clinically important gram + bacteria
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
coagulase test
slide coagulase test: agglutination reacts
staphytect test: agglutination reacts
tube coagulase test: fibrin clot = coagulase positive
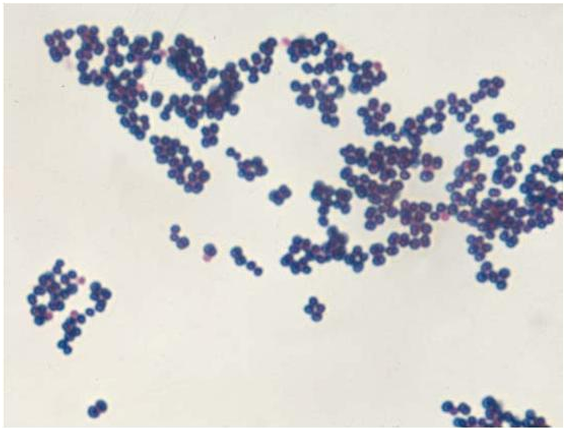
staphylococci
gram positive cocci in clusters
opportunistic bacteria
low intrinsic virulence - usually don’t cause infections in normal patients
may cause serious infections in certain circumstances - immunocompromise. foreign body e.g. staph. epidermidis
virulent bacteria
colonization
infections e.g. S. aureus
normal flora
staphlycocci
staphylococcus aureus
found in moist skin folds, mucosal surfaces, nasopharynx. increased in diabetes mellitus, intravenous drug users and foreign body is present
lots of virulence factors - even though it colonizes healthy adults
infection occurs when there is a break in the skin or there is entry through the mucous membranes allowing access to adjoining tissues
MSRA: methicillin resistance
pathogenesis
gets in - portal of entry
attaches to cells
defeats/evades the immune system
causes damage to host cells
gets out and spreads further
portal of entry
ingestions
inhalation
penetration/inoculation
sexual
transplacental (vertical transmission)
attaches to cells/surfaces
microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) - surface proteins that facilitate initial attachment to hose tissue
fibrin/fibrinogen binding protein (clumping factor) - attachment of blood clots and traumatized tissue
fibronectin, fibrinogen and collagen binding proteins - e.g. collagen binding protein promoted collagen attachment and is found in strains that cause osteomyelitis/septic arthritis
capsule - adherence to foreign bodies e.g. intravascular )IV) catheter
immune evasion
inhibition of phagocytosis (capsule)
survival within phagocytes
production of extracellular substances that promote invasion
invasins
enzymes
virulence factor - coagulase
enzyme - converts fibrinogen into fibrin clot. coats bacterial cells in self protein
virulence factor - protein A
surface protein - binds IgG(heavy chain Fc region) hindering opsonization and phagocytosis
virulence factor - alpha toxin
hemolysin - causes lysis of blood components, particularly monocytes and platelets
virulence factors - staphylokinase
enzyme - dissolves fibrin clots to facilitate spread
virulence factors - hyaluronidase
enzyme - breaks down hyaluronic acid in connective tissue, aiding in tissue spread
virulence factor - toxic shock syndrome toxin 1
superantigen (exotoxin) - stimulates T-cells to over produce IL-1, IL-2 and TNF-alpha
virulence factor - enterotoxin
six types (A, B, C, D, E and G) - cause vomiting and diarrhea when ingested
virulence factors - exfoliative toxins (A and B)
esterase and protease activity - target proteins that maintain epidermal integrity
virulence factors - Panton-valentine leucocidin (PVL)
cytotoxin - causes pores in leukocytes resulting lysis
virulence factor - biofilm
community of bacterial cells attached to a surface - extracellular matrix of polysaccharide or protein protects bacteria from phagocytosis. resistant to antibiotics
transmission of S. Aureus infections
direct contact: person to person spread is common via carraige on the skin (especially the hands)
can also be picked up from contact with the environment - hospital environments are known reservoirs
classification of staphylococcal infections
skin and soft tissue
systemic - invasive
systemic - toxin mediated
skin and soft tissue infections
boils are superficial infections where you get a collection of pus - can be spontaneously draining or be encouraged by a warm moist compress. recurrent may need antibiotic treatment
folliculitis is a superficial skin infection involving hair follicles - treatment not always needed
furuncles and carbuncles are deeper infections usually preceded by folliculitis - common on hairy skin. spontaneous or surgical draining needed. patients can be systemically unwell with carbuncles
S. aureus s the most likely pathogen

systemic staphylococcus aureus infections
bloodstream infection (BSI) or bacteremia/septicemia
pyelonephritis and renal abscess
deep abscesses e.g. brain, liver
endocarditis
usually secondary to BSI
high fever, heart murmur, emboli, non specific features (pain, weight loss), Osler’s nodes
clinicians must investigate for primary focus e.g. IV line site
treatment requires prolonged IV vancomycin and gentamycin
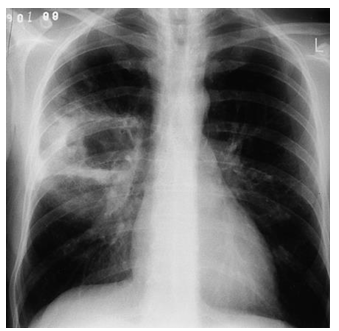
pneumonia
hematogenous - septic emboli/R side endocarditis/IV device
risk factors: viral respiratory infection (influenza or measles), cystic fibrosis, healthcare contact, aspiration
osteomyelitis
hematogenous spread or secondary to local trauma
vertebrae the most common site for hematogenous spread - long bone metaphysis in childeren
diagnosis is made by direct needle aspiration or bone scan
can be acute or chronic
pain, high fever, rigors and high WCC
treatment: IV Flucloxacillin pending C and S
septic arthritis
hot, swollen joint
knee, hip, elbow and shoulder are most common joints affected by metastatic spread i.e. from BSI± endocarditis
treatment usually with IV flucloxacillin (14 days)
toxin mediated conditions
food poisoning/gastroenteritis - short incubation period, self limiting
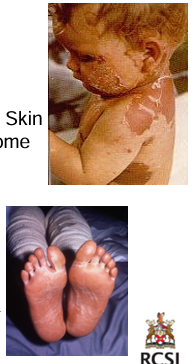
scaled skin syndrome - cleaves middles layers of skin. often occurs in outbreaks
toxic shock syndrome - multi system disease. high fever, hypotension, sunburn rash on soles and palms. vomiting diarrhea, confusion/headache. IV vancomycin plus gentamicin
antibiotics
treatment generally not required for mild soft tissue infections e.g. boil/carbuncle
flucoxacillin if susceptible and significant skin/soft tissue infection for 7-10days
longer duration if systemic infection i.e. 2 weeks for BSI if source/focus removed, 4-6 weeks for endocarditis
exam for signs of metastatic infection. ECHO, scans and repeat blood cultures after 72 hours
coagulase negative staphylococci
staphylococcus epidermis
less virulent than S. aureus i.e. less toxins
opportunistic pathogen
prolific biofilm producer
mainly associated with device related infections e.g. prosthetic joints, intravascular lines etc.
can be highly resistant to beta lactam antibiotics
staphylococcus saprophyticus
frequent cause of urinary tract infection in women of reproductive years
UTI requires empiric treatment with nitrofurantoin, trimethoprim or amoxicillin in this instance
clostridia
gram positive bacilli

clostridium spp.
all form endospores and produce powerful exotoxins
mostly strict anaerobes
ubiquitous organisms i.e. present in soil, water, sewage
C. tetani
tetanus: life threatening illness caused by a neurotoxin (tetanospasmin) resulting in tetanic paralysis
decreasing incidence sue to vaccine
treatment involve use of antibiotics (benzyl penicillin or metronidazole)
neutralization of toxin with tetanus immunoglobulin
C. botulinum
botulism: associates with contaminated food products, usually pork and canned foods with spores or from wound
Botox (toxin) results in flaccid paralysis
serious illness requiring intensive care, toxin neutralization, antibiotics and wound debridement

C. perfrinigens
causes gas gangrene
extremely serious, rapidly progressive infection
imminent risk to both limb and life
rapid destruction of muscle and severe systemic toxicity
prompt debridement of all nonviable tissue is essential
acute onset of heaviness in the area followed by severe pain, devitalization of limb, mottled skin, fluid or gas-filled blisters on the skin

clostridium difficile
bacterium that normally lives in the large intestine - common in the bowel of babies and infants but rarely causes problems
antibiotics = main risk factor for infection
disruption of normal colonic flora
at least 2 types of toxin A and B
C. difficile infection symptoms
variable (depends on the patient)
asymptomatic to potentially fatal
diarrhea, stomach cramps, nausea, fever, loss of appetite, acute abdomen colitis
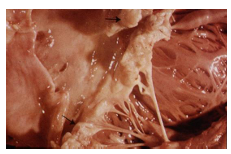
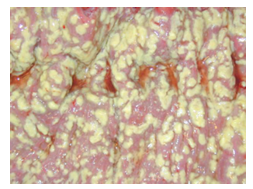
plaques of yellow fibrin and inflammatory debris adherent to reddened mucosa
types of C. difficile infection (CDI)
new
first episode of CDI
recurrent
common 8-50% cases
CDI that occurs within 8 weeks. following the onset of a previous episode
risk of recurrence increases with each recurrence - if a patient has 2+ episodes of CDI, the risk of additional recurrences increases to 50-65%
CDI treatment
isolation and contact precautions
antibiotics should be reviewed and stopped if possible. If not possible to stop, switch to agent with a lower propensity to induce C. difficile
supportive therapy (fluids etc.)
is this severe or non-severe infection?
is this new or recurrent infection?
CDI prevention and control
antibiotic stewardship
infection prevention and control
Corynebacterium diphtheriae
the organism has a worldwide distribution, humans are the only known reservoir
prior to vaccination, significant cause of nursery deaths
at risk: childeren/unvaccinated/overcrowding
reservoir: cases and asymptomatic carriers
spread is by droplet
nasal carriers may shed for weeks
reduced incidence with immunization programs - covered in diphtheria, tetanus and pertussis vaccine
Corynebacterium diphtheriae clinical features
incubation period 2-6 days
may involve any mucus membrane or skin
low grade fever
classified based on site of infection: anterior nasal, tonsillar and pharyngeal, cutaneous, ocular
treatment with benzylpenicillin or erythromycin plus antitoxin
infected person may develop bull neck

rules for antibiotic treatment of infections caused by gram positives
most commonly use cell wall active agents
penicillin
nearly all beta hemolytic streptococci susceptible
high levels of resistance in S. aureus and CoNS
cephalosporins
for penicillin resistant pneumococci
used for treatment of meningitis
used if allergy to penicillin
resistance common is listeria monocytogenes
vancomycin
if beta lactam anaphylaxis
if resistance to beta lactans suspected