Build a Nephron: Proximal Tubule
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
What is Filtered Load and Excretion Rate and how does it relate to reabsorption/secretion
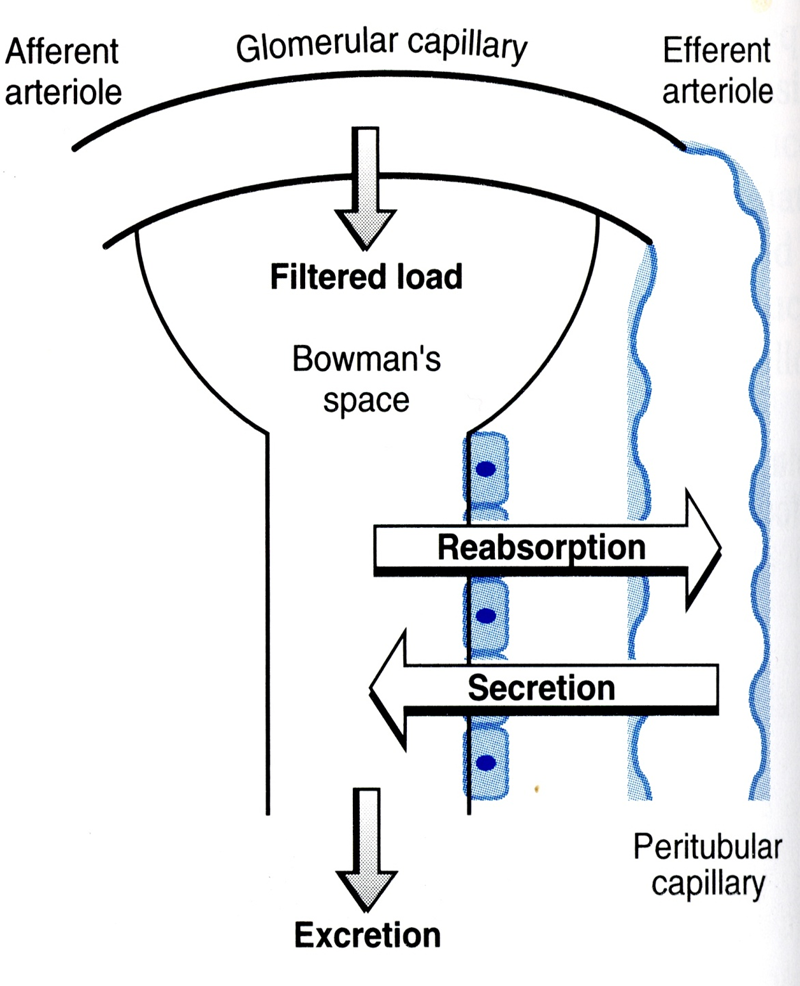
Filtered Load is the total amount of substance that is filtered into the renal tubules by the glomerulus
→ Glomerular Filtration Rate x Plasma Concentration of Substance
Excretion Rate is the total amount of substance that is excreted into urine per unit time
→ Urine Flow Rate x Urine Solute Concentration
If Filtered Load is greater than excretion rate, there is more reabsorption whereas if the opposite is true secretion is occurring
How would you measure GFR for a substance that is trapped in the tubule lumen?
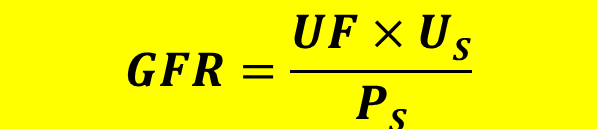
For a substance like Inulin that cannot be reabsorbed or secreted, filtered load is equivalent to excretion rate
1) Because of this you can calculate GFR or clearance based on the above equation
→ urine flow rate
→ urine solute concentration
→ plasma solute concentration
What is Clearance?
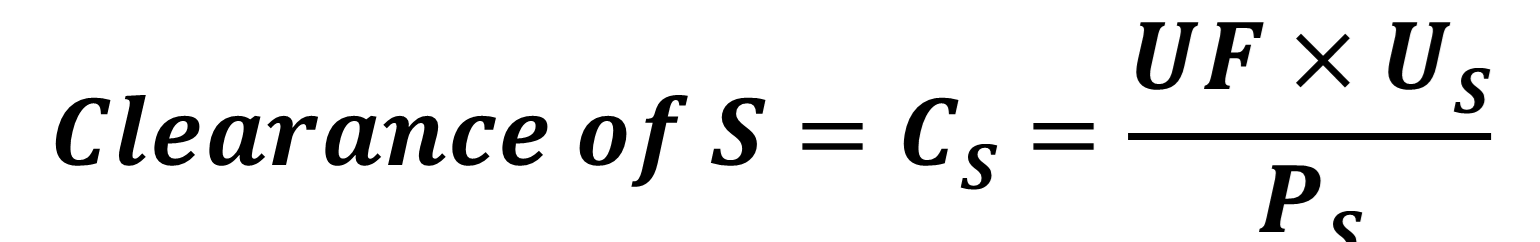
Clearance is the volume of plasma that is completely cleared of a substance by the kidney per unit of time and is a measure of renal function
→ urine flow rate
→ urine solute concentration
→ plasma solute concentration
Describe how the body maintains a constant excretion rate of creatinine
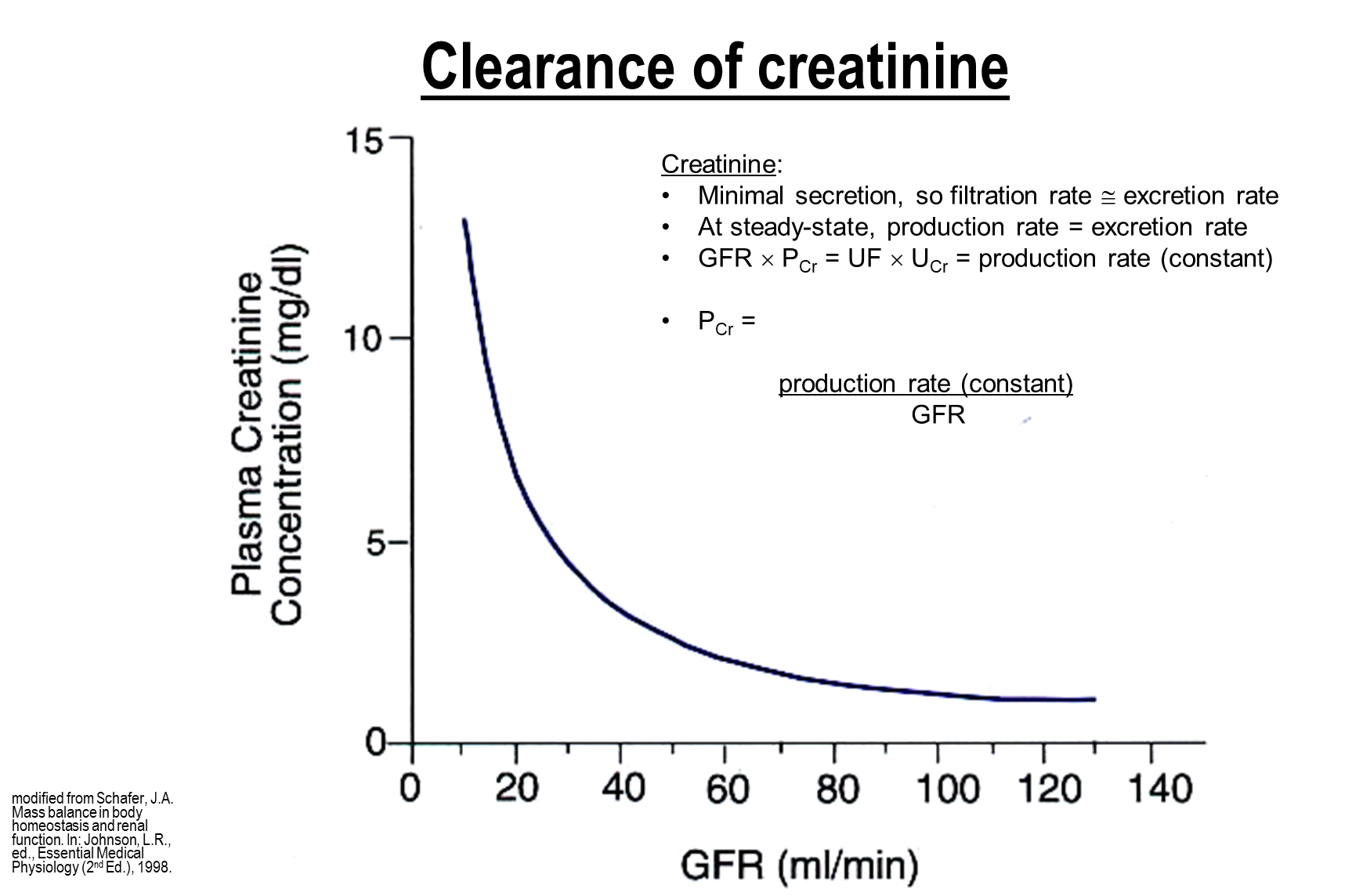
Creatinine is a metabolic byproduct without a dedicated feedback mechanism. Because of this the body aims to keep a constant excretion rate.
→ When the body experiences a decrease in GFR the body will adjust to this by increasing plasma creatinine in order to maintain a constant excretion rate
→ Because of this plasma creatinine can be identified by dividing production rate and GFR and these two factors are inversely related
→ so a halving of GFR would see a doubling of production rate
importantly creatinine buildup is not prevented by this mechanism, steady state is not an indication of normal levels
What is the structure of the proximal tubule cell?
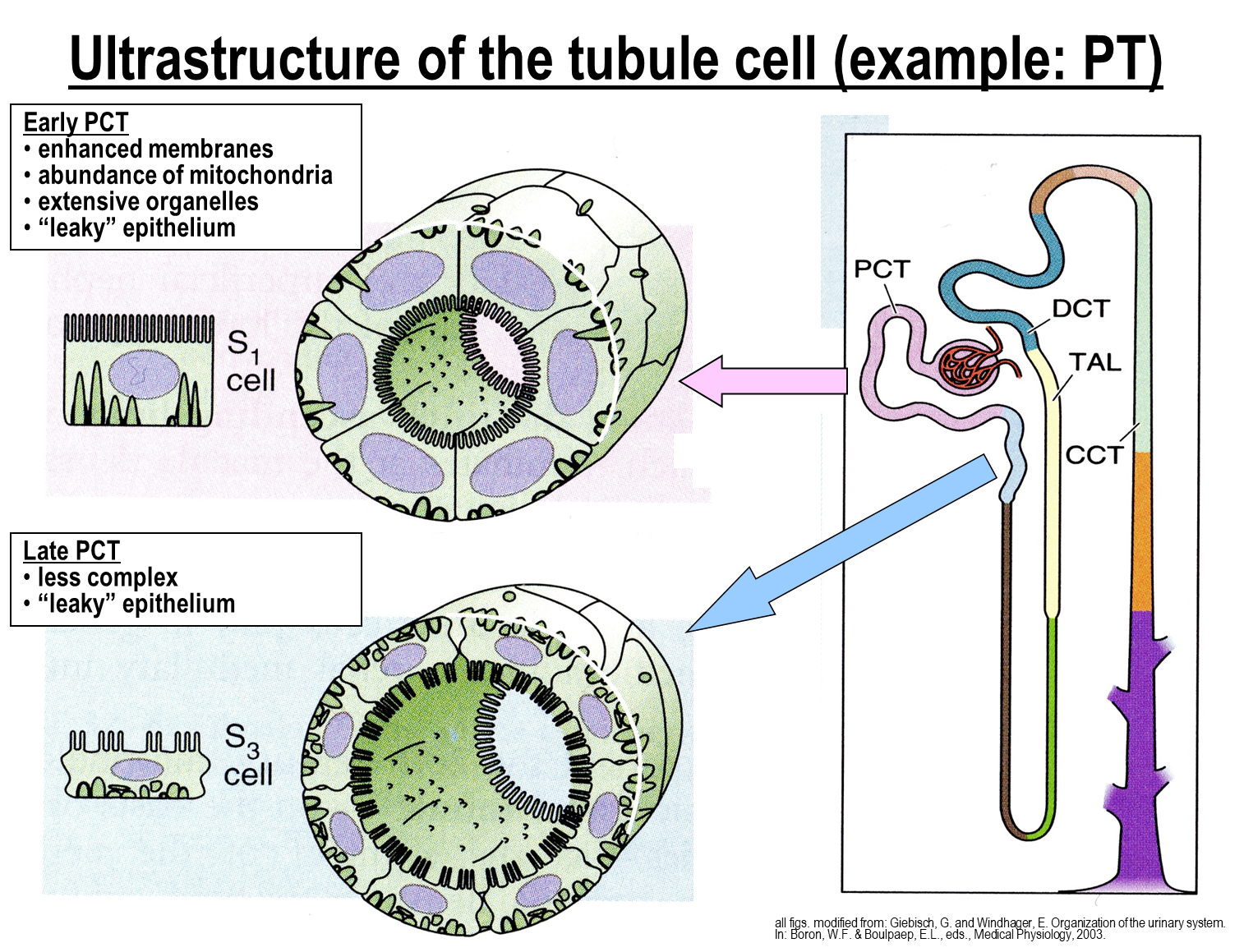
Proximal Tubule Cells are lined by cuboidal cells with microvilli that help to increase surface reabsorption
→ have high levels of mitochondria in order to meet the energy requirements
→ extensive organellar system for transport and protein synthesis
→ is a leaky epithelium allowing for better movement via the paracellular route
What are the important kinetic properties of transporters?
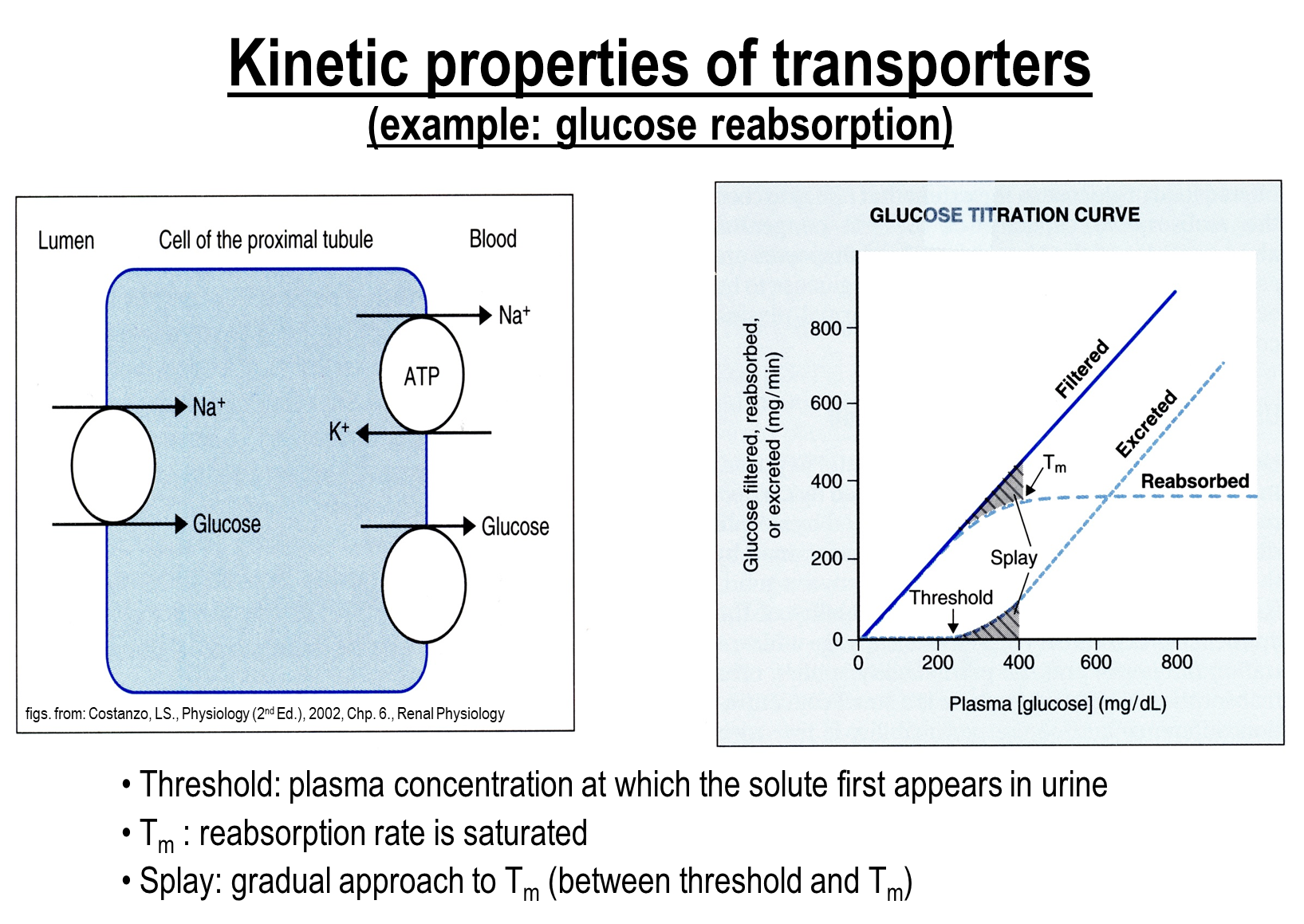
When you plot the filtered load, excretion rate, and the reabsorption rate you can identify several things
1) Threshold
→ plasma concentration at which the solute first appears in the urine
2) Transport Maximum
→ the point where the reabsorption rate is saturated
→ an increase in solute further than this point will not see an increase in reabsorption rate
What solute is reabsorbed the most at the proximal tubule?
The proximal tubule is the major area where reabsorption occurs in the nephron
1) The majority of sodium, chloride, and water reabsorption is performed at the proximal tubule (2/3rds)
What are the sodium transporters found on the early proximal tubule?
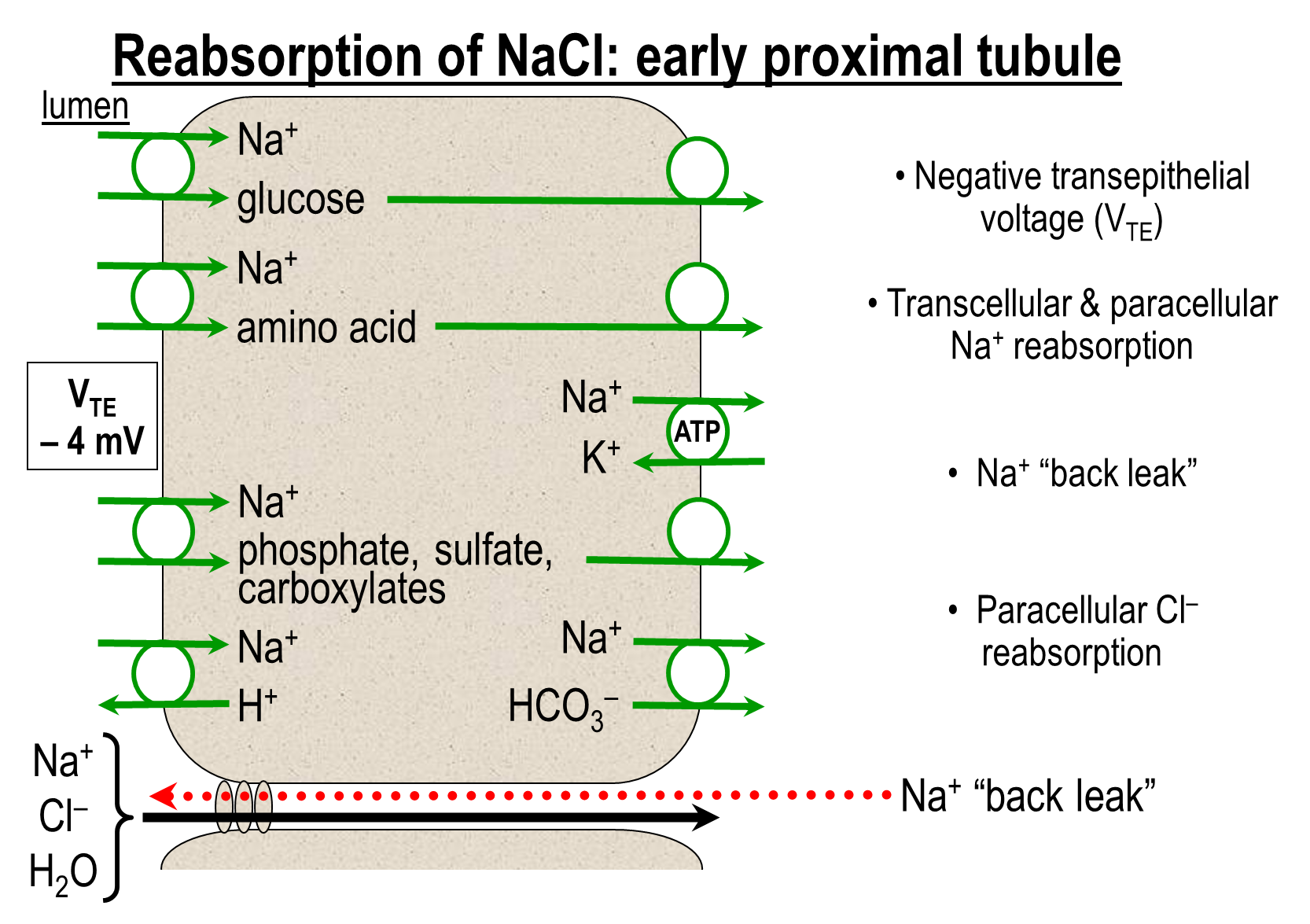
On the apical surface, sodium is reabsorbed from three major transporters. There is also paracellular transport as well
1) Sodium Glucose Transporters
2) Sodium Amino Acid Transporters
3) Sodium Hydrogen Exchanger
4) Various other sodium absorbers coupled to other solutes
On the basolateral surface sodium is pumped out of the cell via two major mechanism
1) Sodium Potassium ATPase
2) Sodium Bicarbonate cotransporter
the presence of sodium amino acid cotransporters creates a slightly negative transepithelial potential
→ this also results in sodium getting pulled back into the lumen
What transport is done at the late proximal tubule?
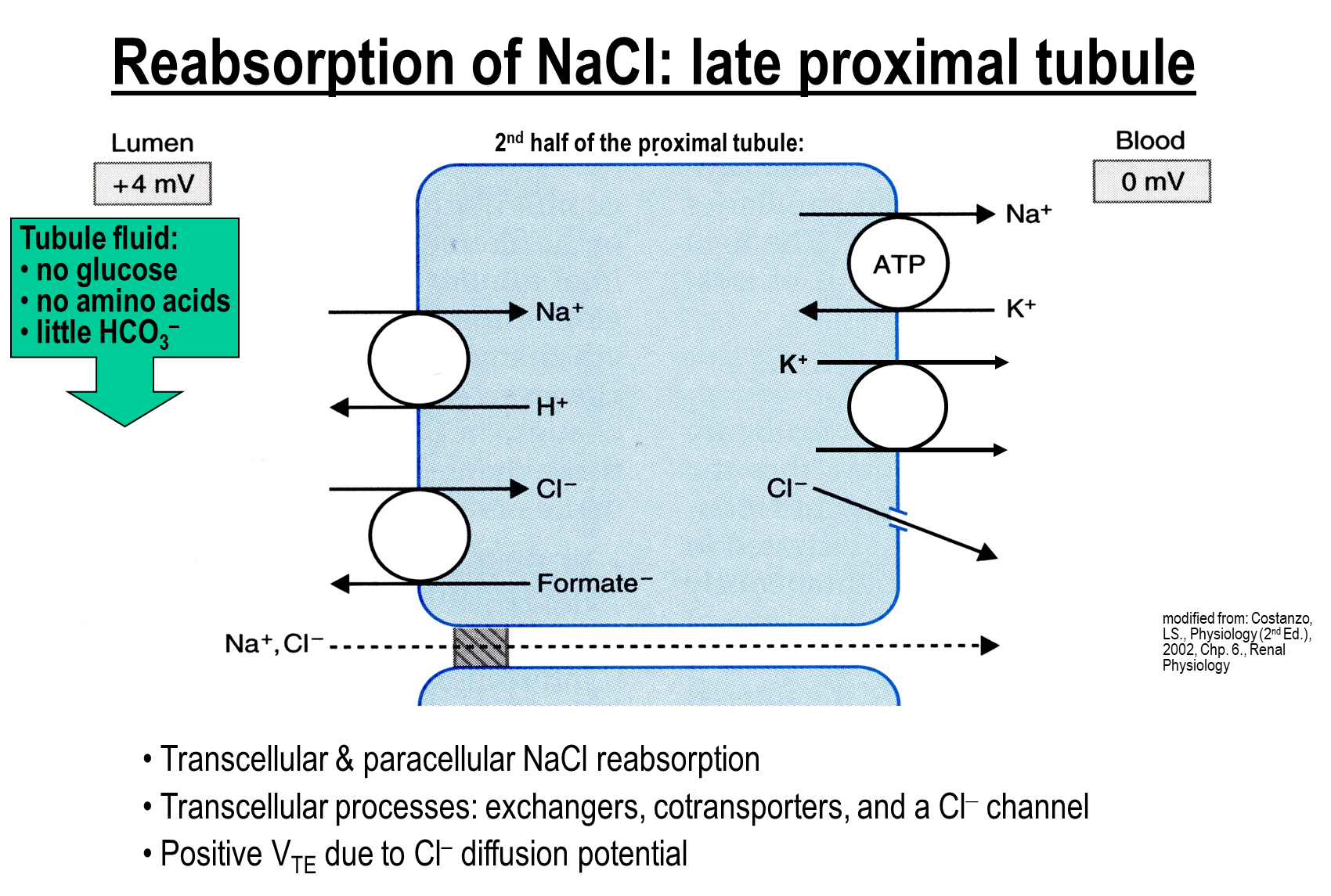
1) Chloride concentration is elevated in the late proximal tubule allowing for movement of chloride through the paracellular route
→ sodium and chloride move through the transcellular route in such large quantities creating a positive transepithelial potential
2) Apical Transporters such as the two below will move sodium and chloride in and transporters on the basolateral surface will move these ions across transcellularly
→ Sodium Hydrogen Exchanger
→ Chloride Anion Exchanger
What is Isosmotic Reabsorption?
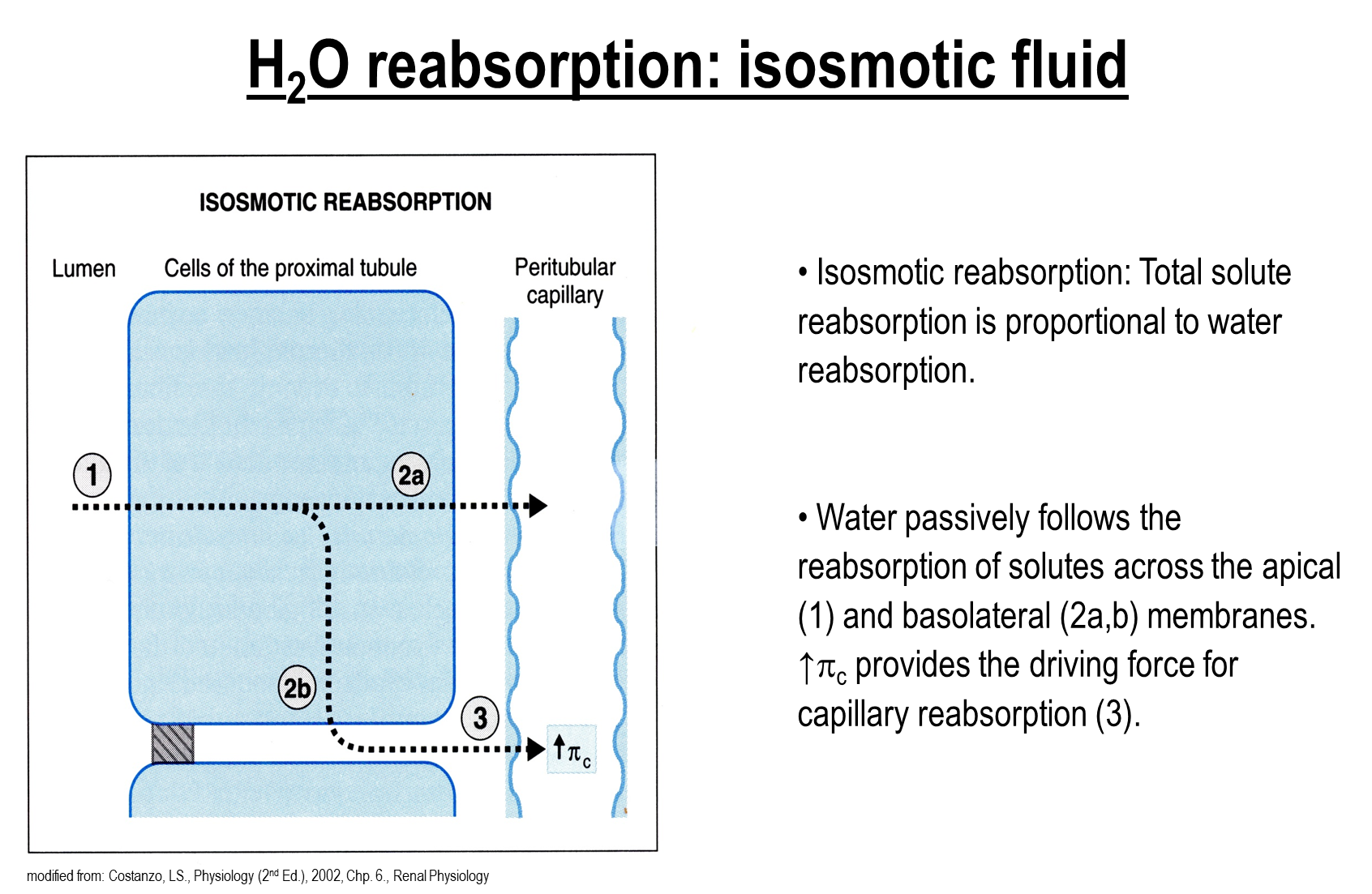
Isosmotic Reabsorption is the process where the total solute being reabsorbed is proportional to the water being reabsorbed
→ this process occurs in the proximal tubules, meaning that the resulting osmolality in the tubule fluid remains the same
→ this occurs because water passively follows solute across the apical and basolateral membranes and is absorbed into the peritubular capillaries due to an increase in colloid osmotic pressure
How does Glomerulotubular Balance work?
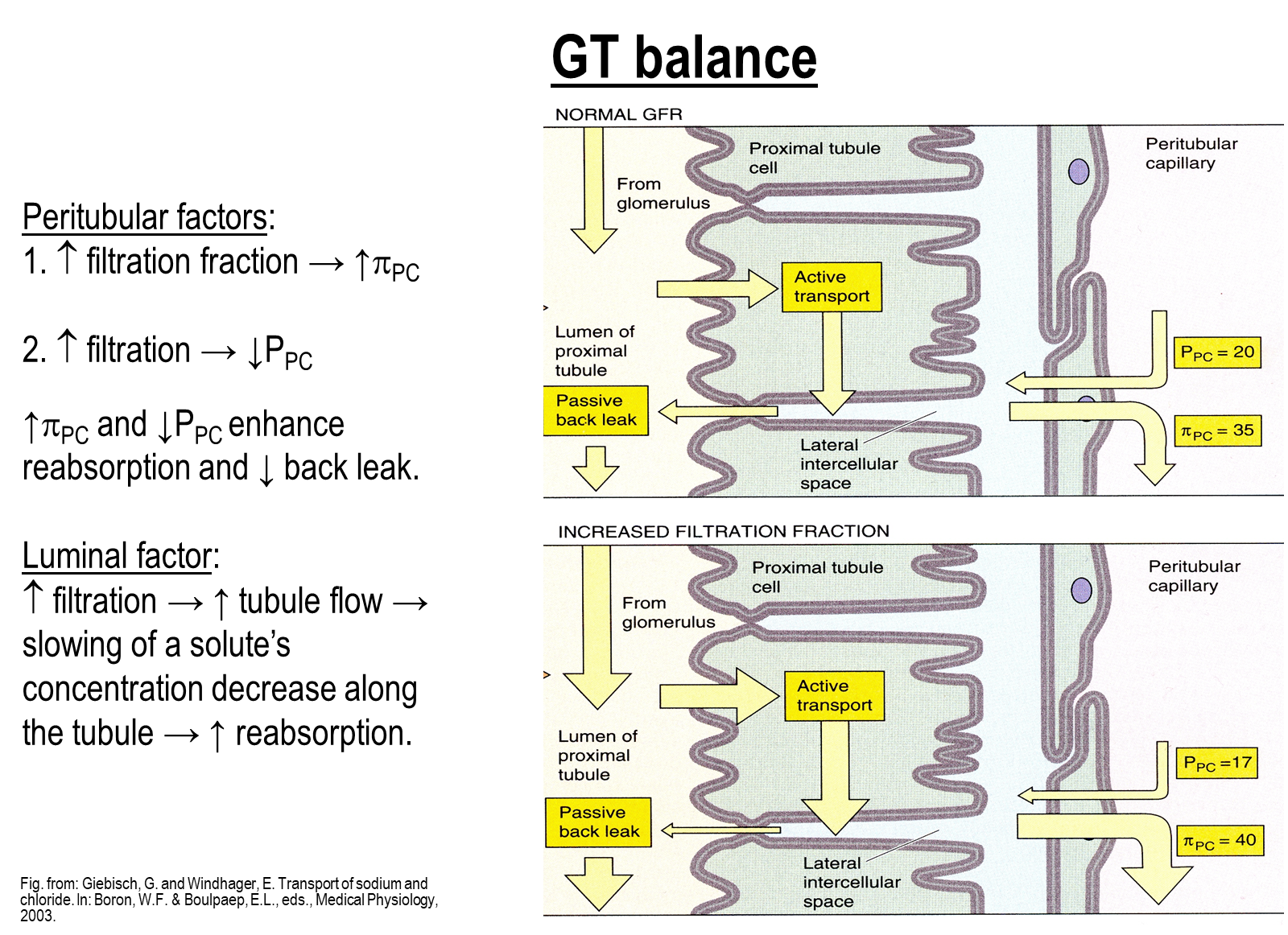
Glomerulotubular Balance allows for a proportional increase in reabsorption where filtration increasesIn will work by changing peritubular factors and luminal factors
1) When you increase the filtration fraction as a result of increasing hydrostatic pressure in the glomerulus this will cause a downstream decrease in hydrostatic pressure and increase in oncotic pressure in the peritubular capillaries
→ decreased hydrostatic pressure occurs downstream of an increased glomerulus hydrostatic pressure due to constriction of efferent arterioles
→ increased oncotic pressure occurs due more fluid being absorbed and the same amount of proteins being left behind
2) Increasing filtration will increase tubule flow leads to slower decrease in concentration of a solute along the tubule
→ this means that more distal portions of the proximal tubule will see a larger concentration and transporters on distal portions are activated at higher levels
Where are metabolic products reabsorbed in the nephron
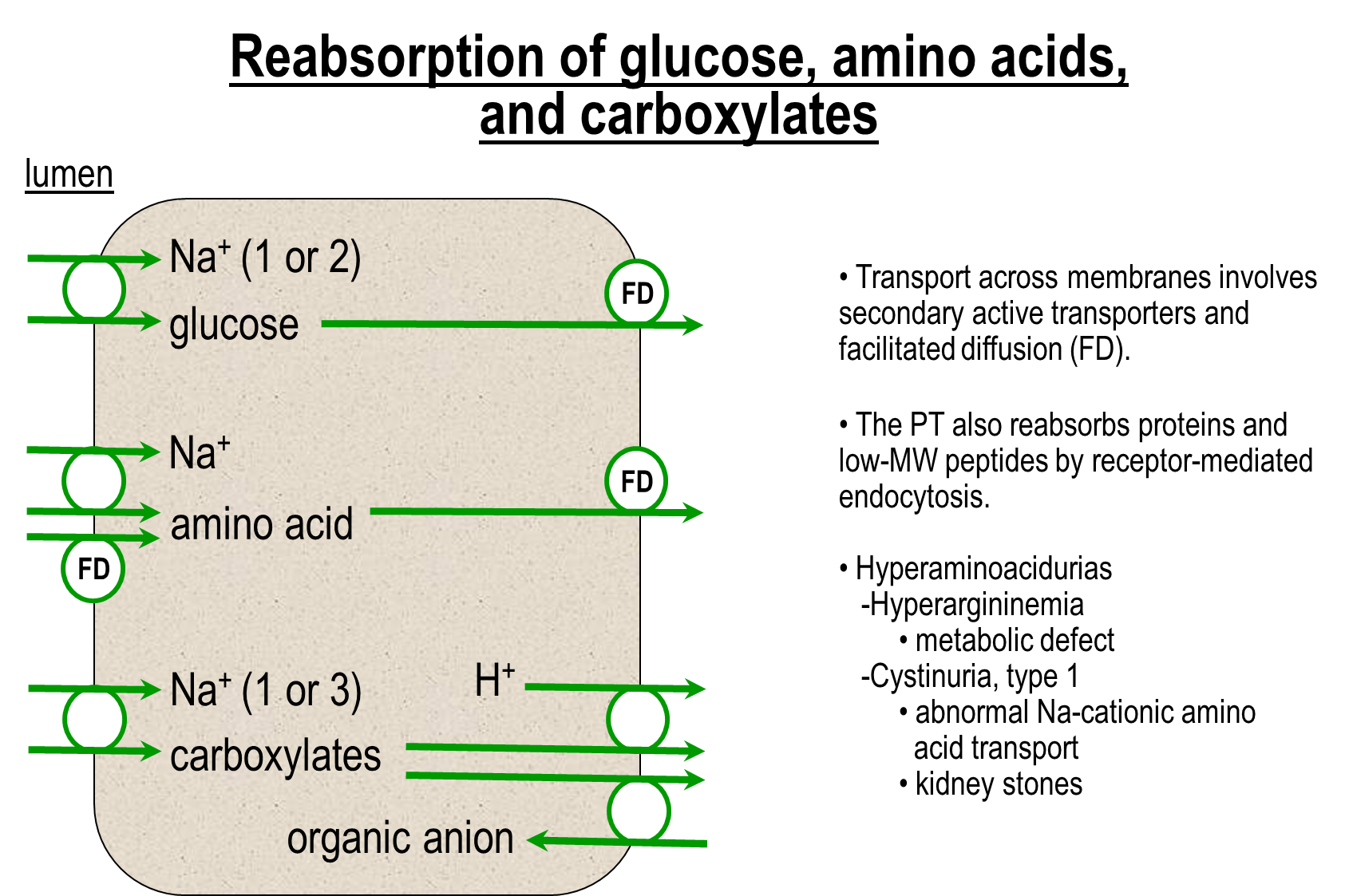
Metabolic products such as glucose, carboxylates and amino acids are nearly all absorbed at the proximal tubule. The majority of these are coupled to sodium movement
1) Apical Transporters
→ sodium coupled glucose, amino acids, and carboxylates
→ proximal tubule also reabsorbs proteins and low molecular weight peptides by receptor mediated endocytosis
2) Basolateral Side
→ transport across membrane involves secondary active transporters and facilitated diffusion
Where does the reabsorption of potassium occur?
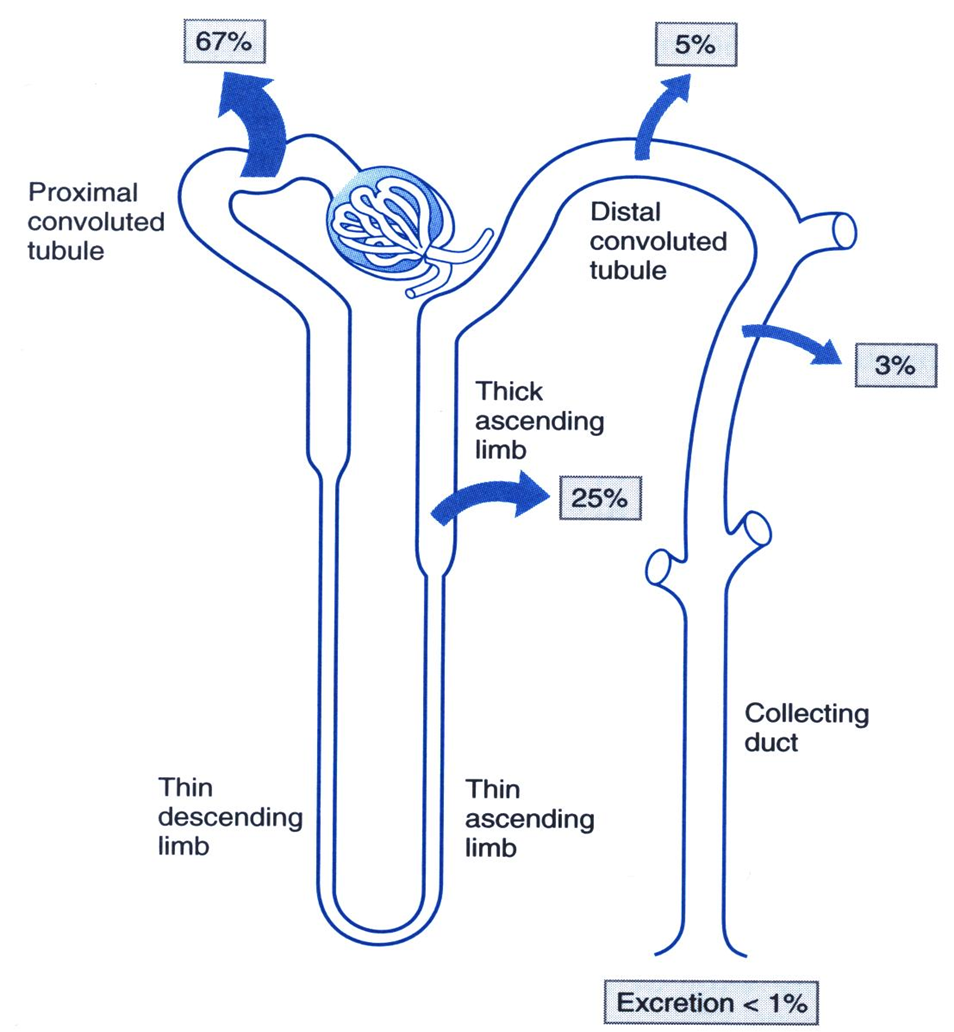
The majority of potassium reabsorption is done at the proximal convoluted tubule, with the rest of it being mostly done at the thick ascending limb
How does reabsorption of potassium occur in the early proximal tubule?
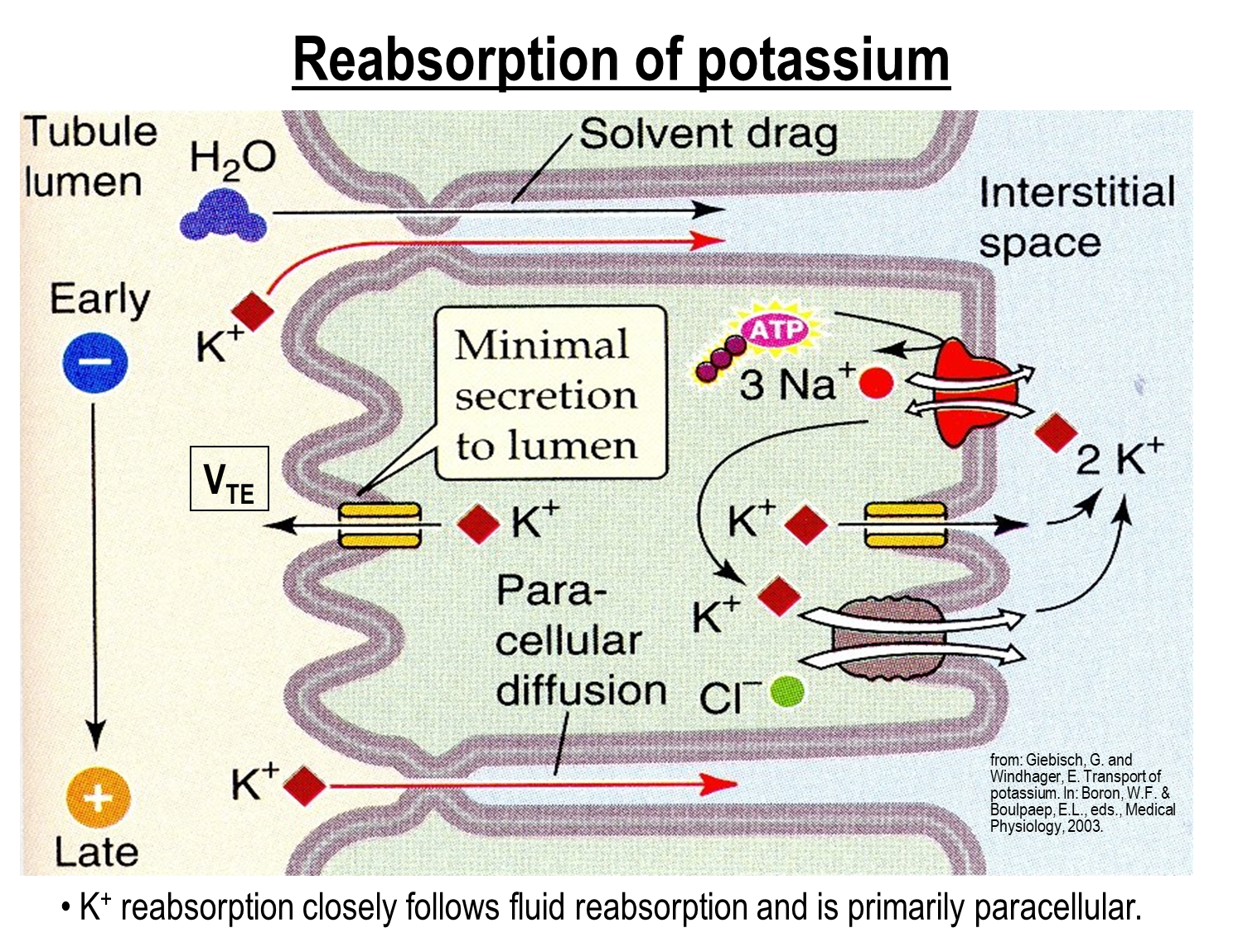
At the early proximal tubule, the majority of potassium is absorbed here and is done via the paracellular route
1) There is also small amounts of potassium secretion into the lumen as well
Where does the majority of calcium reabsorption take place?
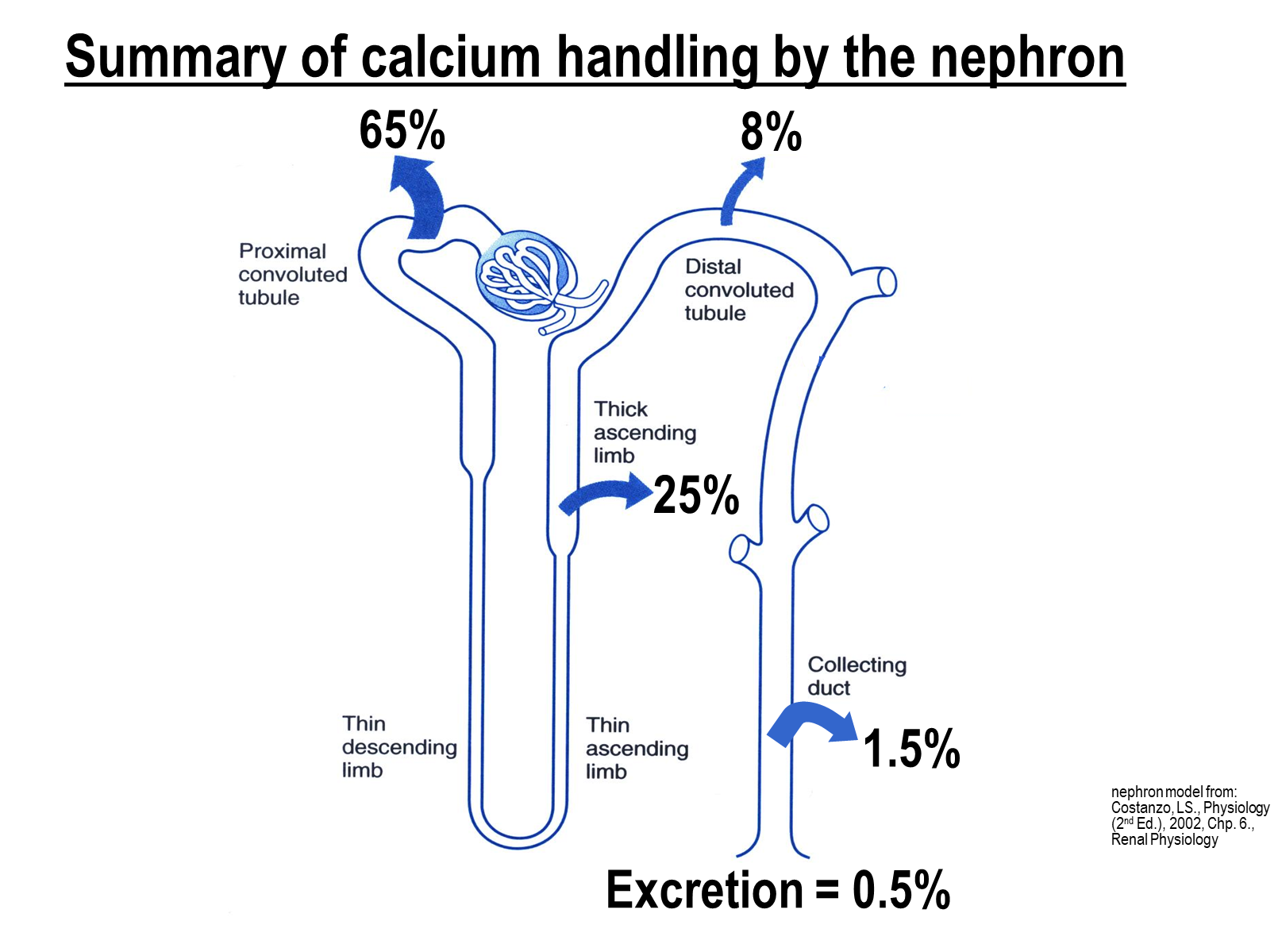
The majority of calcium reabsorption is done by the proximal tubule
→ the thick ascending limb contributes around 25%
→ the distal convoluted tubule contributes around 8%
Where does the majority of magnesium reabsorption take place?
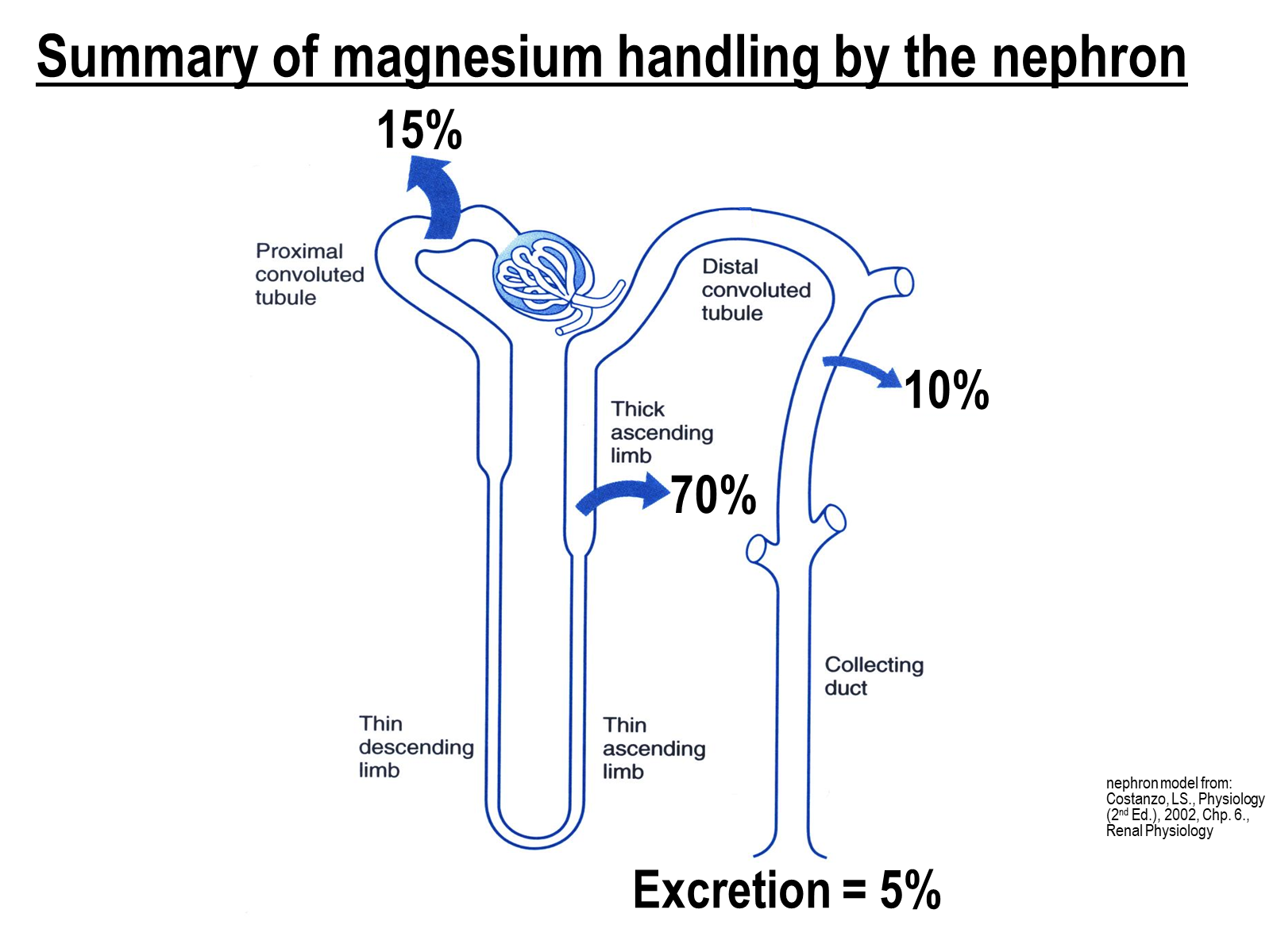
The majority of magnesium reabsorption is done at the thick ascending limb of the loop of Henle
→ the other 15 percent and 10 percent respectively is done by the PCT and DCT
What is the mechanism for calcium and magnesium reabsorption at the PCT?
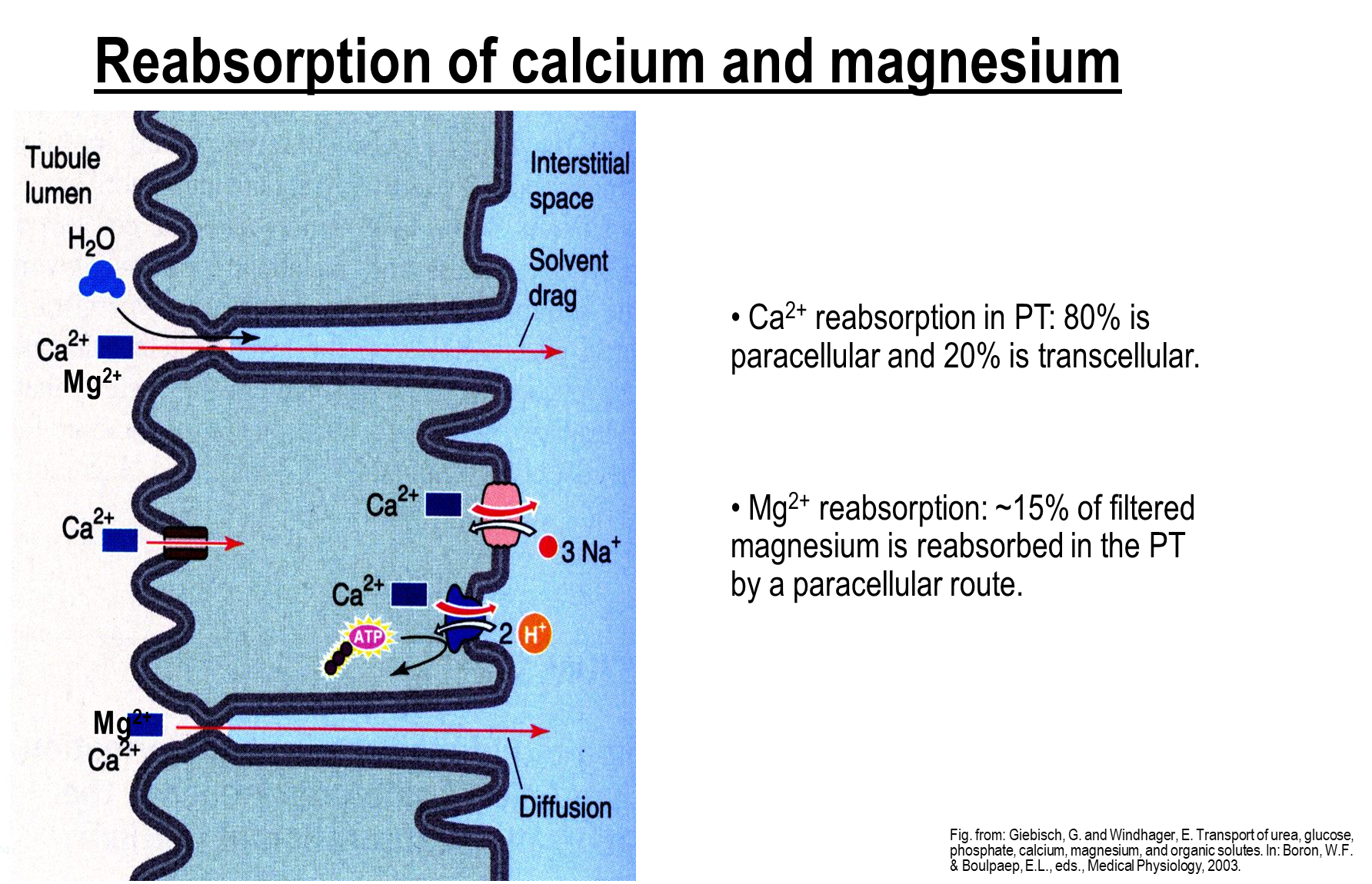
Similar to potassium, calcium and magnesium reabsorption is done via the paracellular route.
There are three proteins that are involved in transcellular reabsorption of calcium movement as well
→ Calcium Channel on the apical surface takes up calcium
→ Sodium calcium exchanger on the basolateral surface
→ Calcium proton exchanger
What is the mechanism for phosphate reabsorption at the PCT?
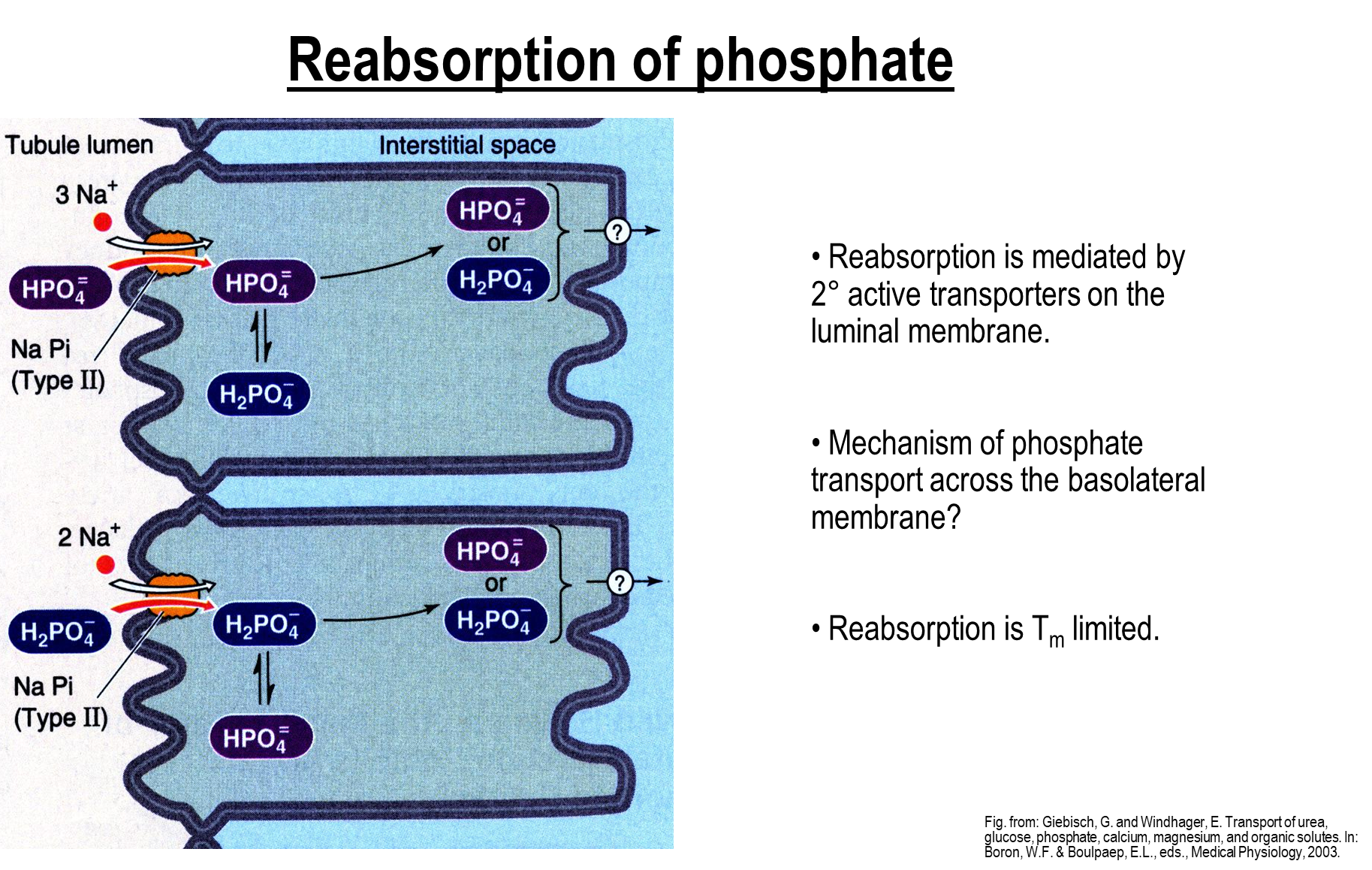
The majority of phosphate handling is done by the proximal convoluted tubule, with the other 10 percent being reabsorbed by the DCT
1) the remaining ten percent is excreted in urine since phosphate acts as a urine buffer
→ reabsorption is transport limited, meaning it is rapidly saturated, and is regulated by pH and parathyroid hormone
2) Apical Membrane
→ Reabsorption via a dibasic and monobasic sodium phosphate transporter
3) Basolateral Membrane
→ it is unknown how phosphate travels across the basolateral membrane
How is Bicarbonate reabsorbed in the proximal convoluted tubule?
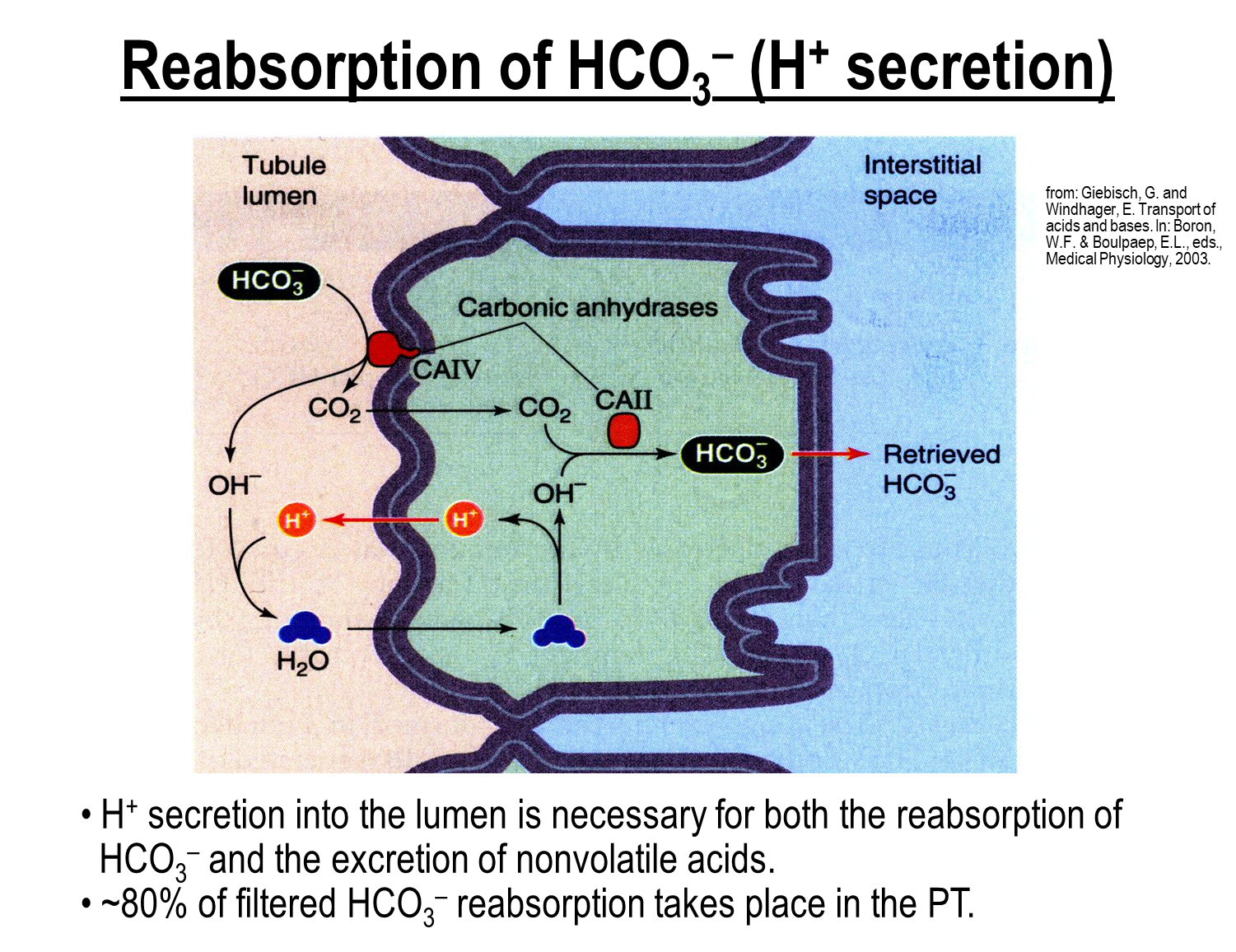
The majority of bicarbonate is reabsorbed in the proximal convoluted tubule. The mechanism for reabsorption is done via carbonic anhydrase
1) Carbonic Anhydrase on the apical surface will convert bicarbonate into CO2 and hydroxide
→ Hydroxide combines with secreted protons in the PCT lumen which forms water
→ The water will enter the cell and deprotonate and form hydroxide again
→ CO2 will pass through the apical surface and then reform with hydroxide making bicarbonate again via carbonic anhydrase II
What can secretion of PAH be used for?
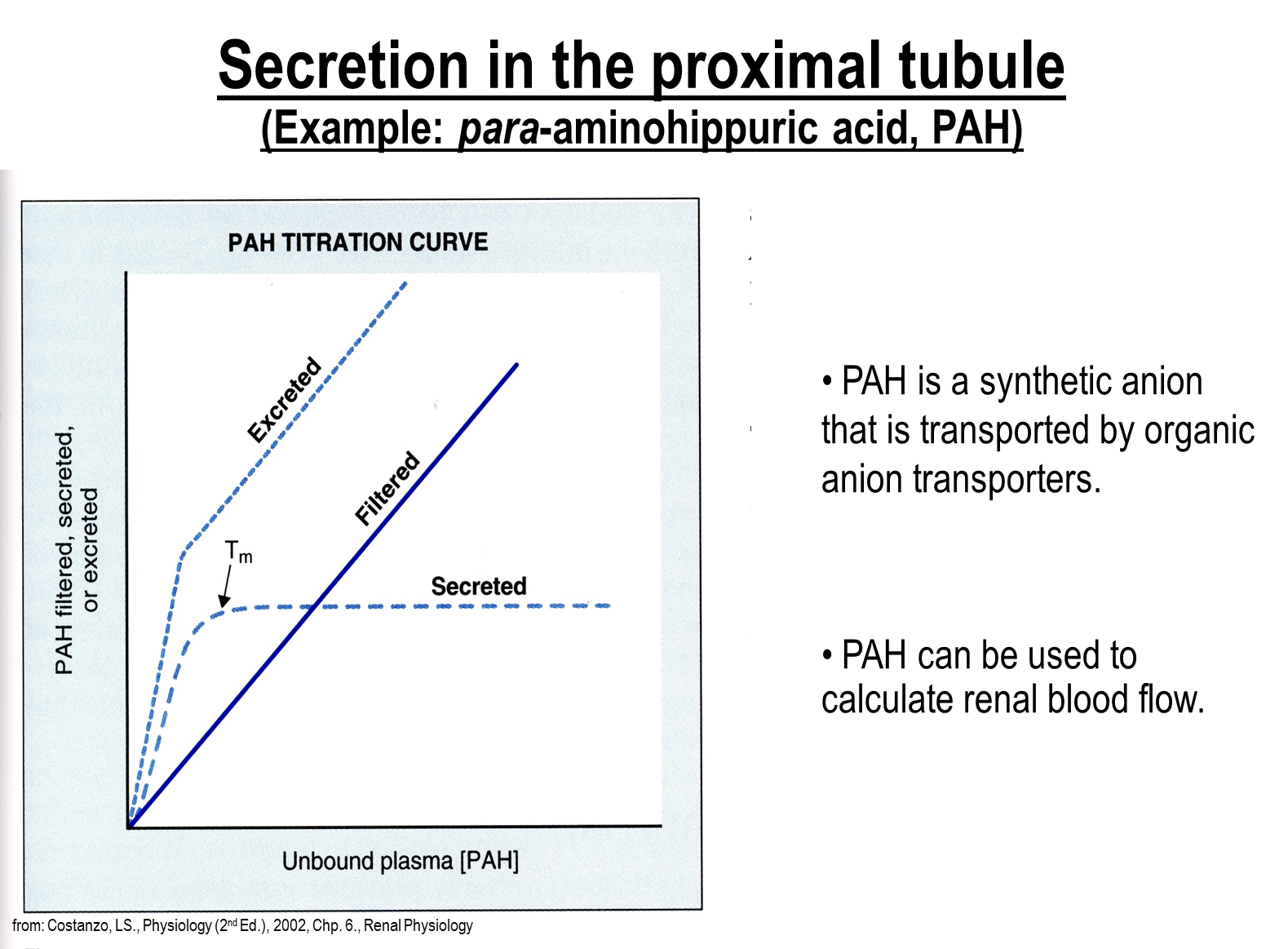
Proximal tubule will secrete both endogenous and exogenous compounds. A good example is para-aminohippuric acid (PAH)
1) PAH is secreted at a faster rate than it is being filtered which means that this can be used to calculate renal blood flow
How does secretion of PAH and cations work?
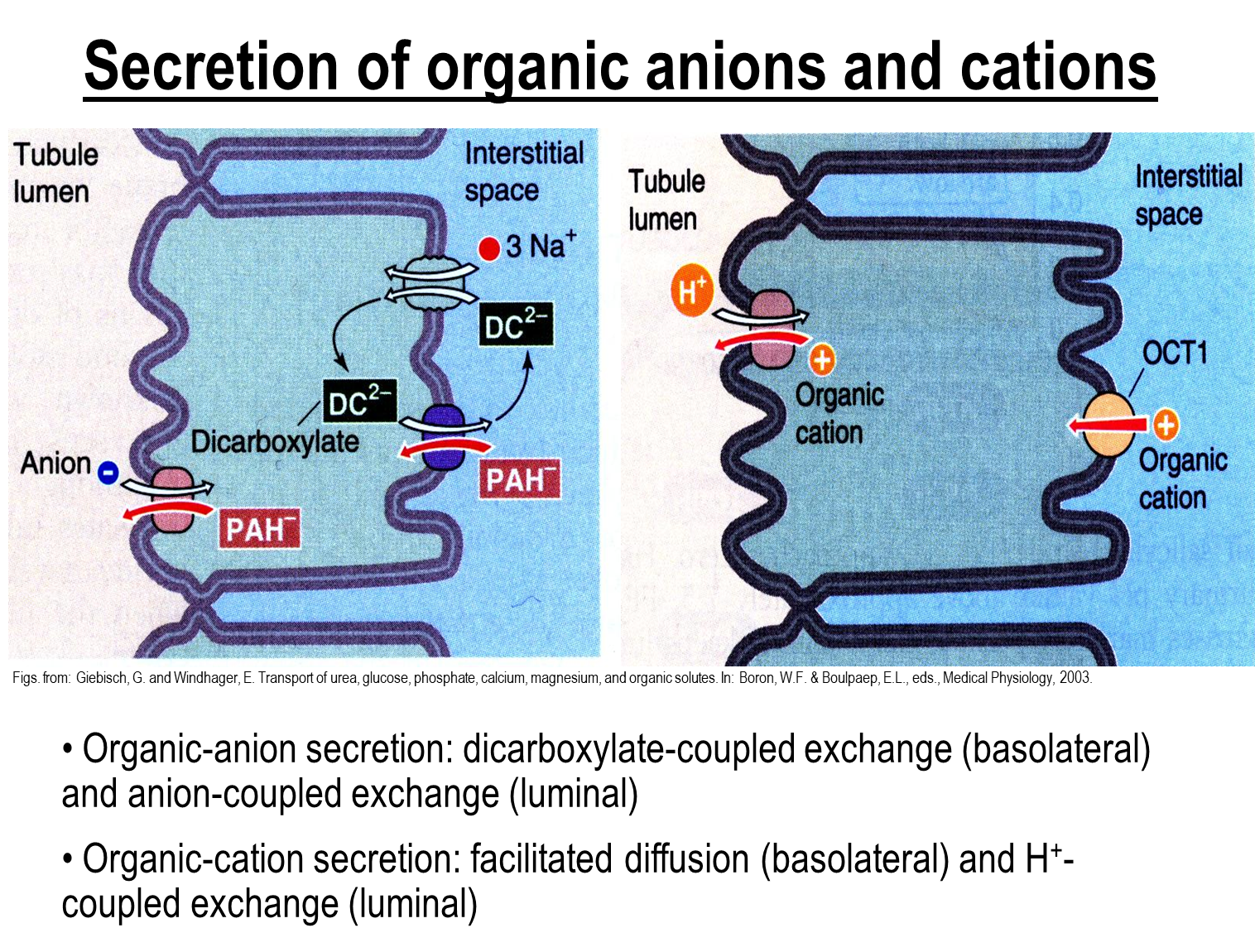
1) PAH will be exchanged with a dicarboxylate on the basolateral surface
→ increased levels of dicarboxylate is created by a sodium dicarboxylate transporter on the basolateral surface
→ apical side PAH is secreted via exchanging with an anion
2) OCT1 is the major transporter for movement of organic cations across the basolateral membrane
→ Organic cations are then secreted into the lumen via exchange with a hydrogen ion