Class 17- The Major Minerals K, Na, P & Bone Health Vit D, osteoporosis
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
inorganic elements are…
are NOT destroyed by heat, air, acid, or mixing
act as binders, can Impact mineral bioavailability in some foods
Phytates and oxalates - considered anti-nutrients bc binds nutrients —> Occur in foods that are plant origin
Excess of some mineral can create an inadequacy of another, Supplements are often to blame
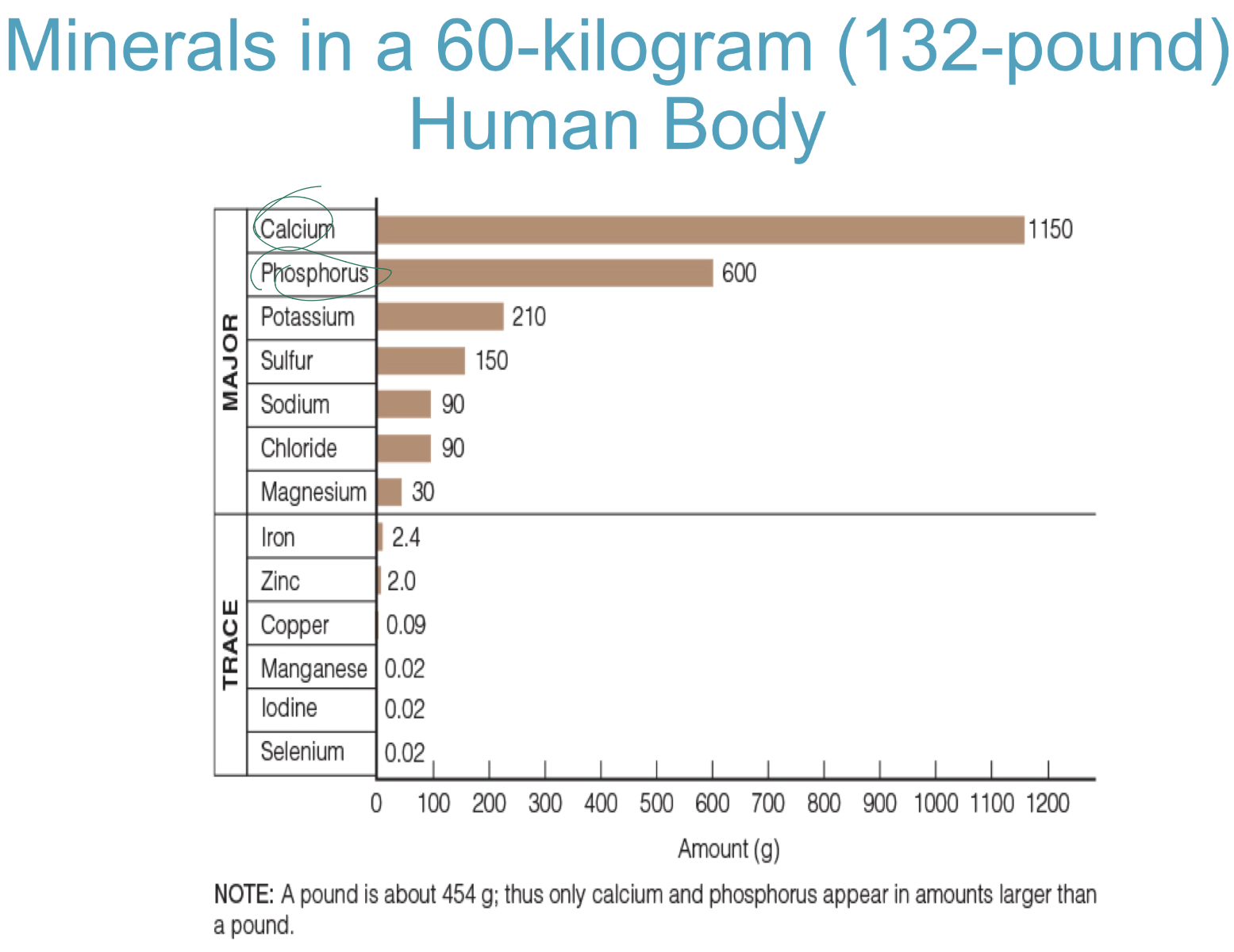
what are the major minerals in human body (7)
how is potassium involved in electrolyte balance?
Intracellular cation
High blood concentraion (cardiac arrest)
Deficiency= Losses (vomiting and
diarrhea)
Diuretics (for
hypertension)
what does sodium have to so with electrolyte balance?
Extracellular cation
Blood volume regulation
Na K ATPase
Roles in the body:
Fluid and electrolyte balance
Acid–base balance
Nerve transmission
Muscle contraction
Readily absorbed and travels freely in the blood
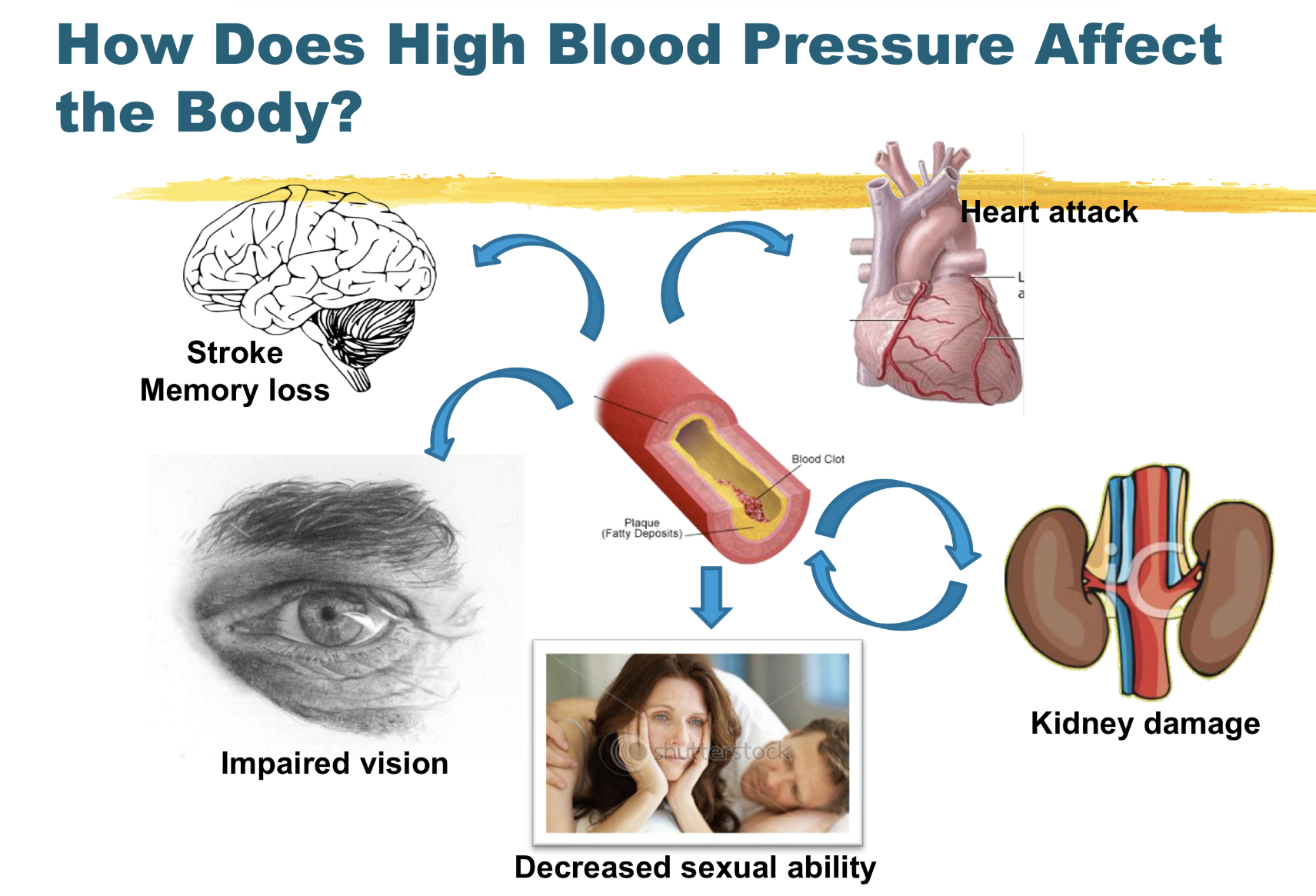
how does high blood pressure affect the body? (5 general things)
increases pressure everywhere!!
what does dash suggest to INCREASE that will help lower BP? (4)
Fibre, Potassium, Magnesium, Calcium
what are bones composed of? what does bone mineral density correspond to?
Composed of:
65% mineral crystals—> Strength and structural support
35% collagen—> Flexibility
BONE MINERAL DENSITY CORRESPONDS to bone strength
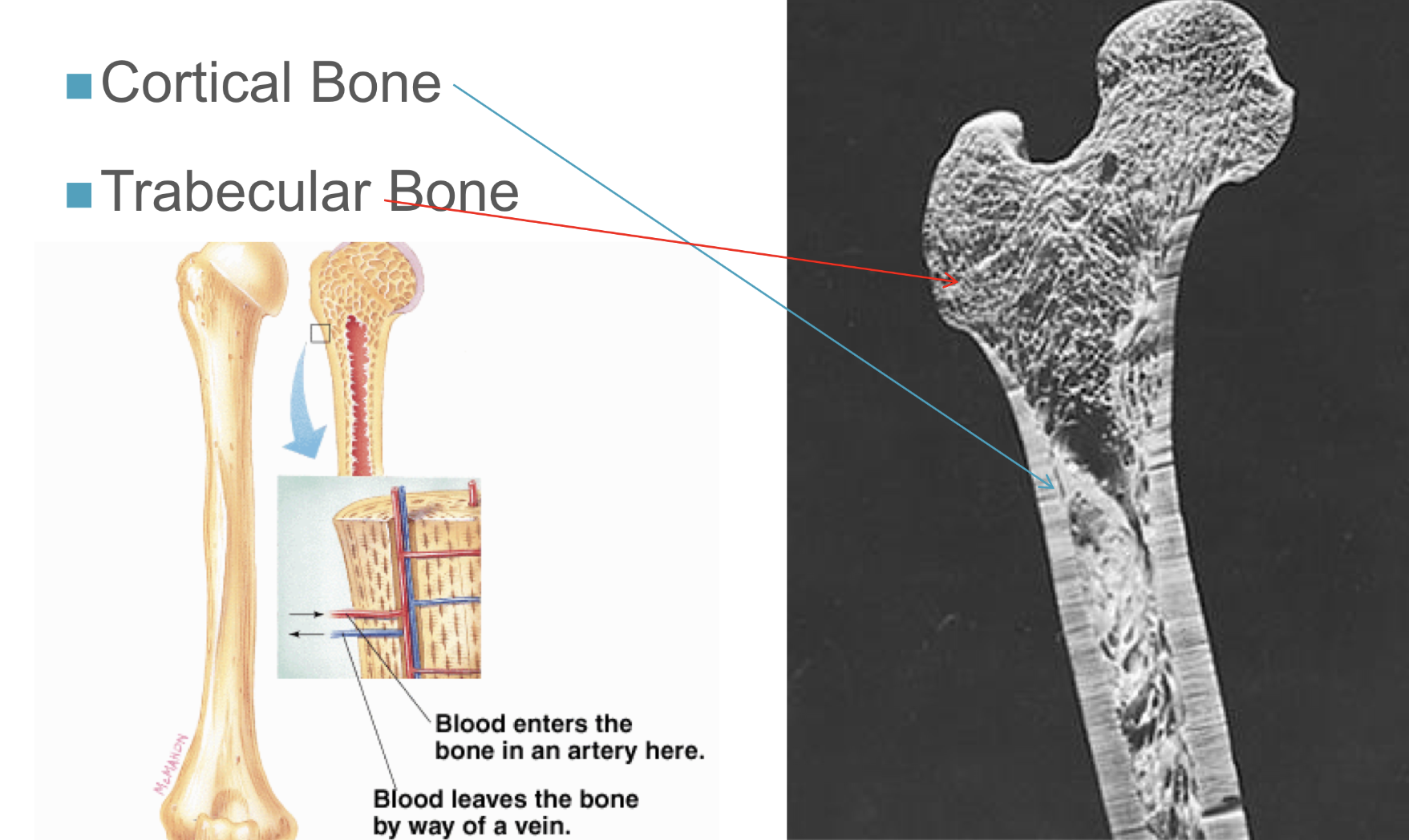
what are the 2 types of bone
TYPES:
cortical
80% of mineral structure, dense outer layer
gives up calcium to blood
trabecular
20% mineral of mineral structure
lacy bubbly structure
impacted by day-to-day intake and need for calcium
how do bones grow?
Genetically programmed to grow in length
Conception to teen years
Ceases at ~14 years (girls), ~17 years (boys)
Bone mineral density accrues at the same time into young adulthood – GOOD NUTRITION IS KEY!
Bone remodelling
Osteoclast and osteoblast activity
Occurs over a lifetime
Osteoclast > osteoblast activity as we age
how do osteoblasts and osteoclasts work tg, what do they do individually?
Osteoblasts and osteoclasts work together to form new bone cells and break down old or damaged bone tissue.
Osteoblasts form new bone tissue.
Osteoclasts break down old bone tissue to make room for new, healthier tissue to replace it
*osteoclast activity occurs more then osteoblast activity with age
BONE REMOLDING: bone growth vs bone modelling vs bone remoldeling
process of new bones being mad, old stuff getting remodelled
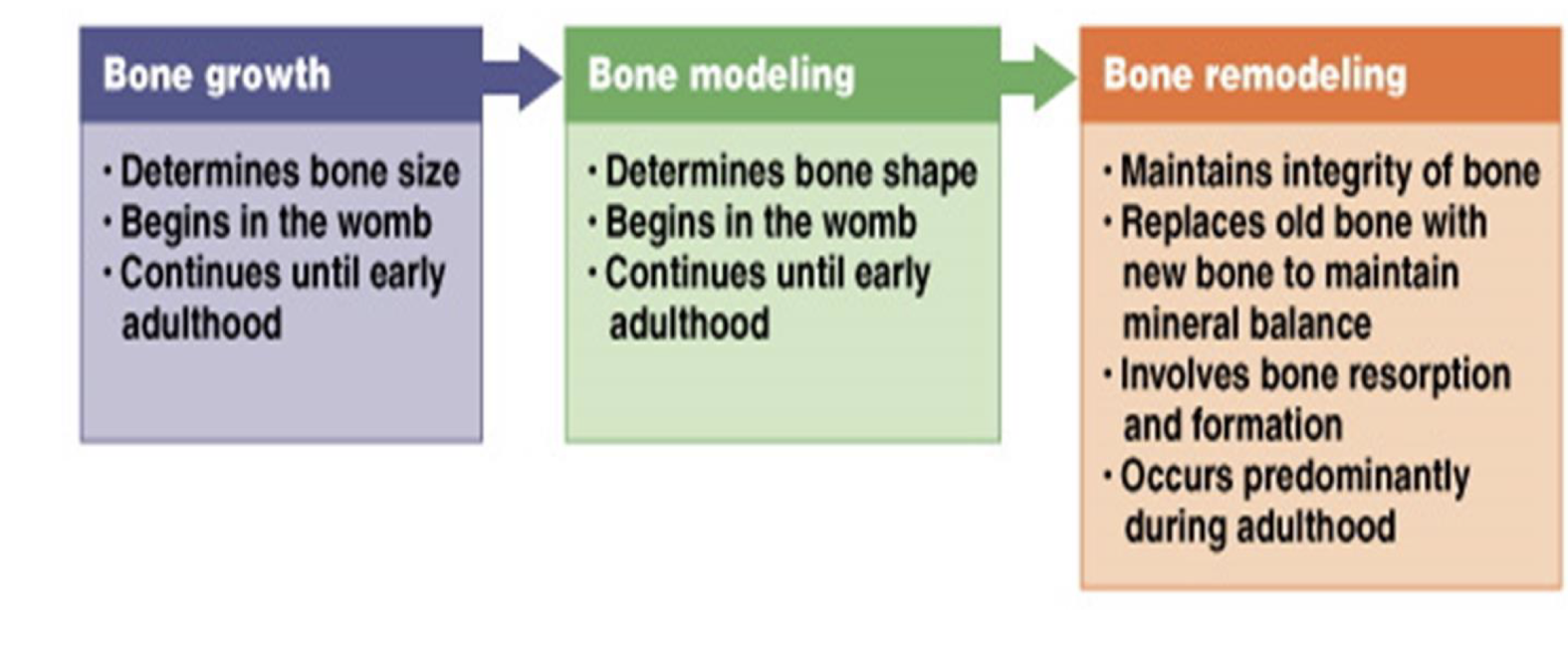
what are two steps of bone remolding,
bone resorption
the surface of bones id broken doens
osteoCLASTS wil erode surface of bones
bone formation
= new bone being formed after resorption
osteoBLASTS produce collagen containing components of bone
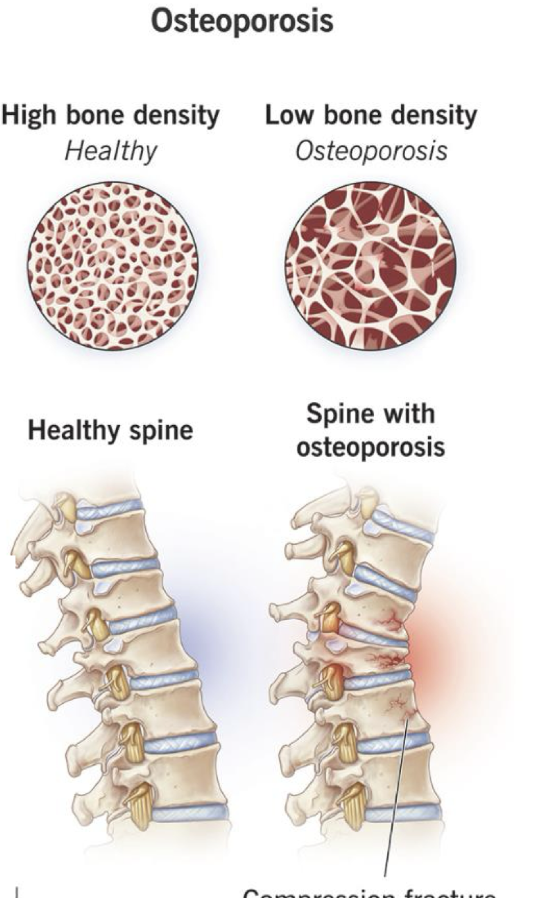
what is osteoporosis?
= disease that weakens bones
characterized by low bone mass & deterioration of bone tissue
inc risk of fractures:
○ Hip
○ Spine
○ Wrist
○ Shoulder
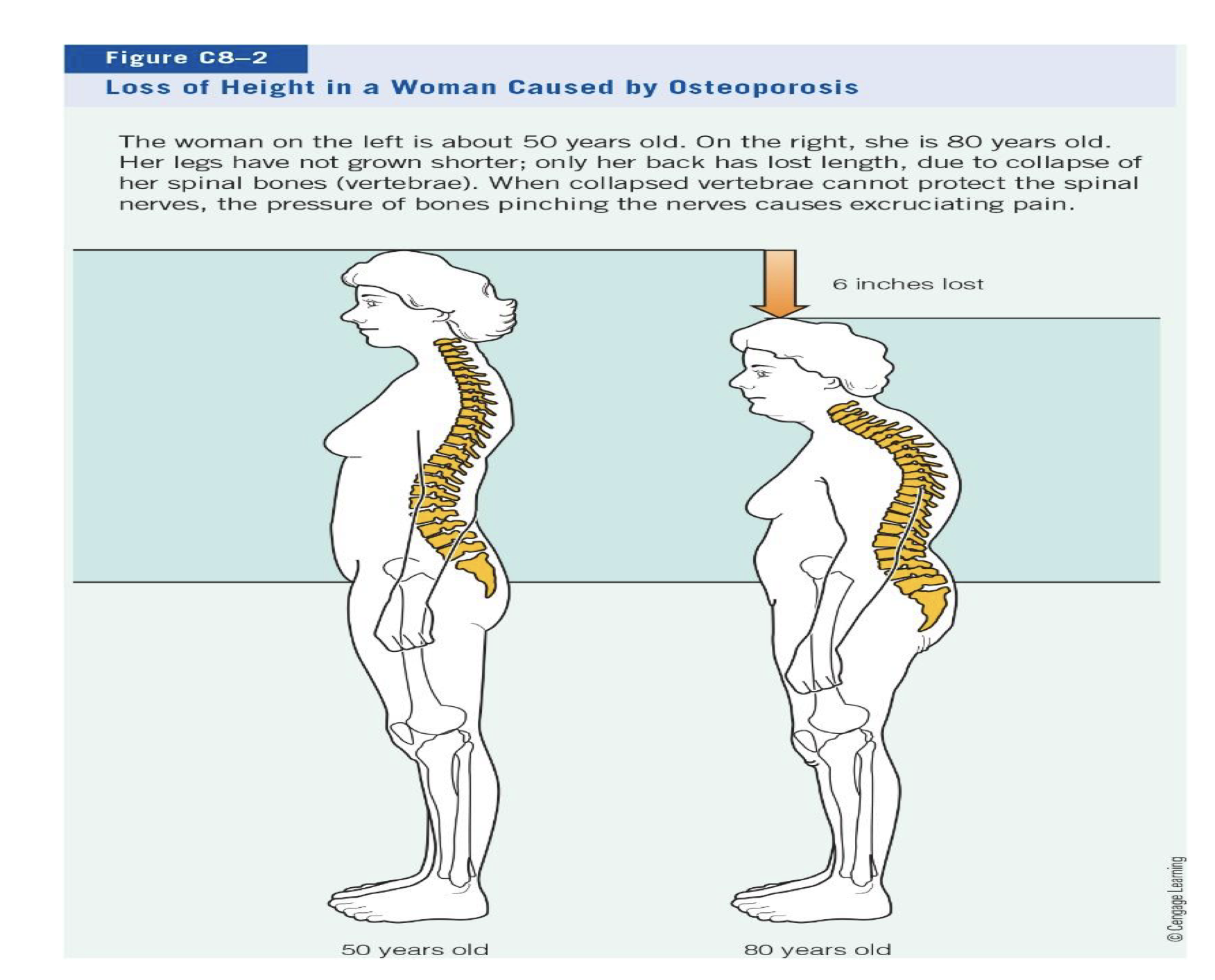
why do some women loose height?
caused by osteoporosis
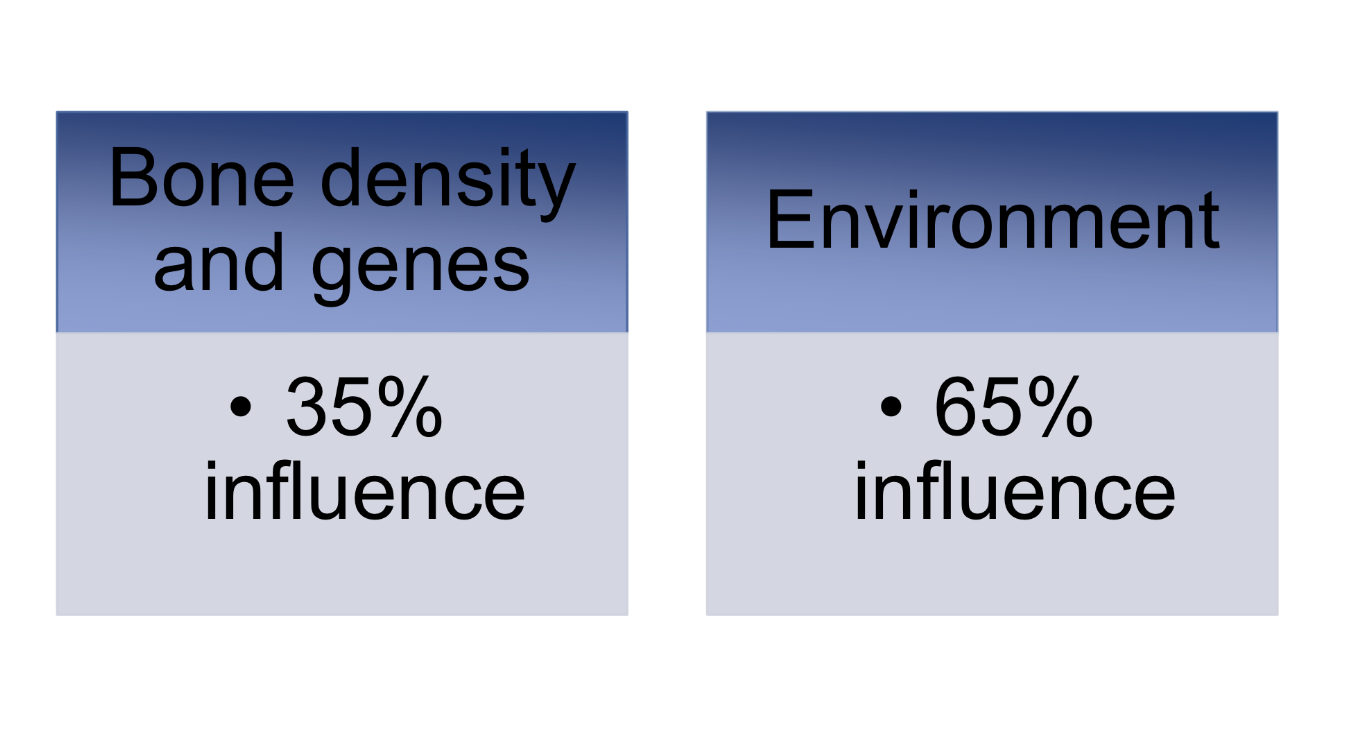
what are stats of environmental VS bone density/genetic causes of osteoporosis? explain environmental influences (2)
environmental:
CALCIUM AND VIT. D
-Bone strength in later life dependent on bone-
building during childhood and adolescence—> so good to build string bones when young!
ESTROGEN DEFICIENCY
- Greater bone lose for women during
menopause (estrogen production diminishes –
20% bone loss 6-8 yr post menopause)
• Men have greater bone density and smaller
losses
what are some non-modifiable risk factors for osteoporosis?
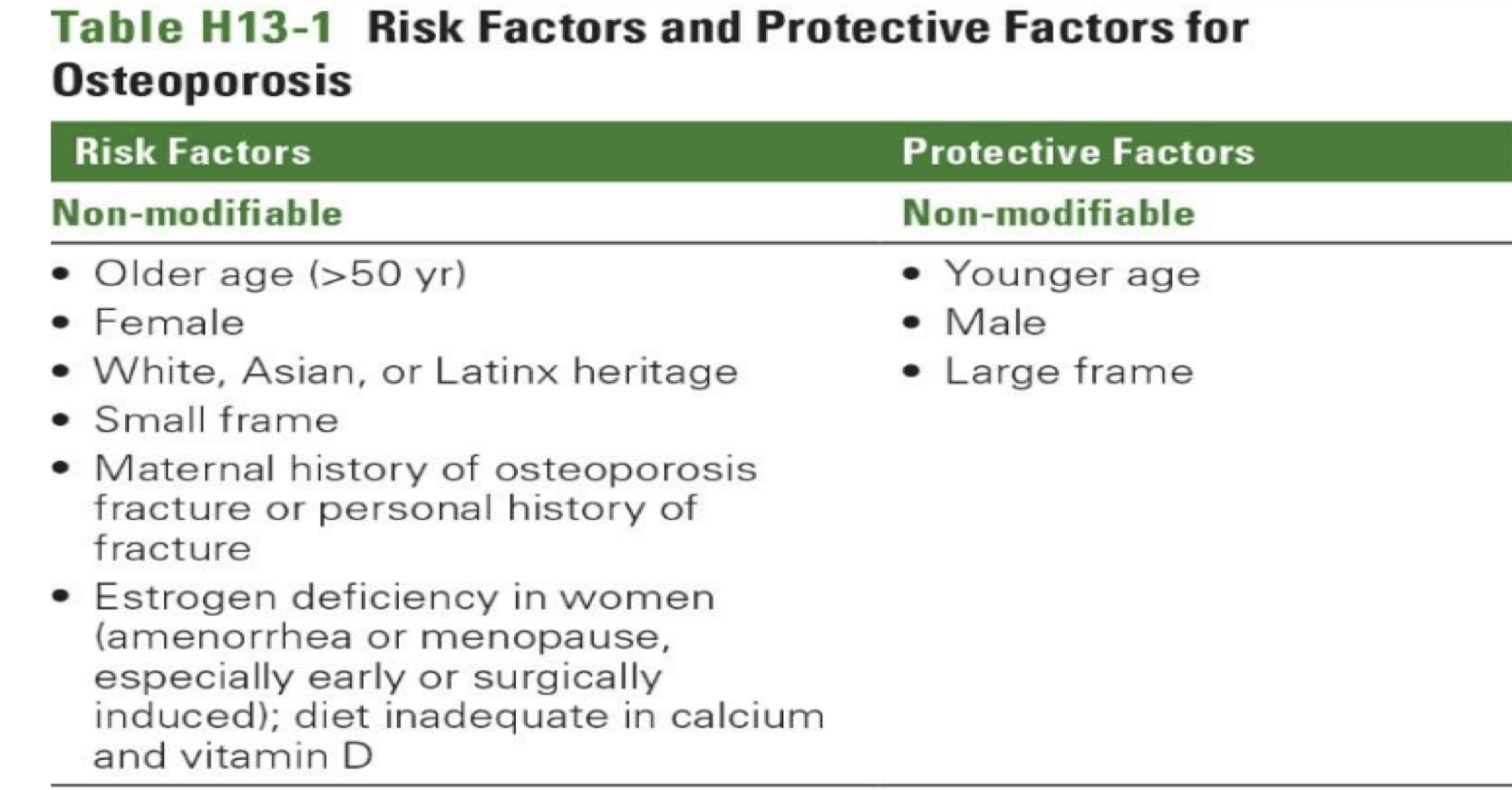
what are some example of modifiable risk factors for osteoporosis?
what is T-score range for normal bone, osteopenia, vs osteoporosis?
NORMAL=
t score -1 score or greater
OSTEOPENIA=
tscore= -1 to -2.5
Bone mineral density 1–2.5 SD below the mean established for a young normal population
OSTEOPOROSIS=
tscore >-2.5
Bone mineral density > 2.5 SD
below the mean established for
a young normal population

explain bone growth team: players, coaches, assistant
Players
protein - collagen
minerals - Ca, P, Mg, Fl
Coaches
Vitamin D, parathyroid hormone
calcitonin
Assistants/Scouts
Vitamins: A, C, K, Bs, omega 3,
phytochemicals
explain the role of phosphorus (what does it work w and form?) and magnesium in bone
PHOSPHORUS
working w Ca , it forms hydroxyapatite mineral of bone
High intake decreases Ca absorption
Typical intake is higher than RDA
MAGNESIUM
Bone structure and regulation of mineralization, vitamin D metabolism
ATP synthesis
Blood clotting, muscle contraction (Ca promotes,
Mg inhibits), blood pressure regulation
roles of Vit K, A, C in bone
Vitamin K
Co-enzyme synthesize bone protein – Osteocalcin Helps bind
minerals to bone
if Deficiency – cannot bind minerals
Vitamin A
Bone remodeling, osteoclast activity BUT will reduce BMD with supplements above UL…
Vitamin C
Cofactor for collagen synthesis (organic matrix)
what does weight train do for bone density?
Working muscles pull on bone, causing
more trabeculae and bones grow denser
Hormones supporting muscle growth
also support bone building
Bones of active people are denser and stronger than sedentary people
Most important factor supporting
children’s bone growth
Lasting benefits for older women
Conclusion: weight training improves
bone density… as does regular aerobic
exercise
what is involved with osteoporosis prevention/tretament, for 1. lifestyle , 2. what meds are prescribed in medical treatment? anabolic agents?
Lifestyle:
Nutrition: Ca, Vit D and..…
Physical activity- including wt training, wt bearing exercise
Quit smoking, decrease alcohol
Medical Treatment:
Anti-resorptive agents inhibit osteoclasts, E.g. Bisphosphonates
Hormone replacements (including SERMs eg Raloxifene)
Anabolic agents to stimulate osteoblasts, E.g. PTH
info on calcium, where is it stored in body?
Most abundant mineral in the body
• 99% stored in bones and teeth
Part of bone structure(hydroxyapatite)
Calcium reserve
Maintain bone turnover(building/breakdown)
• 1 % in body fluids:
- Extracellular and intracellular
compartments
what is calciums roles in disease prevention?
GOOD FOR DEC.:
Hypertension
Blood cholesterol
Diabetes
Colon cancer
Obesity
May help maintain healthy body weight
Osteoporosis
SO —> Reaching peak bone mass means denser bones protect against inevitable age-
related bone loss and fractures.
Osteoporosis is “silent” because the body
shows no symptoms.
smooth muscle contraction requires xxx
smooth muscle contraction requires calcium
how is calcium involved extra VS intracellular
EXTRAcellular
helps maintain BP
participates in blood clotting—> fibrinogen protein+ Ca+vit k
INTRAcellular
Regulation of muscle contraction
Transmission of nerve impulses
Secretion of hormones
Activation of some enzyme reactions
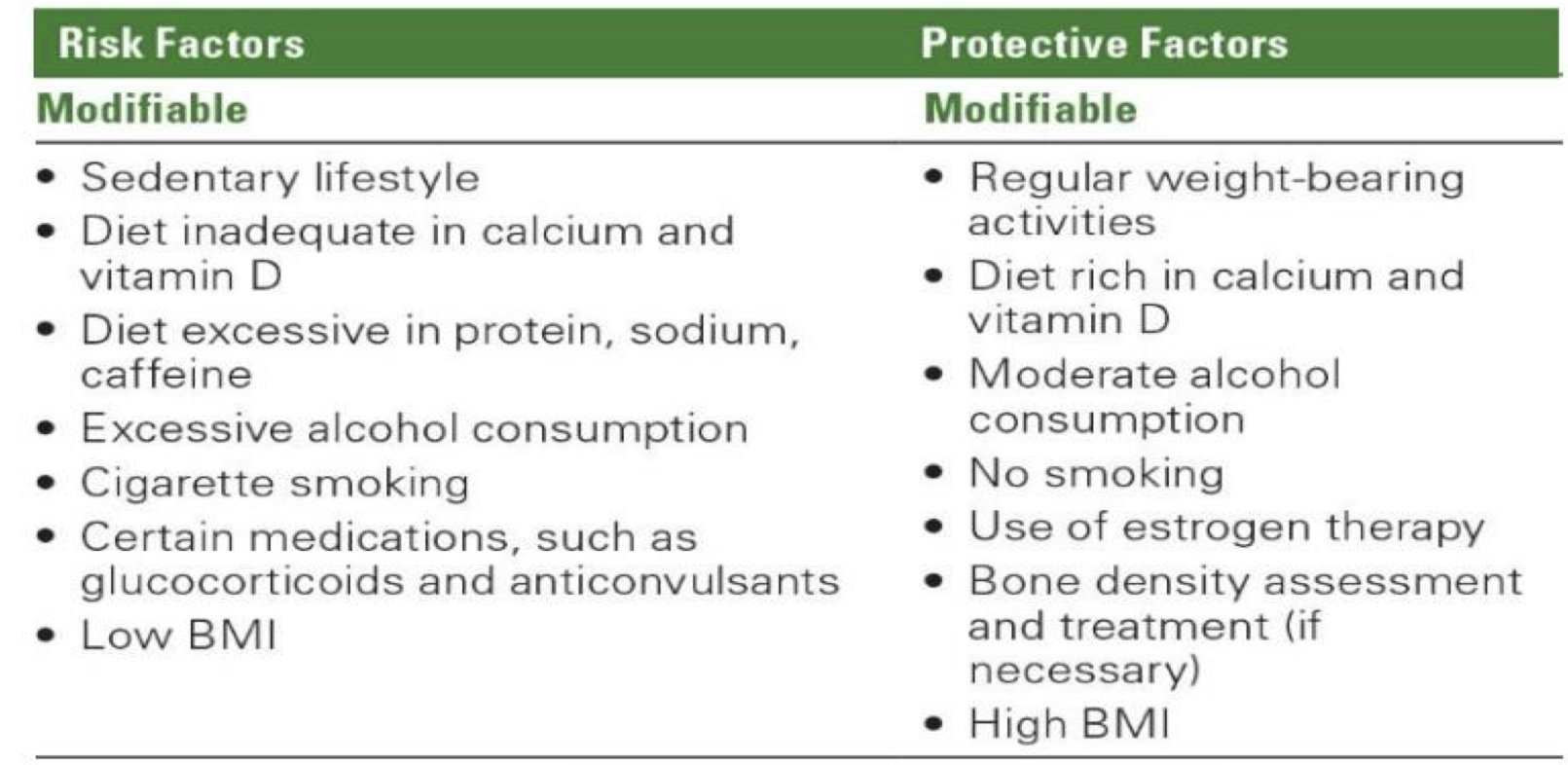
what happens when LOW blood calcium, what is occurs in thyroid, kidneys, intestines, bones, what is final result?
what happens when HIGH blood calcium, what is occurs in thyroid, kidneys, intestines, bones, what is final result?

what age group would have generally more calcitonin
to protect agains high lvls of calcium in blood
NOTE: Calcitonin plays a major role in defending infants and young children against the dangers of rising blood calcium that can occur when regular feedings of milk deliver large quantities of calcium to a small body. In contrast, calcitonin plays a elatively minor role in adults because their absorption of Ca is less efficient and larger bodies |
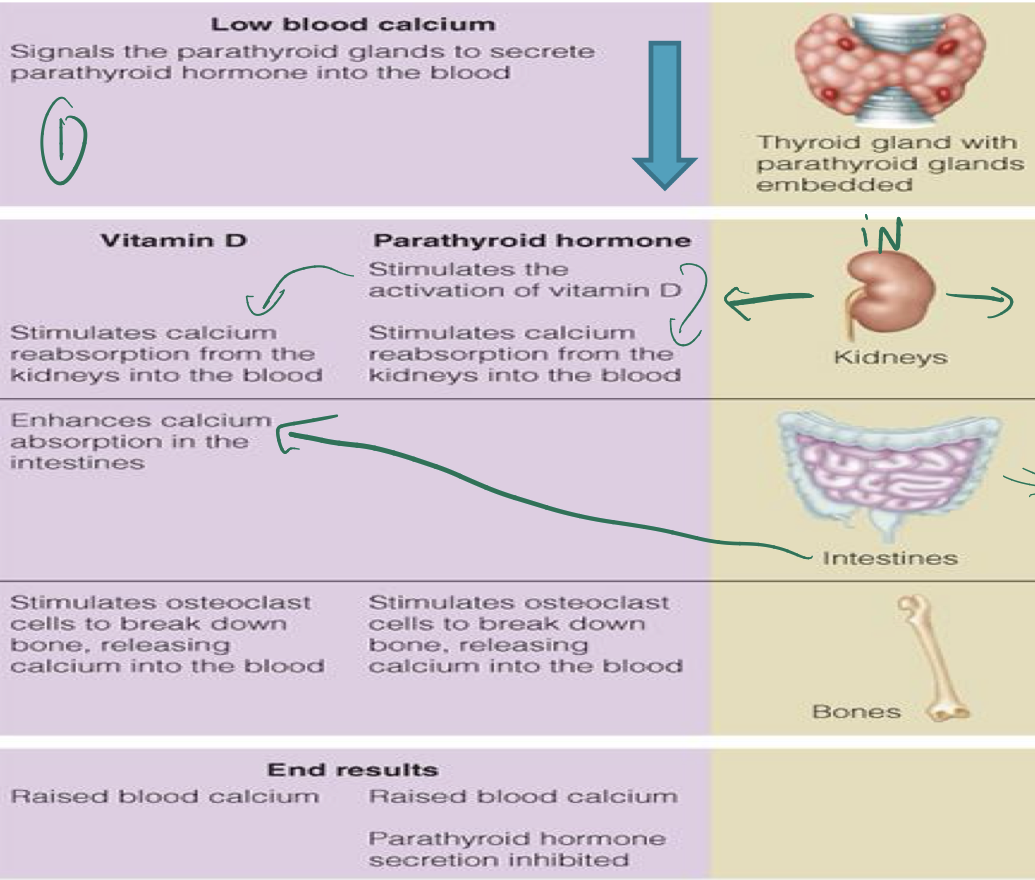
ACUTE VS CHRONIC calcium regulation
ACUTE
Blood Ca MUST be maintained
tetany/rigor
↑ ↓ blood Ca is a problem of regulation NOT DIET
CHRONIC
low dietary Ca - robs the “bone RRSP”
i.e. ↓ bone mineralization
stunting in children
osteoporosis
low calcium diet vs adequate calcium diet affects on: blood calcium vs affect on bones
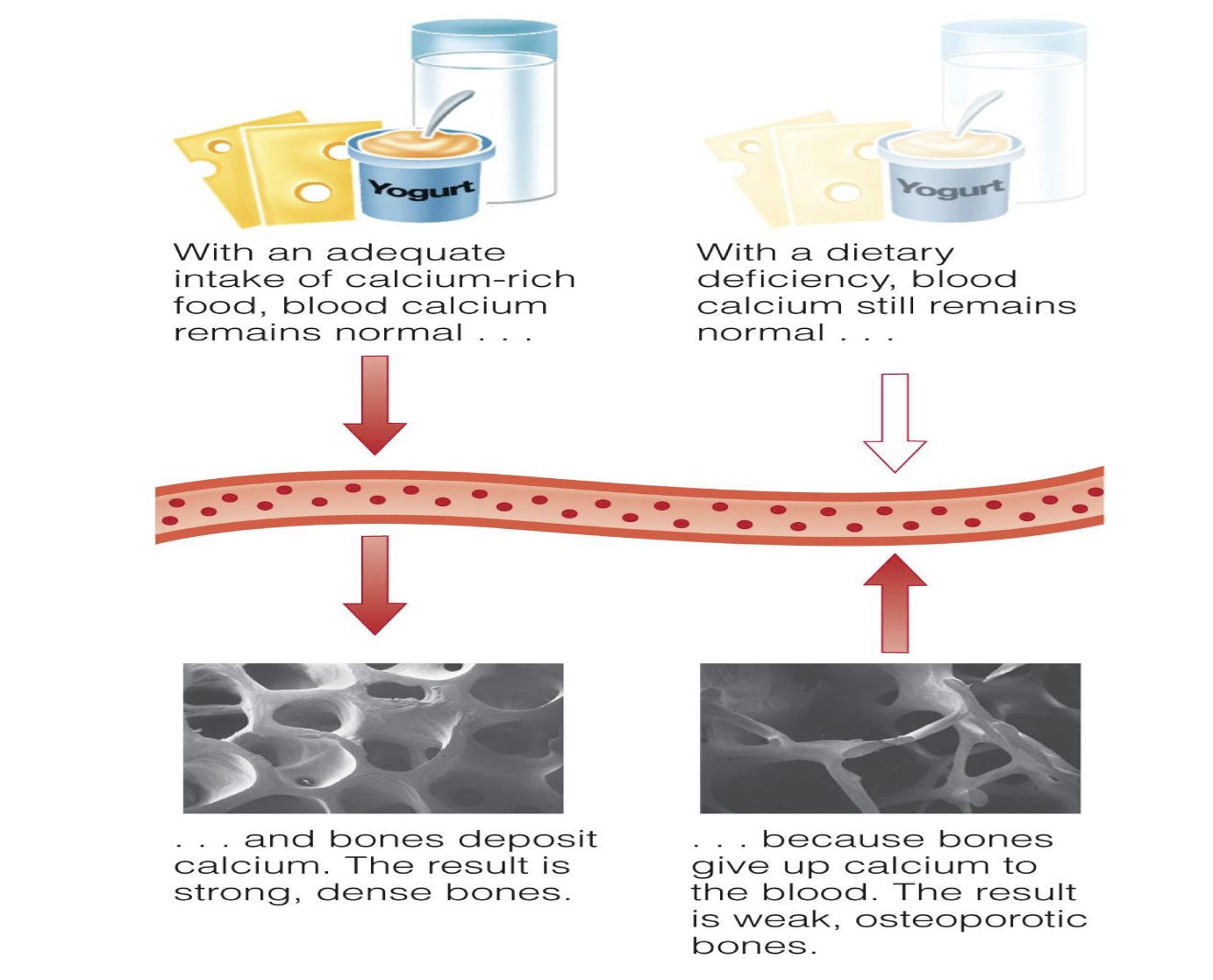
what are some Ca absorption factors? inc vs dec
absorption increased by:
anabolic hormones
gastric acid (meal)
vitamin D
low phosphate intake
lactose (in infants only
absorption dec by:
aging
lack of stomach acid
vitamin D deficiency
high phosphate intake
high insoluble fibre diet
phytates, oxalates
high protein intake
what is urinary calcium excretion influenced by?
Calcium intake
Age
Caffeine BUT Offset by milk in your coffee
Dietary sodium—> Individuals with hypercalciuria should be restrict sodium intakes to minimize urinary calcium excretion
Dietary protein—>Excretion of sulphate from sulphur amino acids
what can calcium toxicity lead to?
constipation, interferes w other minerals absorption, increase risk of kidney stone formation
Compromised Iron Status (and other minerals) Ca inhibits absorption
Milk Alkali Syndrome (metabolic alkalosis and renal failure)
Kidney stones
Vitamin D toxicity and increased serum Ca if supplements contain vitamin D
exposure to contaminants if supplements are from bone meal or dolomite
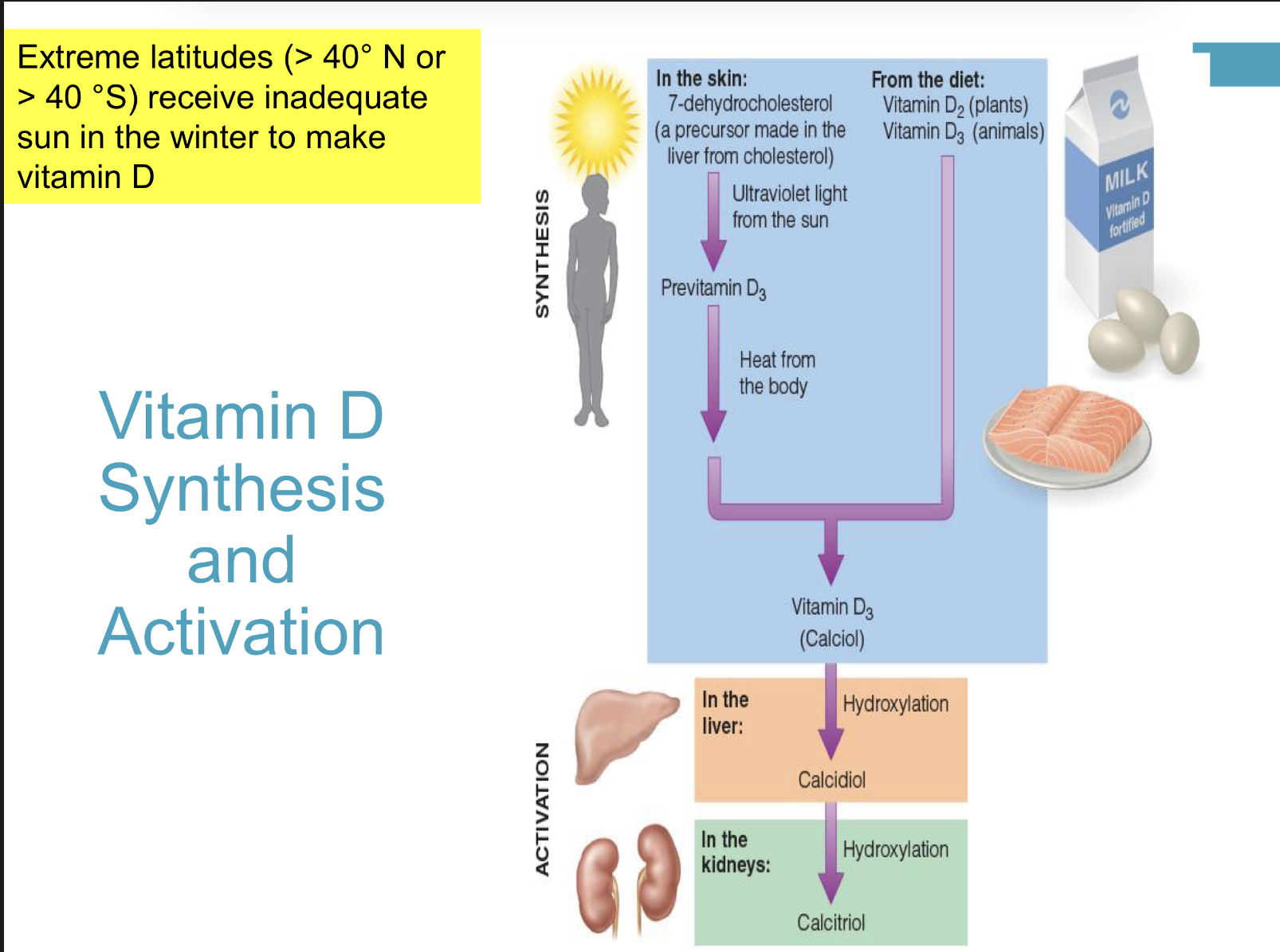
how can Vit D be absorbed from sun vs diet?
what are some vit D functions? what is active form?
Active form is a hormone- Essential for making and maintaining bones
Required for calcium and phosphorous absorption (calbindin)
Regulates blood calcium and levels
Stimulates osteoclasts
Necessary for bone calcification
New functions: immunity and cell differentiation
Brain and nerve cells, protects against cognitive
decline
Adipose cell regulation
is vitamin D a hormone or a vitamin? why?
BOTH
AS A HORMONE BC:
Travels in the blood
Activated in the liver and
kidneys
Acts on intestine, kidney,
bones...
to increase Ca availability
for bone mineralization
and remodeling
AS A VIT BC:
It is essential in the diet
performs a specific function
absence results in
deficiency
We can’t synthesize as much
as we need
Vitamin is activated to a
hormone
what are some factors the reduce how much vit D your body makes?
Limited sun exposure
Sunscreen use Or little skin exposure to sun
Living at a high latitude (most of Canada)
Staying indoors
Cloud cover, smog
Dark skin: people with darker skin absorb less of the sun's ultraviolet
rays
Age, especially if >65y…
Digestion issues – eg: Crohn's or celiac disease, bariatric surgery
Liver and kidney disease
what is vit D deficiency vs toxicity symptoms?
Deficiency:
- Abnormal bone growth (rickets in children;
osteomalacia or osteoporosis in adults)
- Malformed teeth
- Muscle spasms
Toxicity:
- Elevated blood calcium
- Calcification of soft tissues
- Excessive thirst
- Headache
- Nausea
- Weakness

what are some vit D sources
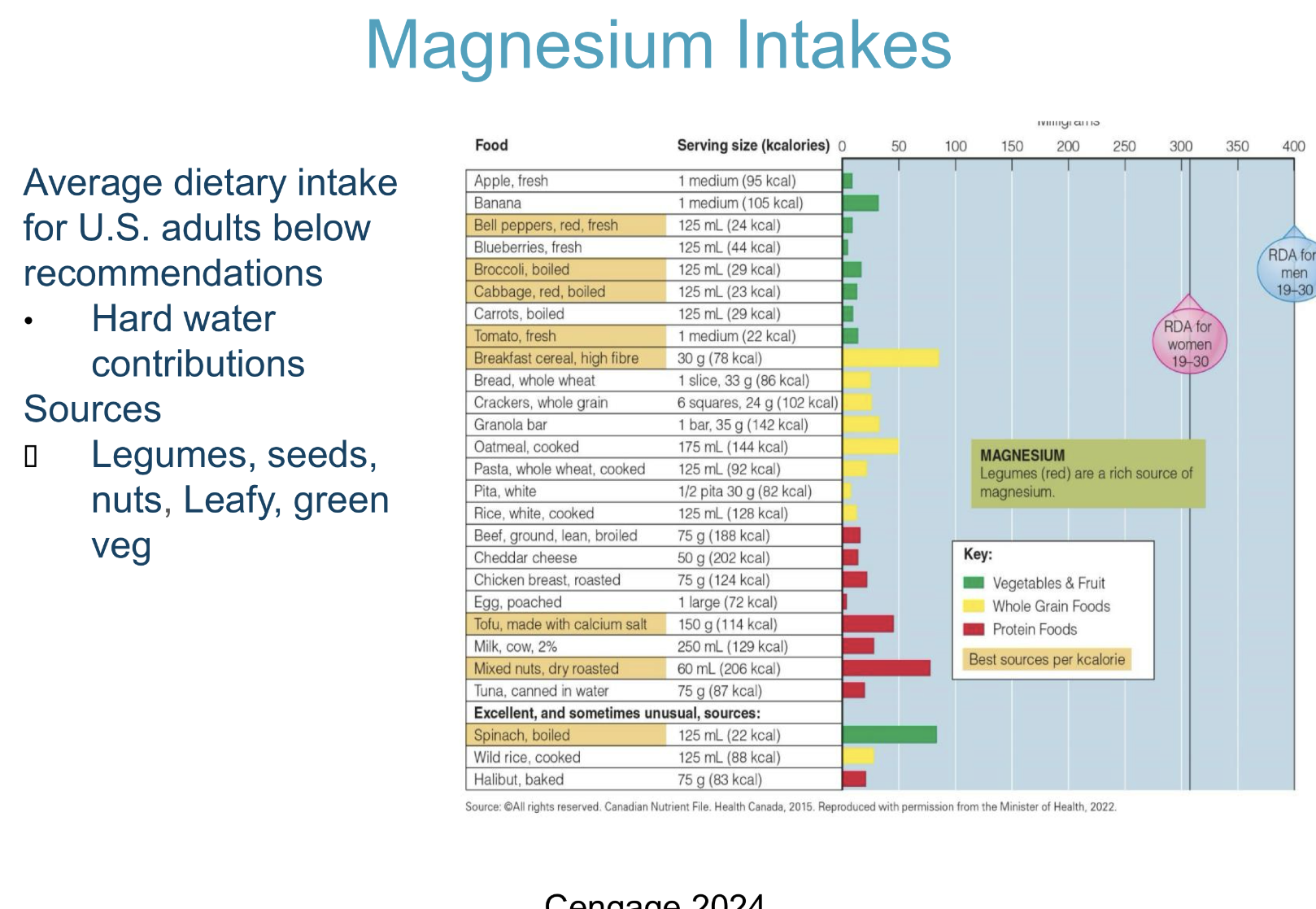
magnesium: storage, roes, UL?
more then ½ Mg storage = in bones, as a reservoir to ensure normal blond conc.
ROLES:
Maintains bone health
Energy metabolism and ATP production
Inhibits muscle contraction and blood clotting
Blood pressure – dietary intake protective, Critical to heart function
Supports normal function of immune system
Deficiency rare – d/t inadequate intakes
Impairs central nervous system activity, circulatory system
UL: 350 mg ….for supplements not foods