H&S Y2 work in progress
1/590
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
591 Terms
What is Duty of Care? (3)
- Always act in the best interest of individuals and others
- Not act or fail to act in a way that results in harm
- Act within your competence and not take on anything you do not believe you can safely do.
Define the legal duty of care
A legal obligation on one party to take care to prevent harm suffered by another
In general, what is the legal situation regarding doctors' duty of care to patients when not at work?
- Outside hospital or a doctor's surgery, a doctor does not normally owe a duty of care if they did not attempt to help. Doctors are not legally obliged to act as 'good Samaritans'
- However, if a doctor states they are a doctor or starts to act as if they are a doctor, then they will have taken on a duty of care to that patient.
How does a doctors duty relate to the Montgomery case
Doctor's duty involved taking "reasonable care to ensure that the patient is aware of any material risks involved in any recommended treatment, and of any reasonable alternative or variant treatments
principles of safeguarding (6)
Empowerment, prevention, proportionality, protection, partnership, accountability
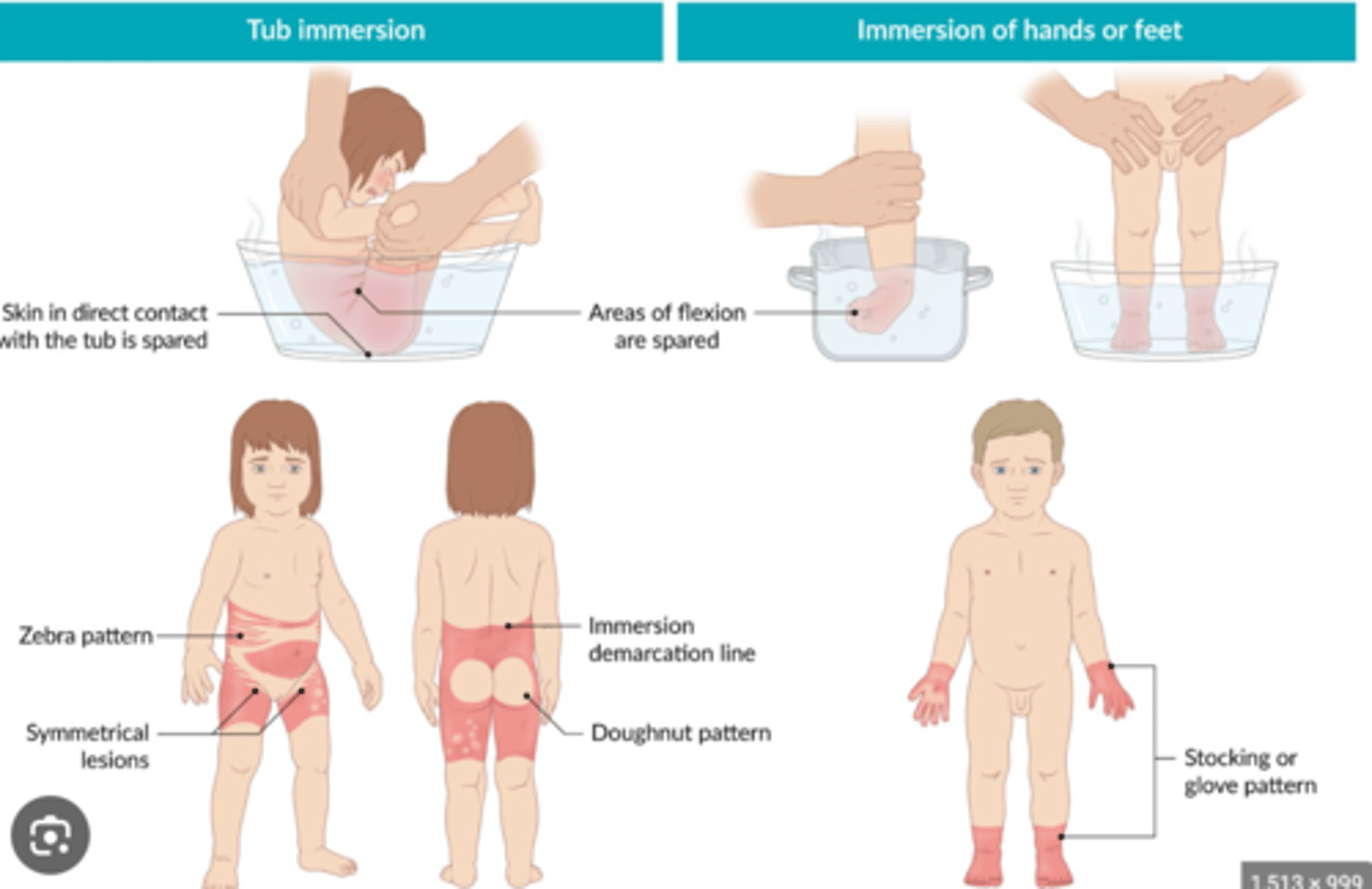
injury patterns of non-accidental burns (5)
- Symmetrical burns of uniform depth
- restraint injuries on upper limbs
- obvious pattern from cigarettes etc
- no splash marks in a scald injury
- doughnut sign (spared skin surrounded by scald)
In 1974 the WHO launched the Expanded Programme of Immunisation. What was this aim of this?
The goal was set to make immunisation against diphtheria, pertussis, tetanus, poliomyelitis, measles and tuberculosis available to every child in the world by 1990
What questions doe PEO ask?
P - Population: Problem interested in, population/person characteristics
E - Exposure e.g drug, pollution
O - Outcomes: Morbidity/death/complications/...
When to use PICO and PEO?
- PICO is best for looking at the effect of an intervention using RCT's
- PEO is best for looking at etiological/prognosis questions
What is global health?
5 reasons why we may see more pandemics in the future?
1. Increased Global travel: 1990: 1 billion travelled by
air, by 2018 that became 4.2 billion
2. Increased Urbanisation: by 2050 66% will live in
urban areas, most growth in Africa and Asia: increase in overcrowding, unhygienic
environments
3. Climate change
4. Increased human-animal contact - zoonotic
diseases
5. Weak health systems = decreased ability to detect + surveil
What is the 10/90 gap?
90% of research and development on health has been oriented toward diseases affecting high-income countries and only 10% on low-income countries.
The idea is that despite the majority of the global health burden being concentrated in developing countries, a significant imbalance exists in the allocation of resources for research and development
What is the solution for the '90/10 gap'? (4 steps)
- Regulation of the quality of imported food, medicines, manufactured goods, and inputs
- Getting timely access to information about the global spread of infectious disease
- Procurements of sufficient vaccine and drug supplies in a pandemic
- Ensuring a sufficient corps of well-trained health personnel
Leder (1990) referred to the "absent body" What is he trying to say?
Most of the time we take our bodies for granted as an
extension of ourselves (we don't think about using it)
*It is only when the body is sick or in pain that it
intrudes on our consciousness and we become aware
of it (dys-appearance)
What is the civilised body?
The functions of the body ('unbounded") should be hidden and
kept separate from public life (urinating, defecating, bleeding,
lactation etc.)
Reasons for increase in body image issues
Individualisation - placing greater emphasis on individual responsibility and personal choices
Healthism - excessive preoccupation with personal health and the belief that an individual's health status is a reflection of their moral character, worth, or value in society
Social media - Filters, photo-editing apps, and digital manipulation contribute to a distorted perception of beauty, fostering unrealistic expectations.
2 aspects of body image
- socio cultural (internalised)
- psychological (self perception)
What type of body image can contribute to eating disorders
Negative body image (dysphoria)
Measures of body image (self perception)
- body appreciation scale (BAS-2)
- Body esteem scale for adolescents and adults (BESAA)
- Body shape questionnaire
- The centre for appearance research valence scale
- The drive for muscularity scale
- The body dissatisfaction subscale of the eating disorder inventory 3 (EDI-3)
- The appearance evaluation subscale and body areas satisfaction scale
biographical disruption
A concept to describe the profound and often disruptive impact that the experience of illness or a significant health event can have on an individual's life narrative or biography.
It refers to the way in which an unexpected health event can challenge and reshape a person's sense of self, identity, and the trajectory of their life story.
3 distinct facets of biographical disruption
1. A taken-for-granted state of wellness
2. Disruption to biography
3. Response to disruption
reasons for falling vaccination levels in UK (3)
- Some speculate a 'vaccine fatigue' after COVID
- It may also be related to strains on healthcare services
- There may also be a resurgence in anti-vaccination
sentiments
Describe vaccination act of 1853 and how it divided opinion
- Vaccination Act of 1853 made smallpox vaccination free and
compulsory. This was very unpopular with section of the British public due to suspicion of using cowpox as a vaccination.
- Anti-vaccination leagues sprang up in the UK
- A smallpox epidemic in 1871 in which 23,000 people
died polarised opinion
- Led to The British Vaccination Act of 1898 included a
'conscience clause' to allow exemption
What is required for a disease to be eradicated using vaccination? (3 requirements)
- Where no other reservoirs of the infection exist in animals or environment
- Where consequences of infection are very high
- Where scientific and political prioritisation exists
Why could smallpox be eradicated (1979) by vaccination? (4)
• Only one dominant variant
• Vaccine was highly effective at inducing sterile immunity
• No animal reservoir > -no other species
• Vaccination was coupled with active surveillance and
containment
Why would eradication of polio be possible?
• No long term asymptomatic carriers for poliovirus in immunocompetent individuals
• No non-primate reservoir in nature
What can we learn from public vaccination in the past?
- Vaccines provoke popular myths and story-telling
- Compulsory vaccination can fuel controversy and mistrust
- Anti-vaccination arguments tend to focus on vaccines.
being ineffective and causing harm
- Support from healthcare professionals and the public
trust is key to successful immunisation programmes
General trend in vaccination coverage of the UK
Coverage decreased for 12 of the 14 vaccine coverage measures reported in 2022-23, with No vaccines meeting the 95% target
Which disease has been re established in the UK after being elimination status in 2017?
Measles
Concerns about vaccine safety are the main reason that parents decline to have their child vaccinated. Therefore it is important to reassure parents about vaccine safety to maintain public health. Can do so by saying what things?
• The risk of not vaccinating your child is significant - e.g measles is highly contagious
• Vaccination is extremely safe and most side effects are very minor e-g fever, aches.
• More serious (allergic) reactions are very rare and we have the equipment to deal with them
• The risks of not vaccinating are far greater than of vaccinating
• Parents need to be informed that vaccinations are safe and effective
Expert Advisory Group formed in 1995 and generated the
what report and why? What were its aims?
"Calman-Hine" report was generated to improve cancer outcomes in the UK:
- All patients to have access to a uniformly high quality of care. (wherever they live)
- Public and professional education to recognise early symptoms of cancer (+ national screening)
- Primary care to be central to cancer care
- The development of cancer services should be patient centred
- The psychosocial needs of cancer sufferers and carers to be recognised
3 levels of care to provide solutions in Calman-Hine report 1995
1. Primary care
2. Cancer Units Serving DGHs
- Treating Common Cancers
- Diagnostic procedures
- Common Surgery
- Non Complex chemotherapy
3. Cancer Centres - population of 1,000,000
- Treating Rare cancers
- Radiotherapy
- Complex chemotherapy
MDT's function in cancer care (6)
• To discuss every new diagnosis of cancer within their site
• To decide on a management plan for every patient
• To inform primary care of that plan (ensure comms maintained)
• To designate a key worker for that patient
• To develop referral, diagnosis and treatment guidelines for their tumour sites according to local and national guidelines
• Audit to ensure thorough running
The NHS cancer plan (2000) covered the broad concepts of prevention, screening, diagnosis, treatment. What was the 4 aims?
• To, save more lives
• To ensure people with cancer get the right professional support and care as well as the best treatments
• To tackle the inequalities in health that mean unskilled workers are twice as likely to die from cancer as professionals
• To build for the future through investment in the cancer workforce, through strong research and through preparation for the genetics revolution, so that the NHS never
falls behind in cancer care again.
Cancer reform strategy (2007) stated what 6 key areas for action (+ describe how)
1. Prevention - through promoting lifestyle choices e.g smoking, HPV vaccination
2. Diagnosing cancer earlier - through The National Awareness and Early Diagnosis Initiative , new referral guidelines AND screening e.g cervical, breast and bowel
3. Ensuring better treatment - through reducing waiting times, chemo audits, Increase in radiotherapy capacity
4. Living with and beyond cancer (i.e improving support) - through National Cancer Survivorship Initiative (ended 2013)
5. Reducing cancer inequalities
6. Delivering care in the most appropriate setting - locally where possible + centralised to improve outcomes
The National Awareness and Early Diagnosis Initiative (as part of cancer reform strategy 2007)
• coordinate a programme of activity to support local
interventions to raise public awareness of the signs
and symptoms of early cancer and encourage people
to seek help sooner
• developing a tool for measuring awareness levels
Cancer screening programmes in UK (3)
1. Breast - Mammograms offered to 50 -71 year olds
2. Cervical - Smears offered every 3 years from age 25-49, and every five years from 50-64
3. Bowel - men and women aged 60-74 are sent a home testing kit every two years to collect a small sample of poo using a Faecal Immunochemical Test (FIT)
A Strategy for Cancer (2011) 4 key aims
• Prevention and early diagnosis - through promoting lifestyle choices, screening changes (e.g digital images) and Increasing access to diagnostic tests in primary care
• Quality of life and patient experience - through Repeating patient experience survey, More one-to one support roles
• Better treatments - through new cancer drugs fund, Reducing variation in radiotherapy
• Reducing inequalities
Independent cancer Taskforce (2015) aims (4)
• Spearhead a radical upgrade in prevention and public health
• Drive a national ambition to achieve earlier diagnosis
• Transform our approach to support people living with and beyond cancer
• Make the necessary investments required to deliver a modern high-quality service, including Overhaul processes for commissioning, accountability and provision
NHS long term plan (2019) key ambitions (2)
• by 2028, 55,000 more people each year will survive their cancer for five years or more; and
• by 2028, 75% of people with cancer will be diagnosed at an early stage (stage one or two).
NHS long term plan (2019) key interventions
• Cancer Alliances
• Early detection - new screening tests
• Rapid Diagnostic Centres
• Faster Diagnosis Standard
• Cancer Workforce Plan
• Targeted Lung Health Checks
5 examples of cancer care policy's
- NHS long term plan (2019)
- Independent cancer Taskforce (2015)
- A Strategy for Cancer (2011)
- Cancer reform strategy (2007)
- The NHS cancer plan (2000)
What is Screening?
the systematic application of a test or inquiry, to identify individuals at sufficient risk of a specific disorder to warrant further investigation or direct preventive action, amongst persons who have not sought medical attention on account of symptoms of that disorder.'
primary vs secondary vs tertiary prevention
Primary - Prevents onset of disease e.g Health Education, immunisations, prenatal classes
Secondary - Detect and cure disease at early stage. E.g. cancer screening e.g Screenings, disease surveillance, control of outbreaks, STD treatment
Tertiary - Minimise the effects or reduce the progression of irreversible disease e.g PT/OT, support groups
Approaches to primary prevention:
High risk strategy vs population strategy
High risk - Targeting high risk sub groups of the population and moving them to lower risk via treatment
Population - aims to reduce the burden of disease
across the entire population
Pros and cons of high risk primary prevention
Pros:
- Appropriate to individual
- Motivated subject
- Motivated clinician
- Cost-effective resource use
- high benefit:risk
Cons:
- Screening difficult (need to find the people)
- Palliative & temporary
- Limited potential
- Labelling
Pros and cons of population primary prevention
Pros:
- Large Potential impact
Cons:
- Prevention Paradox (small individual benefit)
- Poor motivation
- Low benefit:risk
What is prevention paradox?
A preventative measure which brings much benefits to the population but offers little to each participating individual.
eg cigarette tax
What drives thresholds for treating many risk factors?
Weighing the balance between costs and benefits:
• Absolute benefits (no. of deaths prevented)
• Costs to individuals (another tablet?)
• Costs to populations (another million tablets?)
• Absolute harms (no. of people harmed)
Reasons for screening (3)
1. Screening gives the potential for early treatment and better outcomes
2. In some cases, screening can prevent the onset of disease through preventative treatment (e.g. removal of abnormal cells)
3. People may not have any symptoms (asymptomatic)
UK National Screening Committee (2015) 5 criteria
• Condition - Needs to be a significant health problem that is reasonably well understood, with a common Course of disease and a detectable risk factor.
• Test - There should be a simple, safe, precise and validated screening test
• Treatment - There should be an effective treatment with evidence of early treatment leading to better
outcomes
• Programme - must be RCT evidence that the programme is effective in reducing mortality or morbidity AND The benefit from the programme should outweigh the harm
• Implementation - The opportunity cost of the programme should be economically balanced in relation to health
care spending AND There must be a plan for quality assurance and adequate staffing and facilities
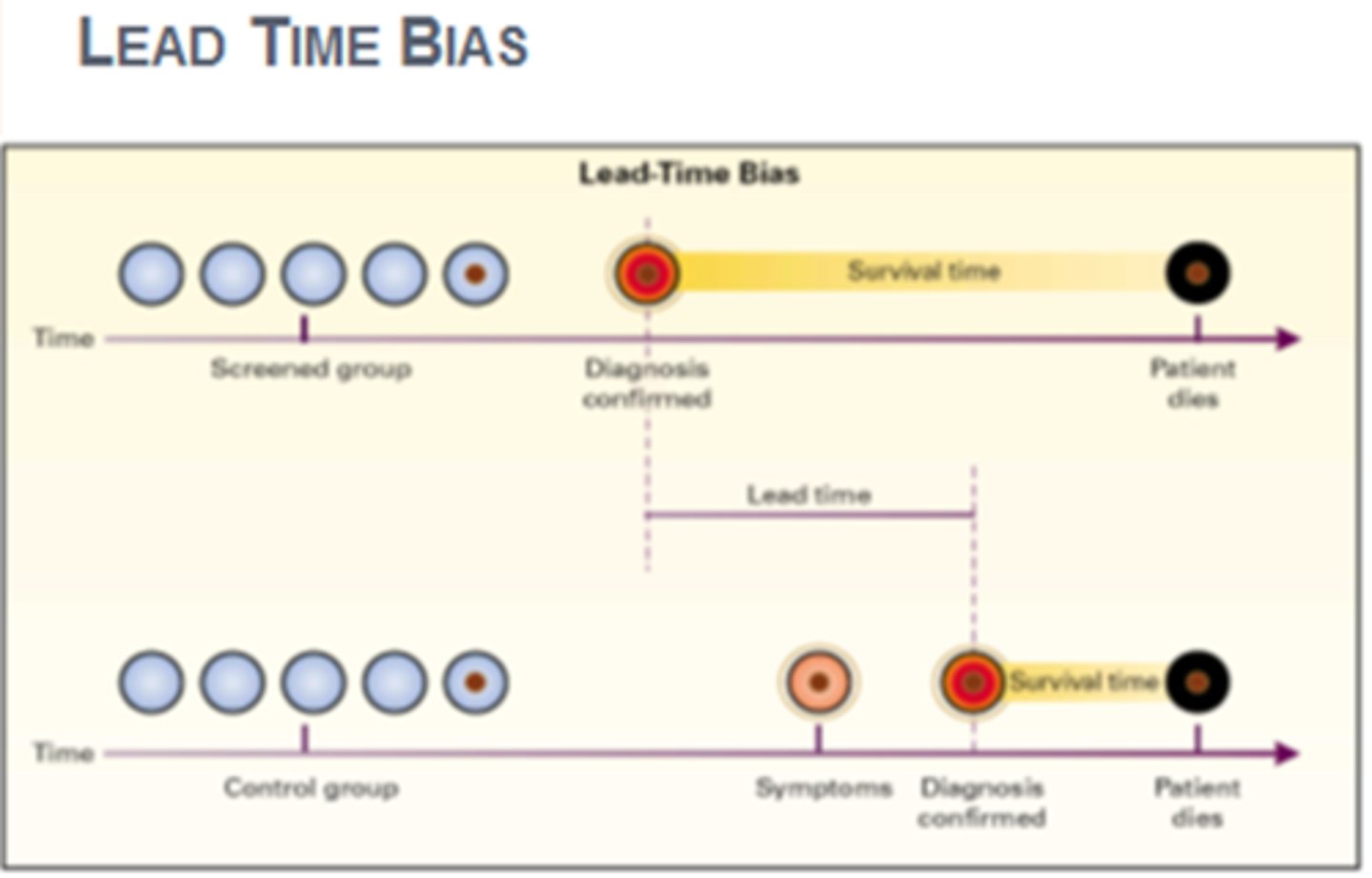
What is lead time bias?
Bias introduced when screening detects a disease earlier and thus lengthens the time from diagnosis to death, falsely increasing survival rate
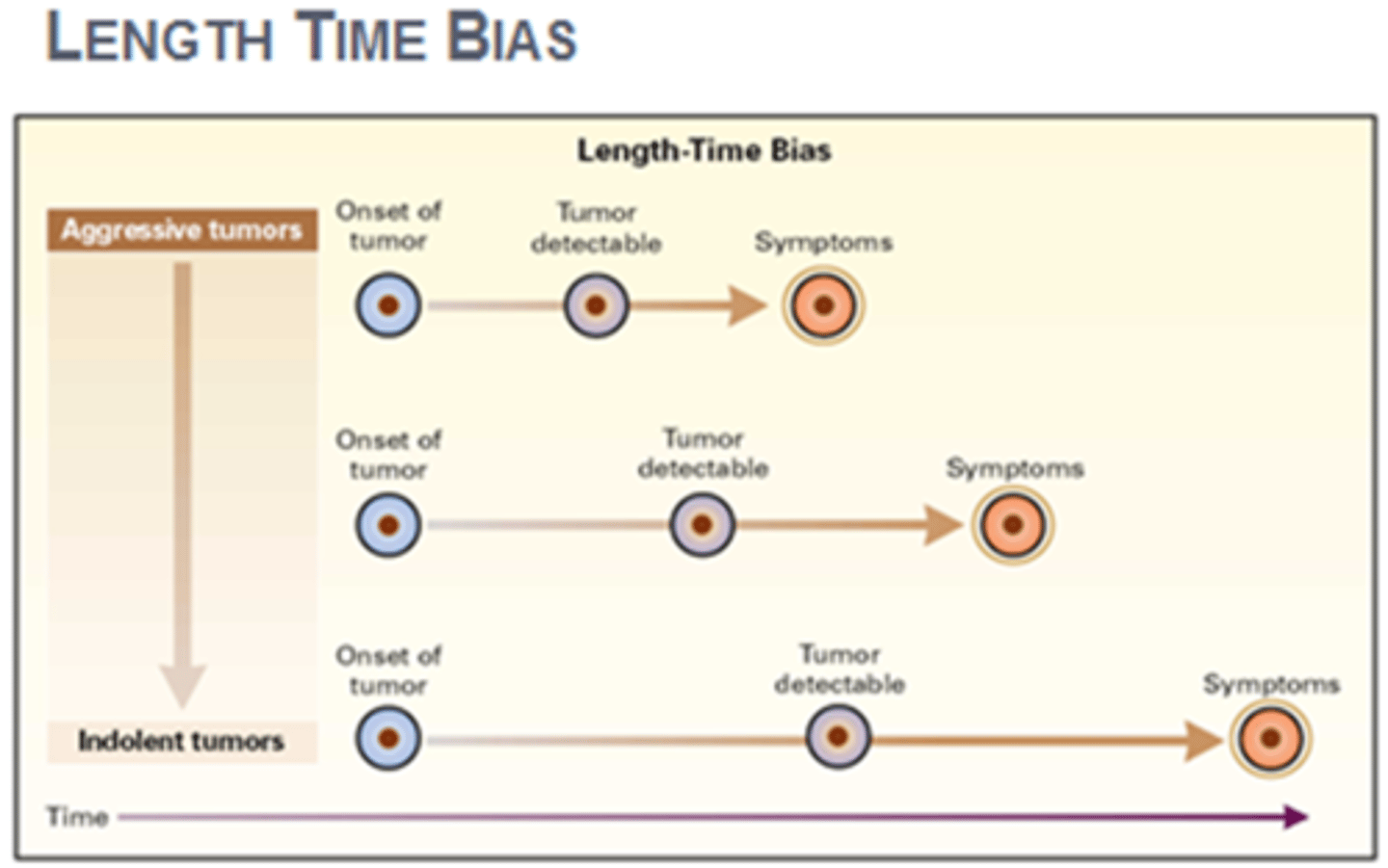
What is Length time bias?
Bias introduced when screening detects asymptomatic (slower/less aggressive) cases that may not usually be picked up, falsely increasing survival rate
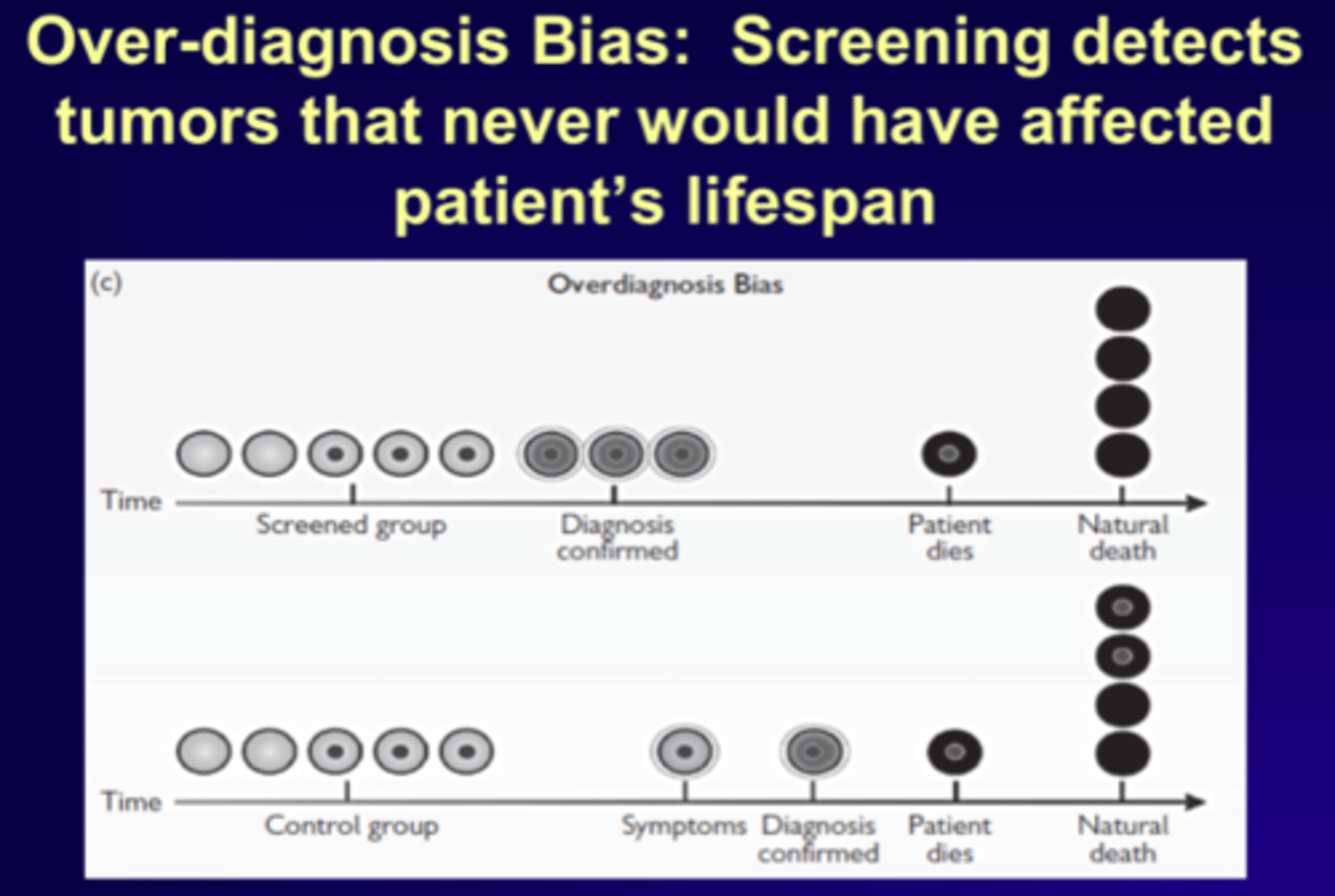
Over diagnosis in screening
Refers to screen-detected cancers that are either:
- Non-growing/progressive
- Growing very slowly
These Cancers are not expected to cause medical problems in lifetime and therefore result in treatment when not needed.
Who is less likely to engage with screening? (4)
• Low socio-economic status/living in deprivation (inverse care law)
• Ethnic minority groups/migrants
• Transgender
• Disabilities
Reliability vs validity
Reliable (consistency)
- Repeated measurements (over time or by different observers) are similar
Valid (accuracy)
- Does is correlate with what we are trying to measure? (for the individual or for the group)
What is sensitivity in a test?
Sensitivity refers to the proportion of affected individuals correctly identified by the test (How good the test is at finding disease)
= True positives/all affected (TP +FN)
How to increase sensitivity in a test? + consequences
DECREASE the cutoff score.
• Good because More people with disease would be flagged for treatment
but
• Bad because More people without disease would also be flagged/unnecessarily treated
What is specificity in a test?
Specificity refers to the proportion of unaffected individuals correctly identified by the test (how good the test is at excluding disease)
= true negatives/ all unaffected (TN + FP)
How to increase specificity in a test? + consequences
To maximise Specificity you would INCREASE the cutoff score. Consequences:
• Good because fewer people without disease would be flagged for treatment
but
• Bad because fewer people with disease would also be flagged
What is a positive predictive value ? + formula
predicts how often positive results are correct (% of people with a true positive result)
= true positives/test positives (TP +FP)
What is a negative predictive value ? + formula
predicts how often negative results are correct (tells us the chance that the patient does not have the condition if the diagnostic test is negative)
= true negatives/test negatives (FN+TN)
Likelihood ratio for a positive result of a test formula
LR positive result
= sensitivity/(1-specificity)
Likelihood ratio for a negative result of a test formula
LR negative result
= (1-sensitivity)/specificity
medical pluralism
the adoption of more than one medical system in terms of health beliefs, behaviours, treatments, or institutions eg combining biomedicine with traditional/ alternative medicine
Overall functions of the clinical record (4)
• Support Patient Care
- Record of contact
- Facilitate communication if transferring
• Improve Future Patient Care
- Training of clinicians
- Audit
- Financial planning
- Management
- Research
• Social purposes- request of patients and other bodies (social services, police etc)
• Medico-legal document- supports both patient and practitioner
Clinical purpose of the patient record when handing over
• Support method of, and structure to, history and examination
• Ensure clarity of diagnosis
• Record treatment plans (hold clinicians accountable)
• Record results/investigations( able to monitor trends easily)
• Enable comprehensive monitoring
• Help maintain a consistent explanation for the patient
• Ensure continuity of care- handovers and transfer of records
• Storage for correspondence
Emerging purposes of the clinical record
- A shared record dependent on messaging such as with
pathology or some electronic prescribing systems
- New requirements for patients to have increasing control of
their health records e.g MYnhs
Non clinical purposes of the patient record
• Providing medico-legal evidence
• Providing legal evidence in respect of claims by a patient against a third party
• Providing reports and information for third parties-think insurance companies!
• To support claims for benefits and other additional social support
What things to include in a clinical record? (for an appointment)
• Presenting symptoms and reasons for seeking health care
• Relevant clinical findings
• Diagnosis and important differentials
• Options for care and treatment (including safety netting)
• Discussion about risks and benefits of care and treatment
• Decisions about care and treatment
• Action taken and outcomes
Pros and cons of handwritten/paper records
Pros
- Functional
- Portable
Cons
- Legibility issues
- Structural issues
- must be dated and signed
Pros and cons of digital records
Pros
- Problem orientated
- Audit trail®
- Searchable
- safer prescribing
- has reminders for patient follow ups (risk management)
Cons
- Open to ransomware attack - Wannacry
2017③
• 111 outage 2022⑤
What is the use of records in audit, research and management?
- Support clinical audit
- Facilitates clinical governance
- Facilitates risk management
- Support clinical research
How can records be used for risk management?
• Prescription alerts
• Reminders 'pop-ups'
• Pre-set algorithms
• Continuity of care
What is an adverse event? + examples
An unintended event resulting from clinical care and causing patient harm:
•Wrong site surgery
•Medication errors
• Pressure ulcers
•Wrong diagnosis
•Failure to treat
•Patient fall
•Hospital acquired infection
• Medicine adverse effects (side effects)
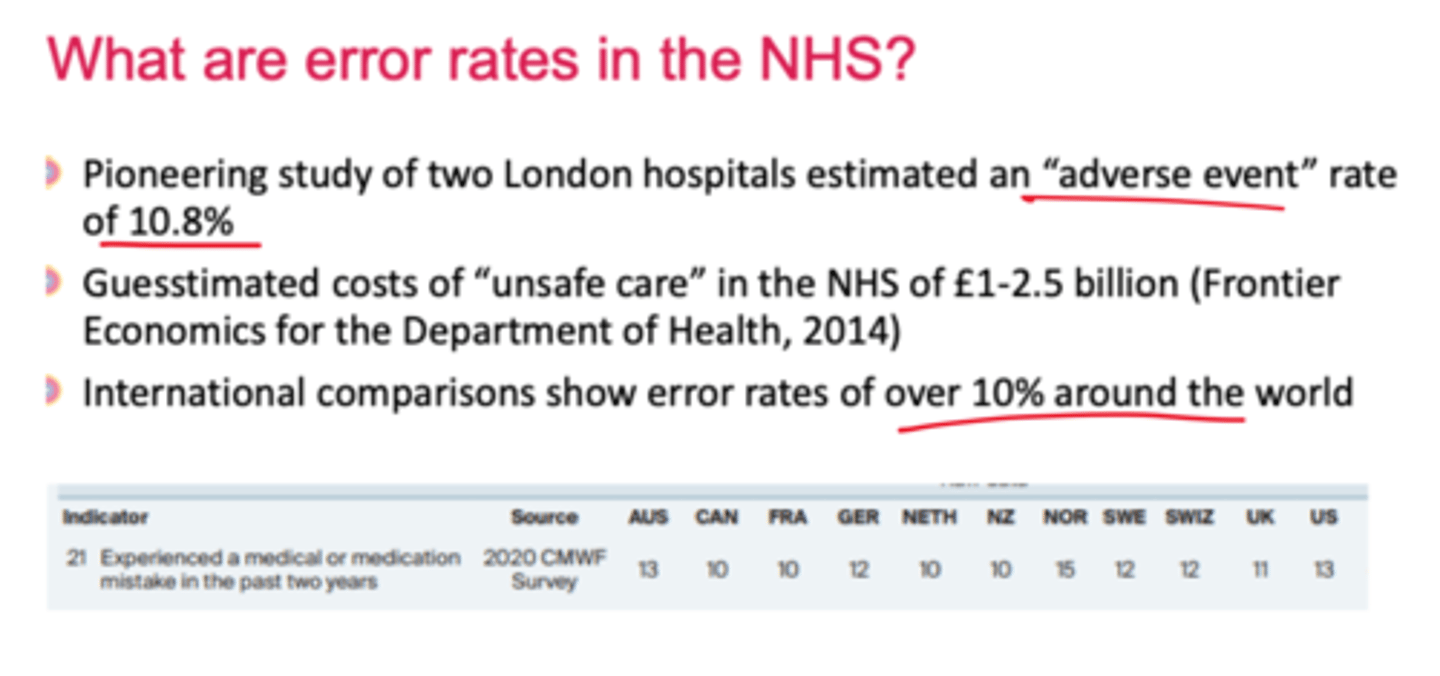
Adverse event rates in the UK
10.8%
What is a serious incident?
Events where the potential for learning is so great, or the consequences to patients, families and carers, staff or organisations are so significant, that they warrant using resources to investigate and act.
what are never events?
Never Events are serious incidents that are entirely preventable because guidance or safety recommendations providing strong systemic protective barriers are available at a national level, and should have been implemented by all
healthcare providers.
What is a near miss?
A situation in which events or omissions, arising during clinical care fail to develop further, whether or not as the result of compensating action, thus preventing injury to a patient. Have to Tell the national reporting and learning system.
How do we know if a hospital is safe?
•Hospital mortality data
•Data on other measures of safety
• Reports of Never Events and Serious Incidents
• NHS safety thermometer
• Patient safety dashboards
• Monitoring and inspections by regulators
• Care Quality Commission (CQC);
• NHS Improvement
Latent conditions/errors vs active failures in hospital
• Latent conditions are usually long standing and unnoticed until they combine with other factors or active failures to
cause an adverse event e.g poor staffing of pharmacists on ward, env. conditions
• Active failures are when an act (unsafe) is directly linked to accident e.g overprescribing a dose
What is Normalisation of deviance?
Failings because staff become blind to what is going on
around them, assuming that the practices being
tolerated are normal (e.g. Mid Staffs)
2 Types of active failures when treating
• Errors via lack of knowledge of:
> Knowledge
> Rules
> Skills
• Violations - knows what to do but chooses otherwise.
4 types of violation (active failure)
• Routine: a violation that has become normal behaviour within a peer group.
• Situational: context-dependent (e.g. time-pressure,
lack of supervision, low staffing).
• Reasoned: deliberate deviation from protocol
thought to be in patient's best interest at the time.
• Malicious: deliberate act intended to harm.
What does the Human factors approach acknowledge in regards to error?
o the universal nature of human fallibility (tendency to make mistakes)
o the inevitability of error
o that error is not necessarily due to incompetence
Who are Healthcare Safety Investigation Branch?
Investigates safety incidents each year in order to provide safety recommendations and share lessons across the whole of the healthcare system.
How to increase safety/minimise errors in healthcare? (8)
1. Avoid reliance on memory
2. Make things visible
3. Review and simplify processes
4. Standardise common processes and procedures
5. Routinely use checklists
6. Decrease the reliance on vigilance
7. Promote hand hygiene and infection control
8. Increase Dr:patient ratio
What to do when an adverse event occurs? (5)
• Report it (incident reporting systems)
• Assess its seriousness
• Analyse why it occurred (Root Cause Analysis)
• Be open and honest with the affected patient and
apologise - Duty of Candour - legal duty
• Learn from the event and put in place actions to reduce
risk of repeat.
A good example of minimising error in healthcare
Surgical safety checklist reduced postoperative complications & death by more than 33%
How the right to an open future relates to IVF
The right to an open future: dilemmas should be resolved so as to ensure that children will have a maximally open future, i.e., will enjoy the widest possible range of opportunities.
(Important in embryo selection in IVF)
Human Fertilisation and Embryology Act (1990) welfare criterion
stated 'A woman shall not be provided with [fertility] treatment services unless account has been taken of the welfare of any child who may be born as a result of the treatment (including the need of that child for a father)'
Human Fertilisation and Embryology Act (1990) welfare criterion criticisms (3)
1. fertile couples don't have to meet this criterion.
2. Predicting the welfare of future children is very
difficult
3. research suggests not the case that a father is always required for a child to flourish.
Reply
• Human Fertilisation and Embryology Act (2008) replaces
"the need for a father" with "the need for supportive parenting".
The pro-life argument
1. Abortion ends the life of a fetus
2. Human fetus has the same moral status as a person
3. It is wrong to end the life of person/a creature with the moral status of a person
Therefore, abortion is morally wrong
Argument against the pro life arguments
'Human fetus has the same moral status as a person', but they don't because they have no rationality, characteristics, subconsciousness etc
What is Gillick competence?
Children (under 16) can consent to medical treatment if deemed competent by medical professional and if they fully understand the proposed treatment. (without need for parental permission or knowledge)
When is gillick competency only valid?
if it is given voluntarily and not under influence or pressure by anyone else
Fraser guidelines (5)
Guidelines which advise that it is lawful to provide contraceptive advice and treatment without parental consent, providing the following criteria are met:
o the young person will understand the professional's advice and the implications of the treatment
o the young person cannot be persuaded to inform their parents
o the young person is likely to begin, or to continue having, sexual intercourse with or without contraceptive treatment
o if their physical or mental health, or both, are likely to suffer if not given treatment
o the young person's best interests require them to receive contraceptive advice or treatment with or without parental consent.
Arguments for IVF (4)
- procreative autonomy (right to have baby)
- provides a valuable option for couples struggling with infertility
- Concerns welfare interests. (i.e pre implantation genetic diagnosis)
- enables same-sex couples and single individuals to have biological children
What is pre-implantation genetic diagnosis and what are the associated ethical issues?
- Genetic profiling of embryos prior to implantation
(as a form of embryo profiling), and sometimes
even oocytes prior to fertilisation
- Can be used for avoiding genetic diseases
- Issues - sex selection, saviour siblings - 'Designer
babies'
Arguments against IVF
- destruction of embryos
- harmful to those trying to conceive e.g MBR
- is unnatural
- can be expensive, limiting access for some individuals or couples, creating disparities in who can afford the treatment.
- IVF process can be emotionally and physically demanding, with potential for stress, disappointment, and side effects from fertility medications.