UBC PSYC 301, Jay Hosking
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Grey Matter
cell body clusters of neurons
CNS: called "nuclei"
PNS: called "ganglia
White Matter
bundles of myelinated axons
CNS: called "tracts"
PNS: called "nerves"
Everywhere Else: called "fibres"
Nissl stains are for ____, while Fibre stains are for ____.
grey matter, white matter
Projection Neurons
have long axons that project to other brain areas, aren't myelinated and communicate info quickly
Interneurons
have short axons that project locally, modify the signal of projection neurons, and are star-shaped
Microglia
small cells on the lookout for problems in the brain, and fixes those problems by going into a prime state where they grow larger and essentially digest the problem
Myelinating Glia: Schwann Cells
wrap themselves around a single axon only to speed up neural communication and found in the PNS
Myelinating Glia: Oligodendrocytes
wrap themselves around several axons to speed up neural communication and found in the CNS
Myelinating Glia: Astrocytes
part of the blood brain barrier, and provide nutrition to neurons, control the neuron and synapse environment, heal neurons and influence the neuron's communication
Mitochondria
powerhouse of the cell and turns what we eat into energy for the cell
Cytoskeleton
microtubules run in the cytoskeleton and kinesin (anterograde transport)/dyenin (retrograde transport) walk along them carrying vesicles to deliver info
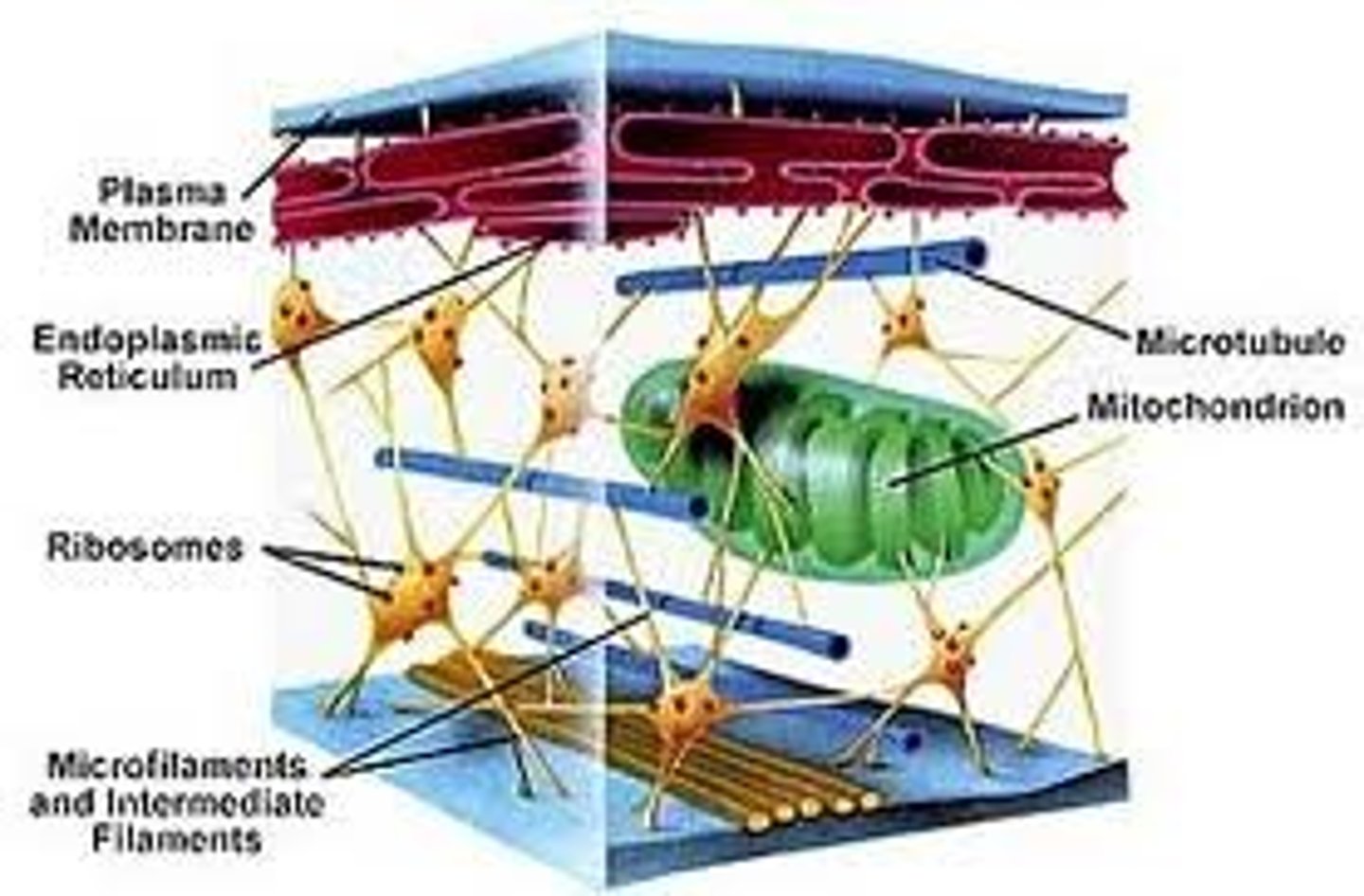
Cell Membrane
hydrophilic bilayer on the outside (interacts with water/polar elements only) and hydrophobic bilayer on the inside (non-polar and repels water), keeping out all dangerous entities
Resting Potential of Cell Membrane
~ -70 mV
Excitatory Post-Synaptic Potential (EPSP)
depolarize the cell membrane, increase the likelihood of the post-synaptic neuron firing an action potential
(i.e decrease the membrane potential from -70mV to -67mV)
Inhibitory Post-Synaptic Potential (IPSP)
hyperpolarize the membrane, decrease the likelihood of the post-synaptic neuron firing an action potential
(i.e increase the membrane potential from -70mV to -72mV)
Absolute Refractory Period (Resting Membrane Potential)
during the repolarization phase (phase 2) of an action potential where the Na+ channels are blocked by the amino acid "ball and chain"
can't fire another action potential during this time
Relative Refractory Period (Resting Membrane Potential)
during the hyperpolarization phase (phase 3) of an action potential where the few voltage-gated K+ channels open and close slowly
can only fire an action potential during this time under the right circumstances
Ionotropic Receptors
ligand-gated ion channels that send signals and open only when binded to
Metabotropic Receptors
G-protein-coupled receptors (GPCRs) that modify signals and cause signal cascades
Autoreceptors
regulate how many neurotransmitters are released, sensitive to only neurotransmitters or hormones released by the cell in whose wall they are embedded
Heterecepters
respond to neurotransmitters, they receive neuromodulators or neurohormones released from adjacent neurons or cells to modify signals
Agonists
increase function in the neurotransmitter system
Antagonists
decrease function in the neurotransmitter system
Glutamate
primary excitatory neurotransmitter that generate action potentials, and is used throughout the brain (so it's not a great target for drugs as it will affect the whole brain)
Drugs that target Glutamate (Antagonist Tranquilizers/Relaxants):
laughing gas
ketamine
alcohol
*Glutamate agonists cause crippling anxiety
GABA
inhibitory neurotransmitter that cause IPSPs, used throughout the brain (so it's not a great target for drugs as it will affect the whole brain)
Drugs that target GABA (Agonists that increase Inhibition):
xanax
alcohol
ether (anesthetic)
*GABA antagonists cause anxiety
Dopamine
an amine, not really the "pleasure molecule" as it plays many important roles in our body like influencing motivation, learning, mood, attention, etc.
Drugs that target Dopamine (all addictive drugs that increase Dopamine transmission):
cocaine
nicotine
heroin
alcohol
*Dopamine Antagonists are used as Schizophrenia medications to decrease motivation
Norepinephrine (Noradrenaline)
causes heterosynaptic facilitation (an increase in amplitude of an EPSP), and causes enhancement of stress and emotion-related memory which is useful evolutionary-wise
Propanolol (Norepinephrine Antagonist):
relaxing, potential PTSD treatment by recalling traumatic memories while on the drug to modify one's emotional response
Serotonin
neuromodulator that effects mood, depletion of serotonin can cause depression
Selective Serotonin Re-Uptake Inhibitors (SSRIs):
helps with depression by blocking serotonin from being removed from the synapse, but is only really useful for major depression
Acetylcholine
controls muscles by propagating nerve impulses across the neuromuscular junction and affects wakefulness, attention, etc.
Nicotine (Agonist):
can have mild effects on attention
Endocannabinoids
has a psychoactive effect caused by our endocannabinoid system (which works via retrograde transmission), and causes forgetting unnecessary info by deliberately weakenins the connection between two cells at a synapse
Cannabis (Agonist):
travels to the brain and binds to the endocannabinoid system
Adenosine
adenosine tri-phosphate (ATP) is cellular energy and adenosine is the byproduct that builds up over the waking day and makes one tired
Caffeine and Theophylline/Tea (Antagonists):
bind to adenosine receptors blocking adenosine from being broken down by the cell, your brain will notice a build up of adenosine and send in more receptors to break it down which causes a tolerance to develop
Endogenous Opioids (aka Neuropeptide and Endorphins)
giant peptide neurotransmitters that exist in a neurotransmitter system (that exogenous opioids mimic)
Fentanyl (Agonist) and Naloxone (Antagonist):
fentanyl is an exogenous opioid that binds to the opioid receptors causing a high
naloxone binds to the opioid receptors and blocks opioids (like fentanyl) from binding and being processed which can save you from an overdose
Central Nervous System (CNS)
consists of the brain and spinal cord
Peripheral Nervous System (PNS)
overarching nervous system that connects the CNS to the rest of the body's organs and muscles
made up of the SNS, ANS, efferent (motor) and afferent (sensory) signals, and the sympathetic and parasympathetic nervous systems
Somatic Nervous System (SNS)
controls voluntary movements of skeletal muscles and conveys info to and from the CNS
Autonomic Nervous System (ANS)
conveys involuntary and automatic movements that control internal organs and glands
Sympathetic Nervous System
mobilizes energy and prepares the body for "fight or flight" situations
Parasympathetic Nervous System
conserves energy and helps the body return to a normal resting state
Efferent Signals
motor signals
Afferent Signals
sensory signals
Sections of the Spine (Top to Bottom)
cervical
thoratic
lumbar
sacral
coccygeal
Major Division of the Brain
Forebrain:
telencephalon
diencephalon
Midbrain:
mesencephalon
Hindbrain:
metencephalon
myelencephalon (or medulla)
Parts of the Meninges (Outermost to Innermost Layer)
Dura Mater (thickest, outermost layer)
Arachnoid Mater (middle layer that's hard to see)
Pia Mater (thin, transparent layer)
Hydrocephalus
condition where the travel of cerebrospinal fluid (CSF) gets blocked and can't get out of the brain, causing ventricles to enlarge and damages the surrounding brain tissue
Treatment:
Shunt to get rid of CSF
Cerebral Angiography
an injection of iodine travels through the bloodstream, showing the arteries and blood vessels of the brain through an x-ray
(useful for ischemias, hemorrhages, anything restricting blood supply)
Computed Tomography (CT/CAT Scan)
fires x-rays at different angles and constructs a 3D model of the brain but doesn't show white vs. grey matter
Magnetic Resonance Imaging (MRI)
employs powerful, very cold magnets which produce a strong magnetic field that forces protons in the body to align with that field and gives you a structural 3D model of the brain
(useful for seeing tumours, seeing all parts of brain tissue)
Diffusion Tensor Imaging (DTI)
relies on how water/hydrogen molecules move freely in the brain (though constrained to moving along the axon since it's skinny) and measuring it's diffusion
(gives a sophisticated map of white matter and can see damage to axons)
Electroencephalography (EEG)
detects electrical activity in the brain using small, metal discs (electrodes) attached to the scalp
(not super useful for detecting brain damage)
Positron Emission Tomography (PET)
uses radioactive cocaine to see what and where it binds to (normally it binds to the striatum) and overall gives an indirect measure of brain activity
Paired Image Subtraction (shows what the mean brain looks like when performing a certain task):
compare the control and dependent conditions, subtract the inactivity and leave the task-specific brain activity to create a mean difference image
(useful for looking at specific systems or proteins and at lifespan and condition changes, how drugs and alcohol lead to a weaker dopamine receptor, measuring Diaschisis)
Functional MRI (fMRI)
detects changes in the BOLD (blood oxygen level dependent) levels, active parts of the brain will have more oxygenated blood coming to them about 6 seconds after first activity causing a peak
Ischemic Stroke
a clot blocking blood flow to an area of the brain as a result from a cerebral ischemia (problems with blood flow to the brain)
3 main causes:
thrombosis; a plug of a variety of things (i.e air, fat)
embolism; a moving thrombosis
arteriosclerosis; walls of blood vessels are thickening and channels are narrowing
*thrombosis and arteriosclerosis can interact
Hemorrhagic Stroke
bleeding inside or around the brain as a result of a cerebral hemorrhage
Multiple Sclerosis (MS)
a progressive disorder in which the immune system seems to primarily attack the myelin sheath of axons in the central nervous system (and also causes some cell loss), causing signals to be lost
Symptoms in advances cases include visual disturbances, muscular weakness, numbness, tremor, loss of motor coordination
relapsing-remitting; goes between having and not having symptoms
secondary progressive; goes from relapsing-remitting to having symptoms all the time
primary progressive; have symptoms all the time
Posterior Parietal Association Cortex
provides info on where body parts are in relation to the external world, receives input from visual, auditory, and somatosensory systems (stretch receptors), output goes to the secondary motor cortex, some go to the dorsal prefrontal cortex, stimulation of this area makes the subject feel like they're performing an action
Damage:
apraxia; inability to perform movements on command
contralateral neglect
Dorsolateral Prefrontal Association Cortex
receives projection from the posterior parietal cortex, projects to the secondary motor cortex, primary motor cortex and the frontal eye field, involved in assessments of external stimuli, may work with posterior parietal cortex in decisions regarding voluntary responses (decision-making), dorsolateral prefrontal cortex motor neurons fire first in motor chain, also critically involved in many other functions (i.e problem-solving, math, working memory, learning)
Damage:
affects a number of sophisticated cognitive functions
problems initiating movement as well
Secondary Motor Cortex
eight areas (2 areas of premotor cortex, 3 supplemental motor areas, 3 cingulate motor areas), projects to primary motor cortex, each other and the brainstem, produces complex movements (both before and during voluntary movements)
the exact role of this area is unclear, however the supplemental area is associated with planning (internally guided), premotor cortex is externally guided (i.e following a cursor on a screen with your finger), premotor areas encode spatial relations and program movements
Primary Motor Cortex
very back of frontal lobe
somatotopic organization; when a specific part of the body is associated with a distinct location in the central nervous system, all the specific parts that control one type of movement (i.e moving hand, fingers, elbow, etc.) are clustered together, disproportionately represent all parts (the bigger the body part, the bigger area in the brain to control it)
receives feedback from joints and muscles, stretch receptors, neurons code for preferred direction not muscles per se (they code for type of movement, not what it's moving)
Damage:
not as disruptive as one might think, affects independent movement (i.e you might have to move all fingers, not just your thumb)
astereognosia; inability to recognize objects just by touching them in your hand
reduced speed/accuracy/force
Cerebellum
receives input from primary and secondary motor cortexes, info about descending motor signals from the brainstem nuclei and feedback from motor responses (i.e stretch receptors) via the somatosensory and vestibular systems, critical for timing and sequence and then corrects our motor behaviour, ipsilateral control of body (controls movement from the same side of the cerebellum)
Damage:
loss of ability to precisely control the direction, force, velocity and amplitude of movements
loss of ability to adapt patterns of motor output to changing positions
difficulties in maintaining steady posture
disturbances in balance, gait, control of eye movement
impairments on measures of attention and executive control, procedural memory, working memory, language and visual-spatial processing
impairments in learning of new motor sequences
Basal Ganglia
made of two parts; the striatum (which is made of putamen and head of caudate) and globus pallidus, other important parts are the subthalamic nucleus and substantia nigra (which when damaged can cause Parkinson's Disease), modulates motor output according to classical view, critical to habit formation and muscle memory, many congitive role (i.e motivation), promotes skill learning