Human Physiology Exam 2 Part 3
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
What are the top two leading causes of death in the U.S.?
Heart diseases and malignant neoplasms
How does blood flow in coronary circulation?
Oxygenated blood from the left ventricle enters the aorta. The coronary arteries divide into smaller capillaries that penetrate the myocardium. Deoxygenated blood from the capillaries collects in coronary veins. The coronary veins then empty into the right atrium.
What is the principle of coronary bypass surgery?
to reroute blood flow around a blocked or clogged coronary artery using a healthy blood vessel taken from another part of the body
Cardiac muscle cells contract without neural innervation is
myogenic
Pacemaker cells
set the rate of the heartbeat
The conducting system initiates
The heartbeat and helps spread the impulse rapidly throughout the heart
Some cardiac muscle cells do not function in contraction, but constitute a network known as the
conducting system
The Purkinje fibers
transmit electric signals down the atrioventricular bundle (bundle of His) to left and right bundle branches.
Sinoatrial (SA) node
Sets the pace of the heartbeat at 60-100 bpm.
Escape rhythm
when action potentials from the SA node fail to reach ventricles, AV node and Purkinje fibers can act as pacemakers
Internodal pathway from SA to atrioventricular (AV) node
Routes the direction of electrical signals so the heart contracts from apex to base. AV node delay is accomplished by slower conductional signals through nodal cells
P wave
atrial depolarization
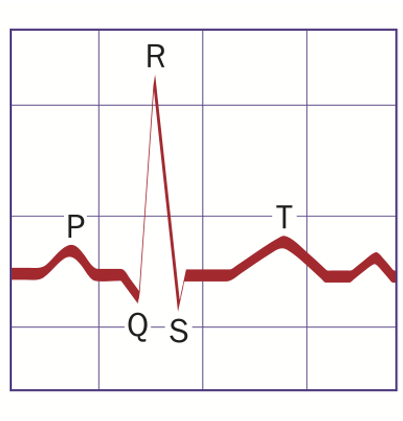
QRS complex
Ventricular depolarization. Also atrial repolarization
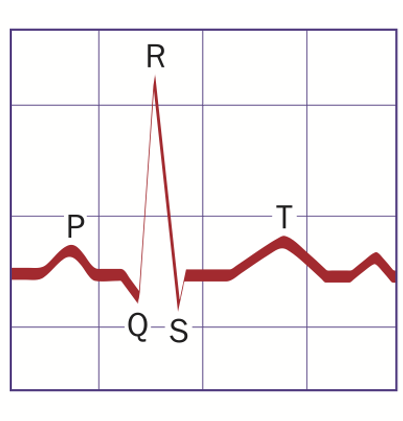
T wave
ventricular repolarization
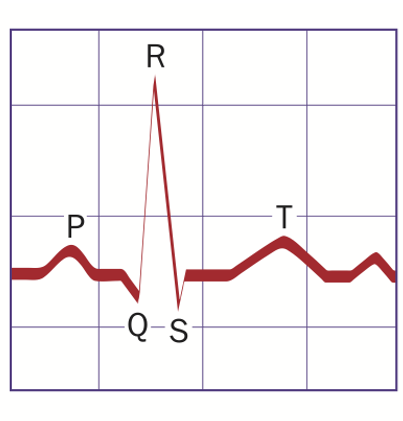
Atrial contraction begins
At the end of P wave.
Ventricular contraction begins
At the end of Q wave and continues through T wave
Atrioventricular (AV) heart block describes
a type of heart block in which the conduction between the atria and ventricles of the heart is impaired
First degree AV block is
a delay in conduction of the atrial impulse, resulting in an increased PR interval of greater than 200 msec
Second degree AV block has two types
Type I second degree AV block involves progressive PR lengthening until the QRS “drops out,” indicating the previous P wave was not conducted to the ventricles. This is typically a nodal block.
Type II second degree AV block occurs in the setting of a constant PR interval with sudden nonconduction of a P wave. It may present as a single nonconducted P wave or a repetitive pattern of nonconduction. This block is commonly infranodal with a wider QRS complex.
Third degree AV block occurs
when P waves are not conducted to the ventricles and a slow escape rhythm is present. The atrial and ventricular impulses are not synchronized, and the atrial rate is faster than the independent ventricular rate.
Systole is
The period of ventricular contraction and blood ejection
Diastole
the period of ventricular relaxation and blood filling
Isovolumetric ventricular contraction
the ventricles are contracting but all valves in the heart are closed, and so no blood can be ejected.
Isovolumetric ventricular relaxation
the ventricles begin to relax, no blood is entering or leaving the ventricles meaning all the valves are closed
The cardiac cycle has four phases
isovolumetric relaxation, ventricular filling, isovolumetric contraction, and ejection
Ejection
The second part of systole is blood moving out of the ventricles.
Blood filling
The second part of diastole is blood moving into the ventricles
“Lub” heart sound
closure of the AV valves at the onset of systole and isovolumetric ventricular contraction
“Dup” heart sound
closure of the pulmonary and aortic valves at the onset of diastole and isovolumetric ventricular relaxation.
Valve does not open fully
Stenosis
Valve doesn't close tightly
Regurgitation
Cardiac output (CO)
The heart is the pump that moves the blood. In reference to the amount of blood moved per unit of time. Cardiac Output = Heart Rate x Stroke Volume
Cardiac cycle is 1/3
systole
Cardiac cycle is 2/3
diastole
Cardiac output is regulated by
Heart rate via sympathetic or parasympathetic nerve and hormone in blood (epinephrine). Also by stroke volume via venous return and ventricular contractility (by nerve and epinephrine)
The sympathetic nerves
innervate the entire heart and releases norepinephrine
Parasympathetic nerves
innervates node cells only and releases primarily acetylcholine
Both norepinephrine/epinephrine and acetylcholine receptors in the heart are GPCRs but have __________ effects
opposite
Pacemaker potential is caused by
hyperpolarization activated cyclic nucleotide gated (HCN) channels
cAMP activates _____ channels
HCN
Why can caffeine increase heart rate?
Caffeine promotes the accumulation of cAMP. The more cAMP, the higher probability that HCN channel will be open, the stronger pacemaker potential, the faster heart rate.
How does epinephrine/norepinephrine increase heart rate? Molecules involved?
WATCH VIDEO
How does acetylcholine decrease heart rate? Molecules involved
The binding of ACh to mAChR triggers the dissociation of Gα-GTP from Gßγ, which directly binds to and opens a K+ channel
What is the Frank-Starling mechanism?
the stroke volume (SV) of the heart increases in response to an increase in the volume of blood filling the heart (the end diastolic volume, or EDV) when all other factors remain constant