Hematology 1
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Lab Results + Physical Exam+ Patient History
what are the three hematologic diagnostics?
Hematology – science of blood and the blood forming tissues
● Anemia – condition with diminished oxygen carrying capacity of the
blood (destruction/loss/diminished production)
● Ineffective Hematopoiesis – failure to produce or release mature
forms of cells into the peripheral blood or cells destroyed in marrow
● Extramedullary Hematopoiesis – formation of blood cells in sites
other than bone marrow; primarily liver and spleen
● Hemolysis – destruction of red blood cells
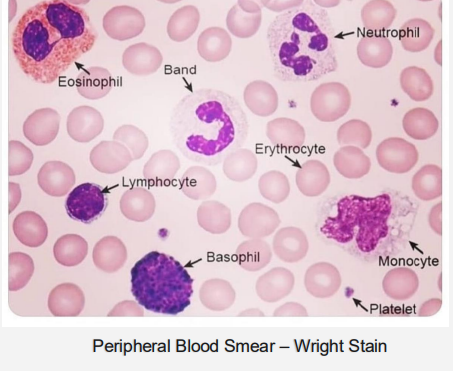
● Peripheral Blood Smear – thin film of EDTA anticoagulated blood on a glass slide; stained and examined microscopically
● “Shift to the Left” – an increase in the immature forms of cells in the
peripheral blood
________ – science of blood and the blood forming tissues
_________ – condition with diminished oxygen carrying capacity of the
blood (destruction/loss/diminished production)
__________– failure to produce or release mature
forms of cells into the peripheral blood or cells destroyed in marrow
__________– formation of blood cells in sites
other than bone marrow; primarily liver and spleen
__________ – destruction of red blood cells
___________– thin film of EDTA anticoagulated blood on a glass slide; stained and examined microscopically
____________ – an increase in the immature forms of cells in the peripheral blood
Whole Blood has :
Platelets, RBC, WBCs, Lymphocytes, Monocytes, Eosinophils , Basophils, Neutrophils
Dont blem it on me
what is 7 things is blood composed of?
Blood cell production; starts before
birth and continues throughout life:
➢ Embryo: Yolk sac
➢ Fetus: Liver, Thymus, Spleen, and
Marrow of all bones
➢ Birth: Bone Marrow (primarily)
❑ Flat bones (sternum, ribs, skull,
vertebrae, pelvis) and Long
bones (femur, humerus)
❑ Extramedullary: Spleen and
Liver
When & Where does blood Cell production (heamtopoiesis) begin?
Specifically in the:
Embryo
Fetus
Birth:
:
Extramedullary:
Platelets
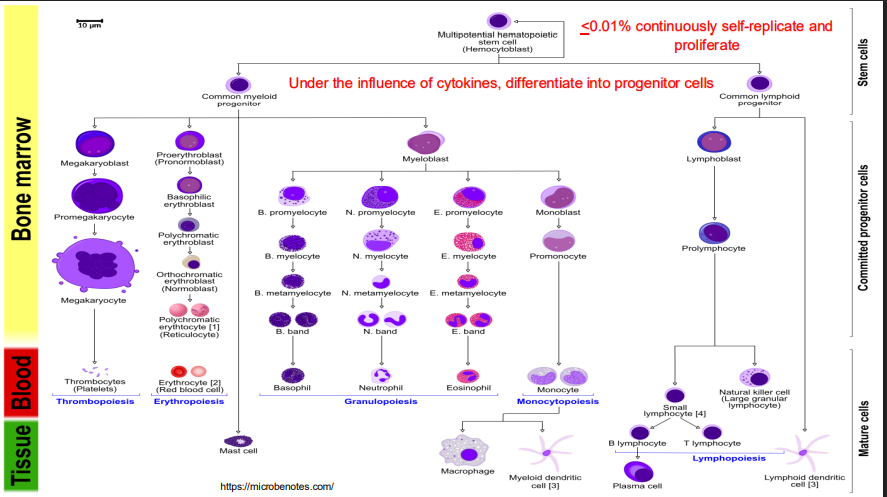
Stem cell → common myeloid → megakaryoblast → Promegakaryocyte → megakarycyte → Thrombocyte
RBC
Stem cell → common myeloid → Proerythoblast (pronormoblast) → Basophilic erythroblast → polychromatic erythoblast → orthochromatic erythroblast→ polychromatic erythrocyte (reticulocyte) → Erythrocyte
Granulocytes
Stem cell → common myeloid → myeloblast → Promyelocyte → Myelocyte → metamyeloctye → Band → Granulocyte
Monocytes
Stem cell → common myeloid → myeloblast → monoblast → promonocyte → monocyte
B&T
Stem cell → common lymphoid progenitor → Prolymphocyte (NK cells come from here) → Small lymphotcyte → B (futher differentiate into plasma) or T
Where are platelets formed from?
Where are RBCs formed from?
Where are Granulocytes formed from?
Where are the Monocytes formed from?
Where are B & T blood lines
➢ Red Blood Cells (RBCs) – Erythrocytes
➢ White Blood Cells (WBCs)
➢ Granulocytes ❑ Neutrophils ❑ Eosinophils ❑ Basophils
➢ Monocytes
➢ Lymphocytes
➢ Thrombocytes - Platelets (PLTs)
What are the types of mature blood cells?
What do they all look like?
➢ Red Blood Cells (RBCs) –
➢ White Blood Cells (WBCs)
➢ Monocytes
➢ Lymphocytes
➢ Thrombocytes -
Protein stimulators: ETI erythropoietin, thrombopoietin, interleukin
protein inhibitors: interferons, lymphotoxis
Name the 3 protein stimulators
Name the 2 protein inhibitors
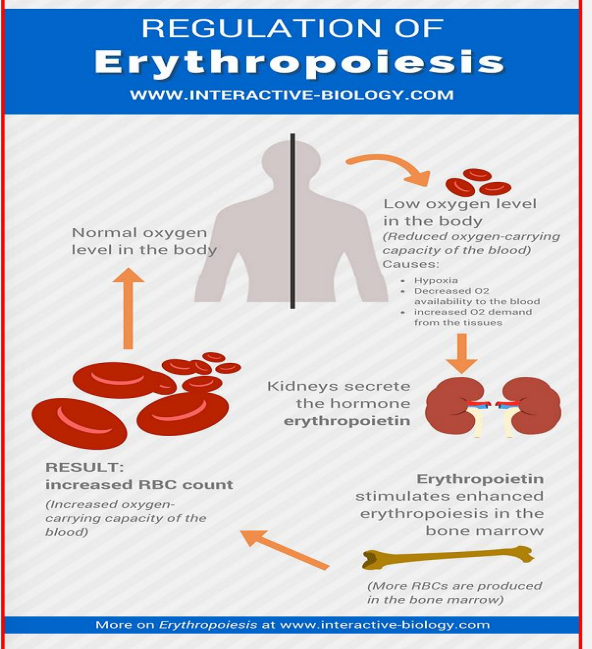
Low Oxygen is Felt
Kidney Secrete Erythropoietin Hormone
Erythropoietin stimulates enhanced erythropoiesis in bone marrow
Bone Marrow Erythropoiesis results in increased rbc count
Oxygen Level returns to normal in the body
Days 1-5:
CMP → Proerythroblast → Erythroblast → Reticulocyte → Erythrocyte
How is RBC production regulated?
how do RBCs form?
Orthochromic
Streaks of RNA/DNA, stain grey/blue
What stage of RBC creation do we lose the nucleus to make room for the Heme group
What are the differences between reticulocytes and mature RBCs
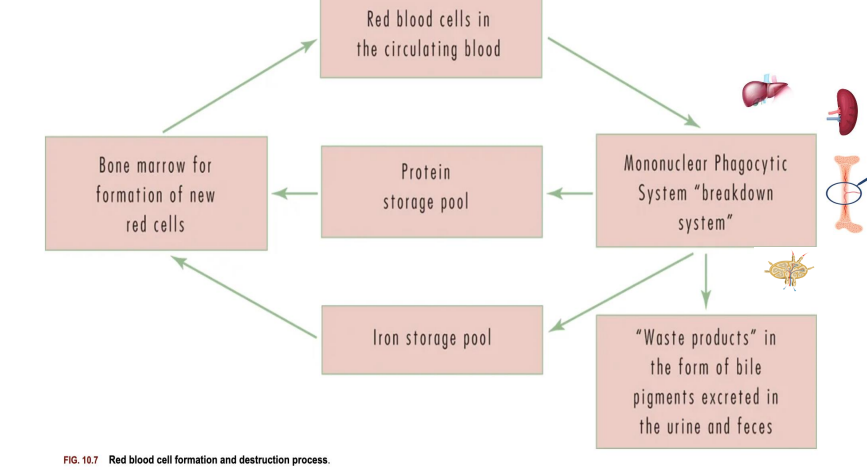
Lose pliability → cleared by phagocytes in spleen, liver, bone marrow, lymph → iron, proteins, etc are reused → waste products (bile pigments) are excreted
Describe the destruction and recycling process of RBCs
Purple top less than 24 hrs old (mix gently), bone marrow sample (slides must be made A$AP), Green top, light blue top
What specimens can be used for CBCs?
hemocytometer: (manual - green for WBCs, Red for everything else)
How can you run a hemocytometer?
➢ CBC – complete blood count RBC: red blood cell (erythrocyte) count – total number in (x 1012/L)
Hb/Hgb: hemoglobin – amount of protein transports oxygen (g/dL; g/L) (10 g/dL =100 g/L)
Hct: hematocrit – packed RBCs (%; L/L)(42% = 0.42 L/L) RBC Indices: parameters that reveal size and amount of Hb in individual RBCs
MCV: mean corpuscular volume (fL/cell) – average size of RBCs]
MCH: mean corpuscular hemoglobin (pg/cell) – average amount of Hgb in RBCs
MCHC: mean corpuscular hemoglobin concentration (g/dL) – average concentration of Hgb in RBCs
RDW: red cell distribution width – variability in RBC volumes (anisocytosis)
PLT: platelet (thrombocyte) count – total number in (x 109 /L) MVP: mean platelet volume (fL/cell)
WBC: white blood cell (leukocyte) count – total number in (x 109 /L) Differential: % of each individual ty
CBC
Hb/Hgb:
Hct:
RBC indices
MCV:
MCH:
MCHC:
RDW:
PLT
WBC
Differential
RBC
rbc direct count
Hemoglobinopathies, reactive conditions, hypoxic environments, EPO tumors, polycythemia vera
Anemia
dehydration (physio), COPD, CHF, Cancer, smoking, high altitude, excess EPO
what is the total number of microliter of blood?
is rbc direct count/analyzer?
what causes erythrocytosis
what causes erythrppenia
increased HgB indicates right
Hemoglobin (Hb / Hgb)
● Concentration of hemoglobin in whole blood
● Direct measure
○ Expressed in grams per deciliter (g/dL or g/L)
● Indication of oxygen-carrying capacity
● Interpretation of levels
○ Increased = physiologic (dehydration), pathologic (COPD,
CHF, Cancer), smoking, living in high altitudes, excess
erythropoietin
○ Decreased = anemia
what is concentration of hemoglobin in whole blood >
Is hemoglobin a direct or indirect measure, and how it is measure?
What is hemoglobin an indication of>
What are increased hemoglobin levels indicating?
what are decreased hemoglobin levels indicating?
Hematocrit (Hct)
● Portion of blood occupied by RBCs
● Expressed as % (%; L/L) [Example...42% = 0.42 L/L]
● Directly measured by centrifugation / automation or
calculated using the following formula
HCT (%)= (RBC x MCV) / 10
● Usually directly proportional to RBC and Hb
○ “Rule of Three” = (RBCx3=Hb, Hbx3 = Hct)
● Indicator of blood volume changes or hydration status
○ Low = anemia, blood loss
○ High = Polycythemia, dehydration
what describes the portion of blood occupied by RBCs?
is hematocrit direct or indirect measure?
what is the hct formula?
hematocrit is usually directly proportional to what?
rule of 3?
What does low hematocrit indicate
what does high hematocrit indicate
MCHC=(Hbg/Hct) x 100
High mchc indicates= iron overload, spherocytosis, macrocytic anemia, blood disorders, medications
low mchc (under 32) indicates what=iron deficiency anemia
what is the formula for MCHC
High mchc (HYPERCHROMIA.) >36indicates
low mchc (under 32) )Hypochromia) indicates what
MCV (size) = Hct/RBC (Reference range: 80-100 fL)
• Direct measure or calculated (10 x Hct / RBC)
• Allows the classification of anemia
what is mcv size equation
what is the mesured as?
what does MCV allow for the classification of?
➢ RDW = variation in volume / size (normal
variabililty <5% )
❑ RDW-CV = SD of MCV x 100 / MCV
❑ RDW-SD = directly measured; not affected by MCV
• Reference range: 11.5-14.6%
Anisocytosis (varying size) vs Poikilocytosis (diff shaped)
Increase RDW indicates what?
what is the RDW equation:
How do you describe RBC which are varying sizes?
how do you describe RBC that are differently SHAPED?
Blood smear- run for anisocytosis OR pokilcytosis
➢ Confirm CBC results
➢ Review erythrocyte morphology
➢ Maturity / presence of abnormal cells
➢ Shape: poikilocytosis (abnormal shape)
➢ Size: anisocytosis (variation in size)
➢ Color: normochromia or hypochromia
➢ Inclusions (infection) / Granulation (toxicity)
➢ Arrangement: rouleaux or aggregates
If you see anisocytosis or Poikilocytosis - what are we running?
what basic things can a blood smear look at ?
in general
shape
size
color
inclusion vs granulation
arragement
anemia is a decrease in the total amount of RBC
Decreased blood cell PRODUCTION?
INTRINSIC BONE MARROW DYSFUNCTION
meds, dx,genetics, nutrition deficiency, hormone imbalance
blood loss?
periods, GI bleeds, trauma, surgery
RBC destruction?
hemolysis, imtravasuchalr, autoimmune, infections, toxins
extravascular, genetics
what is anemia?
what are major causes of Decreased blood cell PRODUCTION?
What are major causes of blood loss?
What are major causes of RBC destruction?
Anemia: yellow eyes, SOB, weak, pale stool, chest pain, angina, heart attack, low BP, fatigue, dizziness, fainting
SEVERE anemia: red eye
what are symptoms of anemia?
what are symptoms of SEVERE anemia?
Reflex tests:
➢ peripheral blood smear
➢ bone marrow biopsy
➢ reticulocyte count
➢ Immature reticulocyte fraction
➢ Reticulocyte hemoglobin content (CHr)
➢ haptoglobin
➢ bilirubin
➢ direct antibody test (DAT) for autoimmune
34
what are some reflex test for anemia>
decreased RBC, BLOOD LOSS, or RBC destruction
so again, what three main things cause anemia
Reticulocyte
Haptoglobin
Bilirubin
Immature RBC with residual RNA that is newly released from the bone marrow
Protein in blood that carries free Hgb to liver for metabolism and excretion
Breakdown product of heme catabolism
Measures the number of reticulocytes in circulation
➢ Reticulocyte = immature RBC with residual RNA, newly
released from the bone marrow into the blood stream
➢ Indicator of bone marrow function to produce RBCs
MCV (they be BIG), MCHC (more hgb)
Reticulocytes can show slightly more blue than red cells
what does a reticulocyte count measure?
what is a reticulocyte?
what does a low or high reticulocyte count give insight to?
what measures can reticulocytes throw off balance?
How can reticulocytes present on cbc?
High reticulocyte: normal bone barrow could be compensating for anemia
Low reticulocyte count: bone marrow dysfunction failure
see why anemia occurred
high reticulocyte count indicate
low reticulocyte counts indicate
why do we run a reticulocyte count
corrects for variance in reticulocyte maturation time in circulation and total rbc circulation
what is the purpose of the reticulocyte INDEX
NOTE: low or high RI is similar to reticulocyte reasons
RETIC-RET-HE/CHR
Measures retic Hgb content in real time and the functional availability of iron during Hgb synthesis
(decreased levels can predict iron deficiency anemia even before it develops)
what is the purpose of RETIC-RET-HE/CHR test?
what can RETIC-RET-HE/CHR test predict?
Separates different types of Hgb in the blood via an electric current to investigate, screen, and monitor hemoglobin disorders - Normal is Hgb A, with little amounts of A2 or HgbF
Separates different types of hemoglobin in the blood by
electric current
● Used to investigate, diagnose, screen, and monitor
abnormal hemoglobin disorders
● Automated analysis
● Interpretation of results
○ Normal = predominant band of Hgb A, small amounts
Hgb A2, and HgbF (fetal)
○ HgbS = Sickle cell anemia
○ HgbC = linked to hemolytic anemia
what does HgB electrophoresis do?
What should you expect to see on a normal electrophoresis?
In adults? In a fetus?
HgbS is a sign of
HgbC is a sign of
HgbF
microcytic (small)
hypochromic (pale)
high RDW: great variation in sizes in microcytic-hypochromic
Small and pale RBCs
○ Low MCV / Low MCHC
○ High RDW
● Most common type of anemia
● Most common cause = Iron
deficiency
what is the most common type of anemia?
Microcytic Hypochromic anemia is the most common cause of ?
how does microcytic-hypochromic anemia mean/ present in the cell?
Normocytic normochromic
normal size and normal color
Anemia with normal sized and colored RBCs that is most commonly caused by chronic disease
what is the most common type of anemia of chronic disease?
how does the blood cell present?
how is the mcv,mchc, and rdw?

Macrocytic -Hyperchromic
Anemia
● Abnormally large RBCs with
more Hgb
○ High MCV / High MCHC
● Represented primarily by
Megaloblastic Anemias (B12,
Folate deficiencies)
● Classic feature of megaloblastic
cells (hypersegmented
neutrophils)
what anemia is commonly found with megaloblastic anemias:
what are they
what is a classic feature of megaloblastic cells?
how would mcv/mchc present?
Methylmalonic Acid
Measures the amount of MMA
(an organic acid by product of
protein metabolism)
• Helpful in early or mild B12
deficiency
• Increased serum MMA indicates
a decreased Vit B12
(MMA) Homocysteine
Amino acid byproduct of
methionine metabolism – not used
to build proteins
• Hyperhomocyteinemia = elevated
if Vit B6, B9, B12 deficiency
• Elevated levels increase risk of
CVD, Stroke, Thrombus,
Osteoporosis, Cognitive decline
what does MMA (methylmalonic acid measure)?
what is mma most helpful with and what does an increase in mma indicate?
what does homocysteine measure?
what does hyperhomocyteinemia measure?
what do elevated homocysteine levels increase the risk of?
DO THE PRACTIC QS on slides
48-53
Hemolytic anemia (normocytic normochromic)
RBCs are broken down faster than they are produced (retics UP, LDH UP) and classified as intrinsic or extrinsic
Intrinsic
defect with in the RBC usually genetic (sickle cell, G6PD, etc)
Extrinsic
Factors outside RBC usually acquired (autoimmune, medications, trauma - check spleen and liver)
what is hemolytic anemia?
Intrinsic/Intravascular Anemia:
meaning
causes
Extrinsic/Extravascular Anemia:
What should you measure if you find extrinsic anemia?
meaning
causes
Haptoglobin
● Measures the amount of haptoglobin
○ Protein produced by the liver
○ Binds with free Hgb to prevent damage to tissues
● Removed from the blood by the liver and spleen
● Clinical Significance of levels
○ Low = oxidative stress / damage to tissues
(Hemolytic anemia, Liver disease, CVD, CA)
○ High = inflammation, medications
What does haptoglobin measure?
How is haptoglobin moved from the blood?
what does high haptoglobin indicate?
what does low haptoglobin indicate?
Direct antibody testing (DAT)
Test that detects antibody coatings on RBCs and a positive result is associated with
+++indicates autoimmune problem not 100% sensitive/specific
can have false + in individuals
neg- none detected
autoimmune hemolytic anemia (hot/cold)
, Hemolytic disease of the newborn, transfusion reactions, drug induced hemolysis
what does direct antibody test detect?
if DAT is positive?
if DAT is negative?
what are DAT associated conditions mc?
Hemorrhagic anemia
What type of anemia is due to excessive blood loss and has NO signs of hemolysis on lab test - can be caused by trauma, menstrual cycles, GI, medications, etc
more practice q
more practice qs