NURS 2001 Midterm Exam
1/45
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
46 Terms
identify the role of a professional nurse in a health assessment, and in regards to health promotion, and disease prevention
-Nursing is the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response
-to promote optimal health, a health care delivery system must provide medical care, but also use disease prevention and health promotion strategies. (understand risk factors and interventions for risk factors-primary, secondary, and tertiary prevention, and health care services/places to go for care)
What role does the nurse play in the health assessment?
They play a crucial role. They gather comprehensive data about the patient through observation, interviews, and physical examinations. This includes taking vital signs, assessing physical and mental health, and identifying any potential health issues. Nurses also document findings, develop care plans, and collaborate with others to ensure patient receives effective and holistic care. Their assessments are essential for creating a complete picture of the patient’s health, which further guides medical treatment and care.
Identify the roles of the nursing process and know how to apply them to different situations.
Assessment - ADOPIE
• Initial Assessment happens first: Establish a
baseline for your patient:
o Review health history
o Conduct a physical assessment
o Manage data according to the Functional
Health Patterns
Types of assessments :Emergency, urgent, comprehensive, and focused
Subjective: The nurse interviews John and learns that he has been experiencing chest pain for the past two days, which worsens with exertion. He describes the pain as tight, squeezing sensation. He also reports shortness of breath, especially when climbing stairs.
Objective: The nurse takes John’s vital signs and finds high blood pressure 160/90, his heart rate is high at 110 beats per minute, and his respiratory rate is 24 breaths per minute. John appears anxious and is using accessory muscles to breathe.
Diagnosis-ADOPIE
• The nursing diagnosis statement:
o Analyze and synthesize assessment data and prioritize. Diagnosis statement has three parts.
NANDA label- the priority problem
The stimulus or etiology of problem (R/T- related to)
Defining characteristics- signs and symptoms,
ineffective behaviors (E/B- evidenced by)
-Based on the assessment data, the nurse identifies potential nursing diagnoses such as ineffective breathing pattern related to respiratory distress and acute pain related to chest discomfort.
3 Types-Problem-focused, 2. risk diagnosis, 3. health promotion diagnosis
Outcome identification- ADOPIE
• Measurable, realistic, patient-centered
goals
-Goals must be Specific, Measurable, Attainable, Relevant, Timely (SMART)
John: “in the next 3 months I will try to quit smoking and exercise more”
Planning Care- ADoPIE
• Determine resources
• Target nursing interventions
o Any treatment based on clinical judgment and
knowledge that a nurse performs to enhance patient outcomes
• Individualized patient care plan
• RN documents on individualized nursing care plan
The nurse sets goals for client’s care, such as “Patient will report a decrease in chest pain within 30 minutes of intervention” and “Patients will demonstrate effective breathing patterns by the end of the shift”.
Implementation -ADOPIE
• Intervention= any treatment based on
clinical judgment and knowledge that a
nurse performs to enhance patient
outcomes
• Nurse driven
• Document at the point of care
-The nurse administers prescribed medications, such as nitroglycerin for chest pain and oxygen therapy to improve breathing. The nurse also provides John with education on relaxation techniques to help manage anxiety.
Evaluate Outcome- ADOPIE
• Judgment of the effectiveness of nursing
care in meeting the goals and outcomes
• Assess the promotion of and barriers to
goal attainment
• May be met, partially met, not met
The nurse evaluates the effectiveness of the interventions by reassessing John’s pain level and breathing pattern. If it is not successful, the nurse may need to adjust care plans and try different interventions.
Recognize sensitive and/or special modes of communication.
cultural sensitivity
Language barriers
hearing impairements
speech and cognitvie impairments
emotional sensitivity
non-verbal communication
confidentiality
Identify the components of an emergency, focused, and comprehensive health history.
Emergency health history
-Chief complaint:
-allergies
-Medications
-past medical history
-last meal
-events leading up to the emergency
Focused health history-specific health related issue usually
-Chief complaint
-history of present illness
-relevant past medical history
-medications
-allergies
-review of systems
Comprehensive health history-mainly used for a checkup
-identifying data
-source of history
-chief compliant
-history of present illness
-past medical history
-family history
-social history
-Review of systems
Gather a complete health history
-opening (greet, purpose, ensure confidentiality, set expectations, assess comfort, invite questions)
Chief complaint: What brings you here? What concerns you? (signs and symptoms)
History of present illness: What lead up to this? (gather specifics, COLDERRST)
Past medical history: Medical conditons, surgeries, hospitalizations (include dates, providers, and outcomes), chronic illness, significant medical event/diagnosis
Allergies: Medications, seasonal, animals, foods, materials, (include reactions, severity and interventions to alleviate)
Medications and supplements: current (prescriptions, over-the-counter, supplements, vitamins)-document name, dose, frequency and reason
Family history: childhood illness, health status of 1st and 2nd degree relatives (cause of death, age of death <55 men; <65 in women
-functional health patterns
• Psychosocial data
o Perceived cognitive abilities
o Attitudes and responses to care
o Mental and emotional status
o Neglect, abuse and violence
o Sexual health
o Cultural implications
-include dates whenever possible
Additional screening
-CAGE questionnaire
C-CUT
A-ANNOYED
G-GUILTY
E-EYE-opener
-cigarette use Pack years = # of daily cigarettes x years of smoking/20)
Perform a complete Review of Systems (ROS). What patient data is placed in the ROS vs Health History?
Review of systems ROS
• General/Constitutional
• Skin, hair, nails
• Head
• Eyes
• Ears
• Nose & sinuses
• Mouth
• Neck & nodes
• Respiratory
• Cardiovascular
• Gastrointestinal
• Musculoskeletal
• Neurological
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/immunologic
ROS cont...
What is clinical judgement in nursing? How do nurses use clinical judgement?
Process by which nurses assess patient situations, make decisions regarding care, and determine the best course of action based on their knowledge, experience, and the information available. It involves critical thinking, problem-solving, and the application of clinical knowledge to provide safe and effective patient care. Nurses use clinical judgement in ADOPIE
Understand the basics of documentation practices. What is the significance? Different methods? The ethical and legal considerations?
Significance
Communication
Legal Record
Quality Assurance
Billing and Reimbursement
Different Methods
Paper records
Electronic health records
SOAP Notes: Method of documentation that includes subjective, objective, assessment, and plan sections.
Narrative Notes: Free-form documentation that allows nurses to describe patient conditions and care in detail.
Ethical and legal considerations
Confidentiality
accuracy
timeliness
professionalism
Describe purpose and process of general survey and collecting vital signs
The general survey is an overall review or first impression that a healthcare provider has of a patient’s well-being. It includes
Appearance
behavior
body structure
mobility
The purpose of obtaining vital signs are to establish baseline, monitor for changes in health status, identify risks, identify health problems, and evaluate treatment.
Process of collecting vital signs
Temperature: Balance of heat produced by the body and heat lost to the environment. You can measure the body temperature using a thermometer, which can be done orally, rectally, axillary, or tympanically. Normal Ranges: 96.8-100.4 average is 98.6.
Pulse: Rhythmic beating of the arteries in response to the ejection of blood from the left ventricle. Normal ranges are 60-100 bpm. Count the pulse rate for 30 seconds and multiply by two. If the heart rate is irregular, count for a full minute
Blood pressure: force blood exerts on the interior walls of the blood vessels Anything over 120/80 is high and anything under 90/60 is low.
Respiratory rate: Breaths someone takes for an amount of time. Count breaths for 30 seconds. If the breaths are irregular, count for one minute. Normal rates are 12-20 breaths per minute
Oxygen Saturation: Hemoglobin that is saturated with oxygen.
pain-COLDERRST
The purpose of vital signs, normal ranges, and expected findings
Patient data: give examples of subjective and objective, primary and secondary data sources
Subjective Data: Information reported by the patient which cannot be measured directly. “I have a headache” “I feel anxious about my surgery” “I’ve been feeling very tired lately”
Objective Data: This is measurable and observable information obtained through physical examination, diagnostic tests, or medical records. Examples include:
-Blood pressure reading of 120/80 mmHg.
-Temperature of 100.4 F
-A rash observed on a patient’s arm.
Primary data sources: These are original sources of information directly from the patient or the patient’s records. Examples include:
-patient interviews or self-reported symptoms
-direct observations during a physical examination
-results from diagnostic tests performed on the patient
Secondary data sources: These are sources that provide information about the patient but are not directly from the patient. Examples include:
-Medical history from previous healthcare providers.
-Family medical history documented in the patient records
-research articles or clinical guidelines relevant to the patient’s condition
Assess and develop a plan of care addressing hygiene practices and self-care behaviors
Plan of care
Set goals: establish realistic and achievable goals for improving hygiene and self-care. For example, “The patient will bathe independently at least three times a week”
Educate: Provide education on the importance of hygiene and self-care for overall health. Teach proper techniques for bathing, oral care, and grooming.
Provide Resources: Offer resources such as assistive devices (eg. shower chairs, grab bars) or referrals to occupational therapy if needed.
Develop a routine: Help the patient develop a daily routine that includes time for hygiene and self-care activities
Monitor and Evaluate: Regularly monitor the patient’s progress and adjust the plan as needed. Provide encouragement and support to help them achieve their goals.
Pain: The categories, sources, and origin of pain. Pain scale, COLDERRST, different pain assessments tools
categories of pain
Acute pain: Short-term pain that typically follows an injury or surgery and resolves as the body heals
Chronic Pain: Long-term pain that persists for months or years, often without a clear cause
Neuropathic pain-Pain caused by damage to the nerves, often described as burning or shooting
Nociceptive Pain-Pain from physical damage or potential damage to the body, such as a cut or a broken bone.
Visceral pain-Pain from the internal organs, often described as deep, squeezing, or aching.
Sources of pain
Somatic Pain: originates from the skin, muscles, and soft tissues. It is usually well localized.
Visceral pain: Originates from internal organs. It is often more diffuse and harder to pinpoint.
Neuropathic pain: Originates from the nervous system and often involves a burning or tingling sensation
Origin of pain
Cutaneous pain: From the skin or subcutaneous tissue
Deep somatic pain: From ligaments, tendons, bones, blood, vessels, and nerves
Visceral pain: From internal organs
Pain scale: A common tool used to assess pain intensity is the numeric pain rating scale where patients rate their pain from 0 to ten.
COLDERRST
Character: What does the pain feel like?Onset: When did the pain start?
Location: Where is the pain located?
Duration: How long does the pain last? Does it come and go?
Exacerbation: What makes the pain worse?
Relief: What makes the pain better?
Radiation: Does the pain spread to other areas?
Severity: How severe is the pain?
Timing: Is the pain constant or intermittent.
Different pain assessment tools
Visual Analog Scale: A line marked from no pain to worst pain where patients mark their pain level
WONG-Baker FACES Pain Rating Scale; Uses facial expressions to help children or those with communication difficulties rate their pain.
CRIES-For infants uses a score of 0-2 in five categories to determine changes from baseline indicating pain. The five factors are:
-Crying
-Increase in oxygen Requirement from baseline
-increase in vital signs from baseline
-expression on face
-sleeping
In infants to children 2-7 years of age, the FLACC scale is used
-Facial expression
-Leg movement
-activity
-crying
-consolibility
Pharmacologic vs. non-pharmacologic pain interventions
Pharmacologic pain interventions
Medications
Non-pharmacologic
Physical therapies
psychological approaches
complementary therapies
education and support
age considerations of pain across the lifespan
-Children and infants may not be able to express their pain as well as adults
Adolescents: May report their pain but might underreport due to fear of treatment or peer pressure
Adults: Adults may be able to communicate their pain clearly but may have varying pain thresholds and coping mechanisms.
Older adults: May underreport pain due to beliefs about aging, fear of medication, side effects, or cognitive impairments.
Describe the relationship of health assessment to health promotion
-health assessments provide the necessary information to tailor health promotion strategies to the individual’s specific needs.
-continuous health assessments can monitor the effectiveness of health promotion actives, allowing for more adjustments and improvements over time.
Explain the infection cycle.
Germs (agent)
-Pathogen that causes infection, like bacteria, viruses, or parasites
Where germs live (Reservoir)
-this is where the infectious agent lives and multiples. This includes humans, animals, and environment like food, soil, and water.
How germs get out (Portal of Exit)
-The way the agent leaves the reservoir. This can be through mouth, cuts on the skin, or stool
Germs get around (Mode of Transmission)
-This describes how the infection spreads from one host to another. It can happen through contact or droplets.
How germs get in (portal of entry)
-this is how agent enters a new host. It can happen through mouth, cuts in the skin, and eyes.
Next sick person (susceptible host)
-the infection needs a susceptible host to thrive. It can happen to babies, children, elderly, people with a weakened immune system, unimmunized people, or really anyone.
List the stages of an infection.
-Incubation period
-prodromal period
-period of illness
-period of decline
-period of convalescence
Use correct techniques for safety and infection control.
Hand hygienist
Personal Protective Equipment (PPE)
Sterile technique
environmental cleaning
safe injection practices
isolation precautions
vaccinations
describe the strategies for implementing standard and transmission-based precautions
• Standard precautions—used in care of all hospitalized patients
Hand hygiene
Use of PPE
Safe injection practices
respiratory hygiene/cough etiquette
environmental cleaning
safe handling of potentially contaminated equipment
• Transmission-based precautions—used in addition to standard precautions for patients with suspected infection
Special Contact precautions: Use gloves and gowns when entering the room of a patient with a known or suspected infection that can be spread by direct or indirect contact. Ensure proper disposal of PPE. Microorganisms: Clostridium difficile
-private room, gowns and gloves, wash hands with soap and water NO HAND SANITIZER
Droplet: Wear a surgical mask when within 3 feet of a patient with a known or suspected infection spread by large respiratory droplets. Patients should wear masks during transport. Micro-organisms: Strep, pneumonia, hib, scarlet fever, rubella.
-private room, mask
Airborne precautions: Use a fit-tested N95 respirator or higher-level respiratory protection when entering the room of a patient with a known or suspected airborne infection. Ensure the patient is in an airborne infection isolation room with proper ventilation. Micro-organisms: Measles, varicella, pulmonary or laryngeal tuberculosis.
-private room, N95, HEPA respirator, negative pressure airflow exchange
identify factors that affect safety in an individual’s environment
Regular
Physical environment
Social environment
health status
age
knowledge and awareness
technology and equipment
Nursing
Physical environment
infection control
medication safety
patient mobility
health status
communication
education and training
Identify patients at risk for injury. Review the Morse Fall Scale and identify what puts a patient at risk.
• Age >65
• History of falls
• Impaired vision or balance
• Altered gait or posture, impaired mobility
• Medication regimen
• Orthostatic (Postural) hypotension
• Slowed reaction time; weakness, frailty
• Confusion or disorientation
• Unfamiliar environment
Nurses must evaluate ALL patients for Fall Risk
History of falling: This is scored as 25 if the patient has fallen during the present hospital admission or if there was an immediate history of physiological falls, such as from seizures or an impaired gait prior to admission. If the patient has not fallen, this is scored 0. Note: If a patient falls for the first time, then his or her score immediately increases by 25.
Secondary diagnosis: This is scored as 15 if more than one medical diagnosis is listed on the patient’s
chart; if not, score 0.
Ambulatory aids: This is scored as 0 if the patient walks without a walking aid (even if assisted by a nurse), uses a wheelchair, or is on a bed rest and does not get out of bed at all. If the patient uses crutches, a cane, or a walker, this item scores 15; if the patient ambulates clutching onto the furniture for support, score this item 30.
Intravenous therapy: This is scored as 20 if the patient has an intravenous apparatus or a heparin lock inserted; if not, score 0
Describe specific safety risk factors for each development stage
Neonate and Infants
• Avoid behaviors that might harm the fetus.
o Shaken baby, ABC of Safe Sleep, secondhand smoke
• Never leave the infant unattended.
• No honey until age 1-year
• Swimming pools
• Use crib rails
o ≤6cm
o No items in crib or over crib
• Monitor setting for objects that are choking hazards.
• Use car seats properly
o 5 point restraint seat belt, rear-facing
Toddler/preschool
• Childproof home environment.
o Gates, firearms
• Prevent poisoning.
• Be alert to manifestations of child abuse.
• Safety equipment
o Life jackets
• Use car seats properly.
• Burns
o Water, stovetop, sun
School-Aged Child
• Help to avoid activities that are potentially dangerous.
• Provide interventions for safety at home, school, and neighborhood.
• Teach bicycle safety.
• Teach about child abduction.
• Wear seatbelts.
Adolescents
• Teach safe driving skills.
o Texting, distraction
• Teach avoidance of tobacco and alcohol.
• Swimming and check water depth
• Teach risk of infection
o STIs, piercings
• Safe sex
• Teach about guns and violence.
• Mental health
o Social media
• Burns
o Sunbathing, tanning beds
Adults
• Remind them of effects of stress on lifestyle and health.
• Counsel about unsafe health habits (reliance on drugs and alcohol).
• Counsel about domestic violence.
• MVAs are the most common cause of death and injury to adults
• Home safety
o CO & fire detectors
• Proactive about occupational hazards
Older Adults
• Prevent accidents.
• Orient person to surroundings (avoid falls).
• Maintain vehicle in working order, schedule eye exams, and keep noise at a minimum.
• Promote safe environment at home (avoid fires).
• Use medication trays (avoid poisoning).
Describe nursing interventions to prevent injury to patients in healthcare settings
Fall prevention
-Assess patients for fall risk
-Ensure that call bells, personal items, ad mobility aids are within reach
-Use non-slip footwear and keep the environment free of clutter.
Proper use of Restraints
-use of restraints only as a last resort and follow the facility’s protocol.
-regularly monitor and assess the patient’s condition when restraints are in use
-provide alternative measures to restraints, such as increased supervision or environmental modifications.
Safe medication administration
-follow the “five rights” of medication administration: right patient, right drug, right dose, right route, and right time.
-double-check medications and dosages, especially high-risk drugs.
-educate patients about their medications, including potential side effects
preventing infections
-practice proper hand hygiene before and after patient contact
-Use aseptic techniques during procedures and dressing changes
-ensure that patients receive appropriate vaccinations and educate them about infection prevention
Pressure ulcer prevention
-Regularly assess the patient’s skin, especially over bony prominences.
-Reposition the patient at least every two hours to relieve pressure
-use pressure-relieving devices such as special mattresses or cushions
Safe patient handling
-use proper body mechanics and lifting techniques to prevent injury to both patients and staff.
-utilize mechanical lifts and transfer devices when necessary
-educate patients and families on safe mobility techniques
Environment Safety
-ensure the patient’s environment is free from hazards, such as spills or loose cords.
-maintain proper lighting and ensure that pathways are clear.
-educate patients about the importance of using assistive devices correctly.
Priority setting frameworks: apply ABC’s, maslow’s, acute vs. chronic
Maslow’s Hierarchy of Needs
Self Actualization: Desire to become the most that one can be
Esteem: Respect, self-esteem, status, recognition, strength, freedom
Love and belonging: Friendship, intimacy, family, sense of community
Safety needs: Personal security, employment, resources, health, property
Physiological needs: Air, water, food, shelter, sleep, clothing, reproduction
ABC’s
Airway
Breathing
Circulation
Acute vs Chronic
-in priority setting, acute conditions usually take precedence over the chronic conditions as they can be life threatening and require immediate attention.
Differentiate between the different types of assessments (emergency, urgent) and a comprehensive exam vs. focused exam
Emergency Assessment: This is conducted in life-threatening situations where immediate action is required.
Urgent Assessment: This is less immediate than an emergency assessment but still requires prompt attention. It is used when a patient’s condition is serious but not immediately life-threatening.
Comprehensive Exam: This is a thorough and complete assessment of a patient’s overall health. (More for a check-up)
Focused Exam: More targeted assessment that concentrates on a specific area of concern.
Describe the principles of respiratory physiology
Ventilation: During inhalation, the diaphragm and intercostal muscles contract, expanding the thoracic cavity. In exhalation, these muscles relax and the elastic recoil of the lungs pushes air out.
Gas exchange: Occurs in the alveoli, tiny air sacs in the lungs. Oxygen from the inhaled air diffuses across the alveolar membrane into the bloodstream, while carbon dioxide from the blood diffuses into the alveoli to be exhaled. This is driven by the differences in partial pressures of gases (Dalton’s Law).
Transport of gases: Once oxygen is the bloodstream, it binds to hemoglobin in red blood cells for transport to tissues. Carbon dioxide is transported back to the lungs in three forms: Dissolved in plasma, as bicarbonate ions, and bound to hemoglobin
Regulation of breathing: The respiratory rate and depth are regulated by the brain, specifically the medulla oblongata and pons, which responds to changes in carbon dioxide, oxygen, and pH levels in the blood. Chemoreceptors monitor these levels.
Compliance and Resistance: Lung compliance refers to the elasticity of the lung tissue and how easily it can expand. Resistance refers to the opposition of airflow in the airways. Factors like airway diameter and lung volume affect both compliance and resistance, impacting ventilation efficiency.
Describe the function and role of the cardiovascular system and the transport of respiratory gases.
transport of oxygen
Transport of carbon dioxide
regulation of blood flow
homeostasis
integration with other systems
Describe age-related differences that influence the care of patients with respiratory problems
• Compared with adults, infants and children
have higher respiratory rates, higher pulse
rates, and lower blood pressure readings.
identify factors that influence respiratory function
age
health status
environmental factors
physical activity
position of body
smoking
obesity
develop nursing diagnoses that correctly identify respiratory problems that may be treated by independent nursing interventions
Impaired gas exchange
-monitor vital signs and oxygen saturation levels regularly
-administer supplemental oxygen as prescribed
-position the patient in a high fowler’s position to enhance lung expansion
-encourage deep breathing exercises and use of incentive spirometry.
Ineffective airway clearence
-asses lung sounds and monitor for the presence of wheezing or crackles.
-encourage the patient to cough effectively and provide techniques for huff coughing.
-administer prescribed bronchodilators
-encourage adequate hydration]
activity tolerance
-assess the patient’s level of fatigue and tolerance to activity.
-plan activités with rest periods to prevent overexertion
Risk for aspiration
-assess swallowing ability and provide appropriate dietary modifications
-position the patient upright during meals and for at least 30 minutes afterward.
-monitor for signs of aspiration, such as coughing or choking during eating.
-educate the patient on safe swallowing techniques.
ineffective breathing pattern
-Monitor respiratory rate, depth, and effort.-provide a calm environment and use relaxation techniques to reduce anxiety.
-teach the patient controlled breathing techniques (Pursed-lip breathing)
-administer prescribed medications for pain management to improve comfort.
Describe strategies to promote adequate respiratory functioning
encourage deep breathing exercises
Maintain optimal position (High-semi fowler’s)
Promote hydration
Use incentive spirometry
Implement airway clearance techniques
avoid environmental irritants
encourage regular physical activity
educate on smoking cessation
monitor respiratory status
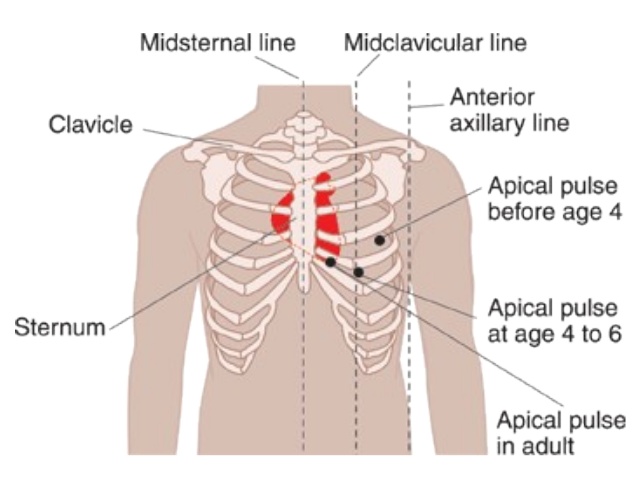
identify common landmarks on the thorax: retraction locations, apical pulse, sternal notch
Retraction Locations: These are areas where the skin pulls inward during breathing, indicating potential respiratory distress. Common retraction areas are the supraclavicular area, intercostal spaces, and subcostal area.
Apical pulse: The apical pulse is typically located at the fifth intercostal space in the midclavicular line on the left side of the chest. This is where you can hear the heartbeat most clearly using a stethescope
Sternal Notch: Visible dip at the top of the sternum between the collarbones. It serves as an important reference point for locating other structures in the thorax.
identify the structures and functions of the cardiac system, upper and lower airways
Cardiac system Structures:
Heart: Composed of four chambers and valves
Blood vessels: Includes arteries, veins, and capillaries.
Functions:
Pumping Blood: The heart pumps oxygenated blood to the body and deoxygenated blood to the body and deoxygenated blood to the lungs for oxygenation.
Circulation: It maintains blood circulation, ensuring that tissues receive adequate oxygen and nutrients while removing waste products.
Upper airways:
Structures
-Nasal cavity: Filters, warms, and humidifies air
-pharynx: a passageway for air and food, divided into the nasopharynx, oropharynx, and laryngopharynx.
-larynx: contains vocal cords and is responsible for sound production
Functions
-air passage: The upper airways serve as a conduit for air to enter the lungs
-Protection: They trap particles and pathogens to prevent them from reaching the lower airways.
Lower airways:
Structures:
-Trachea: The windpipe that connects the larynx to the bronchi
-Bronchi: Two main branches that lead into each lung, further dividing into smaller bronchi and bronchioles
-alveoli: Tiny air sacs where gas exchange occurs.
Functions:
-Gas exchange: the lower airways facilitate the exchange of oxygen and carbon dioxide in the alveoli.
-Air distribution: They distribute air throughout the lungs for efficient respiration.
Differentitate subjective data and objective data identifying expected and unexpected findings
Expected findings for subjective data-A patient might report feeling anxious, experiencing pain rated at 7 out of 10, or stating they have a history of asthma.
Unexpected findings for subjective data: A patient is reporting sudden, severe headache that is different from their usual headaches or stating they feel unusually fatigues without a clear explanation.
Expected finding for objective data: Normal blood pressure readings with normal heart rate.
Unexpected findings for objective data: Abnormal lab results or heart rhythms detected on the ECG.
individualize respiratory and cardiac health assessment considering the condition, age, gender, and culture of patient
Condition: Assessments should be tailored based on existing health conditions.
Age: Pediatric patients may present differently than adults
Gender: Can influence the presentation of certain conditions.
Culture: Can affect health beliefs and practices.
oxygen therapy devices and when they are expected to be utilized
Nasal cannula: This device consists of a lightweight tube with two prongs that fit into the nostrils. It is commonly used for patients who need low to moderate levels of supplemental oxygen.
Expected utilization: Often used in patients with COPD or during recovery from surgery to maintain oxygen levels.
Simple face mask: This mask covers the nose and mouth and delivers oxygen at higher concentrations than a nasal cannula.
Expected utilization: Used when higher concentrations of oxygen are needed, such as in patients with acute respiratory distress or during medical emergencies
Oxymask: It can deliver varying concentrations of oxygen and can be used for mild respiratory distress or more severe cases.
Non-rebreather mask: This mask has a reservoir bag and one-way valves to provide high concentrations of oxygen.
Expected utilization: Used in critical situations where the patient needs a high concentration of oxygen, such a severe hypoxia or trauma.
CPAP: This device provides a continuous stream of pressurized air to keep the airways open
Expected utilization: Commonly used in patients with obstructive sleep apnea or in certain cases of respiratory failure.
BiPAP: Provides two levels of pressure- higher during inhalation and lower during exhalation.
Expected utilizationL Used in patients with more severe respiratory conditions, such as COPD or heart failure.
mechanical ventilator: A machine that provides controlled breaths to patients who cannot breathe adequately on their own.
Expected utilization: Used in intensive care settings for patients with severe respiratory failure or during major surgeries.
describe age related differences that influence the care of patients with cardiac problems
Physiological changes
Comorbidities
Medication sensitivity
Cognitive function
Physical activity
Psychological factors
identify factors that influence cardiac function
Heart rate
contractility
preload
afterload
oxygen demand
electrolyte balance
hormonal influence
age and gender
develop nursing diagnoses that correctly identify cardiac problems that may be treated by independent nursing interventions
ineffective tissue perfusion
Activity inter tolerance
anxiety
knowledge deficit
risk for decreased cardiac output
fluid volume excess
altered heart rate
Describe strategies to promote adequate cardiac functioning
Regular exercise
Healthy diet
weight management
stress management
avoiding tobacco and limiting alcohol
regular health check-ups
medication adherence
hydration
assess for risk factors for cardiac disease
age
family history
smoking
high blood pressure
high cholesterol levels
diabetes
obesity
physical inactivity
unhealthy diet
stress
How are pulses assessed?
Select pulse points
positioning
use of fingers
count the pulse
assess rhythm
evaluate quality
record findings
s/s and interventions for vascular emergencies
Immediate medical attention: Call emergency services for any suspected vascular emergency.
Positioning: Keep the affected limb elevated to reduce swelling in cases like DVT.
Oxygen Therapy: Administer oxygen if the patient shows sings of respiratory distress.
Anticoagulation Therapy: For DVT or pulmonary embolism, anticoagulants may be adminstered to prevent further clotting.
Surgical intervention: In cases like acute limb ischemia or aortic dissection, surgical procedures may be necessary to restore blood flow or repair the affected vessel.
Monitoring vital signs: Continuously monitor blood pressure, heart rate, and oxygen saturation.
Pain management: Administer analgesics as needed to pain management.
Take what you know about the breast assessment and apply it to health promotion of breast health.
Regular self-exams: encourage individuals to perform monthly breast self-exams to familiarize themselves with their breast tissue. This helps in recognizing any changes such as lumps, swelling, or changes in shape or texture.
Clinical breast exams: Recommend regular clinical breast exams by healthcare professionals, typically every 1-3 years for women aged 20-39 and annually for those 40 and older.
Mammography screening: promote mammography as a vital screening tool for early detection of breast cancer. Women should start having mammograms at age 40, or earlier if they have a family history of breast cancer.
Awareness of risk factors : Educate about risk factors for breast cancer, including age, family history, genetic factors, and lifestyle choices such as diet, exercise, and alcohol consumption.
Healthy lifestyle choices: Encourage a balanced diet, regular physical activity, and maintaining a health weight to reduce breast cancer risk
Limit alchohol intake: advise limiting alcohol consumption, as higher intake is associated with an increased risk of breast cancer.
Tobacco cessation: Promote quitting smoking, as tobacco use is linked to various health issues, including breast cancer.
Genetic Counseling: For individuals with a strong family history of breast cancer, recommend genetic counseling and testing for BRCA mutations.
Support groups and resources: Provide information about support groups and resources for those diagnosed with breast cancer or at high risk.