Chapter I
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
Pharmacokientics
refers to what the body does to the drug
Pharmacodynamics
refers to what the drug does to the body
Absorption, distribution, metabolism, elimination
what are the four pharmacokinetic properties
enteral, parenteral, topical
Major routes of drug administration include —, —, and —
enteral
— administration (administering a drug by mouth) is the safest and most common, convenient, and economical method of drug administration.
The drug may be swallowed, allowing oral delivery, or it may be placed under the tongue (sublingual), or between the gums and cheek (buccal), facilitating direct absorption into the bloodstream
activated charcoal
Oral administration provides many advantages. Oral drugs are easily self-administered, and toxicities and/or overdose of oral drugs may be overcome with antidotes, such as —.
low
However, the pathways involved in oral drug absorption are the most complicated. A wide range of oral preparations is available including enteric-coated and extended-release preparations.
Does a low or high pH inactivate drugs?
enteric coated preparations
What type of coating is a chemical envelope that protects the drug from stomach acid, delivering it instead to the less acidic intestine, where the coating dissolves and releases the drug
aspirin
Enteric coating is useful for certain drugs (for example, omeprazole) that are acid unstable. Drugs that are irritating to the stomach, such as —, can be formulated with an enteric coating that only dissolves in the small intestine, thereby protecting the stomach.
oral and sublingual/buccal
what are the two types of enteral drugs
enteric coated and extended release preparations
what are the two types of oral prepations
extended release medications
These medications have special coatings or ingredients that control the drug release, thereby allowing for slower absorption and a prolonged duration of action. These formulations can be dosed less frequently and may improve patient compliance
extended release preparations
Additionally, these formulations may maintain concentrations within the therapeutic range over a longer period of time, as opposed to immediate-release dosage forms, which may result in larger peaks and troughs in plasma concentration. What type of preparations are these?
2-4 hours, 6x dialy
ER formulations are advantageous for drugs with short half-lives. For example, the half-life of oral morphine is —, and it must be administered — to provide continuous pain relief
two
However, only — doses are needed when extendedrelease tablets are used. Unfortunately, many ER formulations have been developed solely for a marketing advantage over immediate-release products, rather than a documented clinical advantage.
sublingual/buccal preprations
this type of oral prepartions allows a drug to diffuse into the capillary network and enter the systemic circulation directly. It has several advantages, including ease of administration, rapid absorption, bypass of the harsh gastrointestinal (GI) environment, and avoidance of firstpass metabolism
parenteral route
This route introduces drugs directly into the systemic circulation. It is also used for drugs that are poorly absorbed from the GI tract (for example, heparin) or unstable in the GI tract (for example, insulin).
true
true or false
Parenteral administration is also used if a patient is unable to take oral medications (unconscious patients) and in circumstances that require a rapid onset of action. In addition, parenteral routes have the highest bioavailability and are not subject to first-pass metabolism or the harsh GI environment.
parenteral adiministration
This drug administration provides the most control over the actual dose of drug delivered to the body. However, these routes of administration are irreversible and may cause pain, fear, local tissue damage, and infections
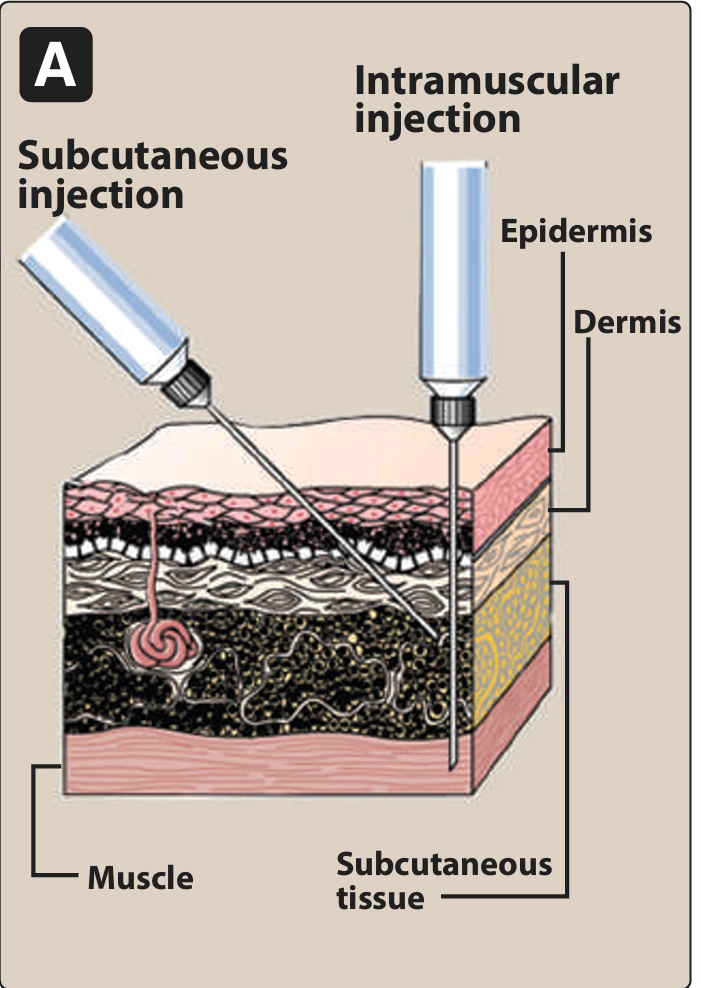
intravascular (intravenous or intra-arterial), intramuscular, and subcutaneous
whtat are the three major parenteral routes
IV injection
what is the most common parenteral route that is useful for drugs that are not absorbed orally
intavenous
what delivery permits a rapid effect and a maximum degree of control over the amount of drug delivered.
It is advantageous for drugs that cause irritation when administered via other routes, because the substance is rapidly diluted by the blood.
bolus, IV infusion
In IV, when injected as a —, the full amount of drug is delivered to the systemic circulation almost immediately. If administered as an —, the drug is infused over a longer period of time, resulting in lower peak plasma concentrations and an increased duration of circulating drug levels
IV
Unlike drugs given orally, those that are injected cannot be recalled by strategies such as binding to activated charcoal. — injection may inadvertently introduce infections through contamination at the site of injection. It may also precipitate blood constituents, induce hemolysis, or cause other adverse reactions if the medication is delivered too rapidly and high concentrations are reached too quickly
aqueous, depot
Drugs administered IM can be in — solutions, which are absorbed rapidly, or in specialized — preparations, which are absorbed slowly.
polyethylene glycol
Depot preparations often consist of a suspension of the drug in a nonaqueous vehicle such as —. As the vehicle diffuses out of the muscle, the drug precipitates at the site of injection. The drug then dissolves slowly, providing a sustained dose over an extended period of time.
simple diffusion
Like IM injection, SC injection provides absorption via — and is slower than the IV route
hemolysis and thrombosis
what risks are lessened by SC administration that are present in IV route and may provide constant, slow, and sustained effects.
false
true or false
SC route can be used with drugs that cause tissue irritation, because severe pain and necrosis may occur.
oral and nasal inhalation routes
this is a route that have almost the same rapid effect as those with IV Bolus.
inhalation
Drugs that are gases (for example, some anesthetics) and those that can be dispersed in an aerosol are administered via —. This route is effective and convenient for patients with respiratory disorders (such as asthma or chronic obstructive pulmonary disease), because the drug is delivered directly to the site of action, thereby minimizing systemic side effects.
desmopressin
this drug is adminitered intransally in the treatment of diabetes insipidus
blood-brain barrier, CSF
The — typically delays or prevents the absorption of drugs into the central nervous system (CNS). When local, rapid effects are needed, it is necessary to introduce drugs directly into the —, This is applicalbe to INTRATHECAL/INTRAVENTRICULAR
amphotericin B
it is used intrathecally for the treatment of cryptococcus menigitis
topical
What application is used when a local effect of the drug is desired
clotrimazole
For example, — is a cream applied directly to the skin for the treatment of fungal infections.
transdermal
This route of administration achieves systemic effects by application of drugs to the skin, usually via a patch. This route is most often used for the sustained delivery of drugs
The rate of absorption can vary markedly, depending on the physical characteristics of the skin at the site of application, as well as the lipid solubility of the drug
nicotine transdermal preprations
this transdermal preaprations is used to facilitate smoking cessation
true
true or false
Because 50% of the drainage of the rectal region bypasses the portal circulation, the biotransformation of drugs by the liver is minimized with rectal administration
rectal route
What route has the additional advantage of preventing destruction of the drug in the GI environment. This route is also useful if the drug induces vomiting when given orally, if the patient is already vomiting, or if the patient is unconscious
Commonly used to administer ANTIEMETIC AGENTS
passive diffusion
The driving force for passive absorption of a drug is the concentration gradient across a membrane separating two body compartments. In other words, the drug moves from a region of high concentration to one of lower concentration.
true
true or false
passive diffusion does not involve a carrier and is NOT SATURABLE
facilitated diffusion
These carrier proteins undergo conformational changes, allowing the passage of drugs or endogenous molecules into the interior of cells and moving them from an area of high concentration to an area of low concentration.
true
true or false
Facilitated diffusion does not require energy and can be saturated
adenosine triphosphate
the hydrolysis of — drives active transport. This mode of drug entry also involves specific carrier proteins that span the membrane.
false
true or false
active transport is not saturable
endocytosis
it involves engulfment of a drug by the cell membrane and transport into the cell by pinching off the drug filled vesicle
exocytosis
Many cells use — to secrete substances out of the cell through a similar process of vesicle formation. it is the reverse of endocytosis
endocytosis
Vitamin B12 is transported across the gut wall via —
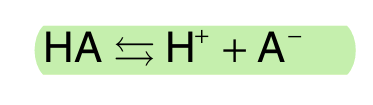
acidic (HA)
Most drugs are either weak acids or weak bases
what drugs release a proton (H+), causing a charged anion (A−) to form (pic)
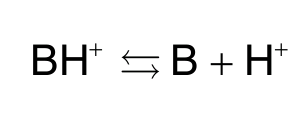
bases (BH+), B
Most drugs are either weak acids or weak bases
Weak — can also release an H+. However, the protonated form of these drugs is usually charged, and loss of a proton produces the uncharged —:
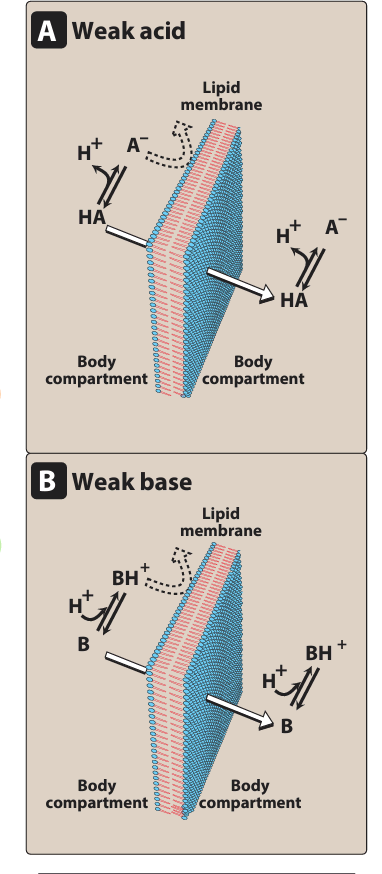
uncharged
a drug passes through membranes more readily if it is —
HA, A-, B, BH+
Thus, for a weak acid, the uncharged, protonated — can permeate through membranes, and — cannot. For a weak base, the uncharged form — penetrates through the cell membrane, but the protonated form — does not.
pKa ionization constant, lower, higher
The — is a measure of the strength of the interaction of a compound with a proton. The — the pKa of a drug, the more acidic it is. Conversely, the — the pKa , the more basic is the drug.
intestine
What organ receives much more blood flow than the stomach, so absorption from this organ is favored over the stomach.
shock
What severely reduces blood flow to cutaneous tissues, thereby minimizing absorption from SC administration?
true
true or false
With a surface rich in brush borders containing microvilli, the intestine has a surface area about 1000-fold that of the stomach, making absorption of the drug across the intestine more efficient.
no
yes or no
If a drug moves through the GI tract very quickly, as can happen with severe diarrhea, is it well absorbed or not?
yes
yes or no
The presence of food in the stomach both dilutes the drug and slows gastric emptying. Therefore, a drug taken with a meal is generally absorbed more slowly
P-glycoprotein
It is a transmembrane transporter protein responsible for transporting various molecules, including drugs, across cell membranes
reduces
P-glycoprotein is expressed in tissues throughout the body, including the liver, kidneys, placenta, intestines, and brain capillaries, and is involved in transportation of drugs from tissues to blood. That is, it “pumps” drugs out of the cells. Thus, in areas of high expression, P-glycoprotein — drug absorption. In addition to transporting many drugs out of cells, it is also associated with multidrug resistance.
bioavailability
It is the rate and extent to which an administered drug reaches the systemic circulation. For example, if 100 mg of a drug is administered orally and 70 mg is absorbed unchanged, the measurement is 0.7 or 70%.
IV
Bioavailability is determined by comparing plasma levels of a drug after a particular route of administration (for example, oral administration) with levels achieved by IV administration.
After — administration, 100% of the drug rapidly enters the circulation.
orally
Bioavailability is determined by comparing plasma levels of a drug after a particular route of administration (for example, oral administration) with levels achieved by IV administration.
When the drug is given —, only part of the administered dose appears in the plasma
area under the curve AUC
By plotting plasma concentrations of the drug versus time, the — can be measured. The total of this reflects the extent of absorption of the drug. Bioavailability of a drug given orally is the ratio of the of this following oral administration to the following IV administration
first pass metabolism
In contrast to IV administration, which confers 100% bioavailability, orally administered drugs often undergo —
This biotransformation, in addition to the chemical and physical characteristics of the drug, determines the rate and extent to which the agent reaches the systemic circulation.
first pass metabolism
When a drug is absorbed from the GI tract, it enters the portal circulation before entering the systemic circulation . If the drug is rapidly metabolized in the liver or gut wall during this initial passage, the amount of unchanged drug entering the systemic circulation is decreased. This is referred to as —
yes
For example, more than 90% of nitroglycerin is cleared during f irst-pass metabolism. Hence, it is primarily administered via the sublingual or transdermal route.]
(YES OR NO)
Drugs with high first-pass metabolism should be given in doses sufficient to ensure that enough active drug reaches the desired site of action.
hydrophillic
Very — drugs are poorly absorbed because of their inability to cross lipid-rich cell membranes.
For a drug to be readily absorbed, it must be largely lipophilic, yet have some solubility in aqueous solutions. This is one reason why many drugs are either weak acids or weak bases.
excipients
Drug absorption may be altered by factors unrelated to the chemistry of the drug. For example, particle size, salt form, crystal polymorphism, enteric coatings, and the presence of — (such as binders and dispersing agents) can influence the ease of dissolution and, therefore, alter the rate of absorption.
true
true or false
Two drug formulations are bioequivalent if they show comparable bioavailability and similar times to achieve peak blood concentrations
Note: Clinical effectiveness often depends on both the maximum serum drug concentration and the time required (after administration) to reach peak concentration. Therefore, two drugs that are bioequivalent may not be therapeutically equivalent
therapeutically
Two drug formulations are said to be — equivalent if they are pharmaceutically equivalent (that is, they have the same dosage form, contain the same active ingredient, and use the same route of administration) with similar clinical and safety profiles.
drug distribution
It is the process by which a drug reversibly leaves the bloodstream and enters the interstitium (extracellular fluid) and the tissues.
IV
For drugs administered —, absorption is not a factor, and the initial phase (from immediately after administration through the rapid fall in concentration) represents the distribution phase, during which the drug rapidly leaves the circulation and enters the tissues
lower
The rate of blood flow to the tissue capillaries varies widely. For instance, blood flow to the “vessel-rich organs” (brain, liver, and kidney) is greater than that to the skeletal muscles. Adipose tissue, skin, and viscera have still (lower or higher) rates of blood flow.
capillary permeability
— is determined by capillary structure and by the chemical nature of the drug. Capillary structure varies in terms of the fraction of the basement membrane exposed by slit junctions between endothelial cells
Liver and spleen = discontinuous capillary structure therefore easier passing
Brain = continuous capillary structure therefore harder passing (through endothelial cells is where the drug passes instead so ionized drugs are not advisable)
albumin
It is the major drug-binding protein and may act as a drug reservoir (as the concentration of free drug decreases due to elimination, the bound drug dissociates from the protein). This maintains the freedrug concentration as a constant fraction of the total drug in the plasma
tissues
Many drugs accumulate in —, leading to higher concentrations in these than in the extracellular fluid and blood.
Drugs may also be actively transported into these, and so reservoirs of these may serve as a major source of the drug and prolong its actions or cause local drug toxicity.
lipophilic, hydrophilic
The chemical nature of a drug strongly influences its ability to cross cell membranes
- drugs readily move across most biologic membranes. These drugs dissolve in the lipid membranes and penetrate the entire cell surface. In contrast, — drugs do not readily penetrate cell membranes and must pass through slit junctions
blood flow to the area
What is the major factor influencing the distribution of lipophilic drugs?
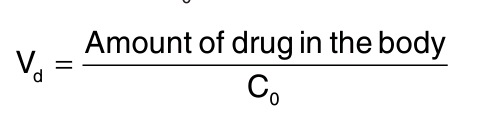
volume of distribution Vd
The apparent — , — , is defined as the fluid volume that is required to contain the entire drug in the body at the same concentration measured in the plasma.
heparin
If a drug has a high molecular weight or is extensively protein bound, it is too large to pass through the slit junctions of the capillaries and, thus, is effectively trapped within the plasma (vascular) compartment.
What drug shows this type of distribution?
aminoglycoside antibiotics
If a drug has a low molecular weight but is hydrophilic, it can pass through the endothelial slit junctions of the capillaries into the interstitial fluid. However, hydrophilic drugs cannot move across the lipid membranes of cells to enter the intracellular fluid.
What drugs show this type of distribution?
ethanol
If a drug has a low molecular weight and is lipophilic, it can move into the interstitium through the slit junctions and also pass through the cell membranes into the intracellular fluid.
What drug exhibit this property?
first order
The fact that drug clearance is usually a — process allows calculation of Vd . It means that a constant fraction of the drug is eliminated per unit of time
hepatic metabolism, billiary elimination, urinary eliminationn
Once a drug enters the body, the process of elimination begins. The three major routes of elimination are —, —, and —
first-order, aspirin
Most drugs are eliminated according to — kinetics, although some, such as — in high doses, are eliminated according to zero-order or nonlinear kinetics.
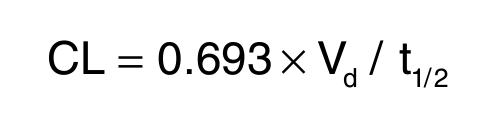
clearance
Metabolism leads to production of products with increased polarity, which allows the drug to be eliminated. — estimates the amount of drug cleared from the body per unit of time.
Michaelis-Menten
First order Kinetics. The metabolic transformation of drugs is catalyzed by enzymes, and most of the reactions obey — kinetics.
first order, linear kinetics
The rate of drug metabolism and elimination is directly proportional to the concentration of free drug, and — kinetics is observed. This means that a constant fraction of drug is metabolized per unit of time (that is, with each half-life, the concentration decreases by 50%).
It is also called as —
zero order, nonlinear kinetics
The enzyme is saturated by a high free drug concentration, and the rate of metabolism remains constant over time. This is called — kinetics (also called — kinetics).
A constant amount of drug is metabolized per unit of time. The rate of elimination is constant and does not depend on the drug concentration.
kidney
What organ cannot efficiently eliminate lipophilic drugs that readily cross cell membranes and are reabsorbed in the distal convoluted tubules?
Therefore, lipid-soluble agents are first metabolized into more polar (hydrophilic) substances in the liver via two general sets of reactions, called phase I and phase II
phase I
What phase reactions convert lipophilic drugs into more polar molecules by introducing or unmasking a polar functional group, such as –OH or –NH
reduction, oxidation, hydrolysis
what reactions are usually involved in phase 1 of drug metabolism?
P450, microsomal mixed function oxidase
The phase I reactions most frequently involved in drug metabolism are catalyzed by the cytochrome — system (also called — oxidases)
CYP
The P450 system is important for the metabolism of many endogenous compounds (such as steroids, lipids) and for the biotransformation of exogenous substances (xenobiotics). Cytochrome P450, designated as —, is a superfamily of heme-containing isozymes that are located in most cells, but primarily in the liver and GI tract.
CYP3A4/5, CYP2D6, CYP2C8/9, CYP1A2
These enzymes have the capacity to modify a large number of structurally diverse substrates. In addition, an individual drug may be a substrate for more than one isozyme. Four isozymes are responsible for the vast majority of P450-catalyzed reactions. They are —
CYP2D6
P450 enzymes exhibit considerable genetic variability among individuals and racial groups. Variations in P450 activity may alter drug efficacy and the risk of adverse events. — , in particular, has been shown to exhibit genetic polymorphism. It’s mutations result in very low capacities to metabolize substrates
Clopidogrel
This drug carries a warning that patients who are poor CYP2C19 metabolizers have a higher incidence of cardiovascular events (for example, stroke or myocardial infarction) when taking this drug.
It is a prodrug, and CYP2C19 activity is required to convert it to the active metabolite.