The Immune System
1/34
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
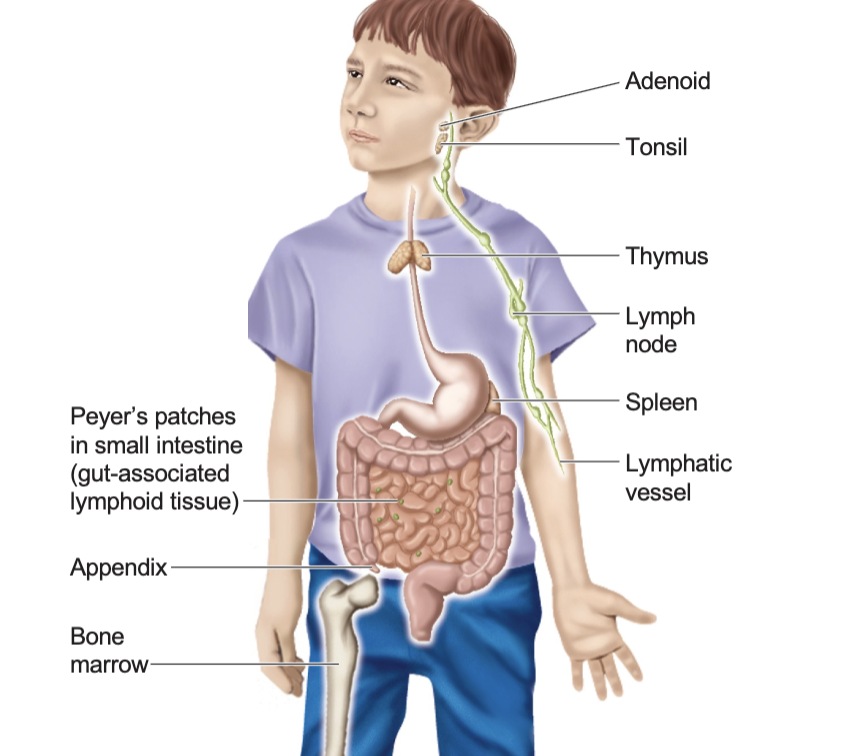
Anatomy of the immune system
Adenoid
Tonsil
Thymus
Lymph node
Spleen
Lymphatic vessel
Peyer’s patches in the small intestine
Gut associated lymphatic tissue
Appendix
Bone marrow
What cells make up the immune system?
Leukocytes, aka white blood cells
Two broad categories
Lymphoid Cells
Myeloid Cells
Lymphoid Cells
T lymphocytes
B lymphocytes
Natural killer cells
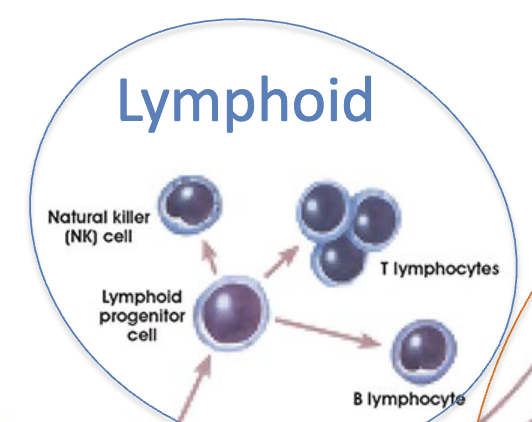
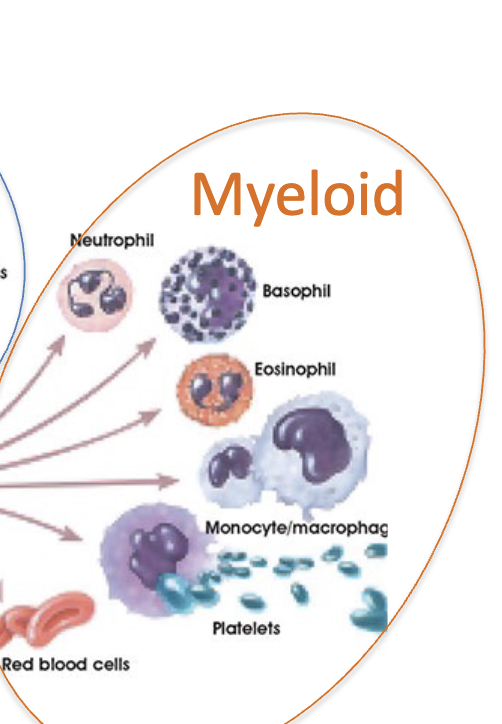
Myeloid Cells
Monocytes (blood)
Macrophages (left the blood and entered tissue)
Granulocytes
Precursors for red blood cells/ platelets
Hematopoietic cells from bone marrow in long bones and hip bones…
Differentiate into lymphoids and myeloids
T Lymphocytes (T Cells)
Originate in the Thymus
Necessary for cell-mediated immunity
Uses T cell receptors
B Lymphocytes (B Cells)
Originate in the Bursa of Fabricius in birds, Bone Marrow in humans
Necessary for humoral (soluble) immunity
Uses B cell receptors (antibodies)
Macrophages (Monocytes in blood)
Professional phagocytic cells
Scavenge our tissues in search of pathogens (dead cells and other debris)
Tissue maintenance
Granulocytes
Different types
Neutrophilic
Eosinophilic
Basophilic
Mast cells
Professional phagocytic cells that release the contents of their granula as part of their specific immune response
Innate Immune Cells
Natural killer cells
Neutrophils
Basophils
Eosinophils
Monocytes/ macrophages
Acquired Immune Cells
T cells
B cells
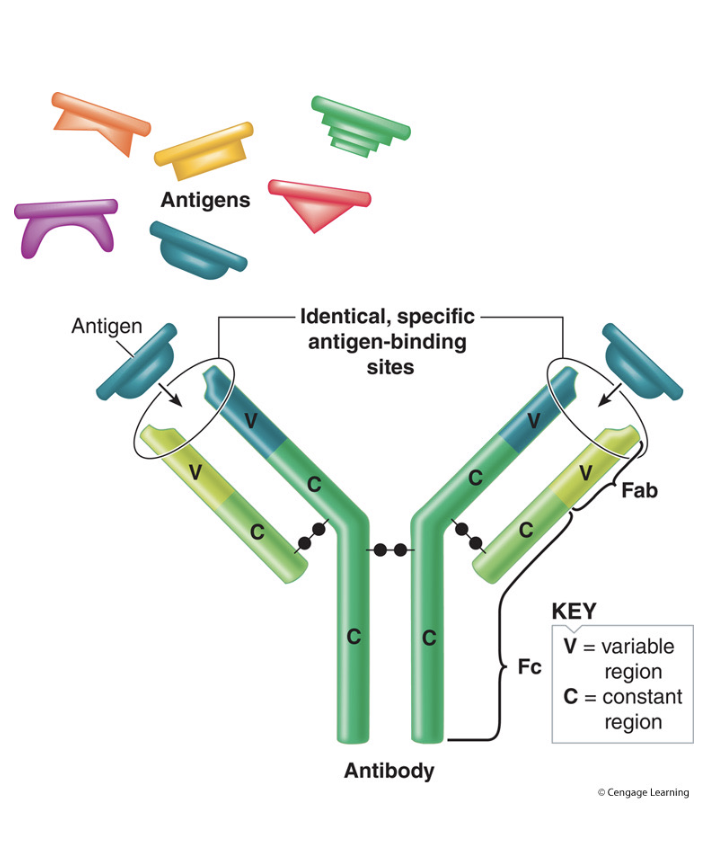
Anatomy of B Cells
2 heavy chains and 2 light chains linked by disulfide bonds
Constant domain determines antibody properties
Tip of the variable domain provides the antigen binding site
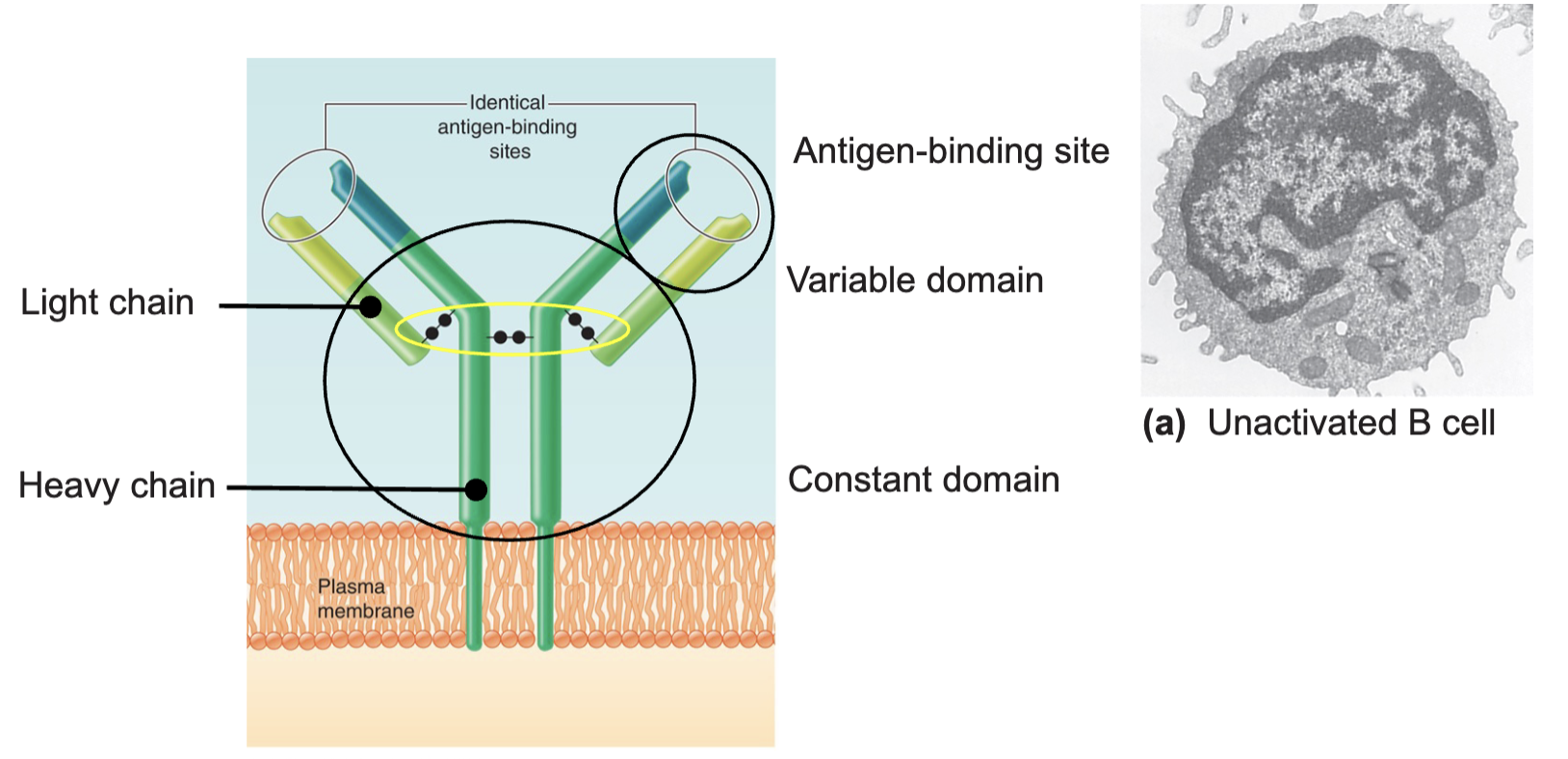
Antibodies
Each B cell makes only one unique antibody
Each antibody is highly specific for one particular antigen
Usually part of a protein, but it can be anything
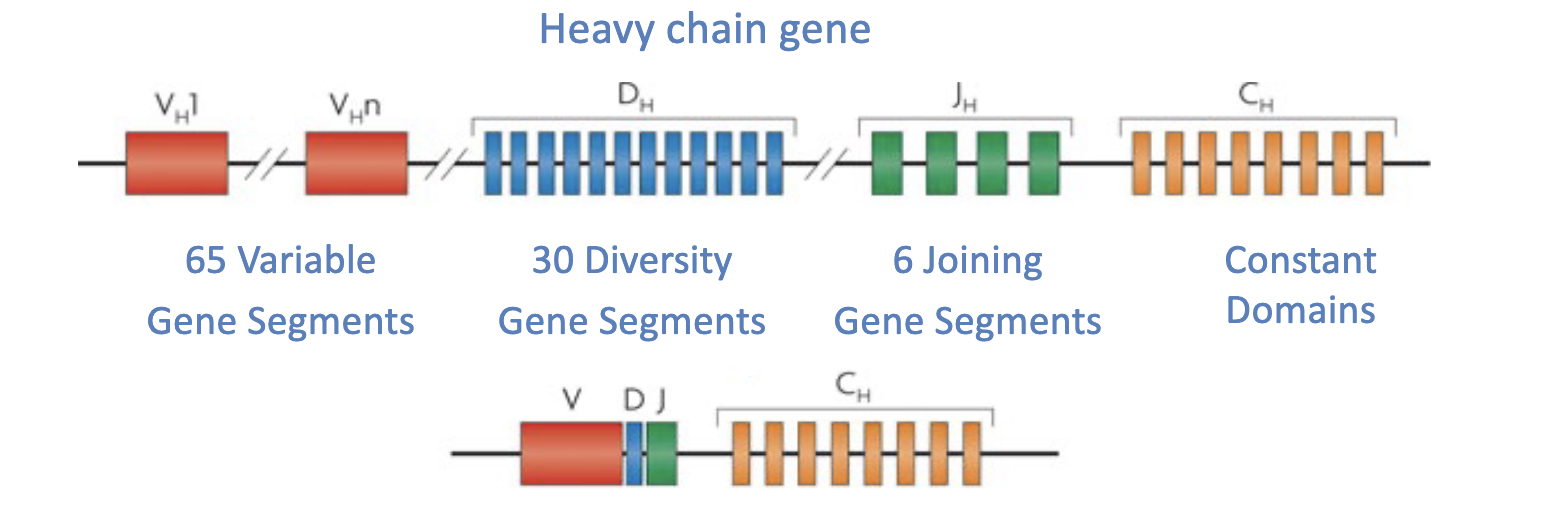
How are antibodies generated?
A random combination of V, D, and J segments (genes) provides 65×30×86~ 12,000 possible unique combinations for just the heavy chain (light chain generated in a similar process)
Over 100 million possible antibodies
What happens when B cells make antibodies that recognize our own proteins?
They are killed off in the bone marrow via negative selection
How do B cells make a difference against a pathogen?
Bacterium (pathogen) binds to matching antigen binding site on B cell
Binding of the antigen and interaction with a helper T cell stimulates the matching B cell to divide and expand the clone of selected cells
Most new B cell clones differentiate into plasma cells, few differentiate into memory B cells
Plasma B Cells
Secrete antibodies (proteins from the ER)
Memory B Cells
Respond to a later encounter with the same antigen
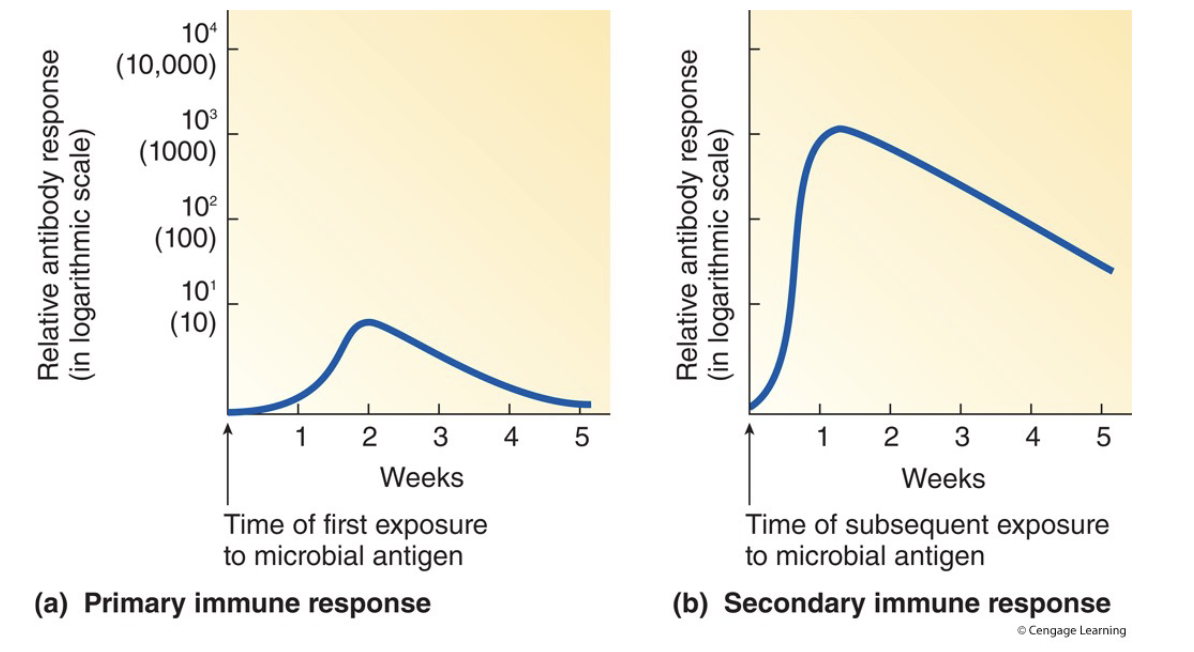
Immunological Memory
Primary Antibody Response
In response to first antigen exposure
Takes a few weeks
Moderate concentration of low-medium strength antibodies
Secondary Antibody Response
In response to subsequent antigen exposure
Takes a few days
High concentration of high-strength antibodies
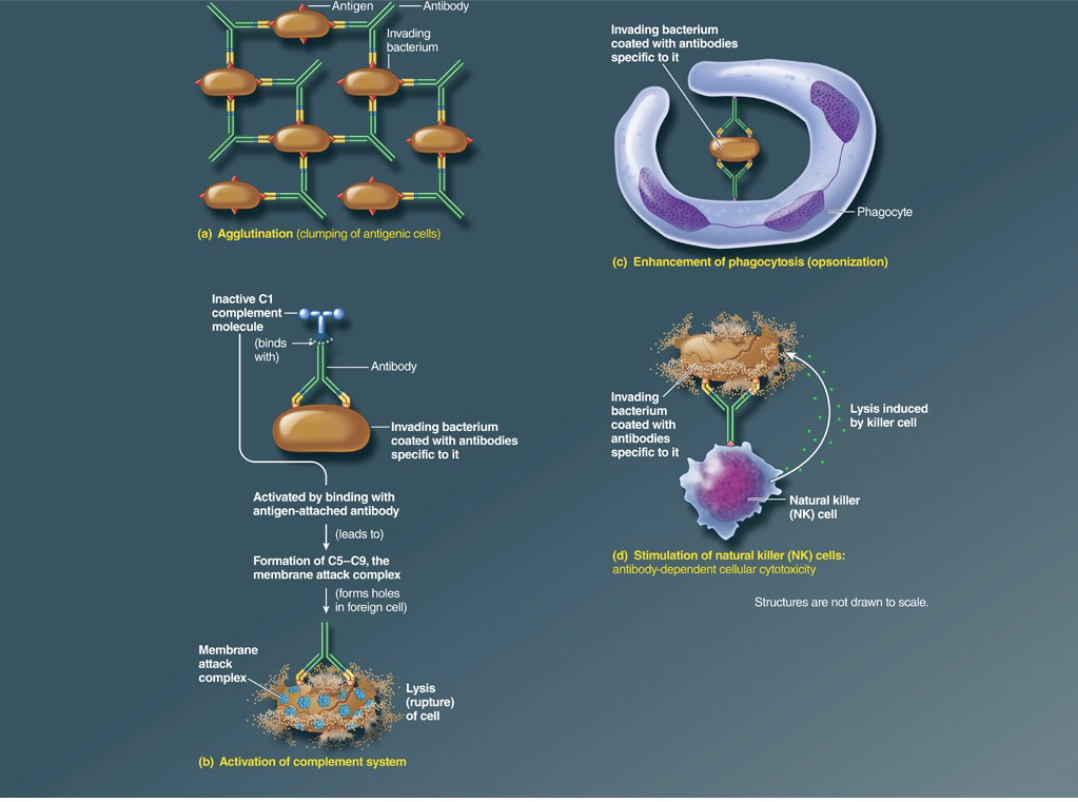
How do antibodies help fight pathogens?
Agglutination- causes antigenic cells to clump together
Activation of the complement pathway- a cascade of biochemical responses that ends with the formation of the Membrane Attack Complex, which kills pathogens
Opsonization- coating the surface of pathogens with antibodies, initiating phagocytosis
Leads to activation of natural killer cells
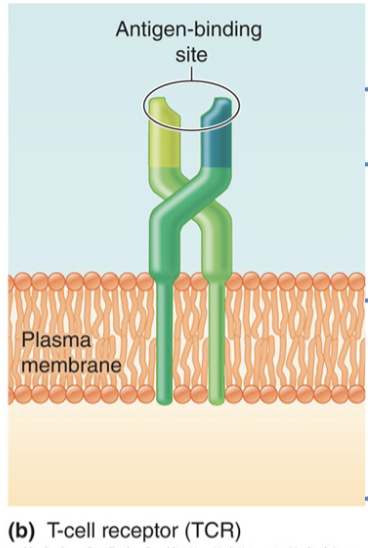
Anatomy of T Cells
Dimer of 2 T cell receptor chains
Tip o the variable domain provides the antigen binding site
Each T cell has a unique TCR, a large T cell repertoire is generated similar to B Cells
Two major types
Helper
Cytotoxic
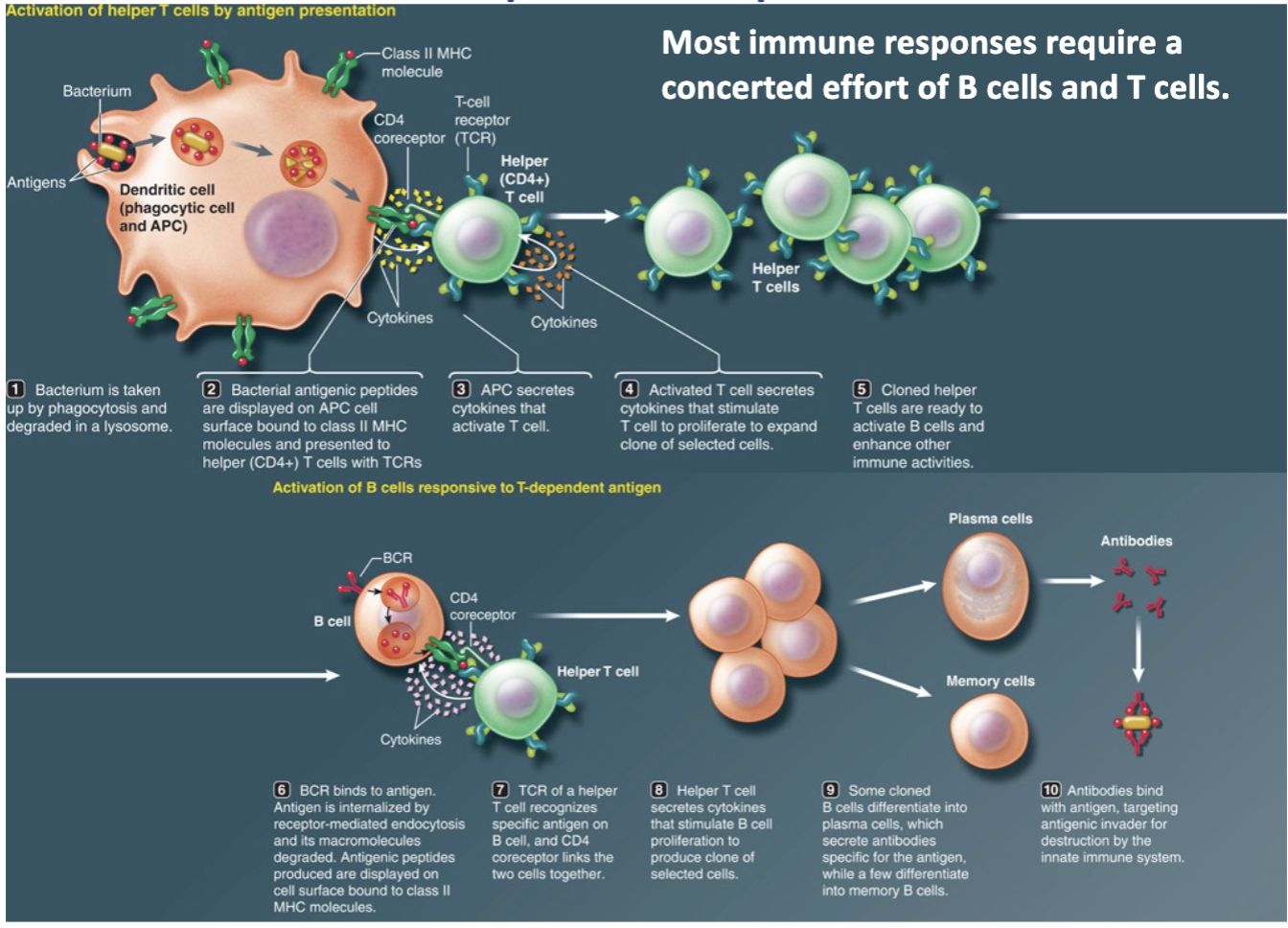
Helper T Cells
Provide essential ‘help’ to B Cells in mounting a humoral immune response
Without, most antibody-mediated (humoral responses) cant take place
Cytotoxic T Cells
Can kill cells via cell-cell contact
Important in the defense against virus infected cells and cancer
T Cells Recognize ‘Non-Self’ in the Context of ‘Self’
Dendritic cell engulfs bacterium
Large molecules of engulfed bacterium are broken down by lysosomes to produce antigenic peptides
New Major HistoCompatibility (MHC) molecule has been synthesized by ER-Golgi Complex
Antigenic peptides bind to newly formed MHC molecules
Antigen is displayed on cell surface bound to MHC molecule
The cell is now an antigen presenting cell (APC)
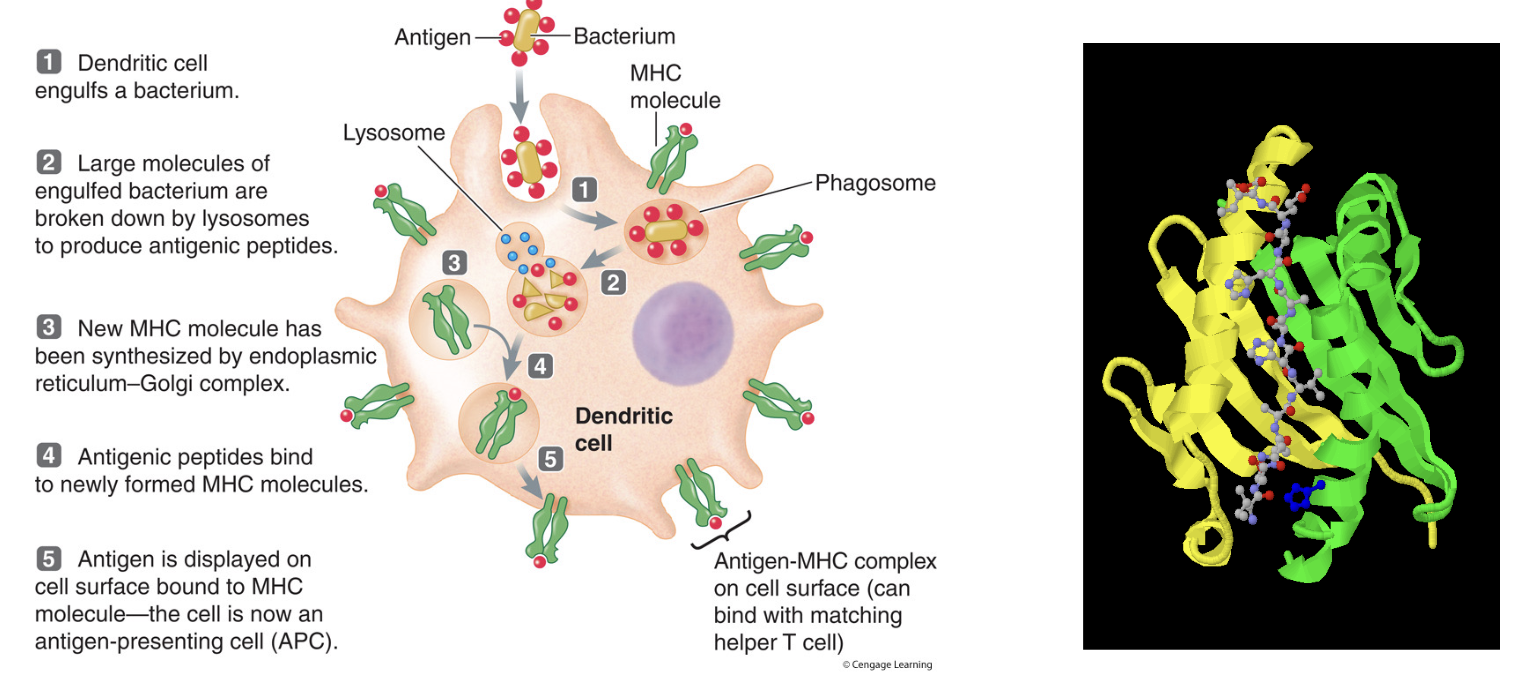
Non-Self
Fragment of a pathogen after degradation in the lysosome
Self
MHC genes, which encode a protein dimer on the cell surface to ‘present’ this small fragment
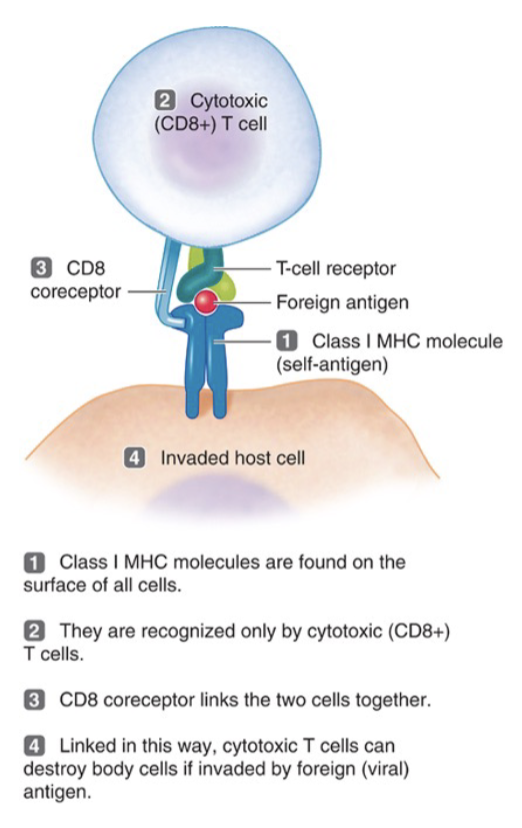
Cytotoxic T Cells
All cells express MHC class 1
MHC-1+peptide is recognized by TCRs on cytotoxic T cells, along with a CD8 co-receptor
If the peptide is ‘self’ nothing happens
If the peptide is ‘non-self’ and is presented in the context of ‘self,’ cytotoxic T cells with the right TCR to recognize the peptide will kill the infected cell
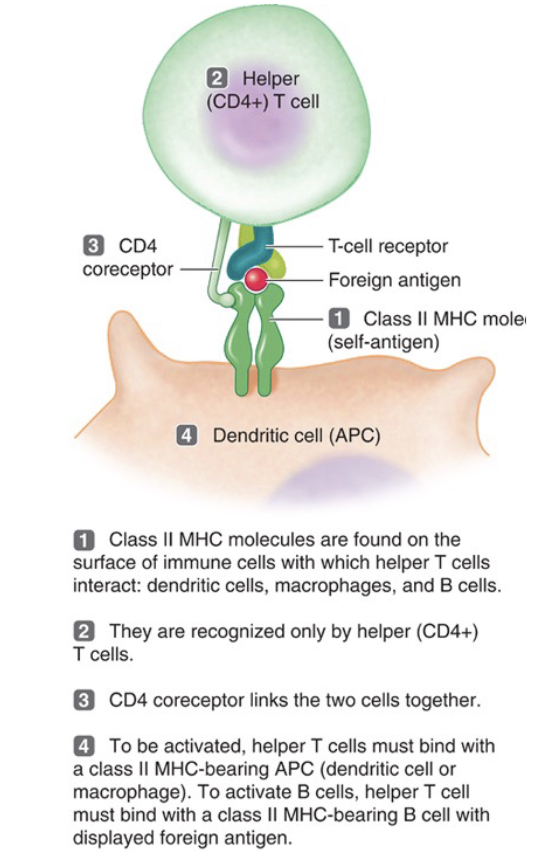
Helper T Cells
Specific antigen presenting cells express MHC class 2
MHC2+peptide is recognized by TCRs on helper T Cells, along with a CD4 co-receptor
If the peptide is ‘non-self’ presented in the context of ‘self’ by an APC, this activates helper T cells
Activation of helper T cells can then provide help to B cells that present ‘non-self’ antigen
Help is provided int he form of cytokines which are soluble signaling molecules released by helper T cells to promote proliferation (cell division) of those B cells that are activated
How to Helper T Cells help B Cells
Role of Innate Immunity
Innate immune cells are really efficient APC
Without antigen presentation, there will be no acquired immune response
Innate immune cells are also very capable of scavenging out bodies for anything damaging (self or nonself) and clean up
Innate immunity provides a much faster, local response (inflammation) to a threat (damage or pathogen)
This usually takes care of the threat and promotes tissue repair
How does innate immunity know to respond?
Innate immune cells recognize pathogen-associated molecular patterns (PAMP)
PAMPs broadly flag to the innate immune system that something is amiss and requires immune response
What are examples of pathogen-associated molecular patterns (PAMP)?
Lipopolysaccharide (gram negative bacteria)
Un-methylated DNA (virus)
Heat shock proteins (self)
Doesn’t occur outside of the cell, is a sign of unusual damage and death
Disorders of the Innate Immune System
Genetic mutations in the signaling pathways of the PAMPs lead to defects of the innate immune system
Increased susceptibility to severe and reoccurring infections
Over-active innate immune responses lead to auto-inflammatory diseases, usually related to the excess strength of signals that promote inflammation
Disorder of the Acquired Immune System
Rare mutations affect the ability to carry out VDJ recombination, no BCR or TCR can be made, causing absence of acquired immune system
Severe combined immuno deficiency, hereditary, X-chromosome linked
Acquired Immune Deficiency Syndrome (AIDS)
Human immunodeficiency virus (HIV) infects and kills CD4 and helper T cells, resulting in a lacker of B and cytotoxic T cell activation