TCAR module 7- head injuries fully solved questions with 100% accurate solutions(Latest Update)
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
in senior trauma patients, which set of vital signs is most alarming
BP 137/82 HR 123
BP 158/91 HR 86
BP 107/79 HR 112
BP 104/60 HR 74
BP 107/79 HR 112
in senior trauma patients, a HR > 90 and a SBP <110 are red flags for deterioration
when an older adult dies as a result of a fall, the most common cause of death is....
brain injury
of all trauma patients with a brain injury, only 7% of them are considered severe
GCS and brain injury severity
3-8 severe
9-12 moderate
13-15 mild
a primary brain injury is any damage that directly results from the initial application of force to brain tissue. such injuries include concussions, lacerations, hematomas, DAIs, and skull fractures. a secondary brain injury is any damage that occurs due to the brains response to the primary injury. common secondary injuries include edema, vascular changes, increased ICP, and numerous inflammatory and biochemical reactions
diffuse injuries directly affect consciousness, focal injuries indirectly affect consciousness
physiologically there only two ways to lose consciousness
shut down the RAS in the brainstem, disrupting the flow of impulses to the rest of the brain (concussion, DAIs, a brainstem legion)
impair both of the cerebral hemispheres (Edema, hypoxia, brain shift, hypoglycemia, seizures, etc)
each of these loss of consciousness etiologies occurs in trauma patients. understanding the distinction helps identify whats happening in an altered patient's brain
the brain can accommodate around slow-growing masses such as tumors and AV malformations. however, the brain poorly tolerates the acute changes associated with traumatic injury (edema or hematomas). instead, patients quickly decompensate
limitations of a CT scan
cant find concussion
only indicated for moderate-severe injuries in children, much more utilized in older adults
post concussion syndrome
lingering symptoms from a concussion
HA, dizziness, poor concentration, and impaired memory
Diffuse axonal injury / shearing jury
axons being torn apart
result from sudden changes in head velocity associated with high energy mechanisms. most common MVC. can also result from direct blow to head, blast pressurization wave, referred energy from blow to other part of body
the axons are disrupted as a direct result to injury, or as subsequent neuronal degeneration. The axons simply "fall apart" in the hours after injury
stunned, stretched, edematous axons may recover- as edema resolves, myelon sheaths are repaired and new dendronic connections are formed
but if the axon is torn, there is no regeneration. there is no putting the axons back together again.
because the brain has limited regenerative and restorative abilities, recovery from a severe DAI is very slow, and usually minimal
in children, commonly associated with child abuse.
a restrained driver involved in a high-speed rollover arrives at this hospital with a GCS of 5. Her brain CT is negative. She survives but never regains consciousness. What is her most likely injury?
- second impact syndrome
- SAH
- frontal contusion
- Diffuse axonal injury
DAI
CT vs MRI
CT- perofmred faster, less expensive, best visualzied bony fractures and other focal lesions
MRI- often requires sedation, takes longer
doesn't involve radiation exposure
DAI wont be present for many hours post injury
so MRIs are never done emergently
second impact syndrome
rare, but often fatal diffuse brain injury
when a patient receives head trauma resulting in concussion, then patient sustains second impact before the brain has completely healed. within minutes of the second blow, the patient collapses due to massive cerebral edema that progresses to herniation
CTE chronic traumatic encephalopathy
a diffuse, progressive, degenerative brain disease with repetitive trauma
symptomatic concussions, or asymptomatic sub-concussive blows.
symptoms don't usually manifest until the fourth decade of life
(football, other contact sports)
initial CT scan of patient with a DAI
usually will not show DAI. 50-80% of DAI patients will have no early CT findings, although some will exhibit the multiple punctate hemorrhages characteristic of this injury
DAI treatment primarily consists of supportive care. damage can range from mild to severe, but patients with a brainstem injury have a high mortality rate
90% of those with a severe injury will die within 6 months. patients with brainstem trauma have the highest mortality rate because vital cardiac and respiratory centers are located in this region
conditions that can produce a brain injury without a direct or indirect force to the head
airway obstruction
blunt carotid vertebral injury
profound hypovolemia
strangulation
cardiac arrest
drowning
drugs and alcohol
not all brain injuries in our trauma patients are the result of a head injury. hypoperfusion, anoxia, and toxins also cause brain damage. major trauma patients are at risk for each of these conditions. dont forget to look beyond head trauma to explain an altered mental status
in adults, which facial bone is most frequently fractures?
-mandible
-maxilla
-nasal bones
-zygomas
the nasal bones
they are the weakest bones in the face
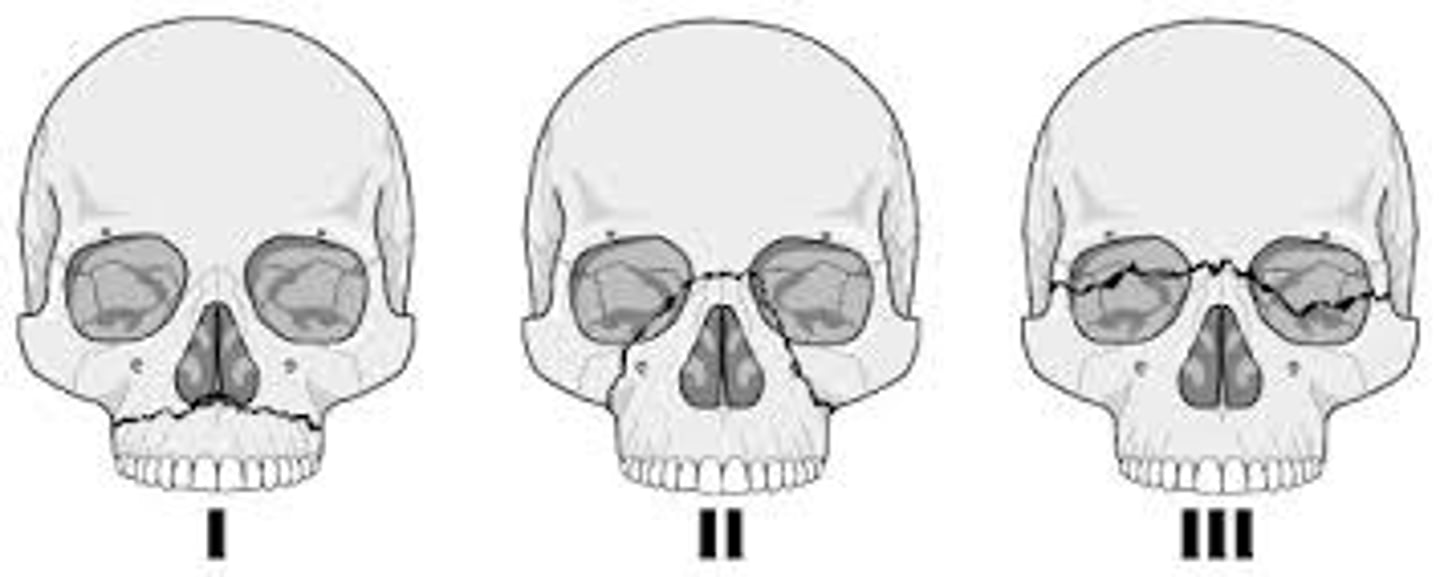
le fort I fx
le fort II fx
le fort III fx- also known as cranio facial dislocation. the entire face is no longer attached to the skull. separtes the facial bones from the cranium
in patients with severe facial injuries, early trach is commonly performed (think Billy) for airway and secretion management
cribriform plate (part of the ethmoid bone)
commonly clinical finding?
CSF leaking out the nose
potential for intracranial infection
if CSF is leaking out, all of the microbes in the nose can infect the brain
the thin ethnoid bone if the only thing separating the nose from the sterile brain
be careful when placing NG tubes in patients with facial fractures! can wind up in brain
nothing should be inserted in the nose with patient with midface trauma
in adults, most skull fractures are...
linear and non displaced
but can also be depressed and displaced
when the mandible breaks, fractures usually occur bilaterally, at the mandibular body or angle
le fort I is a horizontal fracture through the body of the maxilla. pulling the upper teeth moves the hard palate
le fort II also known as pyramidal fractures, involve the central maxilla, nasal, and ethmoid bones. tugging the upper teeth will wiggle the nose
le fort III usually start at the nasal bridge, extend posteriorly through the ethmoid bone, and then laterally through the orbits and zygomas. also known as a craniofacial disjunction
the skull base
which delayed clinical finding is characteristic of an anterior fossa (part of the base of the skull) fracture?
raccoon eyes, periorbital ecchymosis
what delayed clinical finding is a characteristic of a middle fossa fracture?
battles sign
can also have CSF otorrhea
if a patient has this, what other injury must be present? tympanic membrane rupture! how else would the CSF leak out?

what clinical finding is characteristic of a poserior fossa fracture?
uncommon
raccoon eyes, battle signs, and herniation and death
a head CT shows a left, middle fossa, basilar skull fracture. which of the following is an expected clinical finding?
intermittent blood-tinged drainage from the ipsilateral ear canal
even small amounts of blood in the posterior fossa can cause....
herniation and death
the brain can not accutely accomodate extra volume in the posterior fossa. bleeding into this region puts pressure on the cerebellum and brainstem, interfering with essential brain functions (breathing, HR, BP) causing herniation and potentially death.
dura mater
thick, outermost layer of the meninges surrounding and protecting the brain and spinal cord
comparable to periosteum that lines the bone
there is no natural epidural space!
the space only exists when dura is forcefully peeled away from the skull
epidural hematoma
occurs between bone and dural layer

epidural hematoma
whats the most common site? at the temporal bone at the site of the middle meningeal artery
perfect storm- relatively thin bone, vulnerable location, and a major artery is present
classic presentation: immediately unconscious,
lucid interval,
progressive decline in LOC
what are the only two ways to loose consciousness?
shut down the RAS in the brainstem
knockout both cerebral hemispheres
when ICP is elevated, which gets displaced first?
brain
blood
CSF
CSF first
then blood
then the brain will herniate
a midline shift can also be referred to as...
subfalcine hernation
its when the brain shifts across the midline
pupil monitoring when a patient is at risk for herniation
pupillometer can reliably identify and quantify even small changes in the pupil size and reactivity, something the human eye would be unable to do
cranial nerves are peripheral, they dont cross. so pupil changes will be ipsilateral (same side) as the injury
will the patient have left sided or right sided weakness?
weakness will be on the opposite side of the injury
motor signs are contralateral
layers of bone / brain mater from external to internal
skull bone
dura mater
arachnoid mater
pia mater
brain tissue
the falx cerebri and terntorium are folds of dura mater that separate the right cerebral hemisphere from the left, and the upper brain from the lower brain
the source of most EDH is...
arterial bleeding
as pressure in the cranial vault increases, the brain moves downward causing pupillary dilation by compressing cranial nerve ____
II - optic
III- oculomotor
IV- trochlear
VI- abducens
III - oculomotor
the patient with a right epidural hematoma will have....
right pupil dilation and left sided weakness
bedside interventions for the patient with a large, expanding epidural hematoma include....
urgently notifying medical team
preparing patient for emergent surgery
protecting the patients airway
elevate HOB to 30-45 degrees to reduce intracranial pressure
subdural hematomas
unlike an epidural hematoma, there is a subdural space that can semi accommodate for bleeding
usually from a venous bleed
blood accumulates under the dural layer- most commonly caused by tearing of the bridging veins that connect the brain to the dural sinuses
can be acute, subacute, or chronic
what stops subdural blood from migrating to the other side?
the falx cerebri
whats the intervention for a large, expanding SDH?
emergent craniotomy!
epidural vs subdural hematoma- which is a associated with a better longterm outcome?
epidural hematomas
if they are evacuated promptly?
why? epidural bleeds never touches brain tissue. the survival rate is high and patients can have a complete recovery if the clot is quickly removed and bleeding is controlled
in a patient with a SDH, blood is in direct contact with brain tissue. remember, blood outside of circulation is very irritating to surrounding tissues
SDH cause both mechanical pressure, and chemical damage. the blood to brain contact destroys brain tissue
populations at risk for SDH
alcoholics
elderly
babies
are subdurals and epidurals superficial or deep?
they are both superficial
what is the concern with an IPH?
they can occur deep within a vital area of the brain
how would a neurosurgeon evacuate it without disturbing healthy brain tissue?
management is usually supportive, prognosis is usually poor
subarachnoid hematoma
usually the result of small venous tears
bleed within the subarachnoid space- this space is usually filled with CSF
treatment is usually supportive and symptomatic
most major SAH are usually caused by spontaneous arterial bleeding from a ruptured aneurysm or AVM rupture
in a patient with a subdural hematoma blood accumulation always...
occurs on the brain's surface
by definition, a subdural hematoma occurs under the dural layer, on the surface of the brain
the most common source of subdural blood is bleeding from..
the brain-to-dura bridging veins
brain contusions can occur in gray or white matter anywhere in the brain, including the brainstem. During the post-resuscitation period, anticipate a brain-contused patient will have slow, progressive, neurological deterioration as the lesions evolve. bruises are not necessarily minor injuries. about 20% of cerebral contusions severe enough to be noted on an initial CT scan will require surgical evacuation in the hours or days after trauma due to hemorrhagic conversion or tissue necrosis
a traumatic IPH involves an area of bleeding within the brain parenchymal or in the ventricles. these injuries can occur anywhere in the brain but are frequently located deep within vital regions, making sx intervention challenging and risky. thus, supportive care is often the mainstay of management
what changes first, LOC or pupils?
LOC!
you have an alert and oriented patient, then you check his pupils?
does this make sense?
what size shift usually requires sx intervention?
5mm or greater
what is the warfarin reversal agent?
4 factor prothombin complex/ K centra
or
vitamin K and FFP
k centra is usually preferred, patients require multiple units of FFP. can our elderly patients accomodate for almost an additional L in the circulatory system? no
early signs of neurological deterioration
confusion
nausea
agitation
drowsiness
impaired balance
when LOC decreases rapidly, which metabolic disturbance is the most likely cause
hypoglycemia
how do you calculate cerebral perfusion pressure (cpp)?
MAP - ICP
a single episode of hypotension and the TBI patient is twice as likely to die
a combination of hypotension and hypoxia, is associated with up to 75% mortality in TBI patients
TBI interventions
analgesics
sedatives
antipyretics
stool softeners
anticonvulsants
high dose barbiturates
neuromuscular blockate
TBI interventions- temperature specific
no real evidence suggests that hypothermia is beneficial
however, hyperthermia is clearly detrimental to the injured brain and should be aggressively avoided
nursing internvention for a patient that has had a craniectomy
protect the fontanelle!
in the absense of ICP monitoring, the brain injury guidelines recommend keeping SBP > 110 for most adults, but only ?100 for....
50-69 year olds
nose and navel alignment promotes venous drainage (it straightens the jugular veins) as does positioning patients with HOB up 30-45 degrees.
goal of care for the patient with a moderate or severe TBI include keeping pco2 between 35-40 and SPO2 above 90%
longterm outlook ( 5 years) for a patient with moderate -severe TBI
22% died
30% alive, but in worse condition
22 % unchanged
26 % improved
80% of elderly patients with a severe TBI will die in the hospital or require long term care
which of the following is a legally binding document concerning end-of-life preferences?
a. a signed organ donor card
b. wishes expressed to family members
c. an advance directive
d. a power of attorney form
an advanced directive
a cushing ulcer is a for of gastritis that occurs in patients with increased intracranial pressure and requires appropriate prohylaxis to prevent serious GI bleeding
Nurses are the most consistent and present healthcare professionals at most patient's bedside. Trauma nurses are available 24/7 to assess patients, interpret data, manage and troubleshoot equipment, give medications, perform nursing interventions, mobilize necessary resources, and support the patient and family. Nothing can substitute for the knowledge, vigilence, and expertise of a highly-skilled nurse at an injured patient's side.