muscle contractions that move food along)
Submucosal Plexus (Meissner’s plexus):
Located in the submucosa layer of the GI tract
Main function:
Controls GI secretion (e.g., digestive enzymes, mucus)
Controls local blood flow to the GI organs
Parasympathetic regulation- increases the activity of the enteric nervous system
Stimulation of PSP causes a general increase in the activity of the entire enteric nervous system, which enhances the activity of most GIT functions
Sympathetic regulation- inhibits GIT activity. Exterts this effect in 2 ways:
secretes norepinephrine to inhibit GIT smooth muscle
inhibitory effect of norepinephrine on neurons of the entire enteric nervous system
strong stimulation of the sympathetic nervous system can inhibit motor movements of the gut so greatly that it can literally block movements of food
What are the type of reflexes of the Enteric Nervous System (ENS)?
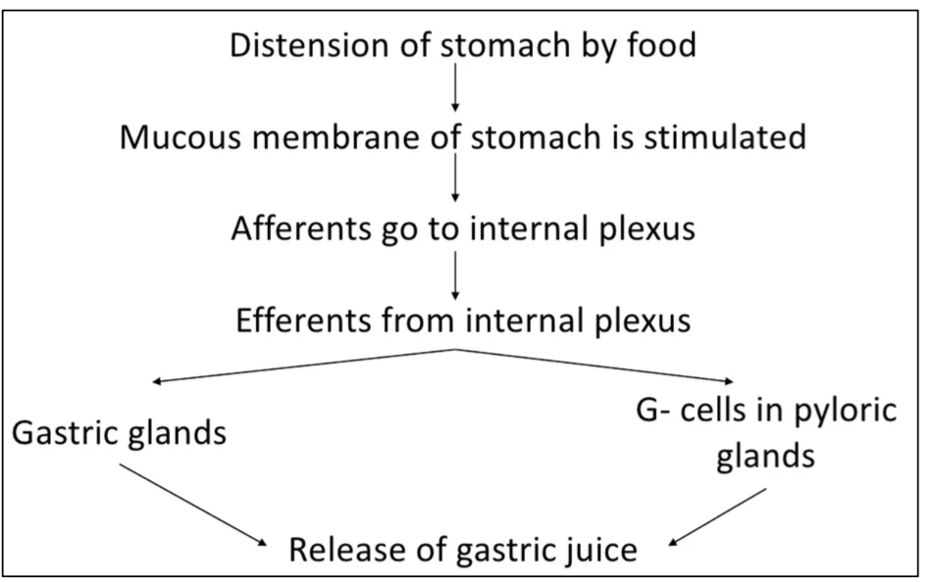
local reflex
short reflex
long reflex
Local reflex:
local reflex- integrates within the gut wall enteric nervous system
controls secretion, peristalsis, mixing contractions, local inhibitory effects
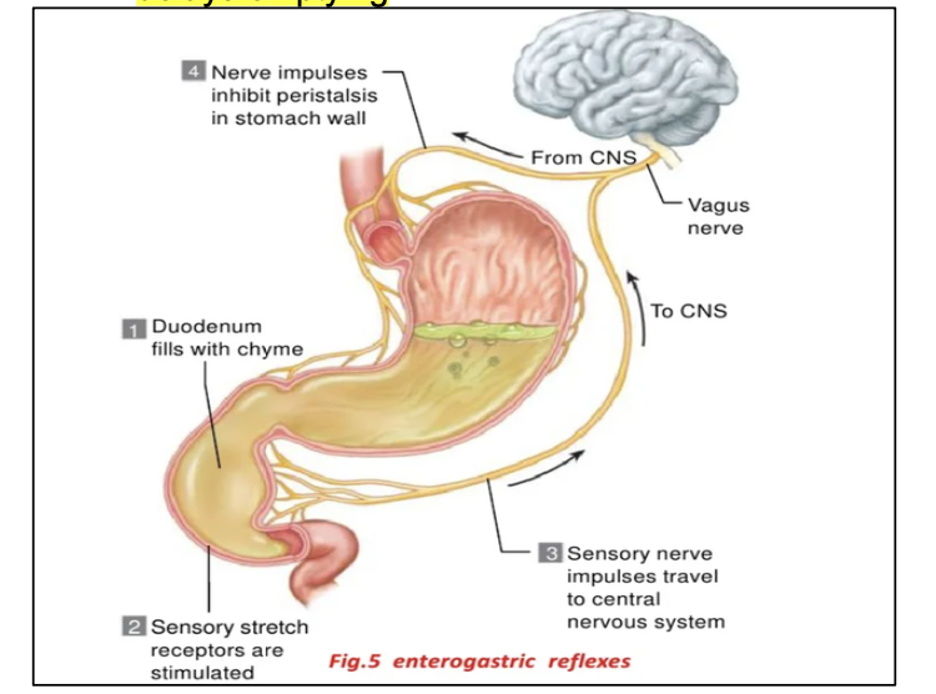
Short reflex:
short reflex- from gut to pre-vertebral sympathetic ganglia then back to GIT:
These reflexes transmit signals long distances to other areas of the GIT
Gastrocolic (Gastroileal) reflex- stomach activity leads to ileocecal relaxation, and increased mass movement in colon
Enterogastric reflex- fat or protein chyme reaches duodenum and send impulses to enteric nerves of the stomach that in turn causes the inhibition of stomachal motility and secretion. Delays emptying.
Coloileal reflex- inhibits emptying of ileal contents into colon
Ileogastric reflex- ileum is distended, reflex inhibits gastric motility preventing more chyme from entering intestine
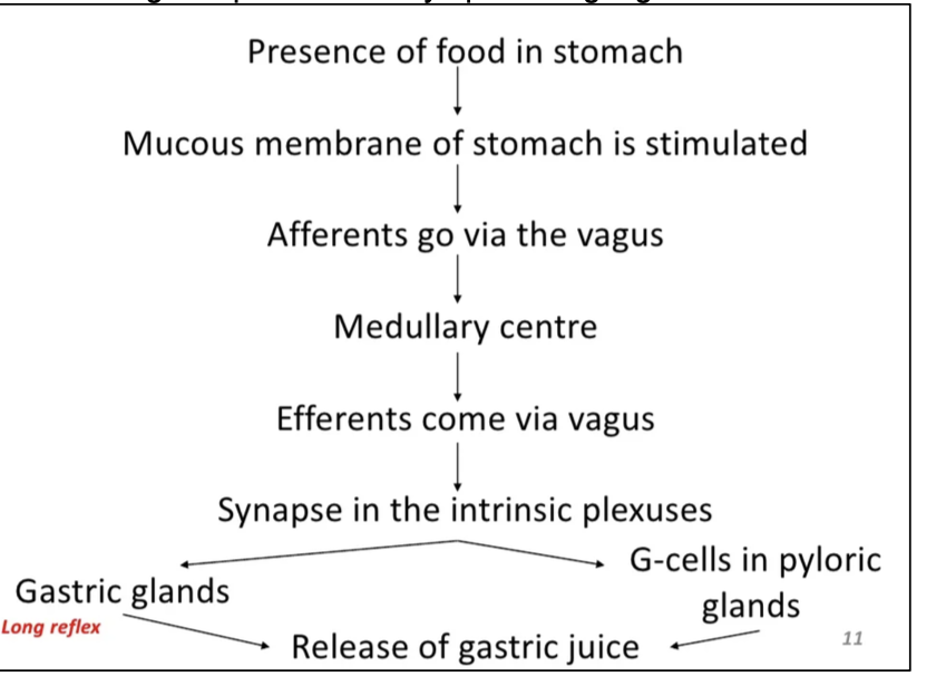
Long reflex:
Long reflex- from gut to the prevertebral sympathetic ganglia (brain) then back to GIT
Vaso vagal reflex- from stomach and duodenum to brain stem and back to stomach via vagus nerve to control gastric motor and secretory activity
pain reflexes that cause inhibition of entire GIT
Defecation reflexes- travel from colon and rectum to spinal cord and back to produce powerful colonic, rectal, and abdominal contractions required for defecation
Whats the Blood flow of the GIT?
Splanchnic circulation involves blood flow to the GIT, spleen, pancreas and liver
Blood from the GIT travels through the portal vein to the liver, where it is filtered and processed
The liver’s sinusoids filter out harmful substances and store nutrients like carbohydrates and proteins
The mesenteric arteries supply blood to the intestines, branching into smaller vessels that reach the muscle layers, intestinal villi, and submucosal areas
These arteries are crucial for supporting the motility, absorption, and secretion process in the gut
The arterial and venous vessels in the villi flow in opposite directions in a countercurrent arrangement
This setup allows oxygen from the arterioles to diffuse directly into the venules, bypassing the villus tissue
As much as 80% of oxygen is “short-circuited,” meaning it is not used by the villi for local metabolic functions
increase gut activity, such as absorption or muscle contractions, leads to increased blood flow to the gut, especially to the villi and submucosa
After a meal, blood flow increases to support digestion and absorption, but it gradually returns to normal after a few hours
Secretory activity is___
digestive or endocrine secretions (hormones, enzymes, etc.) of the organs of the GIT
Secretory activity of the cells in the Stomach
Stomach:
mucus- viscous and alkaline protects from acid and enzyme
intrinsic factor- secreted by parietal cells. Binds with vitamin b12 to help absorb
HCl- parietal cells- kills bacteria, stops carbohydrate digestion, denatures proteins, converts pepsinogen to pepsin
Secretory activity of the cells in the Small Intestine :
Small intestine:
goblet cells- produce protective mucus
endocrine cells- produce regulatory hormones
digestive enzymes, disaccaharidases, peptidases, nucleases
brunner’s glands- stimulates by vagus, secretes secretin
Secretory activity of the cells in the Large Intestine :
Large intestine:
mucus
Secretory activity of the cells in the Liver :
Liver:
bile, cholesterol, fats, fat-soluble hormones, lecithin
Secretory activity of the cells in the Gallblader :
Gallbladder:
stores and concentrates bile, DOES NOT PRODUCE BILE, it is stimulated by cholecystokinin to release bile
Secretory activity of the cells in the Pancreas :
Pancreas:
pancreatic lipase- digests fat
pancreatic amylase- digests carbs
trypsin- digests proteins
chymotrypsin
carboxypeptidase
The chyme composition:
Ingested food + stomach secretions
Examples of Acid Base Balance disorders:
Proteins- HCI denatures proteins. Trypsin, chymotrypsin, and carboxypeptidase digest proteins
Carbohydrates- salivary amylase digests carbohydrates. Stomach acid inactivates salivary amylase, so no carbohydrate digestion in the stomach. Pancreatic amylase continues to digest carbs.
Lipids- bile emulsifies lipids allowing pancreatic lipase to digest lipids
What is the function unit of the liver?
The liver lobule
What is the liver lobule?
The liver lobule is the functional unit of the liver, consisting of hepatocytes arranged in a hexagonal structure around a central vein
portal triad: composed of a branch of the hepatic artery, portal vein, and bile duct
hepatocytes: responsible for functions like bile production, detoxification, nutrient metabolism (e.g. glucose and fat), and protein synthesis (e.g. albumin, clotting factors)
sinusoids: capillary-like vessels that allow for the exchange of substances between blood and hepatocytes
What are the 5 GI hormones that qualify as endocrine?
Gastrin
Cholecystokinin (CCK)
Secretin
Glucose-dependent insulinotropic peptide (GIP)
Motilin
What are the 2 example of paracrine hormones?
Somatostatin
Histamine
Which hormones operate as a combination of Endocrine and Paracrine mechanisms?
Glucagon-like peptide-1 (GLP-1)
Pancreatic polypeptide
Peptide YY
The alimentary tract provides the body with a continual supply of ___
water, electrolytes, vitamins, and nutrients
Order of food digestion:
Ingestion → mechanical digestion (chewing)→ propulsion (swallowing, and peristalsis)→ chemical digestion → absorption → defecation
Motility physiological anatomy of the gastrointestinal wall:
A typical cross section of the intestinal wall:
The serosa
a longitudinal smooth muscle layer
a circular smooth muscle layer
the subucosa
the mucosa
When the RMP becomes less negative, which is call depolarization of the membrane, the muscle fibers before _____
more excitable
When the RMP becomes more negative, which is called hyperpolarization, the fibers become ___
less excitable
Factors that depolarize the membrane (make it more excitable):
Stretching of the muscle
Stimulation by Ach (Acetylcholine) released from the endings of parasympathetic nerves
Stimulation by several specific GI hormones
Factors that make the membrane potential more negative (make the muscle fibers less excitable):
The effect of NE or Ep on the fiber membrane
Stimulation of the sympathetic nerves that secrete mainly NE at their endings
Types of neurotransmitters secreted by the enteric neurons:
Different neurotransmitter substance that are released by the nerve ending of different types of enteric neurons including:
Acetylcholine (most often excited gastrointestinal activity)
Norepinephrine (almost always inhibits gastrointestinal activity)
Adenosine triphosphate
Serotonin
Dopamine
Cholecystokinin (CCK)
substance P
vasoactive intestinal polypeptide
somatostastin
leu-enkephalin
met-enkephalin
bombesin
Hormone- Gastrin
Stimuli for secretion:
Protein
Distention
Nerve (acid inhibits release)
Site of Secretion:
G cells of the antrum, duodenum, and jejunum
Actions:
Stimulates:
Gastric acid secretion
Mucosal growth
Hormone- Cholecystokinin (CCK)
Stimuli for secretion:
Protein
Fat
Acid
Site of Secretion:
I cells of the duodenum, jejunum, and ileum
Actions:
Stimulates:
Pancreatic enzyme secretion
Pancreatic bicarbonate secretion
Gallbladder contraction
Growth of exocrine pancreas
Inhibits:
Gastric emptying
Hormone- Secretin
Stimuli for secretion:
Acid
Fat
Site of Secretion:
S cells of the duodenum, jejunum, and ileum
Actions:
Stimulates:
Pepsin secretion
Pancreatic bicarbonate secretion
Biliary bicarbonate
Growth of exocrine pancreas
Inhibits:
Gastric acid secretion
Hormone- Gastric inhibitory peptide (GIP)
Stimuli for secretion:
Protein
Fat
Carbohydrate
Site of Secretion:
K cells of the duodenum, jejunum, and ileum
Actions:
Stimulates:
Insulin release
Inhibits:
Gastric acid secretion
Gastric inhibitory peptide (GIP):
Glucose-dependent insulinotropic peptide
Functional types of movements in the GIT:
Propulsive movements (Peristalsis), which cause food to move forward along the tract at an appropriate rate to accommodate digestion and absorption
Mixing movements, which always keeps the intestinal contents thoroughly mixed