Anatomy, Physiology, and Pathology
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
The shape and size of the breast could depend on:
(1) Age | |
(2) Weight gain or loss | |
(3) Hormonal use | |
(A) 1 and 2 only | |
(B) 2 and 3 only | |
(C) 1 and 3 only | |
(D) 1, 2, and 3 |
Answer: D. Hormones are the most important factor in breast growth and development; however, breast shape and size change with age and weight gain and loss.
The breast meets the abdominal wall at approximately the
(A) Mid-sternum | |
(B) Mid-axillary line | |
(C) Clavicle | |
(D) Seventh rib |
Answer: D. The upper extent of the breast is at the clavicle at the second or third rib. The lowest extent is the abdominal wall at the level of the sixth or seventh rib. Medial extent is the mid-sternum, and lateral extent is the mid-axillary.
On average, how many lobes are found in an | |
adult female breast: are | |
(A) 0-5 | |
(B) 5-15 | |
(C) 15-20 | |
(D) 25-30 |
Answer: C. The breast is composed of approximately 15-20 lobes.
Separating the breast from the pectoral muscle is a fatty area called the:
Inframammary fold
Retromammary space
Supporting and connective tissue
Milk line
2
The retromammary space is filled with a layer of adipose or fatty tissue as opposed to the supporting and connective tissue (stroma), blood vessels, and various ductal structures that make up the glandular and fibrous tissues of the breast.
The muscle immediately posterior to the breast | |
(A) Pectoralis minor muscle | |
(B) Pectoralis major muscle | |
(C) Serratus anterior muscle | |
(D) Latissimus dorsi muscle |
Answer: B. The breast is loosely attached to the fascia covering the pectoralis major muscle. Latissimus dorsi muscle is a broad triangular muscle located on the inferior part of the back. Pectoralis minor muscle is a thin, flat, triangular muscle lying below the pectoralis major. Serratus anterior is a large, flat, fan-shaped muscle on the lateral aspect of the chest.
Parity refers to:
The condition of being pregnant or having delivered a child
Not having any children
Paring or removal of portions of the breast
Breast tissue that is not the same
1
Parity is the terminology used if a woman carries a pregnancy to a point of viability (20 weeks of gestation) regardless of the outcome.
What is the main purpose of hormone replacement therapy?
Relieve from the symptoms of menopause
Increase proliferation of glandular tissue
Control osteoporosis
1 only
1 and 2 only
2 and 3 only
1,2, and 3
1
Hormone therapy (HR) is mainly used to relieve the symptoms of menopause. It can also increase the proliferation of glandular tissue and can be used to control osteoporosis associated with lower estrogen.
The specialized sweat glands found on the areola are called:
TDLU
Montgomery glands
Retromammary gland
Oil cyst
2
Montgomery glands are specialized sebaceous re glands found on the areola. The TDLU is the terminal aut lobular unit where milk is formed. The retromammary space gland) is the area immediately behind the breast, and oil are benign structures found in the breast.
The duct that drains milk directly to the exterior is called the:
Lactiferous sinus
Ampule
Lactiferous duct
Segmental duct
3
The milk enters the ductal system from the TOUD through the segmental or mammary ducts. As the ducts approach the nipple, it widens to form a dilated structure called the ampulla or lactiferous sinus before draining into the last portion of the ductal structure—the lactiferous duct.
Of the following, which mammogram would likely show very dense giandular breast?
Girl aged 10 years
Man aged 50 years
Woman aged 30 years
Woman aged 70 years
3
The prepuberty breast is composed of very few lobules (glandular components). As a woman ages, the glandular components are replaced with fatty tissue in a process called involution.
Only rarely do men develop glandular components within the breast.
A lesion located in the upper outer quadrant of the right breast is located in the
(A) 5:00 o'clock position | |
(B) 2:00 o'clock position | |
(C) | 10:00 o'clock position |
(D) 7:00 o'clock position |
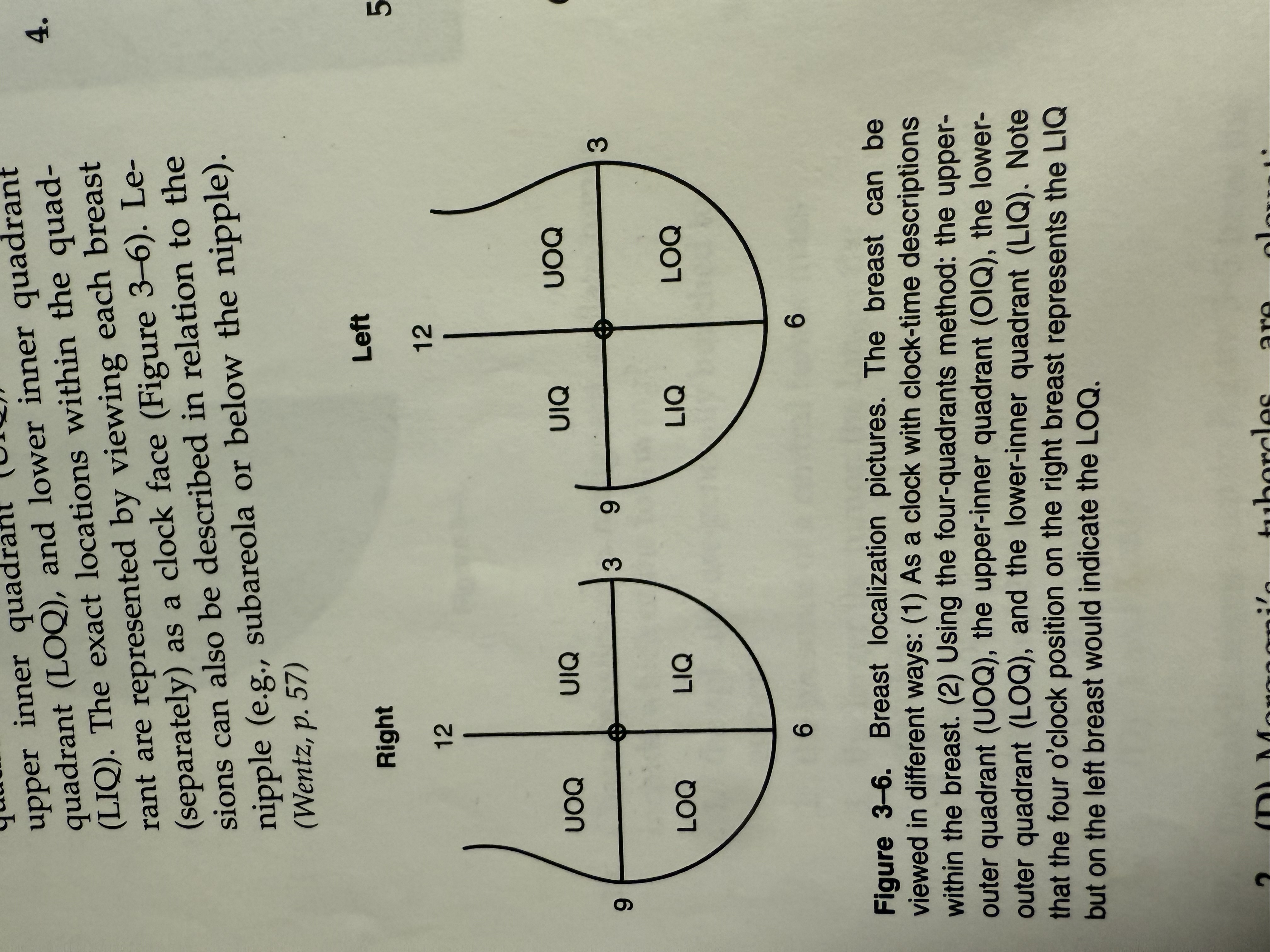
(C) Each breast can be divided into four quadrants: the upper outer quadrant (UOQ), upper inner quadrant (UIQ), lower outer quadrant (LOQ), and lower inner quadrant
(LIQ). The exact locations within the quadrant are represented by viewing each breast (separately) as a clock face (Figure 3-6). Lesions can also be described in relation to the nipple (e.g., subareola or below the nipple).
(Wentz, p. 57)
Morgagni's tubercles are usually found
on the nipple
on the lateral border of the breast
in the terminal duct lobular unit (TDLU)
on the skin of the areola
4
Morgagni's tubercles are elevations formed by the opening of the ducts of the Montgomery's glands, specialized sebaceous-type glands found on the areola, not the nip-ple. (Wentz, p. 11)
An inverted nipple
always indicates breast cancer
sometimes indicates breast cancer
never indicates breast cancer
usually indicates breast cancer
2
The normal nipple can be either flattened or inverted, both unilaterally and bilaterally. However, a nipple that suddenly becomes inverted or flattened can indicate malignancy.
(Logan-Young, p. 16; Wentz, p. 11)
Compression of the breast is most effective and most comfortable when applied to the
(A) medial and lateral aspects | |
(B) inferior and superior aspects | |
(C) medial and superior aspects | |
(D) inferior and lateral aspects |
(D) The breast is most secured at the superior and medial aspects. The lateral borders of the breast and the inferior aspect (infra-mammary crease) are the most mobile portions. Compression is most effective when applied to the mobile aspects of the breast.
(Wentz, p. 45)
The normal breast may have
(A) 5-10 lobes | |
(B) 15-20 lobes | |
(C) | 25-30 lobes |
(D) 30-40 lobes |
(B) On average, a breast has 15 lobes. The number can, however, be as low as 10 or as high as 20. (Harris, p. 4; Wentz, p. 13)
The structure that gives the breast its support and shape is called
(A) Montgomery ligament | |
(B) Cooper's ligament | |
(C) fibroglandular tissue | |
(D) fatty tissue |
(B) Cooper's ligaments are a network of fibrous and elastic membranes. They incompletely sheath the lobes of the breast. The ligaments start at the most posterior portion (base) of the breast and extend outward to attach to the anterior superficial fascia of the skin. Fibroglandular and fatty tissue make up the breast parenchyma. The Montgomery is a gland, not a ligament. (Harris, p. 4; Wentz, p. 13)
The breast extends vertically from the
1st through the 9th rib
2nd through the 9th rib
2nd through the 6th rib
3rd through the 10th rib
3
The breast extends vertically from the clavicle (the second or third rib) to meet the abdominal wall at the level of the sixth or seventh rib and horizontally from the mid-sternum to the midaxillary line (the latis-simus dorsi muscle). (Harris, p. 3; Wentz, p. 11)
The thickest portion of the breast is the
(A) areola | |
(B) nipple | |
(C) tail of Spence | |
(D) inframammary crease |
(C) The upper outer quadrant, which extends toward the axilla, is known as the axil-lary tail or the tail of Spence. It is the thickest portion of the breast. Thorough knowledge of the anatomic extent of the breast is critical in breast imaging. (Logan-Young, p. 16)
Cooper's ligaments attach anteriorly to the
deep fascia of the lobes
fascia of the skin
posterior surface of the breast
connective and supporting stroma
2
Cooper's ligaments are strands of connective tissue that run between the skin and deep fascia to support the lobes of the breast. They start at the most posterior portion (base) of the breast, extend outward, and attach to the anterior fascia of the skin. (Wentz, p. 13)
Fatty tissue is generally _______ and on the mammogram is seen as areas of ___ optical density.
radiolucent/lower
radiopaque/higher
radiolucent/higher
radiopaque/lower
3
Fatty tissue is radiolucent and will therefore show as higher optical density areas on mammograms (white or gray). Fibrous and glandular tissue are less radiolucent and will show as lower optical density on the mammograms (black). (Wentz, p. 12)
Typically, a patient with dense fibrous and glandular tissue throughout the entire breast is
age 20 or younger
age 50 or older
over age 70
under age 45
4
In general, the amount of fat and glandular tissue varies with age. Glandular tissue predominates in younger women, whereas fatty tissue predominates in older patients. A patient under 20 is unlikely to have regular mammograms. (Logan-Young, p. 15; Wentz, p. 13)
Glandular tissue is usually found in the ______ of the breast.
(A) medial and lower inner quadrant | |
(B) central and upper outer quadrant | |
(C) medial and lower outer quadrant | |
(D) upper inner quadrant and central |
(B) The majority of glandular tissue is distributed in the breast bilaterally and is located centrally and laterally toward the upper outer quadrant, extending toward the axilla. Most breast cancer arises from the glandular tissue.
(Logan-Young, p. 17; Wentz, p. 13)
Lymph drainage from the medial half of the breast is generally directed to the
(A) internal mammary lymph nodes | |
(B) external mammary lymph nodes | |
(C) axillary lymph nodes | |
(D) axilla |
(A) The main direction of drainage from the lateral half of the breast tends to be into the pectoral group of axillary lymph nodes and from the medial half of the breast into the internal mammary lymph nodes. (Wentz, p. 13)
Immediately behind the nipple the connecting duct widens to form the
lactiferous sinus
ampulla acinus
TDLU
segmental duct
1
From the nipple orifice a connecting or lactiferous duct immediately widens into the lactiferous sinus (or ampulla). The ampulla is a pouch-like structure that holds milk (when it is being produced). The ampulla then narrows to become the segmental or mammary ducts. These branch into smaller ducts with decreasing diameter until becoming a lobule.
(Logan-Young, p. 15; Thomas, p. 1069)
The portion of the breast that holds the milk-producing element is the | |
(A) ampulla | |
(B) segmental duct | |
(C) lobule | |
(D) lactiferous sinus | |
(C)
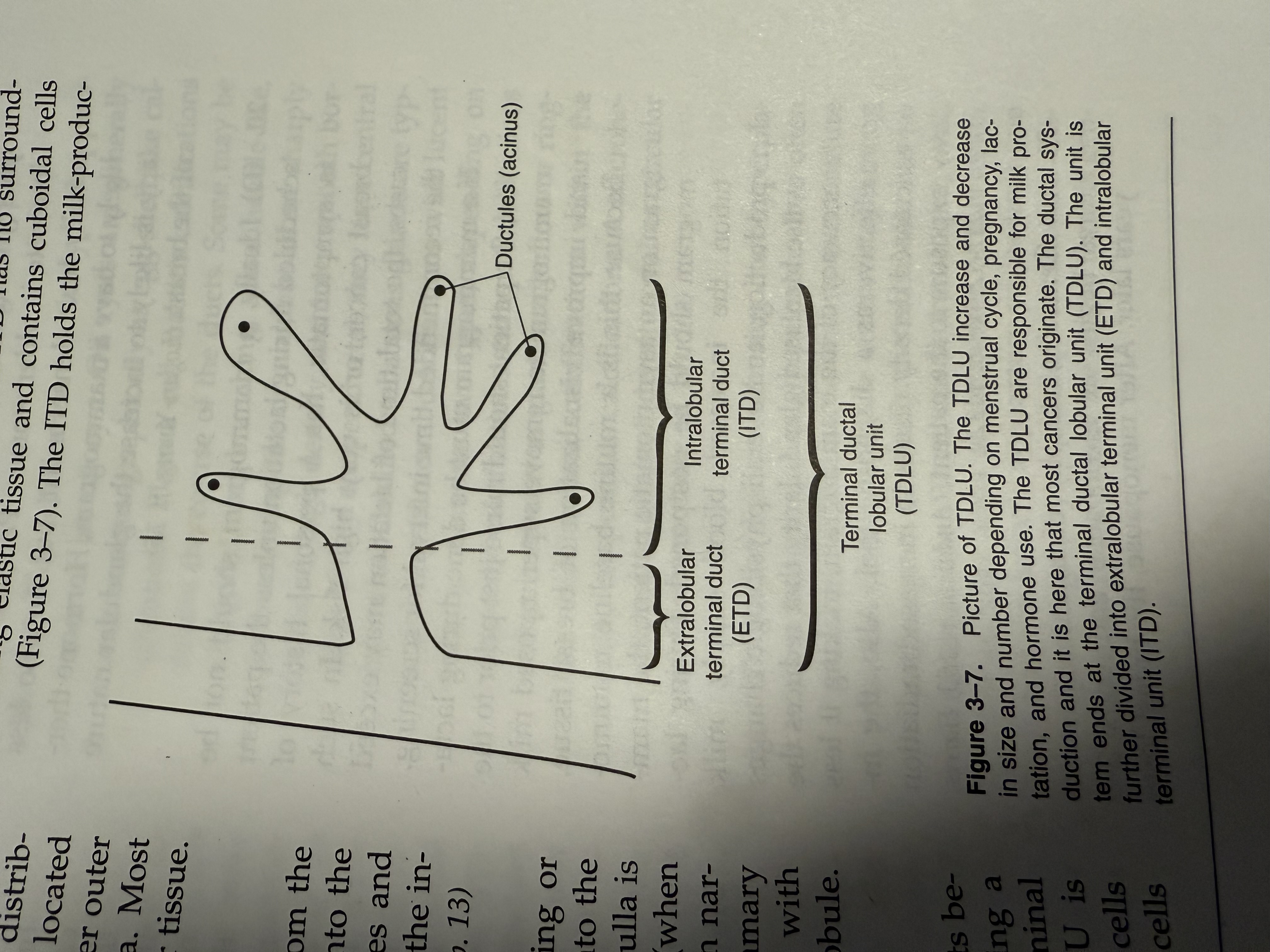
From the nipple, the mammary ducts become smaller and smaller until becoming a lobule. The lobule is also called the terminal ductal lobular unit (TDLU). The TDLU is lined with a single layer of epithelial cells and a peripheral layer of myoepithelial cells and consists of both the extralobular and the intralobular terminal ducts. The intralobu-lar terminal ducts (ITD) hold the alveolar glands, which are the milk-producing elements of the breast. (Logan-Young, p. 15)
Veins are normally located | |
(A) in the periphery of the breast | |
(B) central areas of the breast | |
(C) in the axilla area of the breast | |
(D) in the medial areas of the breast | |
(A) Veins are larger than arteries. Unlike arteries, they are normally located peripherally and easily seen. Mammographically they appear as low-density, radiopaque vessels. Both arteries and veins can be outlined by calcifi-cations. (Andolina, p. 171; Wentz, p. 13)
The terminal ductal lobular unit consists of the
mammary ducts and the extralobular terminal ducts
intralobular terminal duct and the segmental duct
the extralobular terminal ducts and the lactiferous ducts
both the extralobular and the intralobu-lar terminal ducts
4
The TDLUs are further divided into the extralobular terminal duct (ETD), which is a small duct leading into the terminal ductules, and the intralobular terminal duct (ITD), located at the end of the terminal ductules. The ETD is surrounded by elastic tissue and lined by columnar cells. The ITD has no surrounding elastic tissue and contains cuboidal cells (Figure 3-7). The ITD holds the milk-producing elements of the breast, called the ductules or acinus (plural, acini). Each lobule can have 10-100 terminal ductules. (Harris, p. 4; Wentz, p 12)
A patient began taking synthetic hormones 6 months prior to her current mammogram.
The mammogram is most likely to
be unchanged from the previous year
show increased glandular tissue compared to her previous mammogram
show decreased glandular tissue compared to her previous mammogram
show increased fatty tissue compared to her previous mammogram
2
Increased or decreased glandularity of the breast is a part of the normal physiologic changes that take place. It can be related to menarche, hormonal fluctuation whether normal or synthetic, pregnancy, lactation, or menopause. The two most prominent hormones active in pathology are estrogen (responsible for ductal proliferation) and progesterone (responsible for lobular proliferation and growth). (Logan-Young, p. 15; Wentz, p. 12)
The mammogram shows that the patient's breast consists primarily of adipose tissue.
This patient is most likely to be
on hormone therapy
over age 60
under age 20
over age 35
2
Patients over age 60 will most likely have fatty breast; glandular tissues predominate in young women and adipose tissue (fat) predominate in older women. Patients under 20 usually have dense breast, but are also less likely to have a mammogram. Hormone therapy is likely to increase the glandular nature of the breast. (Logan-Young, p. 15)
A patient is to have a routine baseline mammogram, but it is determined that the woman is lactating. What should be done?
Lactating breasts are extremely sensitive; the mammogram should be postponed.
The mammogram should be done; the radiation has no effect on lactation.
Although lactating breasts are extremely dense, the mammogram should not be rescheduled.
Lactation causes increased glandularity; the mammogram should be postponed.
4
Ideally, a mammogram should not be scheduled during lactation unless the patient is symptomatic, has a personal history of breast cancer, or is very high risk. In such cases, the total time of lactation may exceed the recommended time interval for screening.
If a mammogram must be done during lactation, the patient should nurse just prior to the mammogram to remove superimposed milk and improve visualization of breast tissue.
Because this is a routine baseline mammogram on an asymptomatic patient, the mammogram should be postponed. During lactation the increased blood supply, milk production, and overall physiologic changes cause increased glandularity that reduces the accuracy of the mammogram, making it less effective as a diagnostic tool. Also, the increased density results in increased radiation exposure to the patient. (Andolina, p. 153; Harris, pp. 11-12; Wentz, p. 12)
The craniocaudad mammograms of the same woman prior to menopause and 1 year after the onset of menopause are compared. The woman has never taken synthetic hormones.
What is the most likely difference?
The mammogram taken prior to menopause shows signs of atrophy.
The mammogram taken after the onset of menopause shows signs of atrophy.
There will be little or no change in the glandularity of the breast.
The mammogram taken after menopause will show increased glandularity.
(B) Generally, atrophy of mammary structures begins at menopause and ends 3-5 years later. After menopause, the breast loses its supportive tissue to fat, producing a smaller breast, or a larger, more pendulous one. This process is called involution.
Which of the following will affect the ratio of glandular tissue to total breast tissue?
the woman's genetic predisposition
ratio of total body adipose tissue to total body weight
drastic weight gain or weight loss
1 only
1 and 2 only
2 and 3 only
1, 2, and 3
4
The total amount of glandular tissue increases and decreases with hormonal fluctuations, use of synthetic hormones, and menopause. The amount of glandular tissue versus fatty tissue will also depend on a woman's genetic predisposition. It is therefore possible to find young women with fatty breast and older women with extremely dense, glandular breast. Weight gain and loss also increase or decrease the fat content of the breast tissue, thereby affecting the overall glandularity of the breast. (Logan-Young, p. 15;
Wentz, p. 12)
What procedure should be followed if a symptomatic patient who is lactating is scheduled for a mammogram?
The mammographer should attempt spot compression views only.
The mammogram should be done, but the study may be limited.
Lactating breasts are extremely dense; the mammogram should be postponed.
Lactation causes increased glandularity; the mammogram should be postponed.
2
Ideally, a mammogram should not be scheduled during lactation unless the patient is symptomatic, has a personal history of breast cancer, or is very high risk. In such cases the total time of lactation may exceed the recommended time interval for screening. If any of the above reasons apply and if a mammogram must be done during lactation, the patient should nurse just prior to the mammogram to remove superimposed milk and improve visualization of breast tissue. During lactation the increased blood supply, milk production, and overall physiologic changes cause increased glandularity that reduces the accuracy of the mammogram, making it less effective as a diagnostic tool. Also, the increased density results in increased radiation exposure to the patient. (Andolina, p.153; Harris, pp. 11-12; Wentz, p. 12)
A woman is referred to as nulliparous. This means
(A) she has never given birth to a child (B)the woman has had one child
(C)the woman has never produced a viable offspring
(D)she carried a pregnancy to a point of viability regardless of the outcome
(A) A nulliparous is the condition of not having given birth to a child. Parity is the terminology used if a woman carries a preg nancy to a point of viability (20 weeks of ges-tation) regardless of the outcome. Other terminology is multiparity, regarded as having borne more than one child, and prima-para, a woman who has delivered a child of 500 g (or of 20 weeks' gestation) regardless of its viability. (Thomas, pp. 1243, 1317, 1415)
An asymptomatic patient presents with an oval, lobulated tumor with unsharp margins.
There is no evidence of a halo sign.
If the lesion is also radiolucent it is likely to be benign.
The lesion could be malignant.
All oval lesions are benign.
The absence of a halo indicates malignancy schematic.
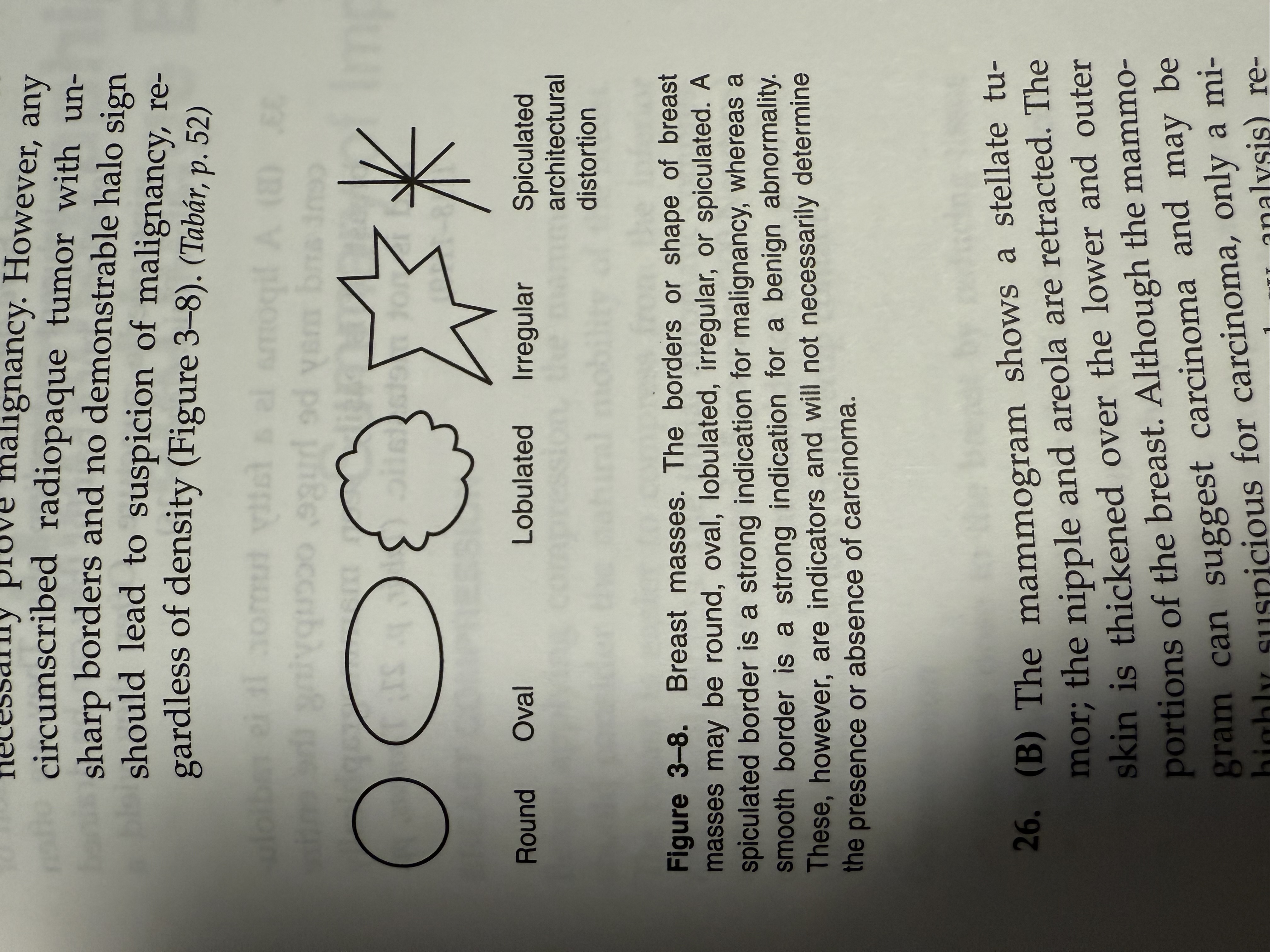
(B) Although a halo is typically present in benign lesions, absence of a halo does not necessarily prove malignancy. However, any circumscribed radiopaque tumor with un-sharp borders and no demonstrable halo sign should lead to suspicion of malignancy, regardless of density (Figure 3-8). (Tabár, p. 52)
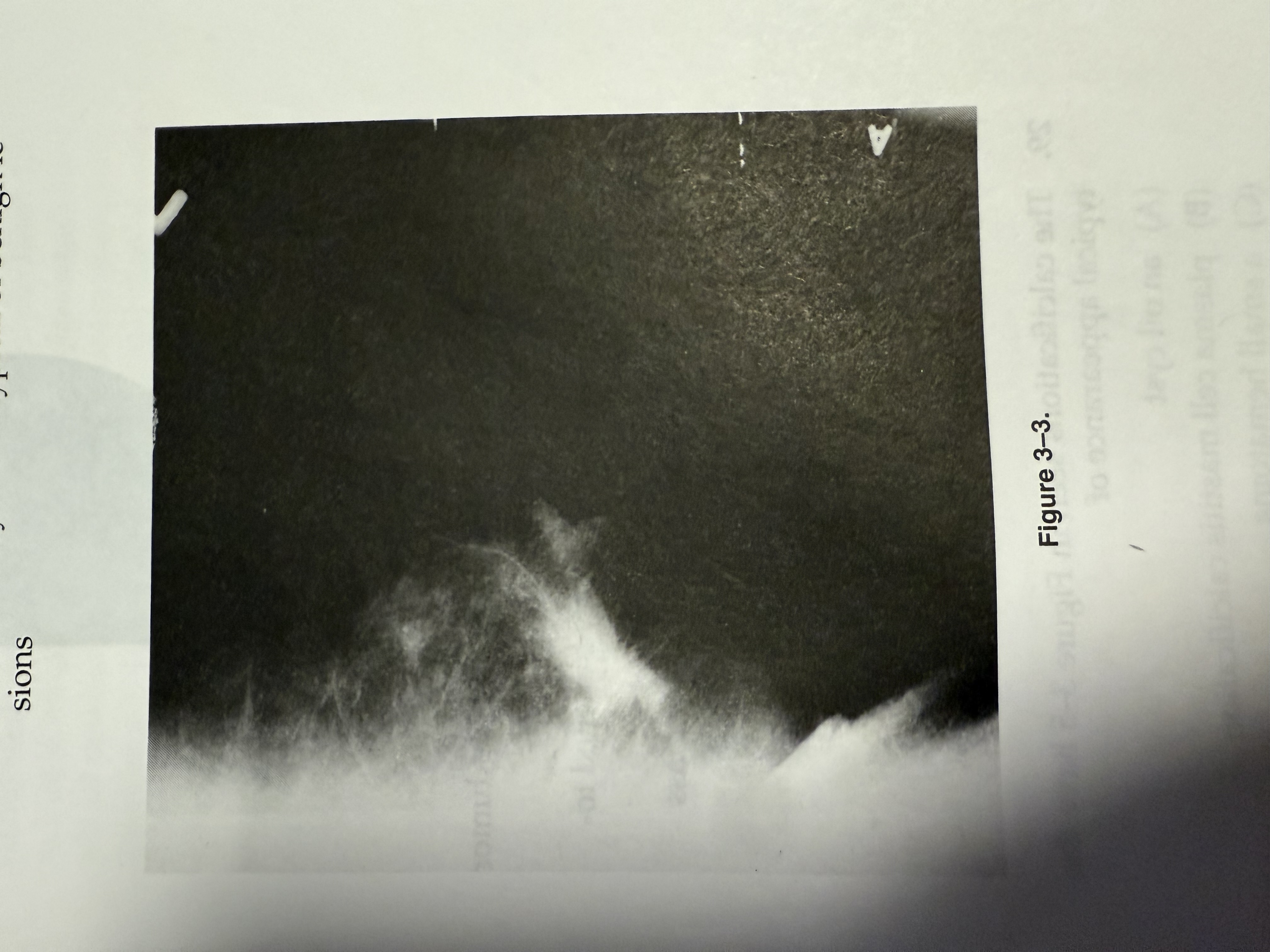
The tumor seen in Figure 3-3 indicates
invasive ductal breast carcinoma
a mammographically malignant tumor
a mammographically benign tumor
a low-density tumor typical of benign lesions
2
The mammogram shows a stellate tu-mor; the nipple and areola are retracted. The skin is thickened over the lower and outer portions of the breast. Although the mammogram can suggest carcinoma and may be highly suspicious for carcinoma, only a microscopic diagnosis (histology analysis) reveals the exact type. The presence of a central tumor mass with associated spicules is typical of malignant stellate tumors. The spicules are dense and sharp, radiate from the tumor surface, and usually are not bunched to-gether. When they extend to the skin or areo-lar region, they cause retraction and local thickening. Generally, the larger the tumor, the longer the spicules. (Tabár, p. 97)
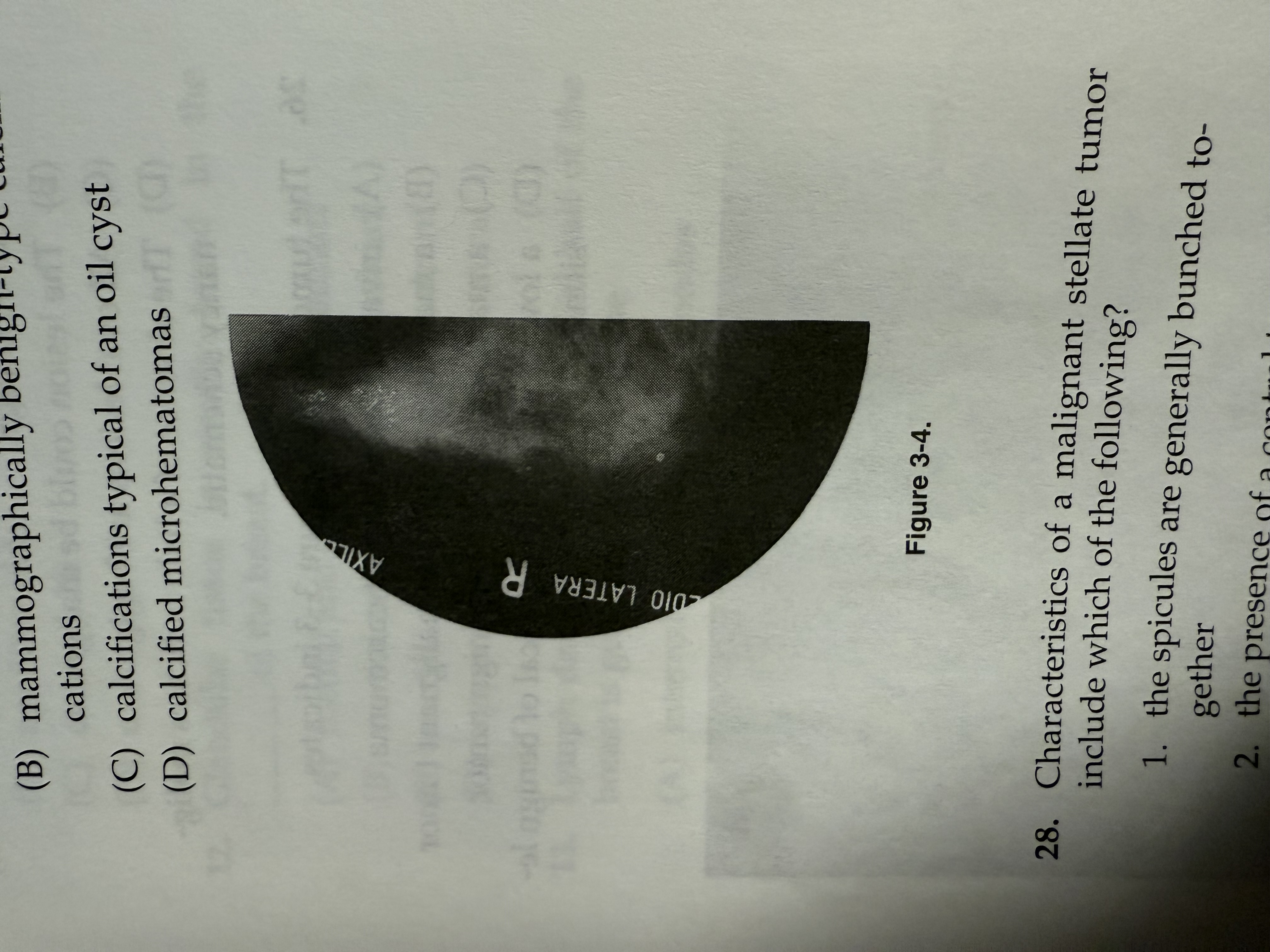
The calcifications seen in Figure 3-4 have the typical appearance of
mammographically malignant-type calcifications
mammographically benign-type calcifications
calcifications typical of an oil cyst
calcified microhematomas
1
These calcifications are typical of mammographically malignant-type casting and granular microcalcifications. Casting calcifications are produced when carcinoma in situ fills the ducts and their branches. The shape of the cast is determined by the uneven production of calcifications and the irregular necrosis of the cellular content. The contours of the cast are always irregular in density, size, and length and the casts are always fragmented. A calcification is seen as branching when it extends into adjacent ducts. Also, the width of the ducts determines the width of the castings. Granular type calcifications are seen as mammographically similar in appearance to granulated sugar or crushed stones. These are also malignant-type calcifi-cations. Oil cysts are generally seen mammo-graphically as eggshell-like calcifications and a microhematoma is a mixed-density oval or circular calcification. (Tabár, p. 154)
Characteristics of a malignant stellate tumor include which of the following?
the spicules are generally bunched together
the presence of a central tumor mass
the larger the tumor, the longer the spicules
1 only
1 and 2 only
2 and 3 only
1 and 3 only
3
A typical malignant stellate tumor has a central tumor with dense spicules radiating in all directions. The spicules are separate and increase in length with increased tumor size.
If the spicules reach the skin, there is localized dimpling or skin thickening. (Tabár, p. 94)
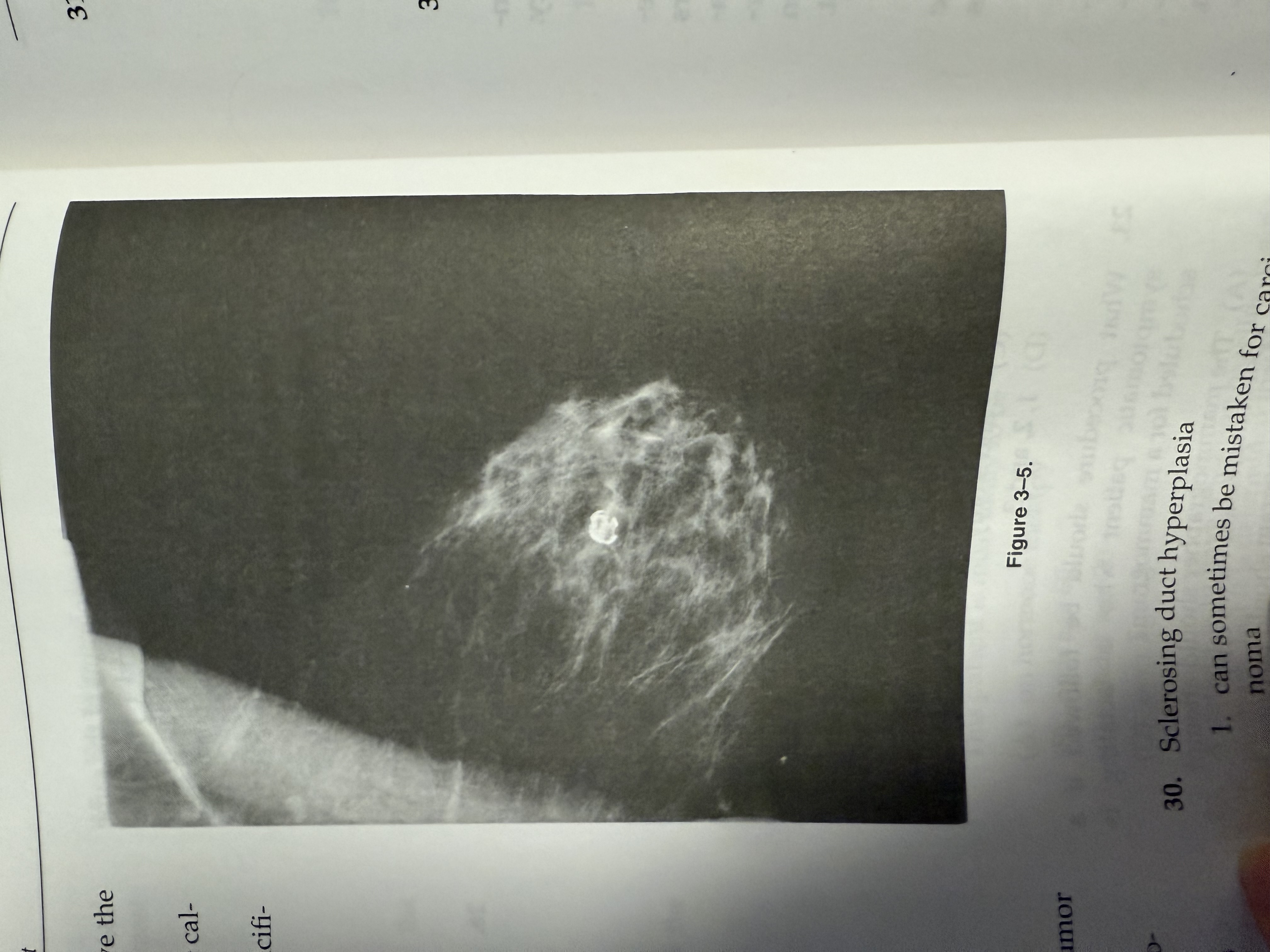
The calcifications seen in Figure 3-5 have the typical appearance of
an oil cyst
plasma cell mastitis calcification
a small hematoma
a calcified sebaceous gland
Sclerosing duct hyperplasia
can sometimes be mistaken for carcinoma
sometimes has a solid dense central tumor
is usually not associated with skin thickening or dimpling over the lesion
(A) 1 only | |
(B) 1 and 2 only | |
(C) 2 and 3 only | |
(D) 1 and 3 only |
D
Radial scar or sclerosing duct hyperplasia is benign and rarely palpable. It is often mistaken for carcinoma and its exact nature is the subject of some controversy among pathologists. Generally, the radial scar has no central tumor. There can be translucent, oval, or circular areas at the center of the lesion and the lesion's appearance varies from one mammography projection to another. Regardless of the size of the lesion, there is gererally no associated skin thickening or dimpling and no discernible palpable mass.
(Tabár, pp. 95-96)