Archer: Cardiology EKG
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
blood flow through heart
deoxygenated blood from body:
1. superior inferior vena cava; 2. right atrium; 3. tricuspid valve; 4. right ventricle; 5. pulmonic valve; 6. pulmonary arteries; 7. out to lungs
oxygenated blood from lungs:
1. pulmonary veins; 2. left atrium; 3. mitral valve; 4. left ventricle; 5. aortic valve; 6. aorta; 7. out to body
preload
amount of blood returning to right side of the heart (from the body)
afterload
pressure against which the left ventricle must pump to eject blood
compliance
Compliance describing how easily the heart muscle expands when filled with blood, allowing it to pump effectively.
contractility
strength of contraction of heart muscle
stroke volume
volume of blood pumped out of the ventricles with each contraction
cardiac output
amount of blood the heart pumps through circulatory system in a minute
Cardiac output = ?
Cardiac output is the amount of blood pumped by the heart per minute, and it is determined by multiplying the heart rate (number of beats per minute) by the stroke volume (amount of blood pumped per beat). The cardiac output is important because it affects the delivery of oxygen and nutrients to the organs
with more preload - blood coming back to the heart more
higher cardiac output
more blood coming back to right side of heart, more stretch in right atrium leads to stronger contraction => ultimately leading to _____________
higher cardiac output
more afterload leads to?
When there is more afterload (resistance to blood flow), it becomes harder for the heart to pump blood, resulting in lower cardiac output.
compliance and contractility incr. then
When compliance (stretchiness) and contractility (strength) of the heart increase, it can pump more blood with each beat, increasing the overall amount of blood pumped by the heart.
incr. stroke volume =
incr cardiac output
causes of decrease cardiac output
-bradycardia
-arrhythmias
-hypotension
-myocardial infarction (heart attack)
-cardiac musc. disease
causes of increase cardiac output
-incr. blood volume
-tachycardia (high HR)
-meds - Ace inhibitors, ARBS, nitrates, inotropes
ekg's
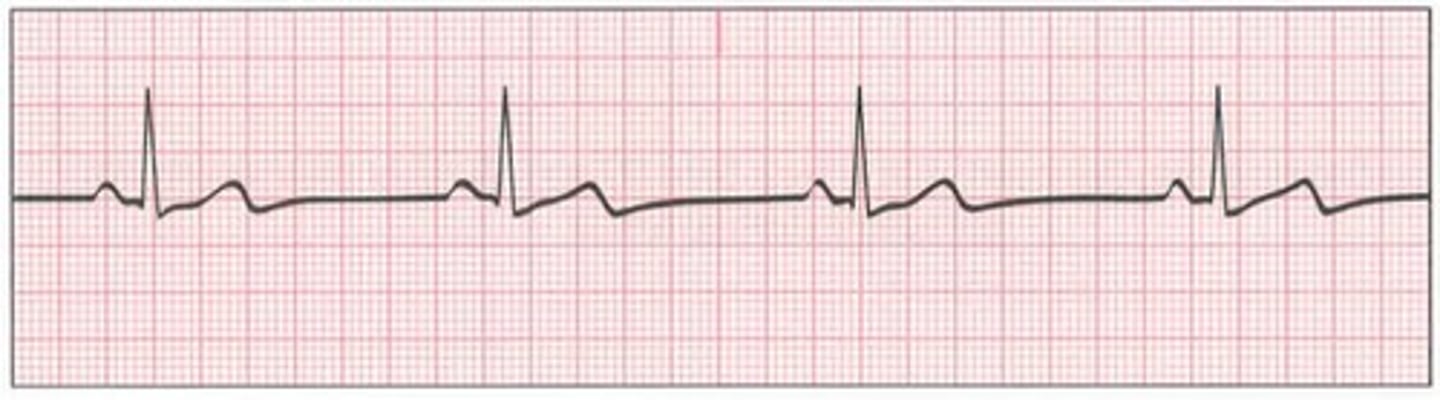
normal sinus rhythm
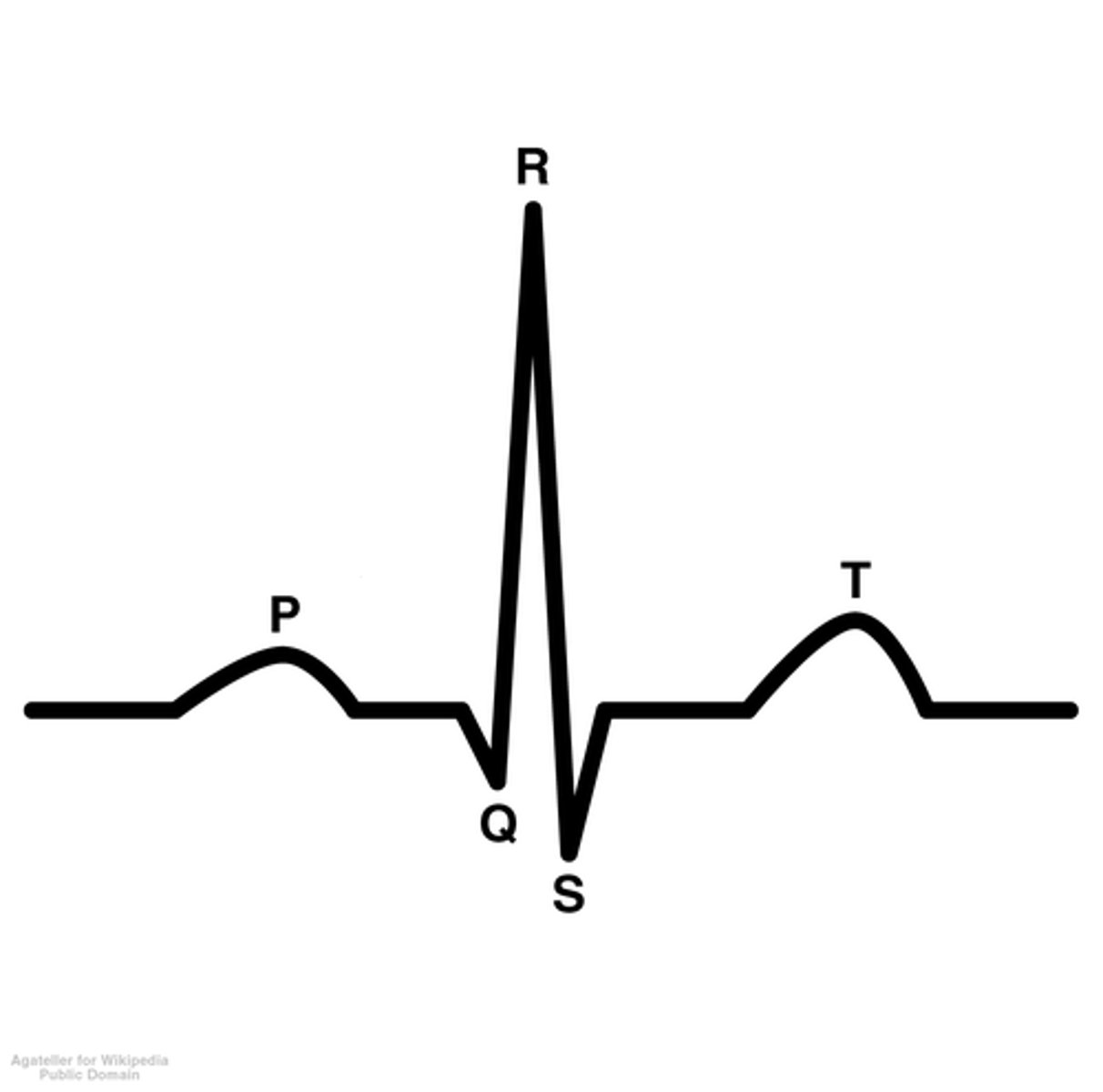
Normal sinus rhythm that has heart beats regularly, with a narrow QRS complex, a consistent rate of 60-100 beats per minute, and each QRS complex is preceded by a P wave.

sinus bradycardia
p for every qrs, looks regular but rate is slower; rate less than 60
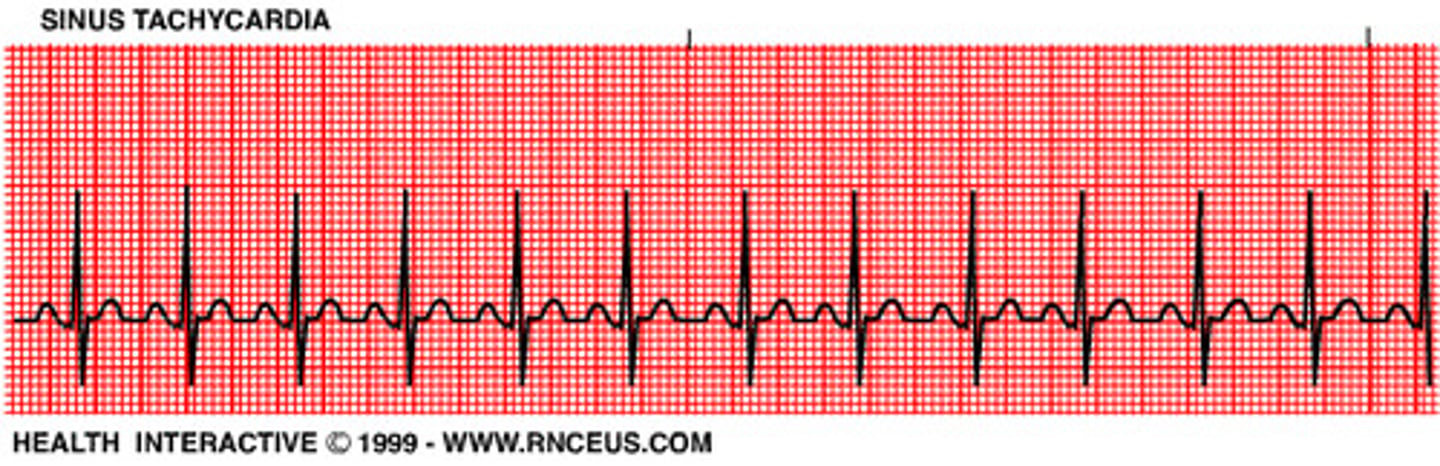
sinus tachycardia
p for every qrs, looks regular but rate is faster; rate greater than 100
tachycardia is a compensatory mechanism to hypotension
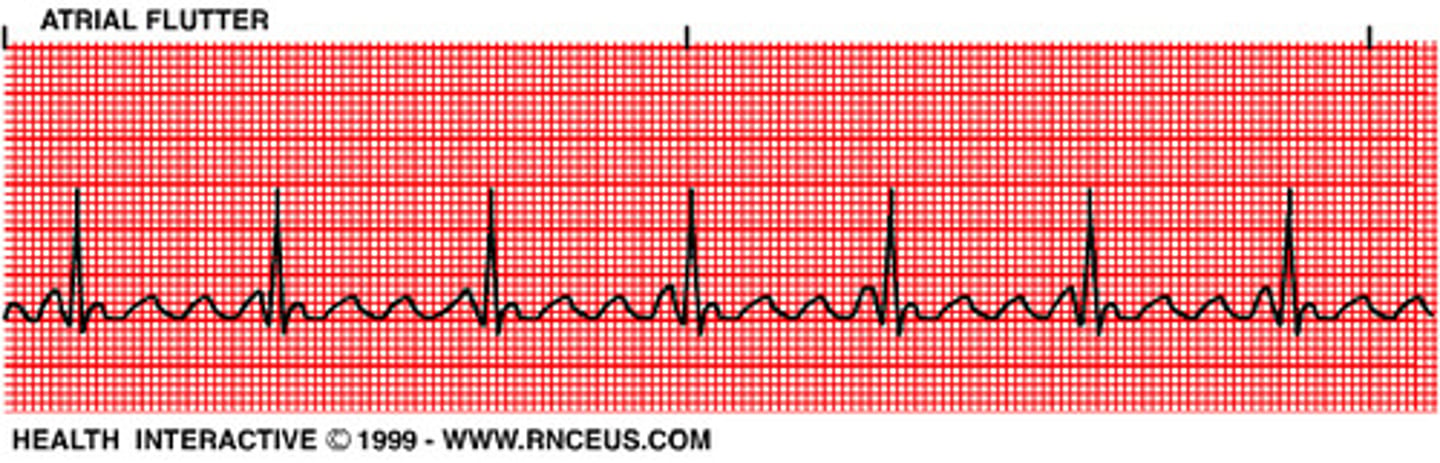
atrial flutter
"saw tooth"
no pr interval
still has qrs
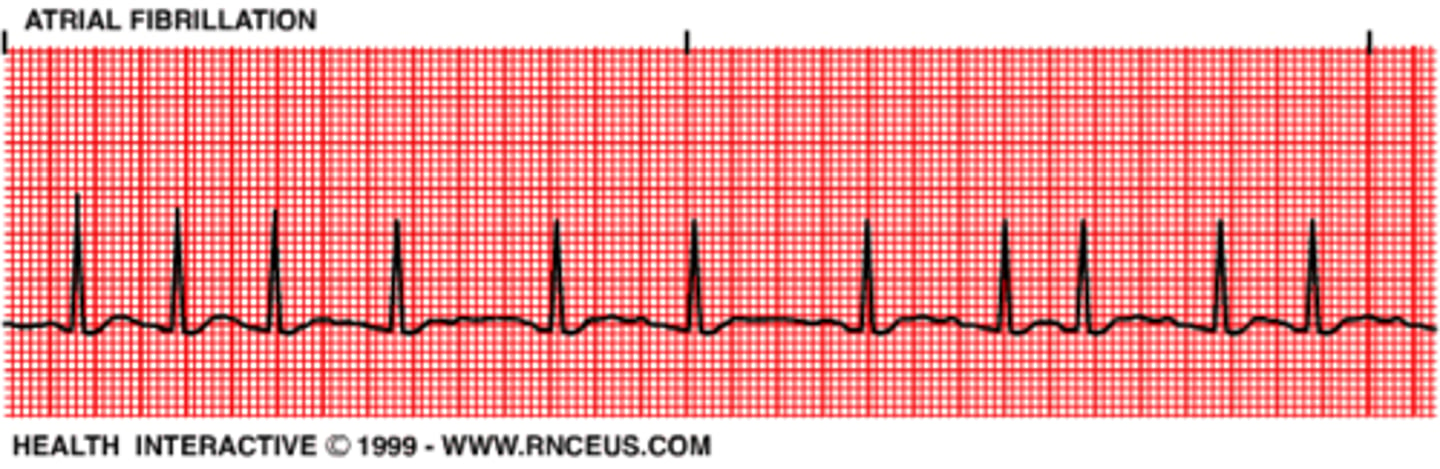
atrial fibrillation
"wavy" lines smaller than saw tooth in atrial flutter
no pr interval
still has qrs
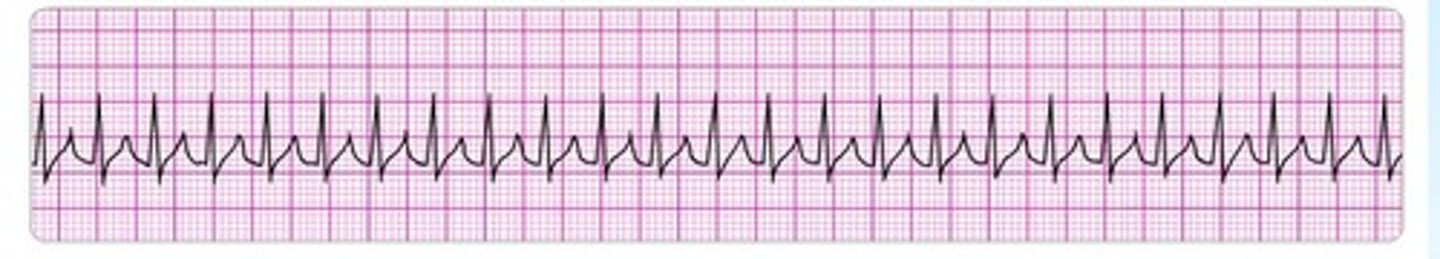
Supraventricular tachycardia (SVT)
p waves are hidden in T waves
rate: 150-250
regular waves (no variation)
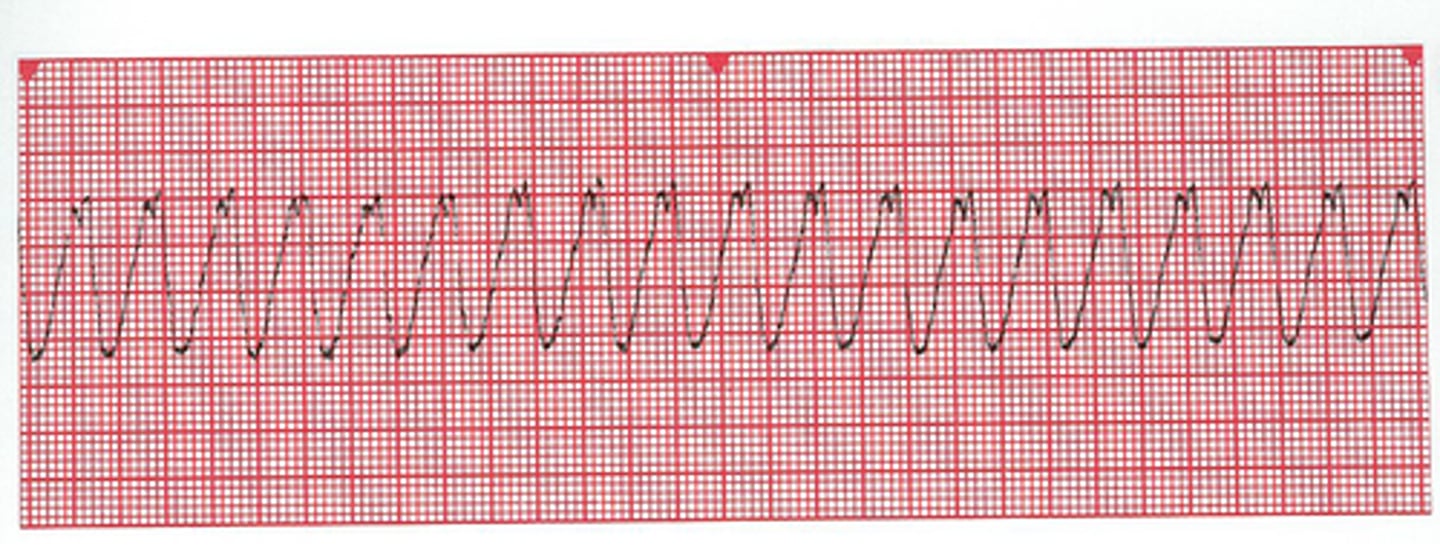
ventricular tachycardia (V-tach)
"wide + bizarre"
qrs are no longer regular
no p waves
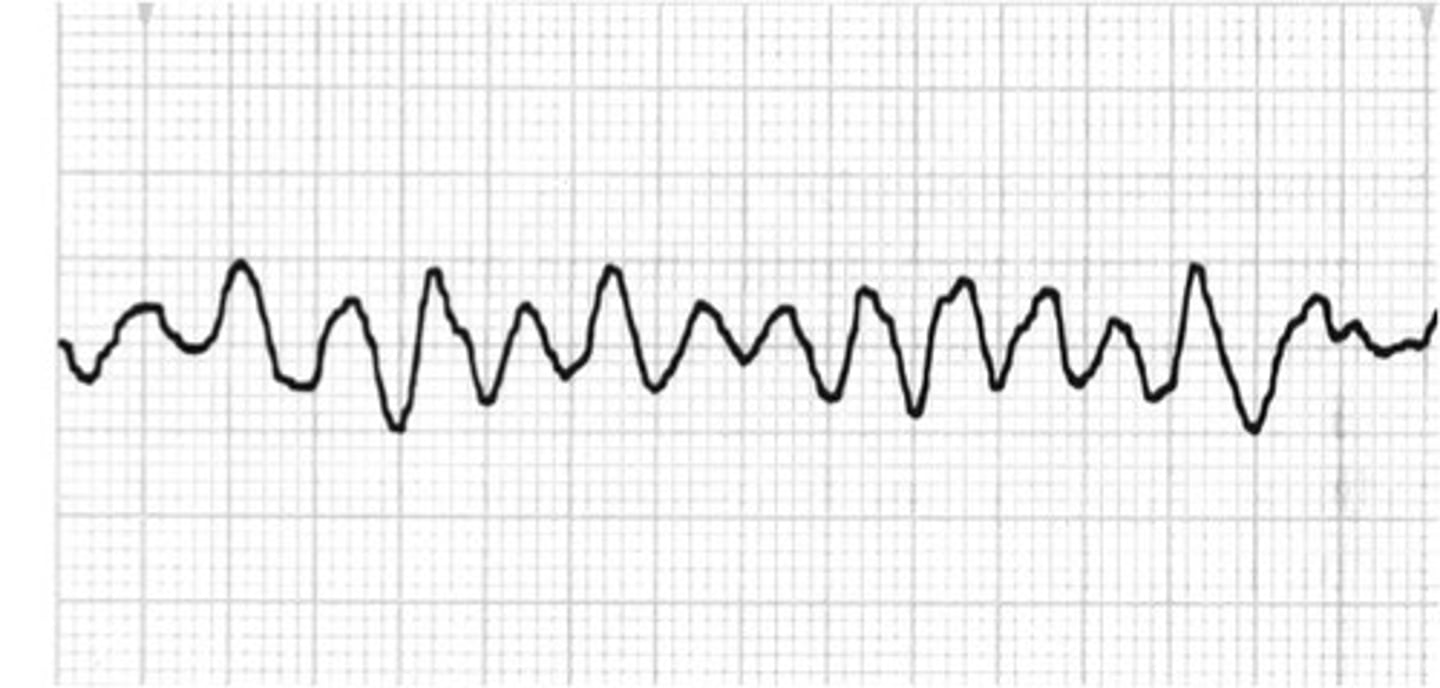
ventricular fibrillation (v-fib)
Ventricular fibrillation (v-fib) is like an electrical chaos in the heart where there is no organized rhythm, resulting in a quivering motion instead of a normal pumping action, and it can be treated with defibrillation.
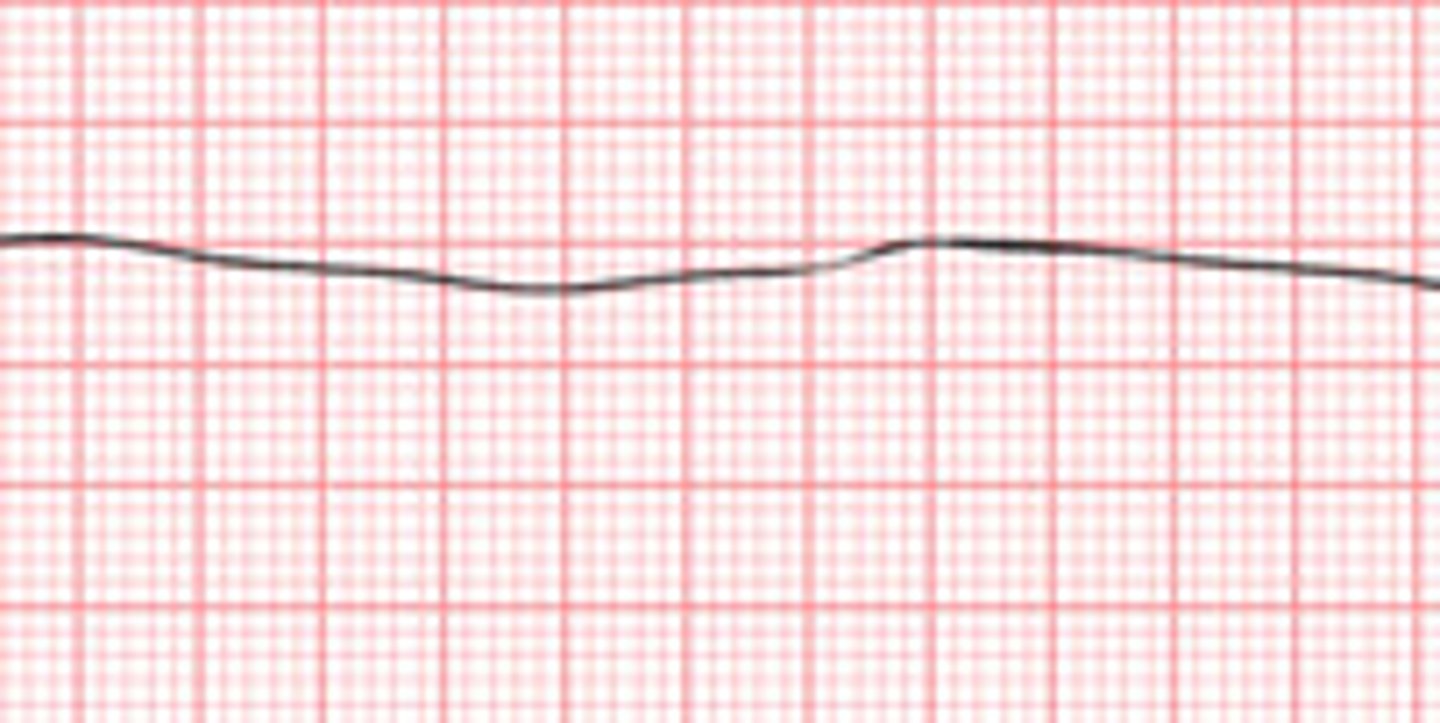
asystole
Asystole is like a flat line on a heart monitor, and the priority nursing action is to assess the patient because in asystole there is no electrical activity, so CPR is needed.
Coronary artery disease
Coronary artery disease is the most common cardiovascular disease, which can be thought of as having two main types: chronic stable angina (like a predictable chest pain) and acute coronary syndrome (like a heart attack).
what is Chronic stable angina? (chronic type of coronary artery disease)
narrowing of coronary arteries with plaque build up=> decr. blood flow to heart => ischemia (inadequate blood flow to heart) => chest pain
treating Chronic stable angina? (chronic type of coronary artery disease)
To treat chronic stable angina, you can use rest or nitroglycerin, which works by dilating veins and arteries; think of it as a "magic pill" that opens up the blood vessels to relieve chest pain, but be careful with light exposure and expect a possible headache.
when nitroglycerine not helping chronic stable angina it becomes
acute coronary syndrome aka myocardial infarction
acute coronary syndrome aka myocardial infarction is
Acute coronary syndrome, also known as a heart attack, happens when there is reduced blood flow and oxygen to the heart, leading to tissue damage and necrosis.
assessment of myocardial infaction
Assessment of myocardial infarction involves intense chest pain, severe indigestion or discomfort, along with shortness of breath.
labs for myocardial infarction
elevated troponin with MI (troponin is a cardiac biomarker)
treatment for MI?
The gold standard treatment for myocardial infarction (heart attack) is taking a patient to a cath lab within 90 minutes to open the blocked artery, before that, giving them oxygen, aspirin, nitroglycerine, and morphine to help with symptoms and blood flow.
education for MI:
avoid isometric exercises; focus on aerobic exercises (ex. walking)
-diet: low fat, salt and cholesterol
Heart failure
heart muscle cannot pump enough blood to meet body's needs
2 types: left and right
Left sided heart failure
Left-sided heart failure is when the left side of the heart is unable to pump blood effectively to the body, causing blood to back up in the lungs, leading to symptoms like pulmonary congestion, wet lung sounds, difficulty breathing, coughing, blood-tinged sputum, a third heart sound (S3), and difficulty breathing while lying down (orthopnea).
Right sided heart failure
Right sided heart failure is when the heart is unable to pump blood effectively to the lungs, causing a backup of blood in the body, leading to symptoms like swollen jugular veins, edema, enlarged liver and spleen, fluid accumulation in the abdomen, weight gain, fatigue, and loss of appetite. The main cause of right sided heart failure is left sided heart failure.
Treatment for HF (left and right)
The treatment for heart failure involves reducing the workload of the heart by decreasing the afterload with ACE inhibitors and ARBs, increasing contractility with digoxin, and promoting diuresis with diuretics to reduce excess fluid.
education w/ HF
Education with heart failure involves following a low sodium diet to release excess fluids, and monitoring daily weight to detect sudden increases of 2-3 pounds in one day, which should be reported.
high blood pressure values
normal being 120/80, elevated being 120-129/80, high blood pressure being greater than 130/80, and hypertensive crisis being greater than 180/120.
non modifiable risk factors for hypertension
fam history, african american race, incr. age
modifiable risk factors with hypertension
obesity, HLD, stress, smoking, high salt intake, caffeine
assessments of hypertension
vision changes, headache, dizzy, nosebleeds, SOB, angina
complications of hypertension
-stroke
-MI
-renal failure
-heart failure
-vision loss
treatment for hypertension
The flashcard is about the treatment for hypertension, which includes taking medications like ACE inhibitors, beta blockers, calcium channel blockers, and diuretics, as well as making dietary changes like reducing salt intake and avoiding caffeine and alcohol, quitting smoking, losing weight, and adopting a more active lifestyle with more walking.
Shock
where the vital organs are not getting enough oxygen, so cells resort to a backup energy source, producing lactate, and the type of shock depends on which part of the cardiovascular system is disrupted.
types of shock
hypovolemic, cardiogenic, distributive
"heart" sends "blood" thru "vasculature"
three things determine type of shock
hypovolemic shock
Hypovolemic shock - there's not enough blood circulating in the body, leading to low blood flow and decreased cardiac output.
causes of hypovolemic shock
Hypovolemic shock occurs when there is a significant decrease in blood volume, which can be caused by bleeding, severe injury, excessive fluid loss from vomiting or diarrhea, or burns.
hypovolemic shock assessment
Hypovolemic shock assessment: Your body initially compensates by speeding up your heart rate, but as it worsens, you'll experience low blood pressure, weak pulses, slow heart rate, decreased consciousness, cool and clammy skin, and reduced urine output.
treatment for hypovolemic shock
The treatment for hypovolemic shock involves fixing the cause and replacing lost fluids with IV fluids, isotonic or blood products. And supporting blood flow with vasopressors that constrict blood vessels.
Cardiogenic shock
-PUMP failure
-heart not pumping blood to body
causes of cardiogenic shock
Cardiogenic shock occurs when the heart is unable to pump enough blood to meet the body's needs, and it can be caused by conditions like heart attack, heart failure, blood clots, or a buildup of fluid around the heart (cardiac tamponade).
assessment cardiogenic shock
Assessment of cardiogenic shock involves looking for signs of decreased perfusion (like low blood pressure, weak pulses, cool and clammy skin, decreased urine output, and altered mental status) as well as signs of volume overload (such as jugular vein distension, crackles in the lungs, shortness of breath, muffled heart sounds, and an S3 heart sound).
treatment of cardiogenic shock
treat the cause:
-if MI: take to cath lab for PCI
-if Pulmonary embolism: use thrombolytics to free of clot
-if tamponade: perform pericardiocentesis: needle inserted into pericardial sack to pull out fluid
in meantime:
-improve contractility with dopamine
-decr. afterload: same meds as hypertension
distributive shock
Distributive shock is like a sudden collapse of the body's blood vessels due to an immune or autonomic response, causing a drop in blood pressure and inadequate oxygen delivery, similar to a deflated balloon unable to distribute air properly.
causes of distributive shock
Distributive shock can be caused by different factors, like an allergic reaction (anaphylactic), a spinal cord injury (neurogenic), or a systemic infection (septic) that triggers inflammatory responses in the body.
assessment of distributive shock
Assessment of distributive shock is similar to cardiogenic and hypovolemic shock, but the skin is warm and flushed instead of cool and clammy, and it can be caused by anaphylactic reactions (hives, rash, swelling, wheezing), neurogenic factors (spinal cord injury), or septic conditions (fever due to infection).
Treatment of distributive shock
Treating distributive shock involves specific interventions for different types: anaphylactic shock requires epinephrine and other medications like corticosteroids, and bronchodilators. Neurogenic shock needs cooling and supportive care, and septic shock involves IV antibiotics and fluids.
when a nclex questions says restless (or restlessness) think of
When a NCLEX question mentions restlessness, think of hypoxia, which means not enough oxygen reaching the brain, leading to decreased blood flow and decreased level of consciousness.