Physl 212 Cardiovascular
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
MAP = TPR x CO
- MAP = mean arterial pressure
- CO = cardiac output
- TPR = total peripheral resistance, determined by total arteriolar resistance
CO = HR x SV
CO-Cardiac output, amount of blood pumped by each ventricle in one minute
HR-Heart rate
SV-Stroke volume, amount of blood pumped out of each ventricle during systole
SV = EDV - ESV
End-diastolic volume (EDV) -amount of blood in each ventricle at the end of ventricular diastole
End-systolic volume (ESV) -amount of blood in each ventricle at the end of ventricular systole
Stroke volume -volume of blood pumped out of each ventricle during systole, ~70 - 75 mL
Poiseuille's equation
R = resistance to blood flow
η = viscosity of blood
l = length of vessel
r = radius of vessel (raised to fourth power)
Applies to laminar blood flow
F = ∆P/R
we have to maintain F, If R decreases as we go from large artery to many arterioles and F is constant
ΔP must decrease
F = flow
∆P = pressure difference between two fixed points
R = resistance to flow
Compliance = ∆Volume/ ∆Pressure
∆P that occurs with ∆V is greater if the compliance of the vessel is lower
Pulse pressure = systolic pressure - diastolic pressure
Diastolic pressure-minimum blood pressure at end of ventricular diastole
Systolic pressure-maximum blood pressure during ventricular systole
Ejection Fraction (EF) = SV/EDV
Stroke volume-volume of blood pumped out of each ventricle during systole
End-diastolic volume (EDV)-amount of blood in each ventricle at the end of ventricular diastole
What is hemodynamics?
Pressure gradient (not absolute pressure) creates blood flow
contraction of heart chambers
blood on the walls of the blood vessels and heart chambers
Flow and resistance to flow can affect pressure
What factors determine the resistance to blood flow?
Viscosity
friction between molecules of a flowing fluid
Length and diameter
determines amount of contact between moving blood and stationary wall of vessel
transitional and turbulent flow
How do the factors affect the resistance to blood flow (Poiseuille's equation)?
R = resistance to blood flow
η = viscosity of blood
l = length of vessel
r = radius of vessel (raised to fourth power)
Applies to laminar blood flow
What are the functions of the cardiovascular system?
To deliver oxygen and nutrients and remove waste products of metabolism
Fast chemical signaling to cells by circulating hormones or neurotransmitters
Thermoregulation
Mediation of inflammatory and host defense responses against invading microorganisms
Describe the path of blood flow in the body and through the pulmonary and systemic circuits.
Pulmonary circulation
-Blood to and from the gas exchange surfaces of the lung
-Blood entering lungs
-poorly oxygenated blood
-Blood leaving lungs
-oxygenated blood
Systemic circulation
-Blood to and from the rest of the body
-Blood entering tissues
-oxygenated blood
-Blood leaving tissues
-poorly oxygenated blood
What is serial versus parallel blood flow?
Series flow
-Blood must pass through the pulmonary and systemic circuits in sequence
Parallel flow
-Each organ supplied by different artery
-Independently regulate flow to different organs
Exception
-digestive organs and liver are in series
List the layers of the pericardium. What are the functions of the layers?
fibrous sac surrounding the heart and roots of great vessels
(1) Fibrous pericardium - Serous pericardium
(2) Parietal
(3) Visceral
Pericardial cavity
- Pericardial fluid decreases friction
-Stabilize heart in its cavity
-Protection from mechanical traumas and infection
-Limits overfilling of chambers
-Prevents distension
List the layers of the heart wall. Describe the structure and function of each.
Epicardium (visceral pericardium)
- Covers outer surface of heart
protecting the heart, producing factors that help the cardiac cells properly develop, and ensuring proper response to cardiac cell injury.
Myocardium
-Muscular wall
-Cardiac muscle cells (myocytes), blood vessels, nerves
-responsible for the contractile function of the cardiac pump.
Endocardium
-Endothelium covering inner surfaces of heart and heart valves
-barrier between cardiac muscles and the bloodstream and contains necessary blood vessels
Why is the wall of the left ventricle thicker than the right ventricle?
The left ventricle has to endure more pressure than the right ventricle
• What is the structure of a myocyte?
Branched ("Y") and joined longitudinally
Striated, one nucleus per cell, many mitochondria
What are intercalated disks?
Dense bands containing intercellular junctions that link adjacent cells mechanically and electrically
What specialized junctions are found at intercalated disks? What are their functions?
Desmosomes
-Anchor cells together in tissues subject to considerable stretching
-Mechanically couple cells
Gap junctions
-Communicating junctions
-Transmembrane channels linking adjacent cells
-Electrically couple heart cells
• Name the four valves of the heart. What is the function and structure of each?
AV valves
-Between atria and ventricles
-prevent backflow of blood into atria when ventricles contract
-valve Left AV (bicuspid or mitral)
-Left AV valve - Two leaflets (cusps)
valve Right AV (tricuspid) valve
-Right AV valve - Three leaflets (cusps)
2)Arterial (Semilunar)Valves
-Between the ventricle and artery
3)Pulmonary valve
-Pulmonary trunk, right ventricle
4)Aortic valve
-Aorta, left ventricle
-Prevent the backflow of blood from the arteries into ventricles when ventricles relax
what is the function of the AV valve apparatus?
Prevents eversion of av valves into atria during ventricular contraction
Valves open from pressure gradients
How do valves open and close?
Forward gradients open valves
Backward gradients close valves
What is the cardiac skeleton? What is its function(s)?
Fibrous skeleton of the heart
-Dense connective tissue
-Separates atria from ventricles
-Electrically inactive
- Support for heart
Coronary circulation
Blood through tissues of the heart
Coronary arteries
originate at aortic sinuses at base of ascending aorta
Coronary veins
drain into the coronary sinus, which empties into the right atrium
Coronary sinus
collection of veins joined together to form a large vessel that collects blood from the myocardium of the heart
Systole (contraction)
Myocardial blood flow almost ceases
Diastole (relaxation)
Myocardial blood flow peaks
What are the two types of myocytes? What are their functions?
Contractile cells
-mechanical work of pumping, propel blood
do not initiate action potentials
Conducting cells
-initiate and conduct the action potentials responsible for contraction of the contractile myocytes (1 % of myocytes)
few myofibrils
Describe the spread of excitation from the SA node to the rest of the heart.
SA node
Internodal pathways
Atrial myocardium
AV node
Bundle of His
Right and left bundle branches
Purkinje fibers
Ventricular myocardium
Why is the SA node important?
Cardiac pacemaker
Initiates action potentials
Pacemaker potential
-Closing of K+ channels, Na+ entering through F-type channels and Ca2+ entering through T-type channels
Depolarization phase
- L-type channels open at threshold and Ca2+ slowly enters cell.
Repolarization phase
-Opening of K+ channels and closing of L-type Ca2+ channels. K+ exits through K+ channels
What is the role of the AV node?
100 msec delay
Delay ensures atria depolarize and contract first
Describe the changes in membrane permeability that underlie the action potential in a ventricular muscle cell
K+ permeability, then Na+ permeability, and then Ca2+ permeability
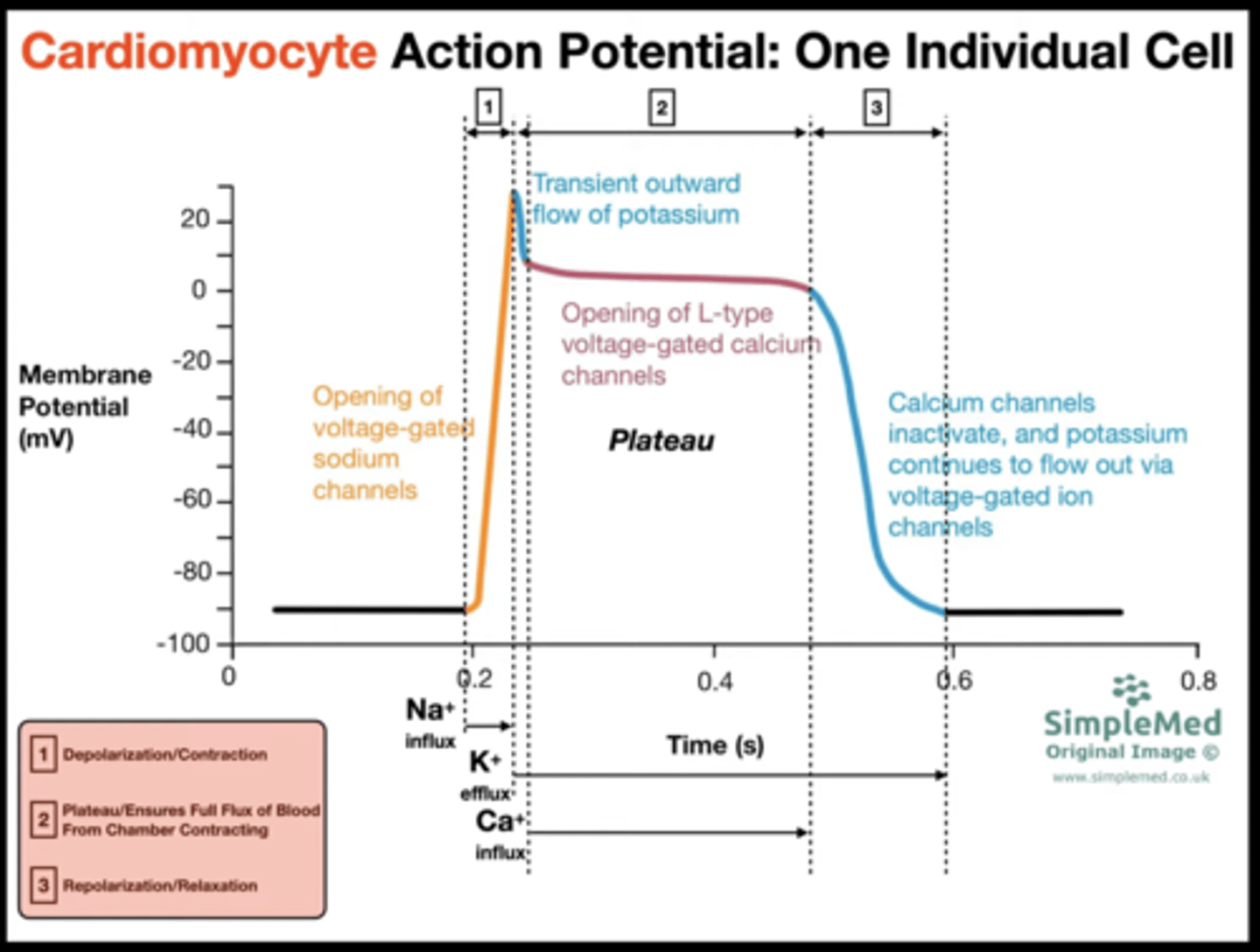
What ions/ion channels are involved in each phase of contraction of a ventricular muscle cell
Stable resting phase
- K+ leak channels
depolarization
-opening of fast voltage gated Na+ channels to threshold
Notch
- transient opening of K+ channels
Plateau
-Ca2+ entering through L-type channels and slow opening of K+ channels to repol the cells
Repolarization
-Opening of K+ channels and closing of Ca2+ channels
What is the pacemaker potential and how does it occur?
Slow depolarization to threshold
Regular spontaneous generation of action potentials
Slow depolarization to threshold
Regular spontaneous generation of action potentials
ECG
electrocardiogram
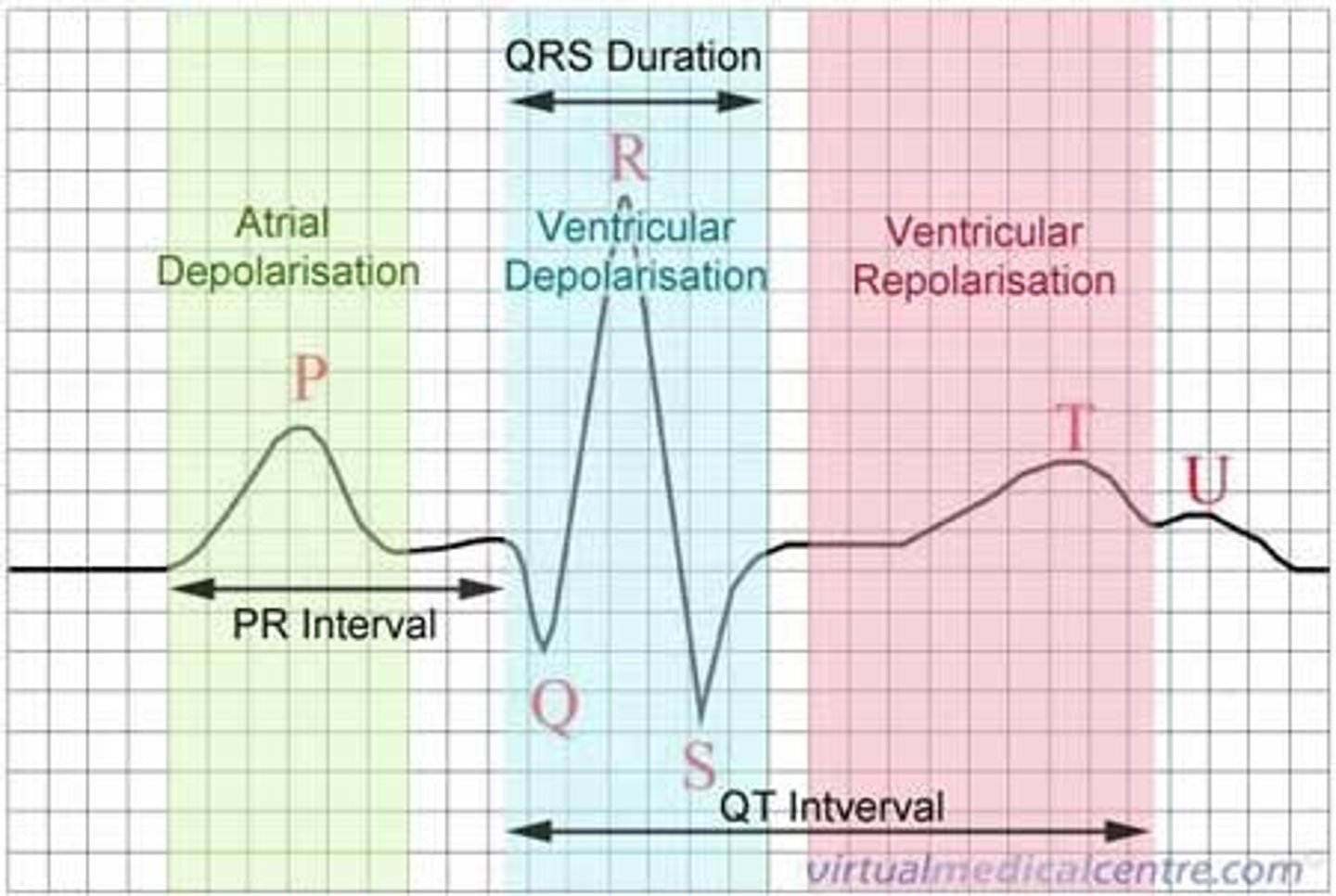
Relate the different waves (P, QRS, and T) to the atrial and ventricular action potentials.
P
- atrial depolarization
QRS
-ventricular depolarization
T
- ventricular repolarization
Describe the sequence of events leading to excitation-contraction coupling in cardiac muscle (contraction and relaxation)
Excitation
opening of plasma membrane L type Ca2+ and T tubules
Flow of Ca2+ into cytosol
Ca2+ binds to Ca2+ receptors
Opening of Ca2+ channels intrinsic to these receptors
Flow of Ca2+ into cytosol
Cytosolic Ca2+ increases
Contraction of muscle cells
Describe the structure of a myocyte
Sarcolemma
-cell membrane of muscle cell
Sarcoplasmic reticulum
-stores calcium ions for contraction
Striated
T-tubules (Transverse-tubules)
-invaginations of sarcolemma; transmit depolarization of membrane into interior of muscle cell
What is the refractory period?
Period of time in which a new action potential cannot be initiated
Absolute Refractory Period
-~ 250 msec
-No response to another stimulus
-Inactivation of Na+ channels
-Prevents tetanus
What are the different phases of ventricular systole
-ventricular contraction and blood ejection
-Isovolumetric ventricular contraction
-all heart valves closed, blood volume in ventricles remains constant, pressures rise. Muscle develops tension but cannot shorten
Ventricular ejection
-pressure in ventricles exceeds that in arteries, semilunar valves open and blood ejected into the artery
- Muscle fibers of ventricles shorten
Stroke volume
-volume of blood ejected from each ventricle during systole
What are the different phases of ventricular diastole
ventricular relaxation and blood filling
Isovolumetric ventricular relaxation
-all heart valves closed,
-blood volume remains constant, pressures drop
Ventricular filling
-AV valves open, blood flows into ventricles from atria.
-Ventricles receive blood passively (atria are relaxed)
Passive ventricular filling
-majority of ventricles
-Atria contract at the end of ventricular filling
End-diastolic volume (EDV)
amount of blood in each ventricle at the end of ventricular diastole
End-systolic volume (ESV)
amount of blood in each ventricle at the end of ventricular systole
Stroke volume
volume of blood pumped out of each ventricle during systole
Cardiac output
the product of heart rate (HR) and stroke volume (SV)
Understand the pressure-volume curve
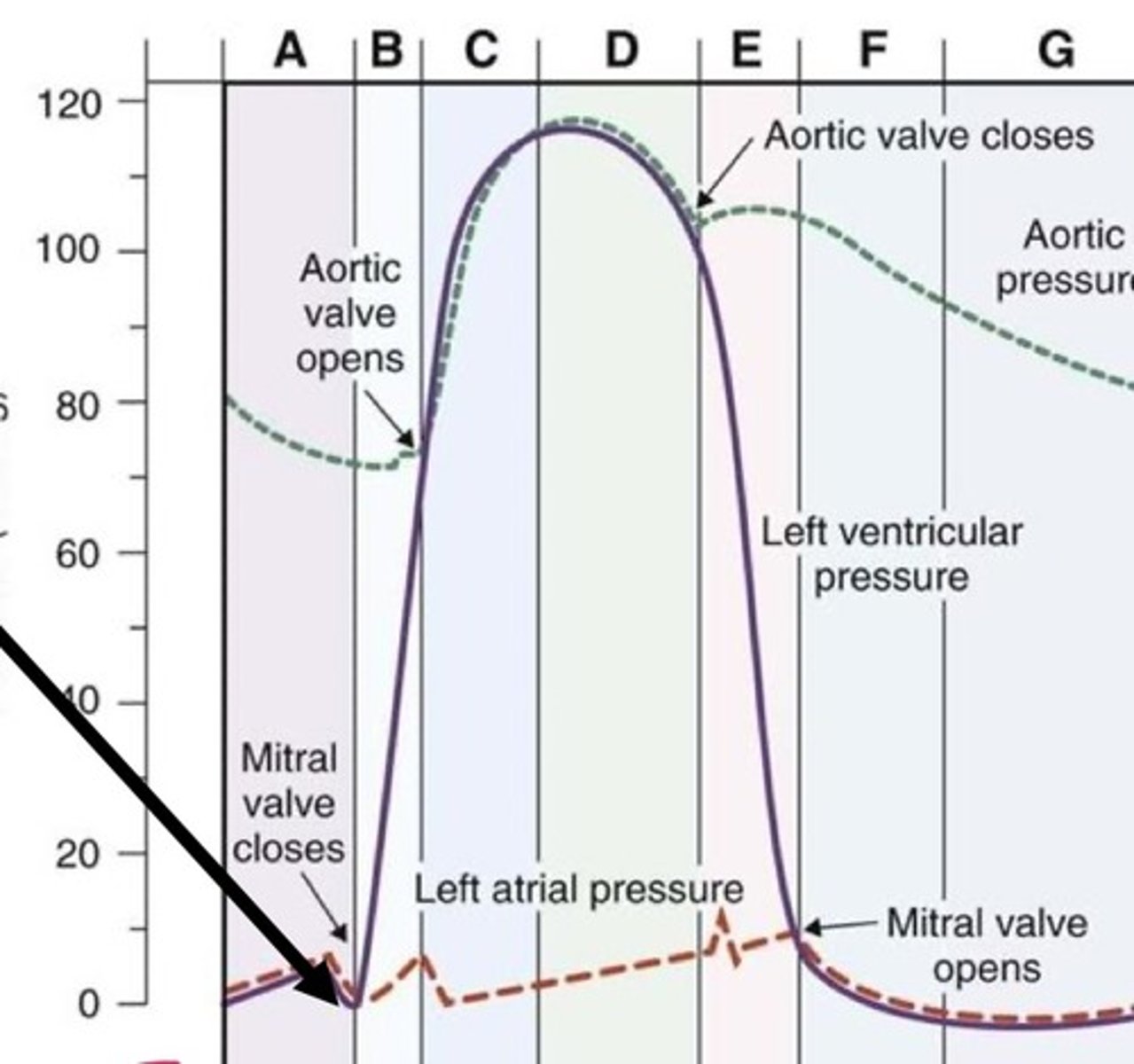
How does the left ventricular pressure curve differ from the right ventricular pressure curve?
The right ventricle develops lower pressures than the left ventricle during systole
Describe the effect of sympathetic and parasympathetic innervation on the heart.
Sympathetic innervation →
atria
- increases contractility
ventricles
-increases contractility
SA node
- increase HR and rate of depol
AV node
- increases conduction
- decreases nodal delay
Parasympathetic innervation →
atria
- decrease contractility
SA node
- decrease HR and rate of depolarization
AV node
- increase nodal delay
- decreases conduction
How do the sympathetic systems affect heart rate, stroke volume, and cardiac output?
Increased sympathetic activity
-Increase heart rate
-↑ the slope of the pacemaker potential
-Increase HR
-Increases F-type and T-type channel permeability
How do the parasympathetic systems affect heart rate, stroke volume, and cardiac output?
Increased parasympathetic activity
-Decrease heart rate
-↓ the slope of the pacemaker potential
-Decrease HR
-Decreases F-type channel permeability
-Hyperpolarizes cells (↑ K+ permeability)
How does SNS alter pacemaker potential
increases the slope
How does the PNS alter pacemaker potential
Decreases the slope
What is the relationship between cardiac output, stroke volume and heart rate?
CO = HR x SV
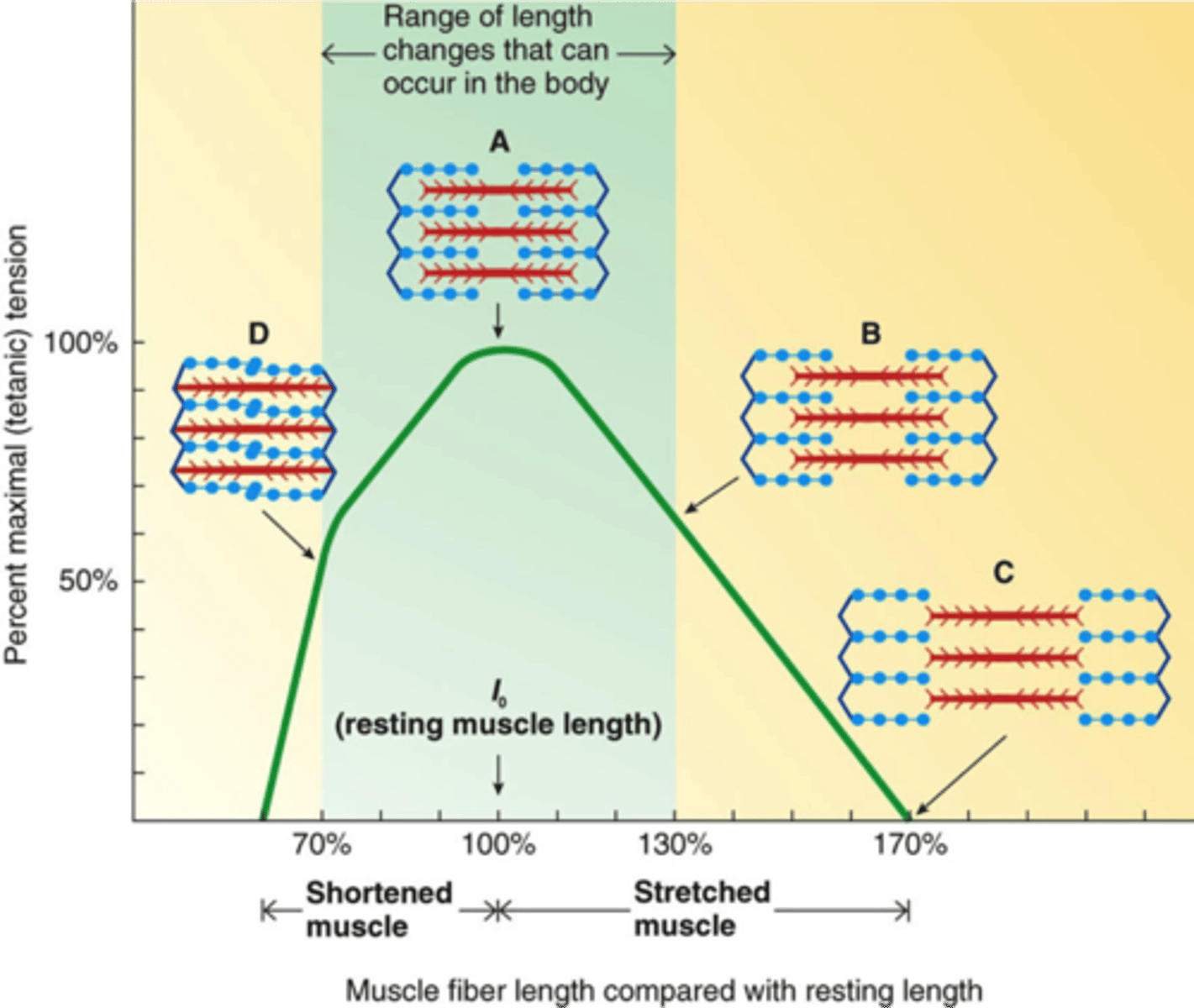
What are the principles of the Frank-Starling mechanism?
Relationship between EDV and SV
Main determinant of cardiac muscle fiber length
-degree of diastolic filling
-preload
Increase filling → increase EDV → increase cardiac fiber length → greater force during contraction and greater SV
What is preload?
tension or load on myocardium before it begins to contract or amount of filling of ventricles at the end of diastole
How does EDV alter the SV?
EF = SV/EDV
increase EDV - greater SV
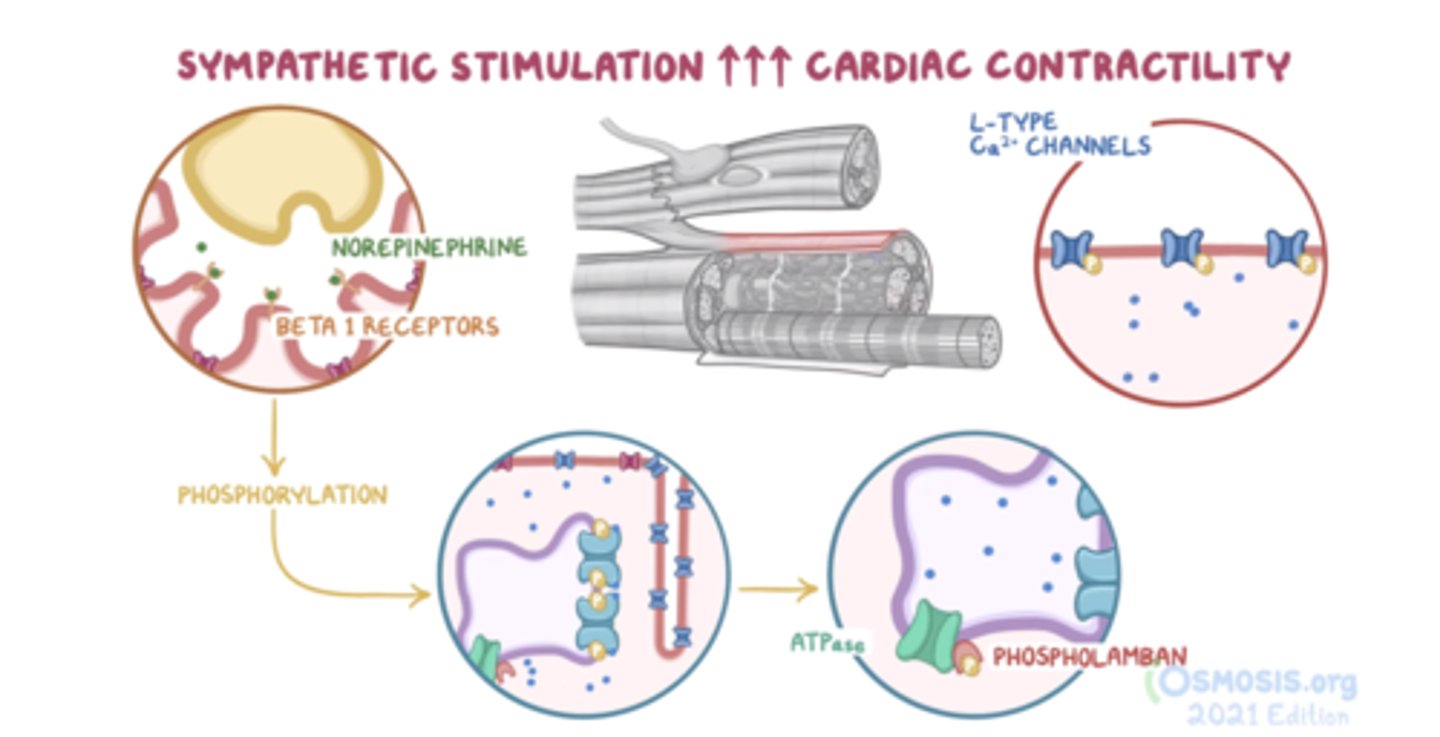
Describe the effects of the sympathetic system on cardiac muscle during contraction and relaxation.
SV is greater at any given EDV
-Ventricular ejection fraction is the fraction of the end-diastolic -ventricular volume ejected
Ejection Fraction (EF) = SV/EDV
- More rapid contraction and a more rapid relaxation
Through what mechanisms does the sympathetic system affect contractility?
What is afterload?
tension (or arterial pressure) against which the ventricles contract
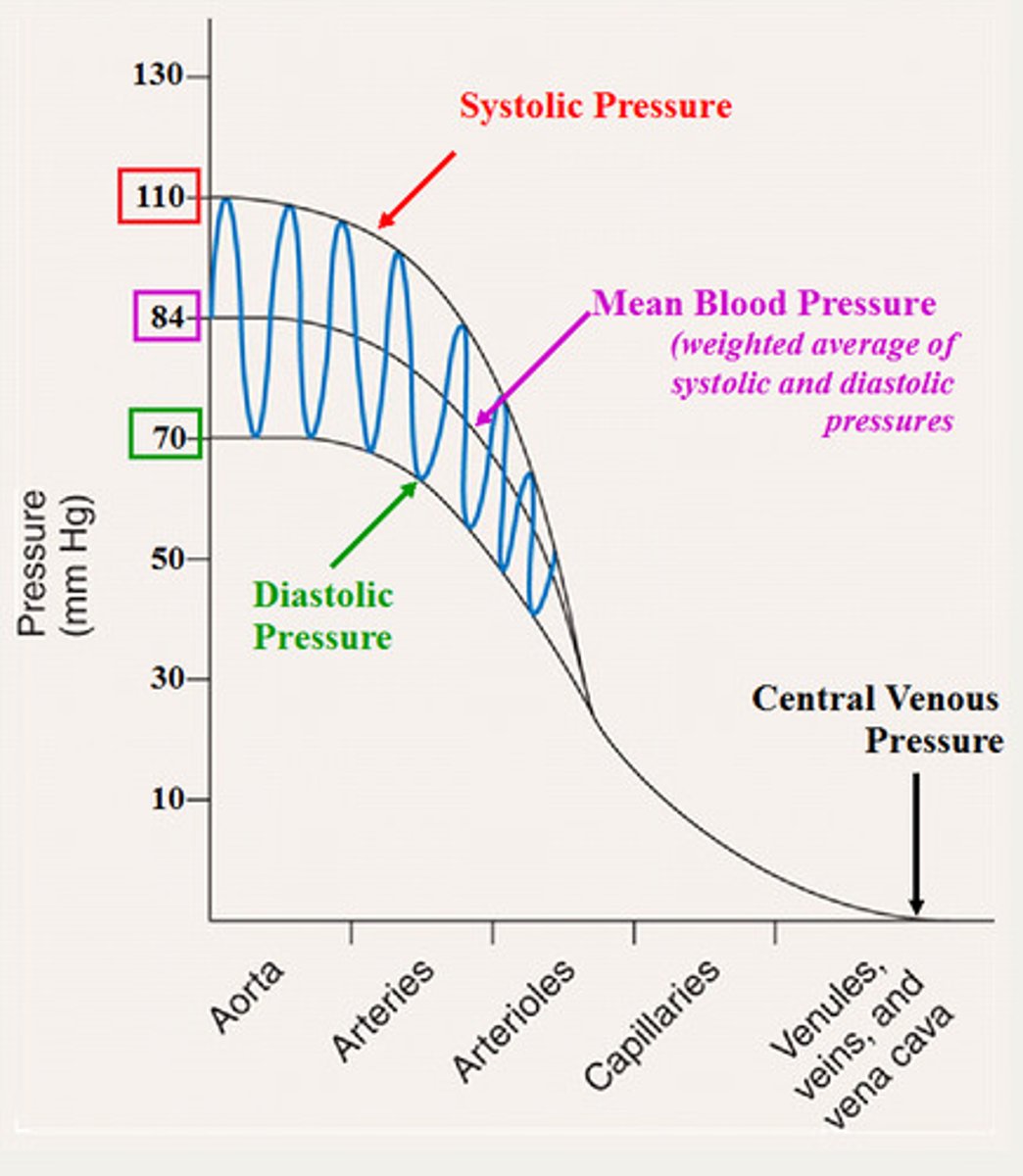
Describe how the pressures change in the arteriole and systemic circuits as the distance from the heart increases. Where does the largest pressure drop occur?
-MAP decreases as distance from heart increases
-Largest drop in pressure occurs across the arterioles
Systolic pressure
maximum blood pressure during ventricular systole
Diastolic pressure
minimum blood pressure at end of ventricular diastole
Pulse pressure
systolic - diastolic
What is mean arterial pressure? How does it change along the circulatory system?
pressure driving blood into tissues averaged over cardiac cycle
What are two functions of the arterioles?
1. Regulate blood flow to organs
-Capillary beds
2. Determine MAP
-Resistance vessels
What is the difference between intrinsic (local controls) and extrinsic factors that alter the basal tone of arterioles?
Extrinsic
-factors external to the organ or tissue
-whole body needs (MAP); nerves and hormones
Intrinsic
-local controls
-organs and tissues alter their own arteriolar resistances
-independent of nerves or hormones
Give examples of extrinsic factors altering the basal tone of arterioles.
Nerves
-Sympathetic innervation
NE
-vasoconstriction (α-adrenergic receptors)
Sympathetic tone can be increased (vasoconstriction) or decreased (vasodilation) (in addition to vessel's intrinsic tone)
Regulating MAP - Noncholinergic, nonadrenergic nerves
NO
-vasodilation
Hormones
Epinephrine from adrenal medulla causes :
-vasoconstriction,(αadrenergic receptors)
-Vasodilation.(β2 -adrenergic receptors)
What changes occur in the pressure volume loop following a change in: contractility, preload and afterload
Increased slope of ESPVR with increased contractility
-ESV decreases
-Increased contractility results in increased SV
Increased preload (filling) results in increased SV
-Increase in EDV
-No change in ESPVR
Ventricle must generate more pressure to eject blood with an increased afterload
-SV decreases
-ESV increases
What does the width and area of the pressure volume curve represent?
Width = Stroke volume
Area = Stroke work
What are the different phases of the pressure volume loop
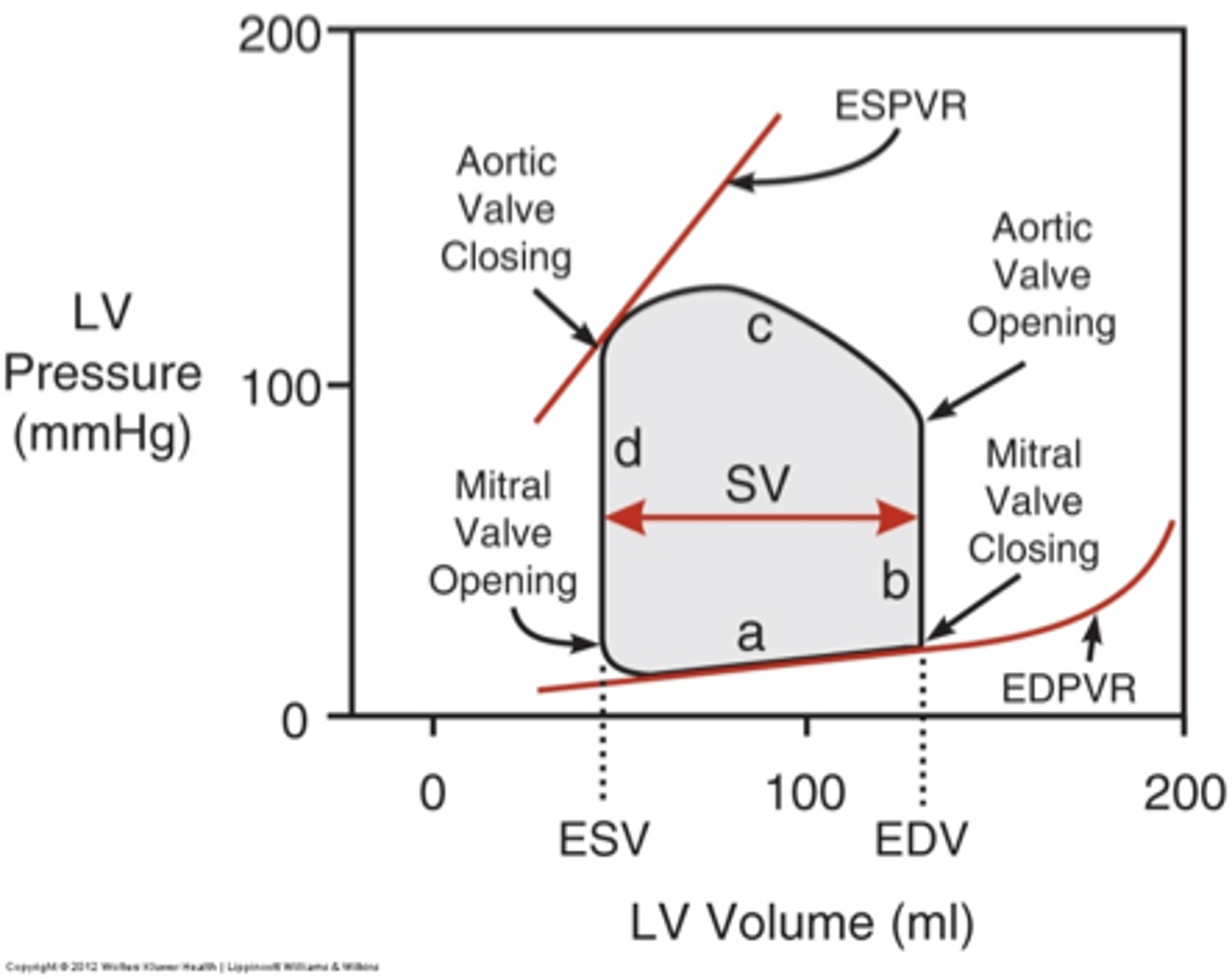
Discuss the key components of the left ventricular pressure-volume loop
Physiologically relevant hemodynamic parameters determined from these loops are:
-stroke volume
-cardiac output
-ejection fraction
-myocardial contractility
Pressure volume loops are generated by real-time measurement of pressure and volume within the left ventricle
What are the key components of the cardiac length-tension relationship?
What is contractility?
strength of contraction at any given EDV
What is the effect of a positive inotropic agent?
Positive inotropic agent
-catecholamines (Epi), exercise
-Increase contractility
-↑ Ca2+ increases contractility
1. Increased Ca2+ influx into cell and Ca2+ -induced Ca2+ release from SR
2. Increased sensitivity of the SR Ca2+ release channel Ca2+
3. Stimulate SERCA to increase SR Ca2+ stores for later release
4. Increased Ca2+ entry into the cell increases SR Ca2+ stores
What is the effect of a negative inotropic agent?
Heart failure
Decrease contractility
↓ Ca2+ decreases contractility
When the arterial baroreceptors increase or decrease their rate of firing, what changes in autonomic outflow occur and cardiovascular function occur?
Increase in MAP increases rate of firing of baroreceptors
• Decrease in MAP decreases rate of firing of baroreceptors
• Respond to changes in pulse pressure
Medullary cardiovascular center
-Medulla oblongata
-Receives input from baroreceptors
-Alters vagal stimulation (parasympathetic) to heart and sympathetic innervation to heart, arterioles and veins
Baroreceptors adapt to sustained changes in arterial pressure
What causes a change in firing of the arterial baroreceptors?
Rate of discharge is proportional to the mean arterial pressure
Describe the arterial baroreceptors.
Respond to mean arterial pressure and pulse pressure
Respond to changes in pressure when walls of vessel stretch/relax
Degree of stretching is directly proportional to pressure
• What is the difference between long-term regulation of blood pressure and short-term regulation of MAP?
Short-term regulation
-Seconds to hours
-Baroreceptors reflexes
-Adjusts cardiac output (CO) and total peripheral (TPR) resistance by ANS
Long-term regulation
Adjust blood volume
Restore normal salt and water balance through mechanisms that regulate urine output and thirst
How do changes in CO and TPR affect MAP?
MAP = CO x TPR
What is the relationship between MAP, CO and TRP?
- MAP = mean arterial pressure
- CO = cardiac output
- TPR = total peripheral resistance
determined by total arteriolar resistance
How does venous return affect the SV? (ie. Frank-Starling law)?
Increased venous return results in increased stroke volume through the Frank-Starling mechanism
The venous system is a low pressure system. What mechanisms aid in returning blood back to the heart
Smooth muscle in veins
-Innervated by sympathetic neurons
Skeletal muscle pump
-Compresses veins
-Venous pressure increases, forcing more blood back to heart
Respiratory pump
-Inspiration causes an increase in venous return
What mechanisms prevent the backflow of blood into capillaries?
Valves
-folds
-Prevent the backflow of blood to capillaries
What is the function of the venous system?
High capacitance vessels
-store large volumes of blood
Highly distensible at low pressures and have little elastic recoil
-Reservoir of blood
What is the difference between filtration and reabsorption?
Filtration
-movement of protein-free plasma from capillary to IF •
Reabsorption
-movement of protein-free plasma from IF to capillary
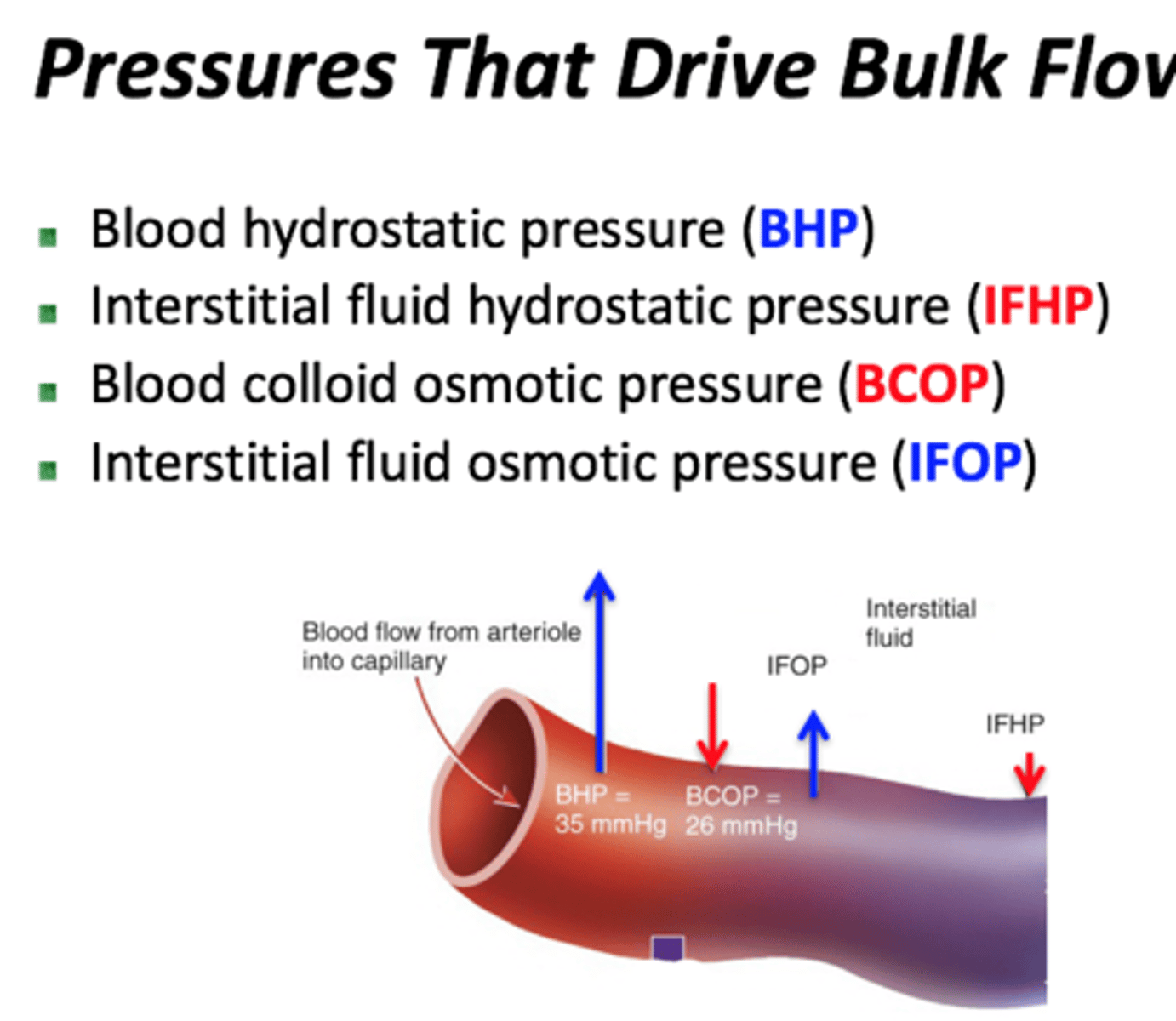
What pressures drive bulk flow
Which end of the capillary favors filtration
arterial end
Which end of the capillary favors absorption
venous end
hydrostatic pressure
the pressure within a blood vessel that tends to push water out of the vessel
colloid pressure
osmotic pressure produced by plasma proteins
Diffusion
movement of substance down its concentration gradient
Transcytosis
transport into, across, and then out of cell
bulk flow
The movement of a fluid due to a difference in pressure between two locations.
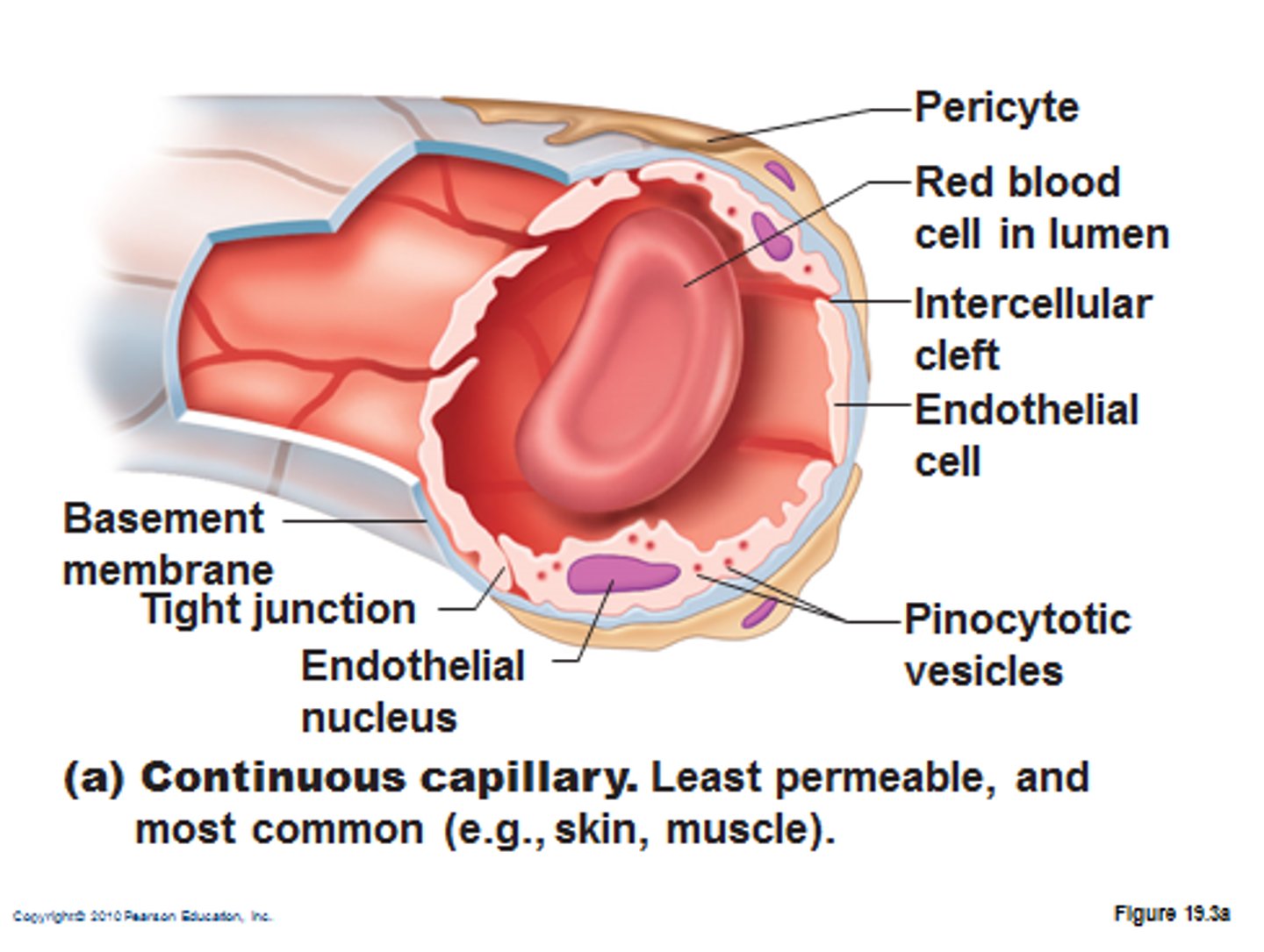
continuous capillaries
Exchange of water, small solutes, lipid-soluble material, no exchange of blood and plasma proteins