Airway
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
Why are unconscious patients more likely to have a compromised airway?
The pharyngeal muscles that usually maintain the airway relax, and the soft tissue of the airway can obstruct itself.
Neutral Position
Used for the initial assessment and management of the airway and in patients with cervical spinal injury. It maintains the neutral anatomical alignment of the spinal column, but is not optimal for airway patency. Supine with earlob aligned with mid-clavice.
Sniffing Positon
Used in patients who require airway management. It optimises airway patency, and is the best anatomical position for insertion of sugraglottic airways. Not appropriate for spinally immobilised patients. External auditory meatus in line with sternum
Lateral position
Patients who are altered conscious, not requiring active airway management. (Arm across chest, roll onto side, and support with knee + blanket under head.)
Neutral Position Adjustments for Paeds
Elevation under thoracic vertebrae to achieve neutral position due to prominent occipitus and short necks.
Triple Airway Manouver
Place either hands on the side of the head and tilt back (head tilt), place fingers behind the mandibular angle and thumbs on the chin lift the jaw upwards (Jaw thrust) and use both thumbs to open mouth to visualise the oropharnyx.
Laryngoscopy Indis, Contras and Equip
ACS requiring airway inspection, no contras, largyngoscope.
How to measure largynscope blade
From the upper incisor to the angle of the mandible
How to use a largynscope
Left hand, insert on patients right side and sweep the tounge to the left. You want to aim to visualise the epiglottis. Once you can see it, exert a lifitng force to expose the vocal chords.
4 Steps to Manual Airway Clearance
Position patient, Check mouth, Position the head (3AM) and check breathing
Nasopharyngeal Airway Indis, Contras and Precs
Supports airway patency in unconscious patient, good for trismus/gag reflex or oral trauma patients. No contras. Precautious of facial fractur or basal skull fracture, as well as TBI/nTBI and CSF leak
How to measure NPA
corner of nose to earlobe & diameter
Oropharyngeal Airway Indis, Contras and Precs
Support airway patency in unconsious patients & good as a bite block. Cant use on trismus patients, gag reflex or TBI/NTBI. No precs.
How to measure OPA
Angle of the jaw to middle incisor
Why do you not need to rotate an OPA in paeds patients?
They have softer palates that can be damaged from that kind of insertion.
How to use Magill’s foreceps
Inspect upper airway with laryngoscope
Prepare foreceps for foriegn body removal - grip with thumb and ring finger
Run the foreceps along the curve of the larygnoscope blade while maintaing view, and advance to the body
Open tips and grip the body, removing it gently
Re-inspect airway
Suction Indis, Contras and Precs
Indicated for suspected fluid obstruction in airway or airway device. No contras. Be cautious of hitting the epiglottis, as it can stimulate it and cause airway obstruction, and be careful when using for croup.
Yankauer Suction
Rigid catheter for suction of visible sectetions, small holes to reduce trauma, can be turned on or off by occluding the control port. Best used for visible secretions or fluids in oropharnyx or nostrils
Y - Suction
Soft cthetar used for suctioning small spaces where fluids are not directly visualised, on/off using control port. Best used for ETT, NPA, stoma and oropharngeal suction in neonates.
Regular Suction Steps
Open package, only exposing connection port and connect it to the suction device via tubing, ensuring the connection is firm.
Turn on the suction, and insert it carefully as to not stimulate the gag reflex
Occlude port to allow for suction of the airway. Avoid delicate structures, and do not use suction for more than 10 seconds at a time.
Turn off when not required.
Airway Stoma Suction Steps
Pre-oxygenate the patient, and remove the stoma cap/HME filter. Use a 10- 12FG catheter.
Select insertion depth - should be the length of tracheostomy/stoma tube if there is a spare tube, if not it must be >10cm to ensure the obstruction is cleared
Connect the port to catheter, ensuring the connection is firm
Change gloves for the sterile tip of the catheter, and turn on suction.
Hold the catheter at 15xm from the tip, inserting it 10cm. If the patient coughs, withdraw a little
Occlude the port while gently withdrawing the catheter, slowly rotating clockwise to clear the length of the tube.
SGA Indis, Contras and Precs
Supra-Glottic Airway. Indicated if patient is unconcious no gag reflex and not breathing normally/can’t maintain their own airway, cant be ventilated effectivley with just the BVM, needs 10+ mins and cant be intubated. Do not use on patients with a gag reflex, strong jaw/trismus or suspected epiglottitis or upper airway obstruction. Be cautious if sniffing position cannot be achieved, if there is vomit in the airway, or enlarged tonsils in paeds or pt’s who need high airway pressures.
How to insert SGA
Position the patient per CWI 190 (sniffing)
Select i-gel size according to patient weight
Put lube into the frame, and use that to smear it onto the back and sides of the i-gel.
Insert into mouth, aiming towards the hard palate gliding down until resistance is felt. Teeth should align with black marker.
SGA weights (+ GT)
2-5kg = 1.0 10
5-12kg = 1.5 12
10-25kg = 2.0 12
25-35kg = 2.5 12
30-60kg = 3.0 12
50-90kg = 4.0 12
90kg + = 5.0 14
SGA troubleshooting
Anticlockwise/Clockwise rotation of the i-gel along the long axis while extering downwards pressure, or thrust jaw while re-inserting. Bigger or smaller gel.
SGA > NG tube sizes
1 - N/A
1.5 - 10
2 - 12
2.5 - 12
3 - 12
4 - 12
5 - 14
How to measure NG tube
Measure from xiphisternum to earlobe to gastric insertion hole, and mark with tape.
How to use NG tube
Insert using lube, and then attack 50ml syringe. Inject 20ml of air, and confirm bubbling. Withdraw stomach contents and kink once it is at the top, attaching to drainage bag and securing to the face with tape. (If after 100-150ml of air nothing comes up, remove tube & reattempt)
Choking flowchart
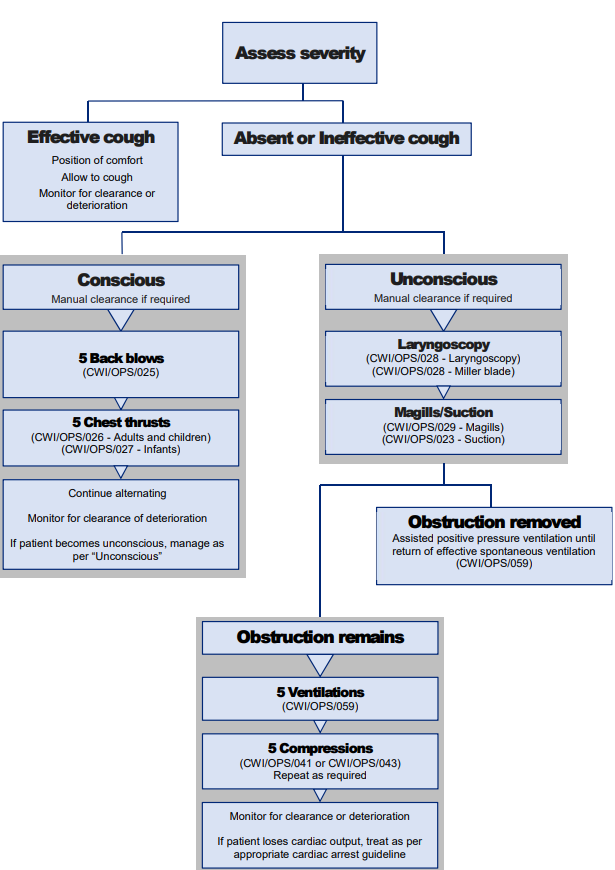
Choking with effective cough instructions
Allow the patient to choose preferred position, and encourage them to cough. Monitor for the removal of obstruction.
Conscious with absent or ineffective cough instructions
Visualise airway, if the obstruction is visible position the patient’s head low and manually clear the airway.
Obstruction remains but conscious (Back Blows) instructions
If obsruction remains post coughing, deliver up to 5 back blows and monitor for removal of obstruction.
Obstruction remains but conscious (Chest Thrusts) instructions
If obstruction remains, adminsiter up to 5 chest thrusts, monitor for removal of the obstruction
Unconscious choking WITH cardiac output instructions
Position patient supine, in sniffing position. Inspect airway, and if body is visible, position laterally and remove it manually.
If not visualised, inspect using laryngyscope and remove with suction or foreceps, giving positive pressure ventilation until spontaneous ventilation returns.
What does an SGA do?
Provides improved airway and ventilation management compared to bag-valve-mask and OPA.
Upper Airway Anatomy
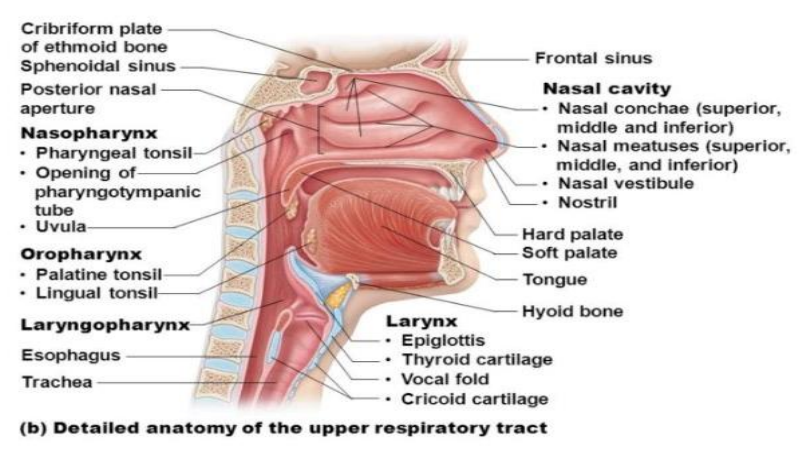
Pharnyx
Muscular tube lined with mucous membrane from the beginning of the esophagus up to the base of the skull. Communicates with posterior nares & acts as a passageway for food, air and as a resonating chamber.
Regions & order (top to bottom) of the Pharynges
Nasopharynx, Oropharynx, Laryngopharynx.
Nasopharynx
Situated behind the nasal cavity above the soft palate. Communicates with the nasal cavities through the nasal conchae and the tympanic cavity through the eustachian tube.
Oropharynx
Encompassed by the soft palate above and the epiglottis below, communicates with the mouth through the oropharyngeal isthmus and contains the palatine tonsils.
Laryngopharynx
OR HYPOPHARNYX. Extends from the upper border of the epiglottis to the lower border of the cricoid cartilage. Contains piriform recesses in which swallowed foreign objects may lodge.
Differences in the Paediatric Larnyx
Higher and more anterior (sits at the level of the 2nd & 3rd cervical vertebrae instead of 6th-7th in adults.
Harder to visualise due to position
Tonsils can easily enlarge and obstruct the airway
Epiglottis
Spoon-shaped plate of elastic cartilage that lies behind the tongue and is visualised during laryngoscopy. It prevents aspiration by covering the glottis (opening of larynx) during swallowing.
What is the Vallecula?
A furrow/channel between the base of the tongue and the epiglottis. It has important implications for airway management - eg. no epiglottis = the blade isn’t in the vallecula. Advance further down the midline and control the tongue.
Tounge
Muscular organ that sits in the mouth, covered with mucosa (pink moist tissue) and tiny papillae & taste buds. Anchored to the mouth by webs of tough tissue & muscosa. Its front tether is the frenum, and it is anchored to the back of the mouth at the hyoid bone.
Trachea
Cartilaginous and soft. Subject to collapse and obstruction in paeds patients (kinking) and requires correct positioning to function correctly.
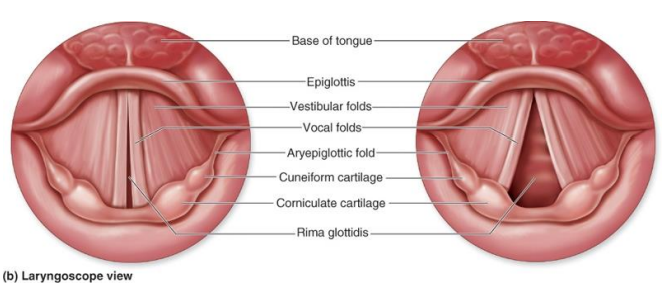
Vocal Folds
aka Vocal Chords. They are twin infoldings of mucous membranes that are stretched horizontally across the larynx. They vibrate and modulate the flow of air leaving the lungs during speech.
Anatomy of the Vocal Folds
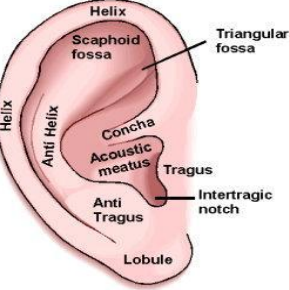
Anatomy of the Ear
Where is the suprasternal notch?
Midline, in between the clavicles
Mandible angle
Where the jaw juts outward from.
What are the external nares & occiput?
Nostrils, allow air in. Occiptal lobe, very back of the skull.
What is a gag reflex
Reflex contraction of the laryngopharynx. Can be evoked by touching the posterior roof of the oropharynx near the tonsils or the back of the pharynx. It’s mediated by the glossopharyngeal and the vagal nerves. It helps to prevent the lower airway from aspiration by expelling objects away from the trachea. Can result in gagging or vomiting.
When do patients start to lose gag reflex?
GCS 9
What does a gag reflex indicate?
A patients ability to protect their own airway.
Common Upper Airway Obstructions
Tounge, Foreign body, Laryngeal Spasm & Oedema, and Trauma.
UAO - Tounge
The tongue loses muscle tone when a patient falls unconscious, and so it falls posteriorly into the oropharynx or epiglottis.
UAO - Aspiration
Vomit in the upper airway and aspiration into the lungs
High risk choking patients & why
Elderly - weakened airway reflexes & muscle tone required to expel objects, neurological impairment (MS, Stroke etc..), and being on cough suppressants, poorly fitted dentures, sedatives etc..
Kids under 4 - smaller airways, easily obstructed, more likely to put shit in their mouth, swallowing mechanisms are less develiped, they cant easilt change body position or posture to clear obstruction.
UAO - Laryngeal Spasm
Involuntary spasm of the vocal cords reducing airflow
UAO - Laryngeal Oedema
Swelling in the larynx, usually caused by allergic reactions.
UAO - Trauma
Teeth, dentures, blood, etc..
Priorities in Emergency Airway Management
Early recognition & escalation.
Quick positioning of the patient
Generally fast care = less O2 loss
Why is positioning so important in unconscious patients?
Establishes and maintains a clear airway. It can help drain fluids out of the airway, keep tongue positioned correctly, etc..
Why is airway management important?
Essential step as it acheves oxygenation & ventilation. These two things prevent neurological dysfunction & death, as O2 is flowingg freely through the airway.
Neutral position in Adults
External auditory meatus in line with the mid-clavicle (/suprasternal notch). Usually put a towel under the ocuiput,
How to 3 airway manouvere?
Head tilt - tilt patient’s head slightly backward by pushing gently on the forehead.
Chin Lift - the other hand is placed on pt chin, and moved anteriorly to maintain an open airway
Jaw thrust - place hands on either side of pt’s face. Thumbs on the zygomtic arch, and fingers behind the mandibular angle. Thrust the jaw forwards from mandibular angle.
What is a Nasopharngeal Airway?
Soft flexible tube consisting of a flange, cannula, and bevel/tip that goes in through the nasal cavity.
NPA Advantages & Disadvantages
Tolerated better than OPA in semi-conc
Less likely to cause vomiting in pt’s with gag reflex
Able to be used in pt’s with trismus or dental trauma
Rapidly inserted
May cause nosebleed (epistaxis)
Smaller internal diameter than OPA
Difficult to suction
Does not isolate trachea
May obstruct post insertion
Difficult to insert if nasal trauma or deforminty
What do a battles sign & raccoon eyes indicate?
Both indicate basal skull fracture.
What is an OPA?
Oropharyngeal airway. Semi circular shaped airway made of hard plastic, inserted through the mouth and over the tounge. Blocks tounge from falling backwards. Made of the flange, body, tip and channel,
OPA Advantages & Disadvantages
Prevents tounge from falling backwards and occluding the airway
Hard plastic prevents teeth clenching
Larger diameter = better for oxygenation & suction
Must be measured correctly to avoid malfunction
What does an SGA do?
Forms a low-pressure seal around the posterior perimeter of the larynx and is positioned superior to the oesophageal sphincter that enables positive pressure ventilation.
SGA Advantages and Disadvantages
Provides an improved airway and ventilation Mx opposed to facemask & OPA/NPA
Lower risk of aspiration (3.5% instead of 12.4% with just BVM)
Can be inserted in the left or right lateral positon, or sitting
Insertion can fail and may require ongoing troubleshooting
Three attempts thats AT
Difficult to secure
Airway preparation gear
Standard precaustions, eyewear & clean gloves, facemask, positioning, suction, indis/contras, measure adjunct, lube, cleanliness of adjunct, correct insertion
Why are laryngoscopes used?
Enables best visualisation of oropharynx, maximised view of foriegn body or fluid.
How to measure laryngoscope blade?
Middle inscior to mandible angle.
What is a tracheostomy?
Surgical hole made in the trachea, where a tube is passed. Attached to a ventilation bag/machine, and is for long-term care. It bypasses upper obstructed airway, cleans secretions and provides safer & easier oxygen delivery to the lungs.