Gas Transport in Blood
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
Is O2 & CO2 soluble in blood?
O2 is not soluble at all
CO2 is somewhat soluble, still mostly insoluble
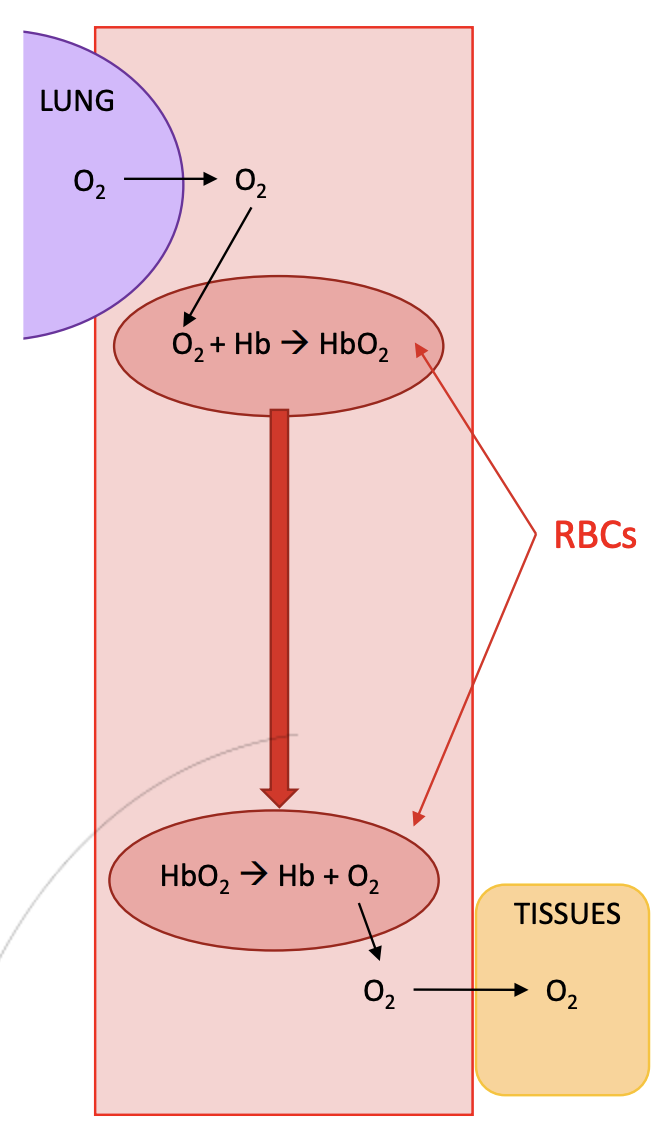
O2 transport
1.5-2% is carried within blood plasma
98% is carried within red blood cells, binding to the carrier molecule haemoglobin.
Equation: Hb + O2 ↔ HbO2
Travels down the pressure gradient, from alveolus to capillaries
Dissolves in plasma
Diffuses into red blood cell (RBC)
Reversibly binds Hb
Moves through blood as HbO2
Once at tissues, dissociates from Hb
Diffuses out of RBC and into tissues
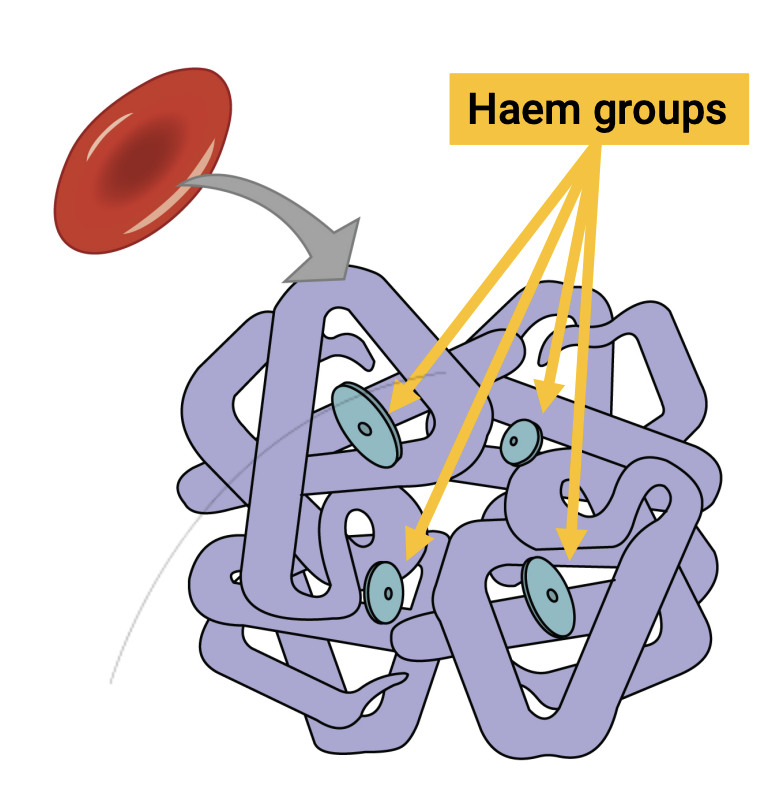
Haemoglobin
Made up of 4 subunits
Each subunit contains a group of Iron (Haem group)
O2 binds to the iron within the Haem group
give blood its red colour (like how rust is red)
Each red blood cell can carry up to 4 O2 molecules
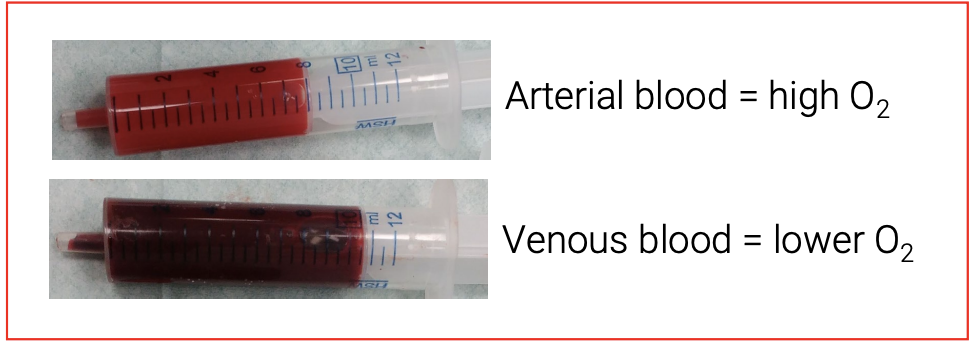
Is arterial and venous blood red and blue respectively?
No dummy
Is the Hb and O2 relationship directly propoertional?
No, as when one O2 molecule binds to Hb, it increases the affinity of other O2 molecules binding to the remaining Haem groups.
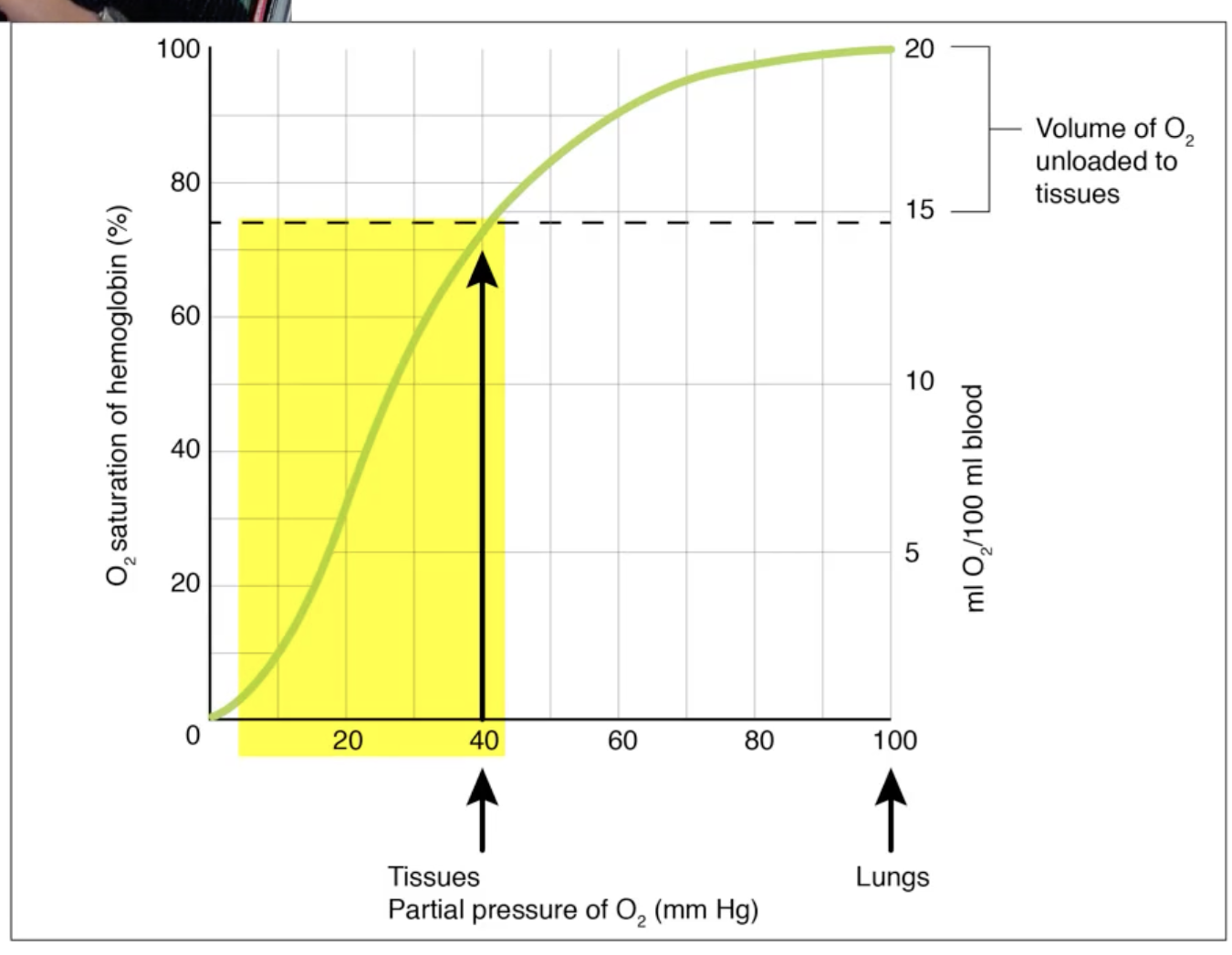
O2/Hb dissociation curve
Curving Plateauing end
For oxygen absorbtion in lungs
Curve plateauing up top: pO2 (partial O2 pressure) present in lungs. essentially 100% saturation of haemoglobin.
But 40 pO2 in tissues.
Despite the partial pressure decreasing from 100 to 40, Hb saturation still remains high (from 100% to ~75%).
This is to ensure the red blood cells retain O2 even as the partial pressure drops from the lungs to around the body.
Lots of redundancy
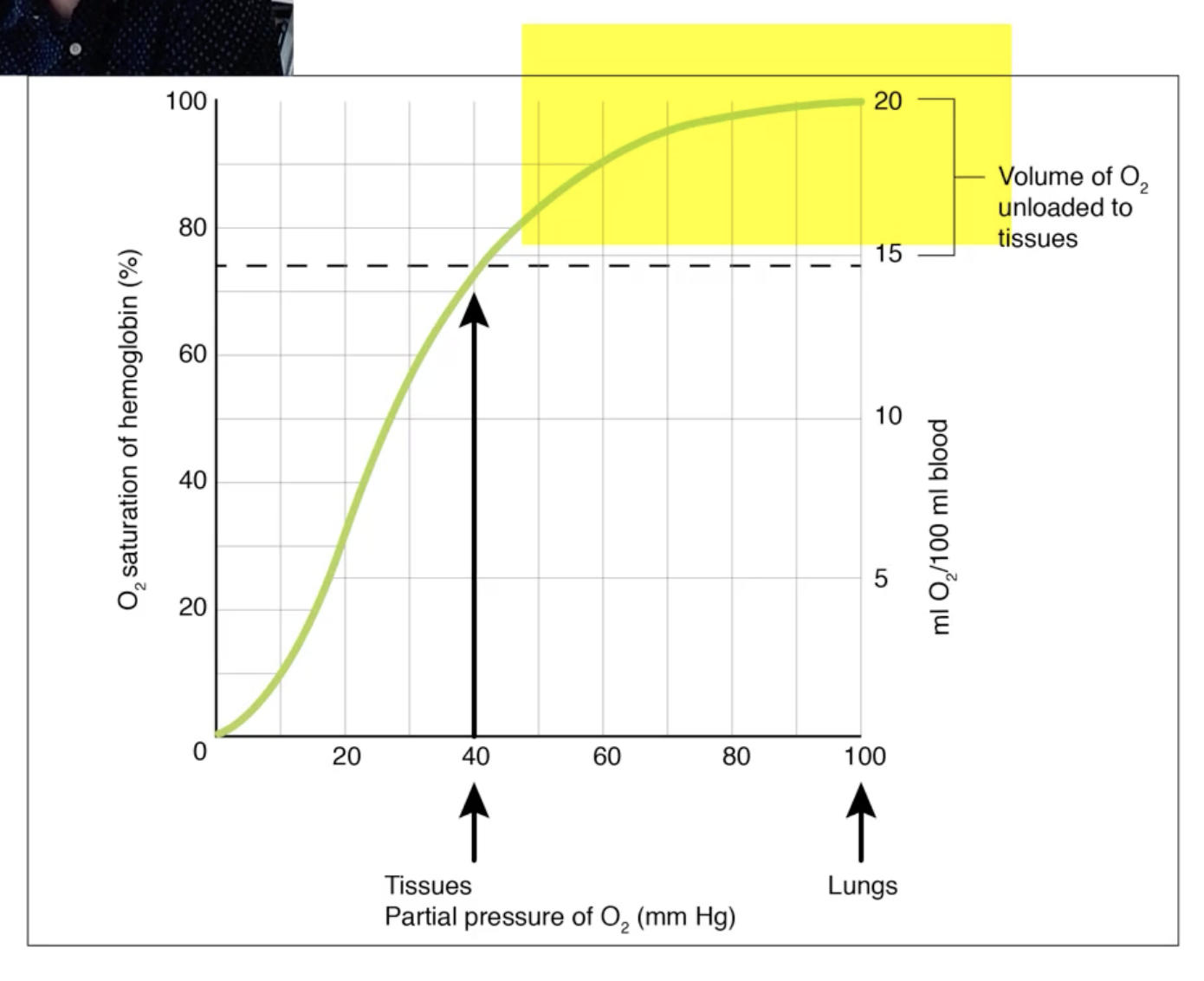
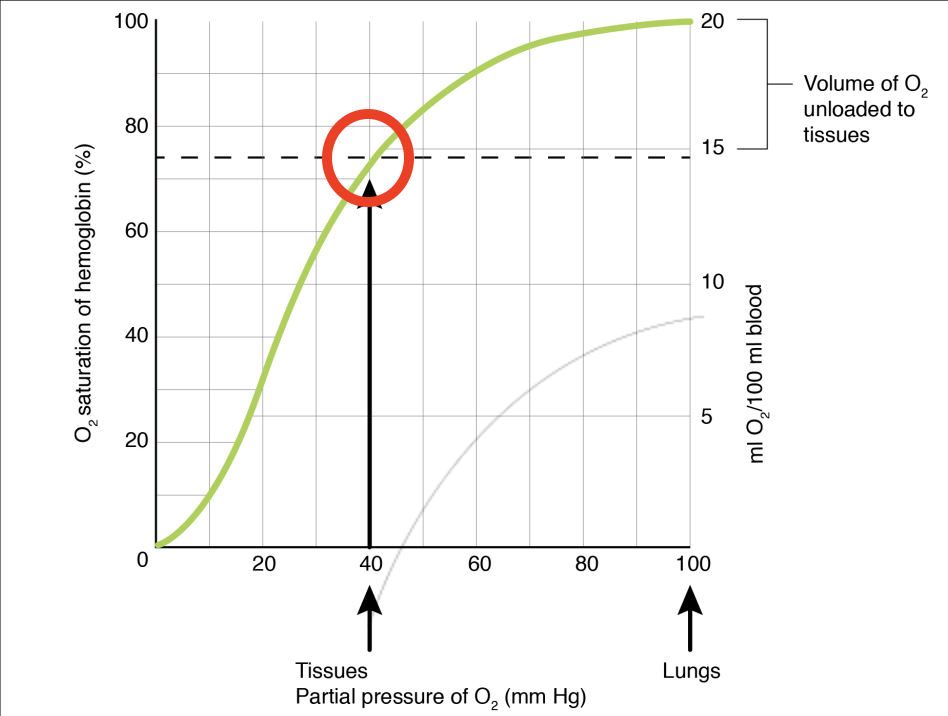
O2/Hb dissociation curve:
Curving Plateau Steep start
For Oxygen delivery to tissues
Even small drops in pO2 (e.g. if a tissue is a bit more metabolically active) mean more much O2 will be released by Hb
Good for delivering O2 to tissues as needed
O2/Hb dissociation curve:
Key point
Usually only deliver ~25% of the O2 carried by red blood cells (RBCs) to the tissues – lots of spare capacity if needed
‘Deoxygenated’ blood in veins still has a lot of O2 in it!
Factors that:
Decrease Haemoglobin/O2 affinity
Increase in temperature
increase in pCO2
decrease in pH (more acidic environment)
Haemoglobin is more likely to deliver O2 to a metabolically active tissue
Factors that:
Increase Haemoglobin/O2 affinity
Decrease in temperature
Decrease in pCO2
Increase in pH (more basic environment)
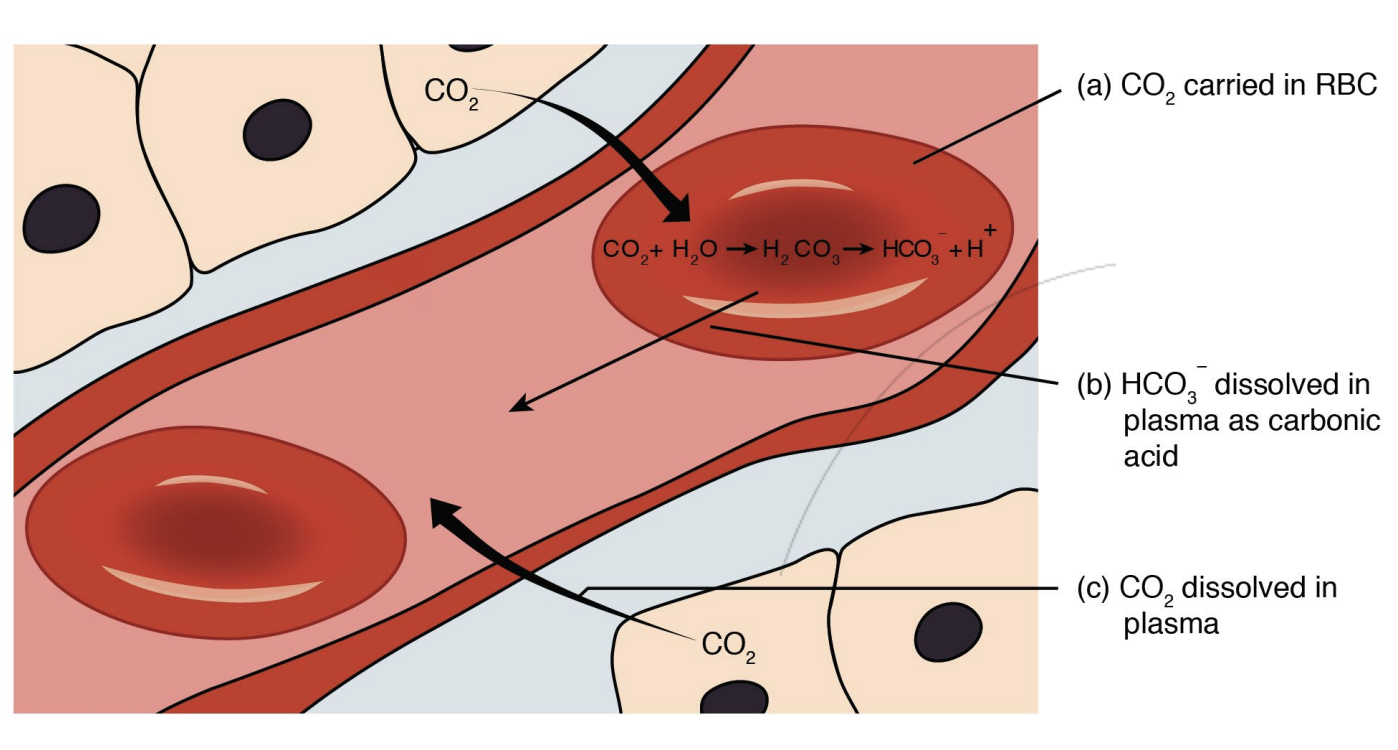
3 Ways of CO2 transport
Bound to Hb (~20%)
In the form of bicarbonate ions (~70%)
Dissolved in plasma (~10%) as CO2 is more soluble than O2
CO2 binding to Haemoglobin
CO2 binds to a different part of Hb (i.e. the amino acid portion rather than the haem) but otherwise the same as O2/Hb transport
No competitive binding
CO2 transported as Bicarbonate ions:
Carbonic anhydrase reaction
Red blood cells secrete an enzyme (carbonic anhydrase). This enzyme facilitates the reaction.
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
(reaction occurs within the red blood cell)
Carbonate ion is able to travel within the plasma
Process is reversed when CO2 is entering the lungs