Renal regulation of potassium
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
17 Terms
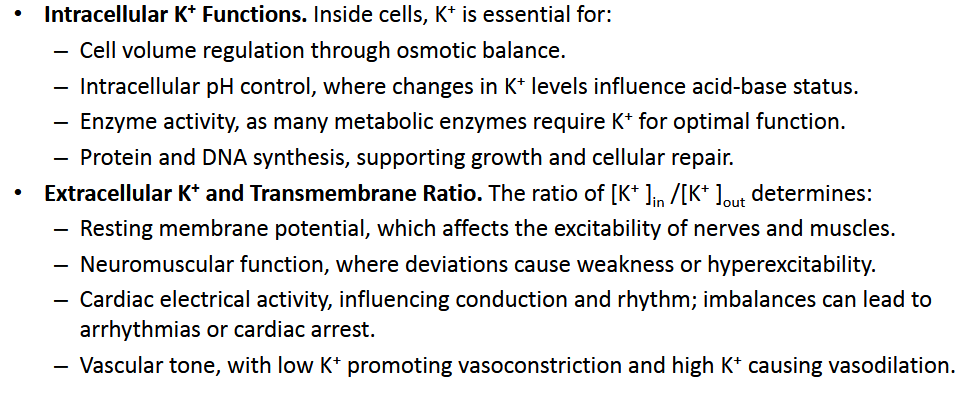
[REVIEW] Physiological role of intracellular and extracellular potassium
Describe the Two Regulatory Mechanism of K+
Cellular K⁺ uptake
Occurs within minutes after a meal.
K⁺ is rapidly shifted from the ECF into cells, reducing plasma K⁺ levels.
Renal excretion:
Occurs over hours.
Kidneys excrete excess K⁺ to maintain long-term balance
What is the normal range of Potassium in the Body? Distribution of ECF/ICF
Describe the Causes of Hypo/Hyper Kalemia
Describe how these factors can affect K+ levels:
Acid-Base Disorders
Plasma Osmolality
Cell Lysis/Vigorous exercise
Physiology of potassium balance:
Normal Level: 3.5–5.0 mEq/L
98% = ICF; 2% = ECF
Hypokalemia Causes:
Diuretic,
vomiting,
genetic defects in distal tubule Na⁺/Cl⁻ symporters
HyperKalemia:
Renal failure,
ACE inhibitors,
K⁺-sparing diuretics,
dietary K⁺ supplements
Modulating Factors:
Acid-Base Disorders:
Acidosis → ↑ plasma K⁺ (H⁺ “in”, K⁺ “out” of cells)
Alkalosis → ↓ plasma K
Plasma osmolality:
↑ osmolality → ↑ K⁺ efflux
Cell lysis & vigorous exercise → ↑ K⁺ plasma (due to the release of intracellular K⁺ )
Describe Cellular K+ Uptake:
Key transporters?
Hormonal Regulation
Systemic Coordination
Key Transporters:
Na⁺/K⁺-ATPase:
NKCC (Na⁺-K⁺-2Cl⁻ cotransporter):
Hormonal Regulation:
Insulin: Stimulates Na⁺/K⁺-ATPase activity and glucose uptake via GLUT4.
Catecholamines (e.g., epinephrine):
(β₂-AR) activate cAMP signaling, enhancing K⁺
uptake (reabsorption).α-AR inhibits insulin release, while β₂-AR stimulates insulin secretion.
Aldosterone: Binds MR → increasing Na⁺/K⁺-ATPase
expression.
Systemic Coordination:
Pancreas (β cells): Releases insulin in response to β₂-AR stimulation.
Adrenal gland: Produces aldosterone (cortex) and epinephrine (medulla) during acute changes in plasma K⁺
Describe the mechanism in which Acidosis causes Hyperkalemia
Mechanism:
Low pH → Inhibits Na/H Exchanger and Na/HCO3- Cotransporter → Reduced intracellular Na+ and High H+ inhibits Na/K ATPase and NKCC → Slows down K+ Uptake
Increased H+ Intracellular levels → Displaces K+ from its intracellular binding sites → promote K+ Exit

Describe how K+ Excretion Varies
Where is K+ Secreted?
K+ Excretion:
K+ depletion (~0%- 2%)
Normal K+ intake (15-80%)
Increased K+ intake (up to 150% of filtered load)
K+ Secretion:
DT/ Cortical CD: Principle Cells
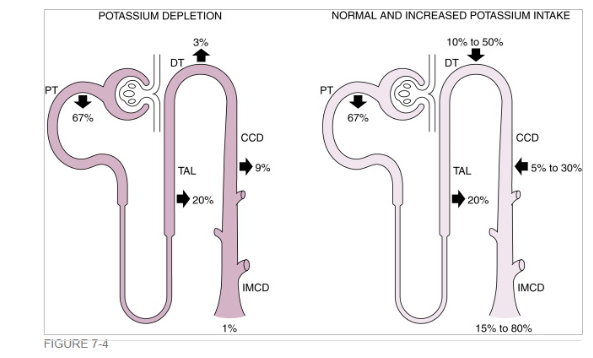
Draw out K+ Transport @ PT/ TAL
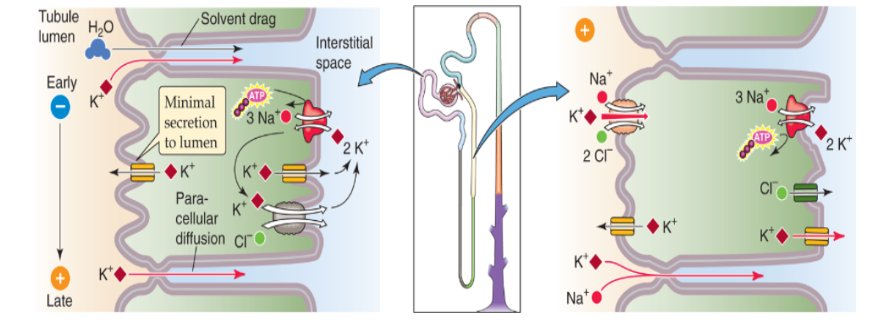
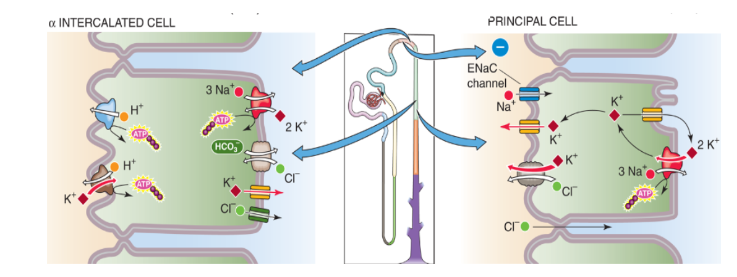
Describe K+ Transport in DT and CD
Alpha-intercalated cells
reabsorb K+/ Secrete H+
Activated by Low K+
Transporters: Via K,H ATPase and H-ATPase
Principal cells:
secrete K
Main Determinants = Na+ delivery to the DT→ Reabsorption via ENaC→ Electrochemical Gradient (More positive intracellular, less out, K+ leaves Cell)
Transporters: K,Cl-symporter, K- channels (multiple: ROMK and BK)
Describe Regulation of K + secretion by the distal tubules and collecting ducts
What are the Three mechanisms that governs K+ Secretion in DT/CCD
What physiological factors regulate K+ Excretion (4)
Pathophysiologic Factors?
The mechanism of K + secretion by the DT and CCD:
Na,K-ATPase activity and Na⁺ reabsorption:
Maintains intracellular [K⁺] → creates electrochemical gradient for K⁺ secretion
Electrochemical Gradient: Drives K⁺ movement through K⁺ channels and K⁺/Cl⁻ symporters
Apical membrane K⁺ permeability
ROMK (Renal Outer Medullary K⁺ channels)
BK ( (“Big” K channels, Ca²⁺-activated, “big” – large-conductance calcium-activated potassium channels)
Physiologic factors that regulate K excretion:
Plasma K⁺ concentration: Directly influences K⁺ secretion rate.
Aldosterone: Enhances Na⁺ reabsorption and K⁺ secretion.
Angiotensin II: Inhibits ROMK channel activity, decreases K⁺ secretion.
Arginine Vasopressin (AVP): Modulates water and electrolyte balance, indirectly affecting K⁺ excretion.
Pathophysiologic factors:
Flow rate of tubule fluid
Diuretics: loop (inhibitors of NKCC), thiazides (inhibitors of NaCl symporter), and osmotic diuretics stimulate K+
excretionAcid-base disorders.
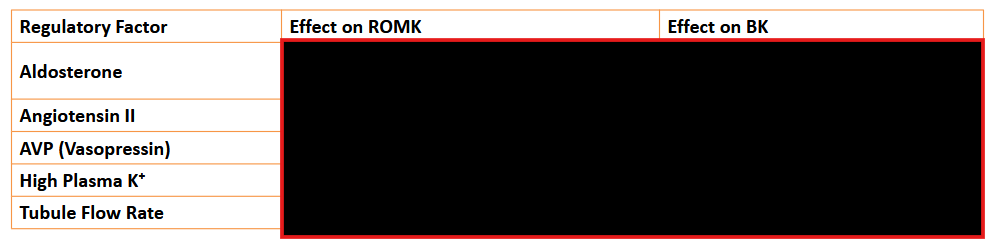
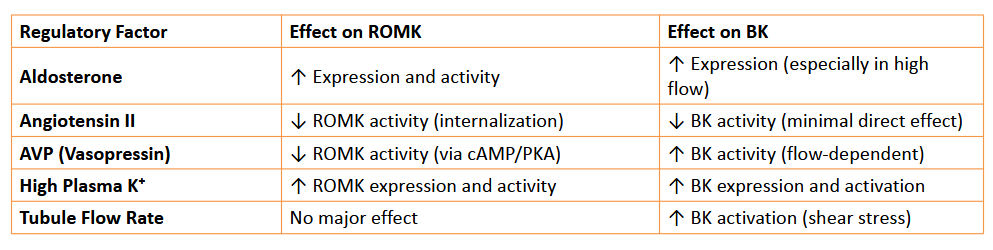
Differentiate between ROMK and BK
ROMK vs BK:
Both Secrete K+
Activation:
ROMK mediates routine K⁺ secretion,
BK channels are recruited during high K⁺ loads or increased flow states
Regulation:
ROMK:
Upregulation via aldosterone
inhibited by Ang II and AVP.
BK:
Strongly flow-dependent;
activated by high K⁺ and aldosterone.
High plasma K⁺: Stimulates both channels to enhance K⁺ secretion.
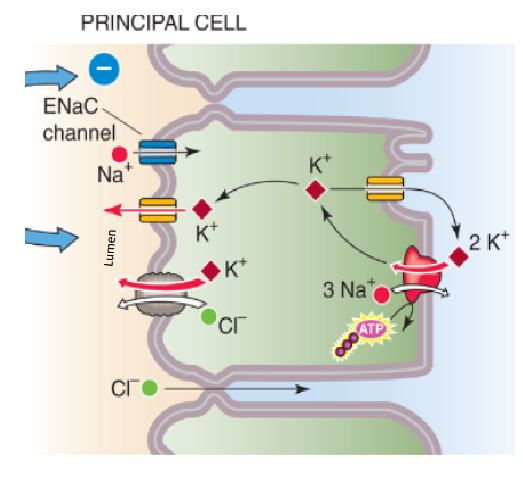
Describe how Na+ delivery to the principal cells regulates K+ secretion
Na⁺ Reabsorption: Na⁺ enters principal cells via ENaC channels, following its electrochemical gradient.
Na⁺/K⁺ ATPase: pump moves 3 Na⁺ out / 2 K⁺ in → maintaining low intracellular Na⁺ and high K⁺.
Electrochemical Gradient: This active transport creates positive Voltage inside Cell/ and Less Positive in Tubular Lumen
K⁺ Secretion: lumen-negative potential drives K⁺ efflux into the tubular fluid through apical K⁺ channels
Describe how High K+ Dietary Levels lead to Kidney Modification (increased K+ Excretion)
Mechanism in Late DT/Cortical CD
Supporting role in PT, TAL, DT
How does the Body sense High K+ levels?
Primary Site of Action of this modification (enhanced K+ Excretion): in Late DT/Cortical CD
Mechanism in Late DT/Cortical CD:
↑ Na⁺ reabsorption → electrochemical gradient → K⁺ secretion
High plasma K⁺ → aldosterone secretion, which:
Upregulates Na⁺/K⁺-ATPase
Increases ENaC channels \
Increases # of K⁺ channels for secretion.
↑ Tubular flow rate → detected by cilium in principal cells → ↑ intracellular [Ca + +] → opens BK channels
Supporting Role in PT, TAL, early DT:
High plasma K⁺ reduces Na⁺ reabsorption (=enhances Na+ reabsorption in DT/CD)
Mechanism on how K+ inhibits Na+ reabsorption:
Inhibition of Na⁺/H⁺ exchanger
Inhibition of NKCC
Chronic High K+ Intake:
decreased expression of Na⁺/H⁺ and NCC
K+ Detection: zona glomerulosa cells
have resting membrane potentials that are highly sensitive to extracellular K⁺
K+ Increases → Opens VG Ca++ channels → Aldosterone Release/Synthesis
What is the Effect of AVP on K+ secretion by the DT and CD
NET Effect: AVP does not change overall urinary K⁺ excretion (K⁺ secretion remains constant)
Stimulation of K+ Secretion:
increases Na⁺ conductance → depolarizes
apical membrane → ↑ driving force for K⁺ efflux.increases apical K⁺ permeability → ↑ K⁺ secretion.
Inhibition:
AVP reduces tubular fluid flow → ↓ K⁺ secretion

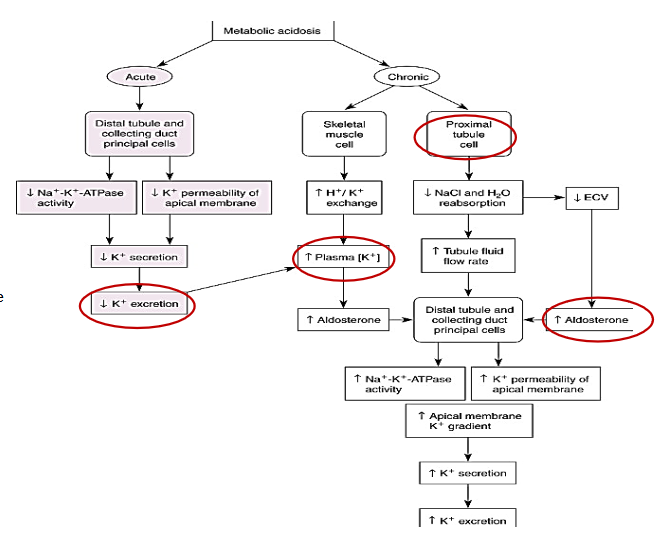
Compare the effects of Acute vs Chronic Acidosis on K+
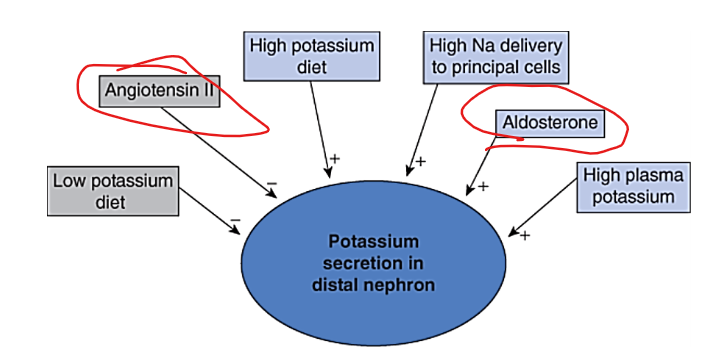
How do these factors impact K+ secretion in distal Nephron:
Low Potassium Diet
ANG II
High Potassium Diet
High Na+ Delivery to principal Cells
Aldosterone
High Plasma K+
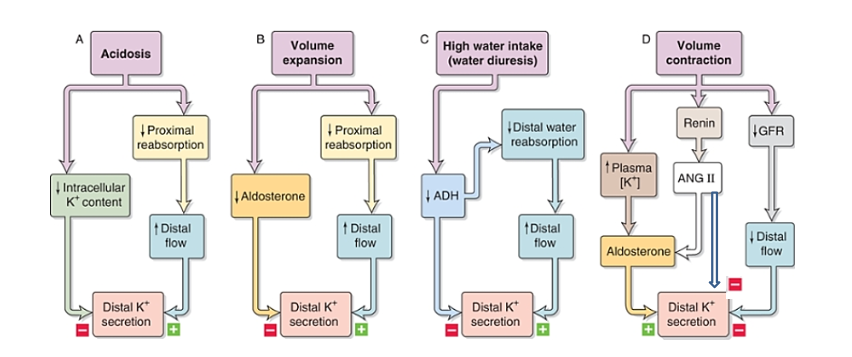
Describe how These conditions impact Distal K+ secretion (hint: all conditions increases/Decreases K+ Secretion):
Acidosis
Volume Expansion
High Water Intake (water diuresis)
Volume contraction