T1 DHP1 1036DOH (only do starred cards)
1/418
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
419 Terms
acquired pellicle
A colourless, acellular film composed of complex sugar-protein molecules in saliva. forms normally on the teeth within minutes of cleaning.
properties of acquired pellicle (dimensions, where on teeth, where thicker?)
- 0.1 to 0.8 nanometers
- forms on exposed tooth surfaces, restorations and on calculus
- thicker near gingiva
dental biofilm/plaque biofilm/microbial dental plaque definition
dense, non-mineralised complex mass of bacterial colonies in a gel-like intermicrobial matrix
(simpler terms: A thick, soft cluster of bacteria living together in a sticky, gel-like substance)
dental biofilm/plaque biofilm/dental plaque properties
- adheres firmly to acquired pellicle, teeth, calculus, fixed + removable restorations
- microorganisms other than bacteria can be found
- not visible with the naked eye
- removed by brushing and flossing
stages in biofilm formation
- pellicle forms
- bacteria attach to pellicle
- bacteria grow, multiply
- biofilm matures (inc. in mass + thickness)
- matrix forms (mixture or microorganisms)
- discontinued oral hygiene practice continues
- bacteria numbers increase rapidly
dental biofilm significance
1. Initiation and progression of dental caries and periodontal disease
2. The pathogenic microbes are transmissible + infectious
3. Formation of calculus initiated

what is the periodontal ligament? what is its function?
a layer of soft connective tissue that covers the root of the tooth and attaches the tooth to the bone of the tooth socket
suspends and maintains tooth in socket
what is cementum? what is its function?
a thin layer of hard, mineralised tissue that covers the surface of the tooth
anchors end of PDL fibres to tooth to stay in socket, protect dentin
what is alveolar bone/alveolar process? what is its function (just need one answer for this)
bone of the upper or lower jaw that surrounds and supports the roots of the teeth
gingiva function
a seal around the cervical portion (neck) of the tooth
Holds the tissue against tooth during mastication
gingival sulcus and junctional epithelium definition
GS: space between free gingiva and tooth surface
JE: forms base of sulcus and joins gingiva to tooth
what is gingivitis?
bactieral infection of gingiva
damage to gingival tissue
REVERSIBLE
clinical characteristics of gingiva
colour
contour
consistency
bleeding on probing
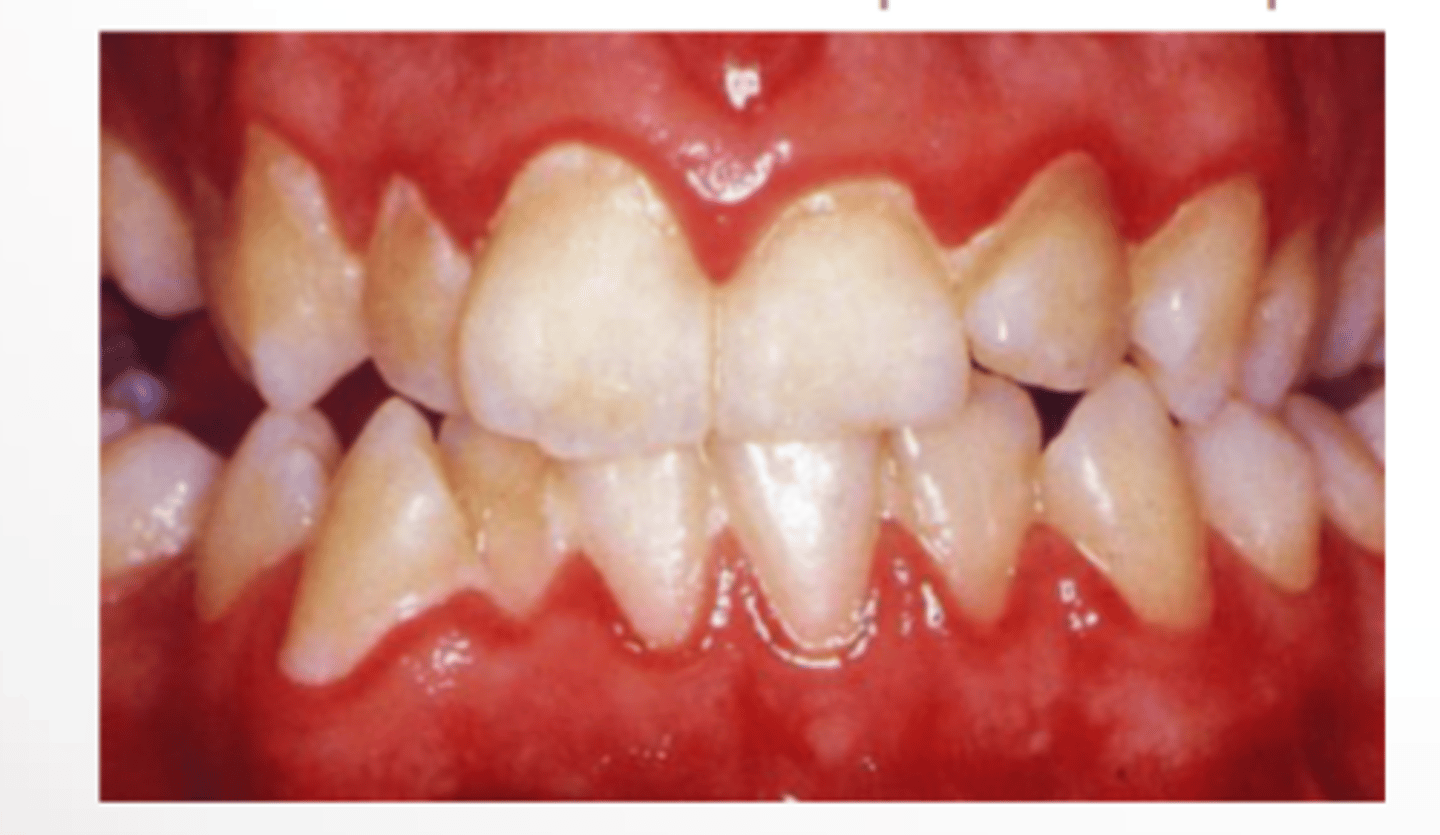
healthy v diseased gingiva in relation to clinical characteristics: colour, contour, consistency and bleeding on probing
COLOUR
healthy - pale, pink
diseased - dark or bright red
CONTOUR
healthy - interdental papillae pointed, knife edge margin
diseased - bulbous interdental papillae, rounded margin
CONSISTENCY
healthy - firm, stippling
diseased - soft, loss of stippling, smooth, shiny
BLEEDING
bleeding present - sign of gingival inflammation/disease
why is bleeding important for examining gingiva
healthy gingiva doesnt bleed
early sign of gingival inflammation, because it precedes colour change and enlargement
important for treatment planning, instruction and motivation
gingival bleeding indices
Gingival Bleeding Index (GBI)
use floss
Eastman interdental bleeding index (EIBI)
wooden interdental cleaners
Gingival index (GI)
mouth mirror and periodontal probe
periodontal disease primary risk factors, local and systemic contributing factors and host response to biofilm bacteria
PRF
dental biofilm
LCF
increases plaque pathogenicity and retention
SCF
conditions, habits (smoking), diabetes (increase susceptibility)
HRTBB
body’s response to infection, immune system
periodontal disease
bacterial infection of periodontium
occurs in kids and adults
IRREVERSIBLE
affects tissues that support teeth: gingiva, perio ligament, bone, cementum
clinical signs of perio disease
pockets
bone loss
loss of attachment
gingival recession
furcation
four phases of treatment for periodontal disease
preliminary phase
assessment and data collection/evaluation
hygienic phase (non surgical therapy)
patient education
scaling/polishing, debridement
corrective (surgical phase)
implants, bone grafts, crown lengthening, gingivectomy
maintenance therapy
regular assessment
patient education
scaling/perio debridement
hygienic phase of perio therapy aims
interrupt/stop progress of disease
allow tissue to heal and resolve inflammation
postpone disease reoccurence
motivate patient
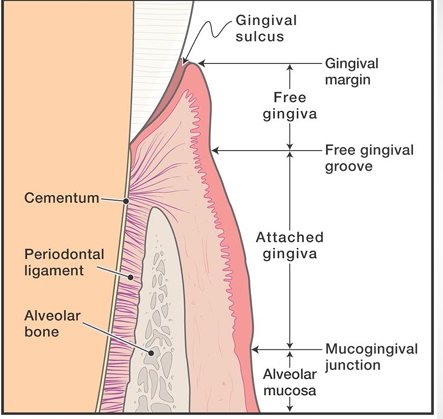
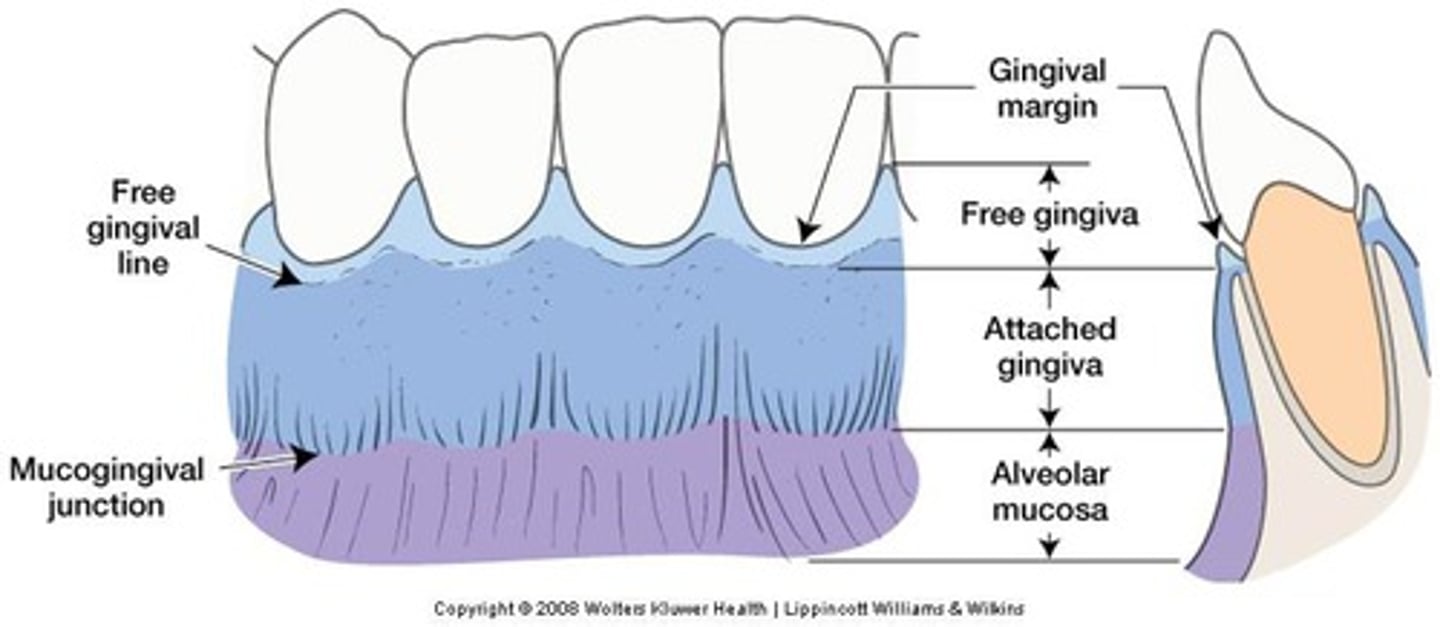
look at this diagram
supragingival plaque (where on tooth, what attracted to it, occurs on where?)
- coronal to margin of free gingiva
- micro-organisms from saliva selectively attracted to pellicle
- occurs on rough surfaces of teeth, restorations, malpositioned teeth and carious lesions
how does plaque form?
bacteria fed by sugar in the food
bacteria rich plaque converts sugar to acid
acid attacks tooth, eventually causing demineralisation
this appears as whitish areas on the tooth
if it isnt removed, it continues to attack the tooth and will cause decay
preventive dentistry
Goal is that each individual maintains optimal oral health
• Brush and floss daily
• Disclose periodically to evaluate effectiveness
• Follow a fluoride program while teeth are developing, includes professional applications
• Schedule regular dental visits, examination, scale and polish and necessary treatment
what is demineralisation?
Demineralization happens when acids from bacteria dissolve the minerals in enamel and dentin, weakening it. These bacteria feed on sugars (fermentable carbohydrates) and produce acids as a result.
If the teeth are exposed to these acids too often, demineralization can happen faster than the teeth can repair themselves (remineralisation). Over time, this leads to a hole in the tooth called a cavity (cavitated carious lesion).
subgingival plaque (what, where)
- apical to margin of free gingiva (beneath gingival margin)
- down growth of bacteria from supragingival plaque
- pocket holds plaque against tooth
- can occur in overhanging margins of restorations
clinical aspects of dental plaque/biofilm (distribution and detection)
DISTRIBUTION
location
surfaces
factors influencing plaque accumulation
DETECTION
direct vision
use of explorer/probe
disclosing agent
clinical record
distribution of dental plaque/biofilm LOCATION and SURFACES
- supragingival, gingival, subgingival and fissures
- proximal surfaces, gingival third of crown, (least on palatal surfaces of maxillary teeth bc activity of the tongue)
physical factors influencing plaque/biofilm accumulation
- crowded teeth
- rough surfaces
- areas difficult to clean (overhanging restorations, under calculus ledges, caries)
- POOR SELF CARE/PLAQUE CONTROL
direct vision detection of plaque
- thin plaque (translucent + invisible)
- stained plaque (yellow, green, tobacco)
- thick plaque, tooth appears dull, dingy and matted-fur like
use of explorer when detecting plaque
- tactile examination, surface somewhat slippery
- removal of plaque - removed when explorer passed over tooth surface, should adhere to it
disclosing agent when identifying detection of plaque important note!
- do not apply until evaluation of oral mucosa and gingival colour recorded
clinical record for plaque
index or plaque score
kept for comparison purposes
plaque evaluation included in complete charting and oral examination
quantitative evaluation of plaque disclosing
- solution (professional use)
- tablets (home use)
qualitative evaluation of plaque disclosing
- GC triplaque
- select area, professional use only, difficult to remove
what are plaque indices?
- used to make clinical record of plaque/biofilm present
name plaque indices
- silness and loe (thickness of plaque, six teeth only, quick)
- o'leary, drake and naylor (ONE WE USE - measures plaque present, individual tooth surfaces)
- grant, stern, everett (plaque FREE score, all teeth)
- podshadley and haley (extent of plaque and debris)
- greene, vermillion and greene (assesses cleanliness, debris/calculus)
calculation of plaque according to o'leary drake and naylor plaque
number of teeth present x 4 = total number of available tooth surfaces
% with plaque = (number of surfaces w. plaque x 100) / total number of available tooth surfaces
significance of dental biofilm/bacterial plaque
- initiation and progression of dental caries and periodontal disease
- particular groups of microorganisms associated with certain infections
- formation of calculus
- oral cleanliness
- accumulation on teeth/tongue (halitosis/ unpleasant appearance)
what is material alba?
- loosely adherent mass of bacteria on top of dental plaque
- indicative of plaque removal neglection
- bulky and soft, white/grayish white and resembles cottage cheese
dental calculus characteristics
- mineralised dental biofilm
- hard, tenacious deposits
- CANNOT BE REMOVED WITH BRUSHING AND FLOSSING
- forms on natural teeth, implants, restorations, dentures etc
- external surface is a living layer of bacterial plaque
3 basic steps of calculus formation
1. pellicle formation
2. biofilm formation
3. mineralisation (supra and subgingival basically same)
calculus detection supragingival
visual examination (beneath gingival margin/underneath, not adapting closely to tooth surface, dry tooth surface, change in gingiva colour)
tactile examination (periodontal probe, explorer)
supragingival calculus characteristics and common sites
- above gingival margin
- white/beige
- may be discoloured
- lingual aspect of mandibular anterior teeth
- buccal surfaces of max. molars
- crowded teeth
subgingival calculus characteristics
- beneath gingival margin
- detected by tactile means (probe)
- brown/black
- localised
- heaviest in mesial/distal surfaces
subgingival calculus detection
VISUAL EXAMINATION
- at edge/beneath gingival margin
- margin not adapting closely to tooth surface
- air blast - deflect margin
- change in colour of gingival tissue
- transillumination
TACTILE
- periodontal probe
- dental floss
- explorer
significance of calculus
- Key in gingival and periodontal infections
- Drives inflammatory periodontal disease progression
- Disease-causing bacteria thrive on rough calculus surfaces:
-- Supragingivally for gingivitis
-- Subgingivally near pocket lining for periodontitis
- Daily biofilm control by patients and professional calculus removal can reduce gingival inflammation.
food debris (remember ilcopo)
- increased bacterial activity
- large embrasures
- carious lesions
- overhanging restorations
- partially erupted teeth
- orthodontic appliances
what is the most common carie causing bacteria?
- streptococcus mutans
you need all 4 factors to get a dental carie. what are these factors? (remember Mc st - yk like mc street)
1. microorganisms
2. cariogenic diet
3. salivary factors
4. tooth resistance
types of dental caries
- pit and fissure
- smooth surface
- early childhood caries
- root caries (if root surface exposed, cementum is softer than enamel so higher risk)
what is fluoride? what does it do on tooth surfaces?
- F- chemical ion found in earth crust
- naturally occuring amount depends on type of soil and rock the water drains through
- fluoride on tooth surfaces prevents and treats early signs of decay
fluoride is made available at the tooth surface by two means:
1. systemically (pre-eruptive exposure - by circulation)
2. topically (directly to exposed surfaces of erupted teeth - post-eruptive exposure)
topically applied fluorides can be swallowed during tooth development to provide both...
1. pre-eruptive (during developing teeth of young children exposure)
2. post-eruptive (after teeth enter oral cavity)
according to epidemiologic evidence, maximum caries inhibiting effect occurs when there is...
1. systemic exposure before tooth eruption
2. frequent topical exposure throughout life
levels of carie prevention
1. primary prevention (measures used so disease doesn't occur (like water fluoridation)
2. secondary prevention (treatment of early disease, prevent progression of potentially irreversible conditions (eg topical application))
3. tertiary prevention (replace lost tissues, rehabilitate oral cavity to function as near to normal as possible - (eg replacement missing teeth)
fluoride metabolism (remember FADE)
1. fluoride intake (water, food, brushing, rinses etc)
2. absorption (through GI tract, blood stream etc)
3. distribution and retention
4. excretion
fluoride intake step of fluoride metabolism
- can get taken in via food, water, dietary supplements
- varying amounts ingested from differing sources
absorption step of fluoride metabolism
gi tract and bloodstream
GI TRACT
- rapidly absorbed by passive diffusion as hydrogen fluoride (HF)
- rate and amount depends on gastric acidity and solubility of fluoride compound
- most that isn't absorbed in the stomach - absorbed by small intestine
- less absorption when taken with milk/other foods
BLOOD STREAM
- plasma carries iodine monofluoride (FI) for dist. and elimination throughout the body
- maximum blood levels reached ~30min after intake
- normal plasma levels are low, rise and fall according to intake
distribution and retention of fluoride metabolism
- plasma distributes F to all tissues and organs
- 99% fluoride located in mineralised tissues (bone)
- [ ] fluoride highest at surfaces next to tissue fluid supplying fluoride
- once enamel fully matured, the fluoride deposited during development can ONLY be altered by dental caries, erosion or mechanical abrasion
excretion step of fluoride metabolism
- excreted through kidneys mostly in urine
- limited transfer from plasma to breast milk for excretion by that route
three stages of tooth development and fluoride
1. pre-eruptive (mineralisation stage)
2. pre-eruptive (maturation stage)
3. post-eruptive
pre-eruptive mineralisation stage of fluoride and tooth development
-F ions replace hydroxyl ion in hydroxyapatite crystalline structure in enamel
-this is fluorapatite - more resistant to acid attack
- results in development of shallow occlusal grooves (reduces risk of fissure caries)
- F available to developing teeth by blood plasma to tissues surrounding tooth buds
pre-eruptive maturation stage of fluoride and tooth development
- after mineralisation complete and before eruption date, F deposition continues in enamel surface
- F taken up from tissue fluids surrounding tooth crown
- more F acquired by outer surface than underlying layers
post-eruptive stage of fluoride and tooth development
- continues from eruption throughout lifespan of the teeth
- [ ] F on outermost surface of enamel dependent on topical sources of F (dentrifices, fluoridated water, mouthrinses etc)
- continuous presence of F can inhibit carie progression
- uptake most rapid on enamel surface during first years of eruption
what is dental fluorosis? what are its effects?
- form of hypomineralisation
- cumulative rather than threshold
- during mineralisation, enamel highly receptive to free F ions
- results from systemic ingestion of excessive amounts of fluoride during tooth development
- normal activity of ameoblasts may be inhibited - can result in discontinuity of crystal growth
- can appear clinically in varying degrees
in dentin, where is the highest concentration of fluoride?
at the pulpal surface, until after recession of perio. attachment when root surface exposed to oral cavity
fluoride uptake depends on two things, what are they?
- level of fluoride in the oral environment
- length of time of exposure
why would demineralised enamel that remineralised in the presence of fluoride have a greater concentration of it than sound enamel?
- hypomineralised enamel absorbs fluoride in greater quantities than sound enamel
what two things in the oral cavity are reservoirs for fluoride?
saliva and biofilm
criteria for water fluoridation and compounds used
1. solubility in water
2. inexpensive
3. readily available
compounds: (solid) sodium fluoride, sodium silico-fluoride, (liquid) hydrofluorosilicic acid
benefits of water fluoridation
1. topical source of fluoride on erupted tooth surfaces throughout life
2. dominant role in decline of prevalence and severity of dental carie rates (27%)
three basic topical effects of fluoride to prevent dental caries: (inhibit, enhance, inhibit)
1. inhibit demineralisation
2. enhance remineralisation of lesions
3. inhibit bacterial activity by inhibiting enolase (enzyme needed by baccys to metabolise carbs)
clinically, you should document (fluoride)
1. caries risk level
2. current use of fluoride toothpaste and exposure to fluoridated water
3. type, [ ], mode of delivery and postoperative instructions of professional topical fluorides provided
4. type, amount and instructions for use of prescription/over-counter patient applied fluoride products recommended
the benefits of using toothpastes may be ____________, ___________ or _______
preventive, therapeutic or cosmetic
why would you use toothpaste?
- application of therapeutic agents
- superficial cosmetic effects
- reduction of biofilm and gingivitis
- prevent dental caries (remineralisation of early non-cavitated ones too)
- reduction of dentin hypersensitivity
- reduction of supragingival calculus formation
name different types of fluoride
- stannous fluoride
- sodium fluoride
- sodium monofluorophosphate
what agents would you use for reduction of biofilm formation? why?
zinc citrate and zinc chloride (triclosan was used but banned for environmental effects)
used to prevent attachment of bacteria to tooth surface
for in-home treatment of dentin hypersensitivity (the first intervention for this), what chemicals should you administer?
- potassium nitrate
- sodium fluoride
- pro-arginine formula
for supragingival calculus formation, what toothpastes would help inhibit it and what would it contain?
- tar-tar toothpastes
- zinc salts (zinc Cl and zinc citrate), pyrophosphate salts
removal of extrinsic stain on tooth surface is dependent on two things...
- mechanical removal of stained biofilm
- delivery of bleaching agent
for halitosis, certain ingredients can reduce malodor by inhibiting the production of VSC. what is VSC? what ingredients would do this?
- VSC = volatile sulfur compounds
- chlorhexidine, CPC and zinc formulations would reduce VSCs
- stannous fluoride with sodium hexametaphosphate would too
what are the most common ingredients in a toothpaste?
- abrasives
- humectants
- water
- all 20-40% prevalent
approximately how much of the formulation will the active ingredient take up?
1.5-2% of formulation
name one active ingredient for each of these therapeutic benefits:
antibiofilm/antigingivitis:
anti calculus:
desensitizer:
oral malodor:
AB/AG: stannous fluoride
AC: tetrapotassium pyrophosphate
D: arginine
OM: essential oils
detergent in toothpaste benefits, give an example
- lower surface tension
- loosen surface deposits
- contribute to foaming action
- example is sodium lauryl sulfate (SLS)
abrasives purpose in toothpastes, give 2 examples
- cleaning and polishing agent
- polishing = smooth tooth surface (prevent/delay accumulation of stains and deposits)
- examples: silicates, calcium carbonate
what is the RDA?
relative dentin abrasion values for a common toothpaste range, from:
0-70: low
70-100: med
100-150: high
150-250: harmful
binders (thickeners) purpose in toothpastes. give 1 example
- stabilise formulation
- prevent separation
- example: seaweed colloids
humectant purpose in toothpastes, give 1 example
- retain moisture and prevent hardening on air exposure
- glycerol, xylitol, sorbitol
preservatives in toothpastes purpose, give 1 example
- prevent bacteria growth, prolong shelf life
- alcohol
flavouring agents in toothpastes purpose, give examples
- mask ingredients that may have unpleasant flavour, or for patient acceptance
- essential oils (wintergreen, clove, cinnamon)
- xylitol, glycerol, sorbitol
consideration for selection of toothpastes for paediatric patients
- birth to tooth eruption: parents clean child's gingiva with soft infant toothbrush
- eruption of first tooth: start brushing 2x daily, soft age appropriate toothbrush
- 2-5 yr old: pea-sized amount of toothpaste >3 yrs, MUST SUPERVISE, spit out and don't swallow toothpaste
name a high fluoride toothpaste
neutrafluor 5000
whitening toothpastes
oral b 3d white
colgate optic white
children’s toothpaste active ingredients and mode of action
AI
sodium fluoride 500 ppm
MOA
sodium fluoride - reduces caries risk by inhibiting demineralisation and promoting remineralisation
tooth mousse
active ingredient: 0.2% 900ppm CPP/ACP + fluoride
prevent dental caries
prevent ortho-related demineralisation
erosion protect
dentin hypersensitivity