Adrenal Tumors and Disorders
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
17 Terms
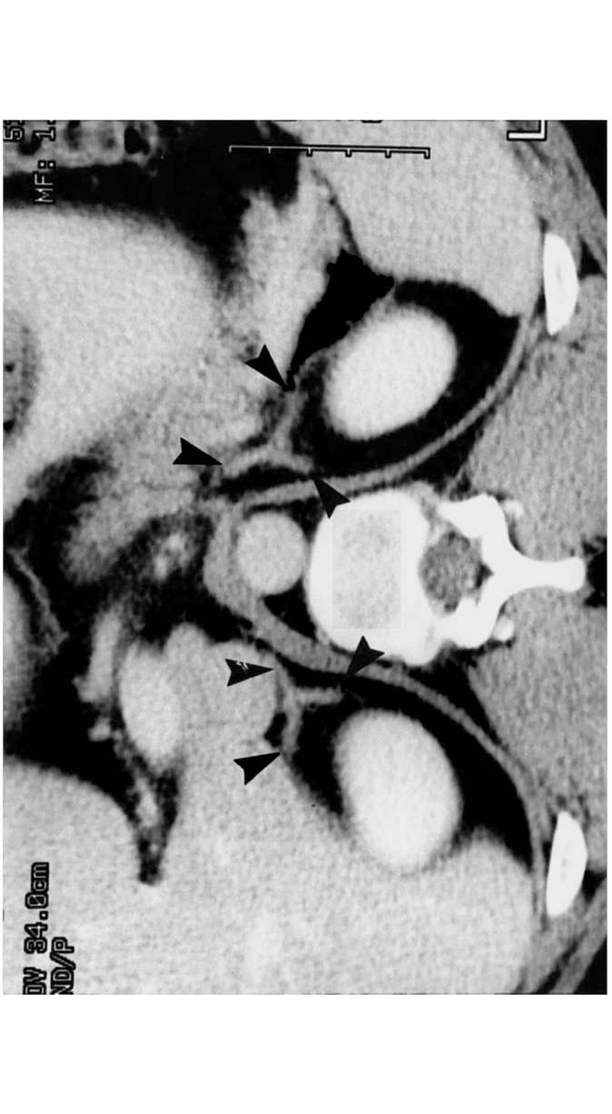
What do the adrenal glands look like on imaging? What is its blood supply?
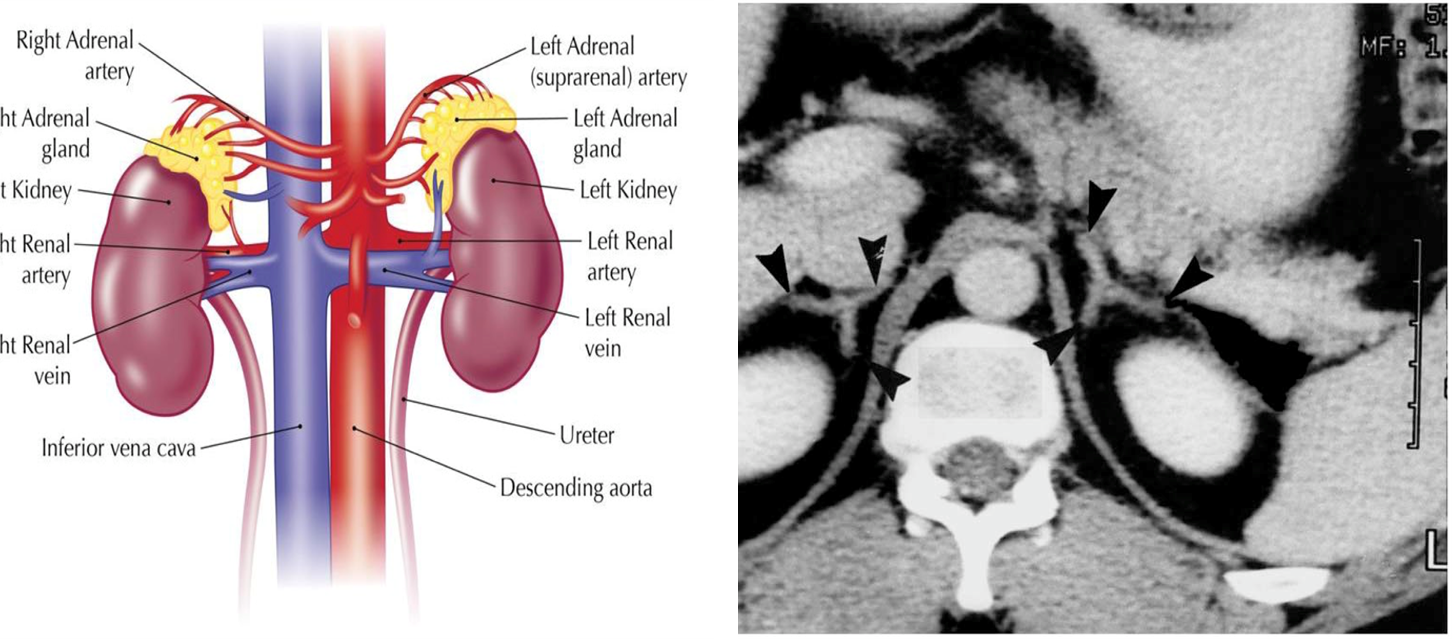
On imaging, adrenal glands appear like a wish-bone shaped organ that sits anterior and medially to the kidneys
1) These adrenal glands are supplied from three different sources
→ Phrenic
→ Aorta
→ Renal
2) These glands are then drained by the adrenal veins which have different drainages depending on which side it is on:
→ Right adrenal vein drains into the inferior vena cava
→ Left adrenal vein drains into the renal vein
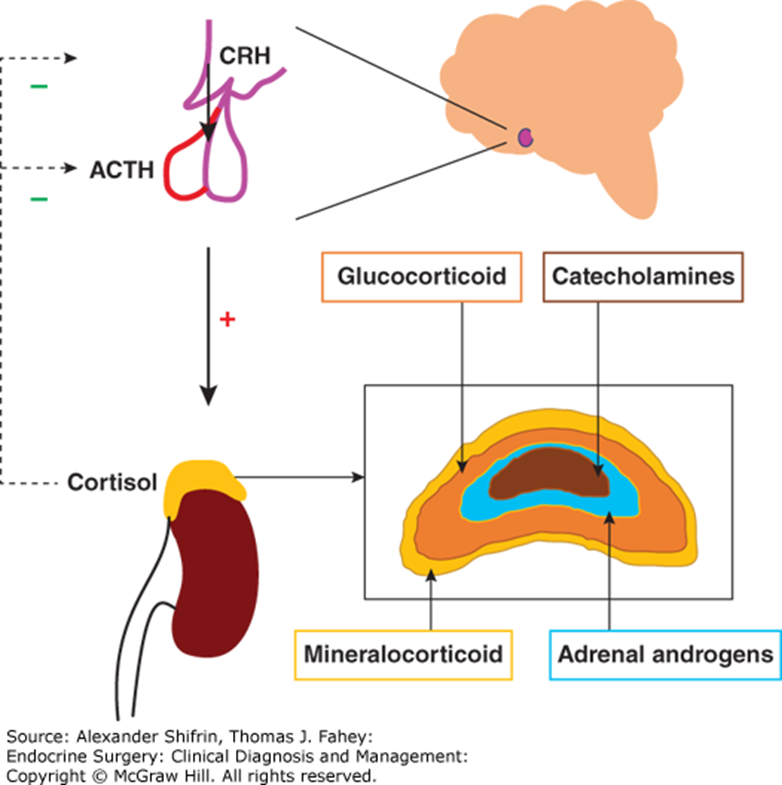
What are the symptoms of functional tumors found at each adrenal layer?
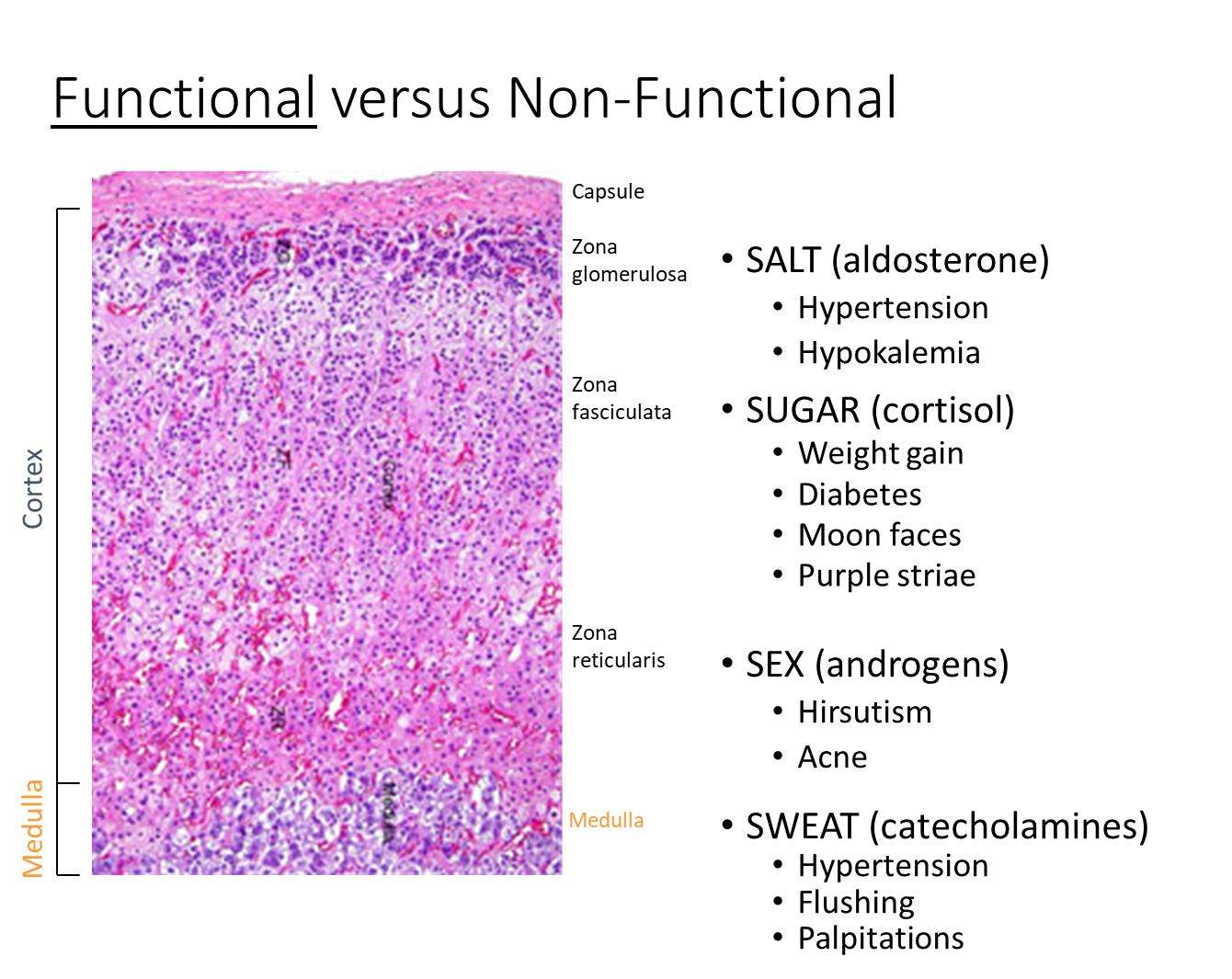
1) Zona Glomerulosa - SALT/Aldosterone
→ Hypertension
→ Hypokalemia
2) Zona Fasciculata - SUGAR/Cortisol
→ Weight Gain
→ Diabetes
→ Moon Faces
→ Purple Striae
3) Zona Reticualris - SEX/Androgens
→ Hirsutism (excessive hair growth)
→ Acne
4) Medulla - SWEAT/Catecholamines
→ Hypertension
→ Flushing
→ Palpitations
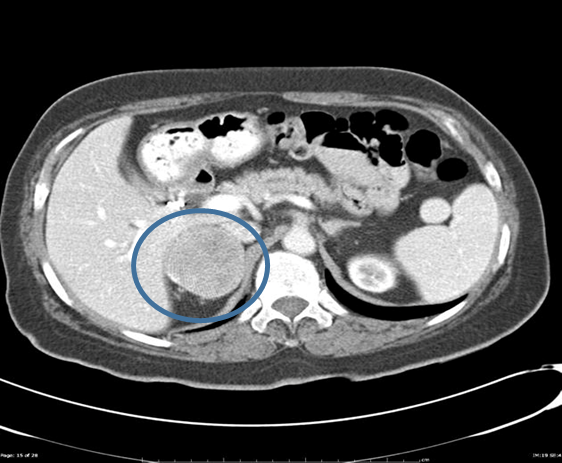
What is an Incidentaloma? What tests should be done?

Many patients will have adrenal incidentalomas which are unexpected, asymptomatic masses that are larger than 1 cm and are found incidentally through imaging
Make sure to measure labs
1) Cortisol
→ dexamethasone suppression test - evaluates ACTH levels by suppressing cortisol production
→ 24-hour urine cortisol - evaluation of cortisol
2) Renin and Aldosterone Levels
3) Sex steroid secreting tumors are very rare, but are considered adrenal cortical carcinoma
4) Plasma free metanephrines is used to measure medullary overactivity
What is a Pheochromocytoma?
Pheochromocytoma is a catecholamine producing neuroendocrine tumor found in the adrenal medulla
1) Patients will have high sympathetic activity due to increased release of norepinephrine and epinephrine
→ patients will be sweating, hypertension, and tachycardic due to alpha and beta activation
→ patients will be dehydrated due to intravascular constriction
2) Important testing includes plasma or urine fractionated metanephrine + normetanephrines levels
→ all patients need genetic testing to rule out genetic syndromes
3) Treated with surgery but you need to perform an alpha and beta blockade
What genetic syndromes is pheochromocytoma associated with?
There are four major diseases that are associated with pheochromocytoma
1) MEN2A/2B
→ importantly with MEN2A, medullary thyroid cancer is often first identified. It is important to then see if the patient has pheochromocytoma prior to treatment in order to prevent hypertensive crisis
2) Neurofibromatosis
3) von Hippel-Lindau Syndrome
4) SDHA/B
What is the treatment of pheochromocytoma?
Pheochromocytoma is treated surgically, but prior to surgery you need to do an alpha blockade and beta blockade
1) Alpha Blockade is done first
→ during surgery, stress can lead to uncontrolled catecholamine release
→ may lead to hypertensive crisis if alpha receptors are not blocked
2) Beta Blockade is done second to prevent unrestricted alpha agonism
What is an Aldosteronomas?
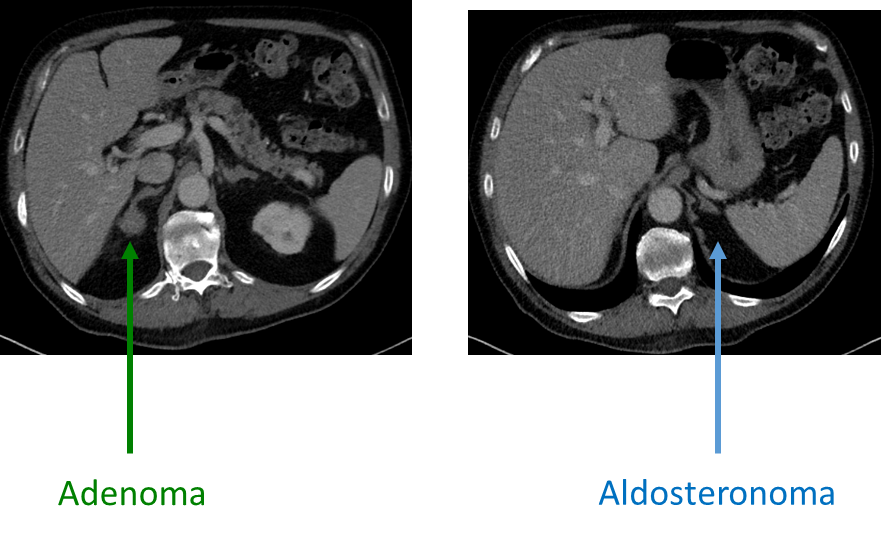
Aldosteronomas or Conns Syndrome are tumors of the zona glomerulosa that causes hyperaldosteronism
1) Hypersecretion of aldosterone often leads to hypertension and hypokalemia due to rapid uptake of sodium and secretion of potassium and hydrogen
→ patients should have suppressed renin release
2) Most common cause of aldosteronomas are bilateral hyperplasia
→ patients with bilateral hyperplasia are unable to be surgically treated, and need to be treated with a aldosterone antagonist
→ unilateral tumors can be treated with resection
What is Cushing’s Syndrome?
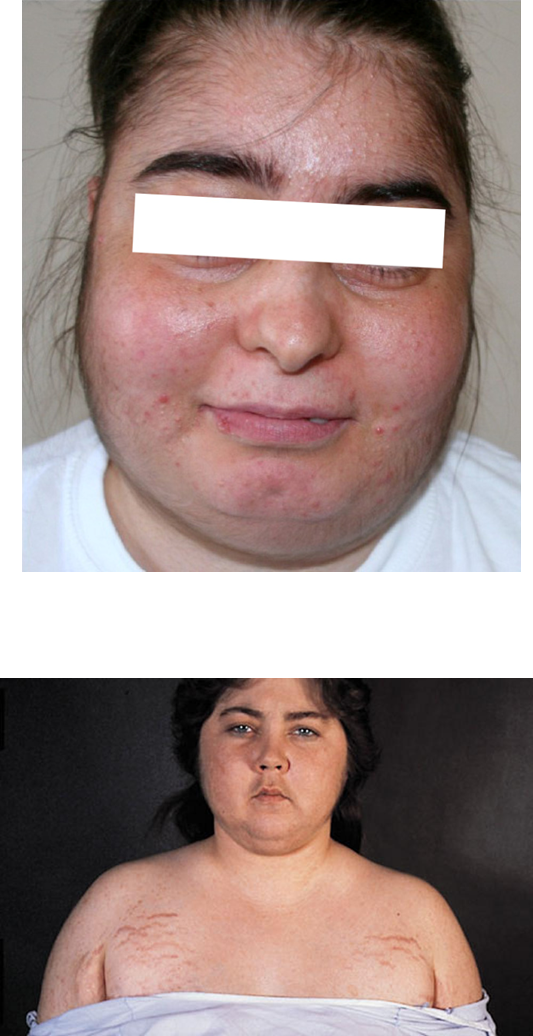
Cushing’s Syndrome is a disorder of cortisol excess
→ differentiated from Cushing’s Disease which refers to Cushing Syndrome caused by a pituitary adenoma
1) Cushing Syndrome results in elevated cortisol levels leading to increase in gluconeogenesis and stress response
→ patients have weight gain, moon faces, diabetes, and purple striae
→ cortisol also has immunosuppressive effects that causes poor wound healing
2) Most common cause of Cushing Syndrome is exogenous steroids
→ can also be caused by primary adrenal lesions or pituitary tumors
How is Cushing’s Syndrome diagnosed and treated?
Cushing’s disease can either be ACTH dependent or independent
→ ACTH-dependent - ACTH will be elevated and is pituitary in origin
→ ACTH-independent - ACTH will be normal or low
1) Tested with a 24-hour urine cortisol or a dexamethasone suppression test
→ dexamethasone suppresses cortisol production, and if high after suppression indicates autonomous cortisol production
2) Treated with surgical resection
When do you treat non-functional incidentalomas?
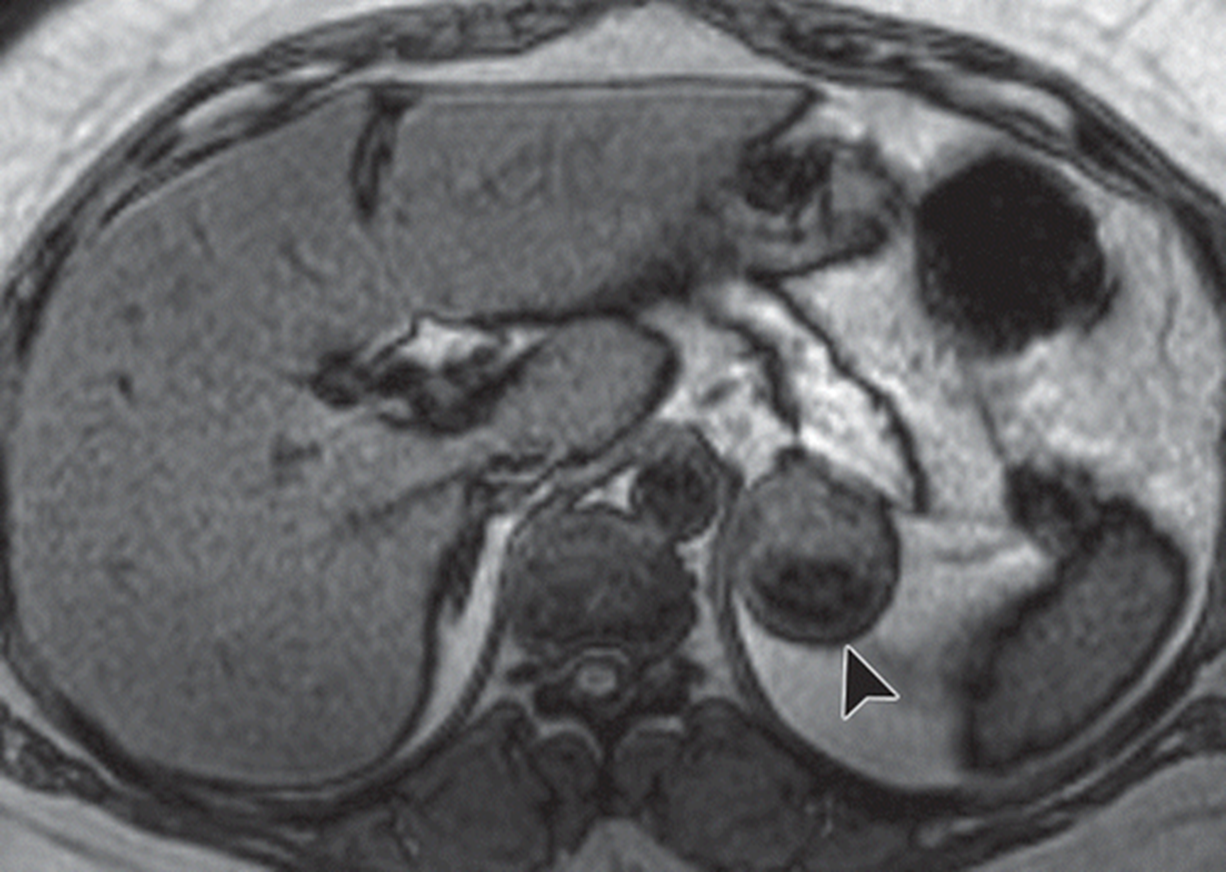
Nonfunctional Incidentalomas are often round and well circumscribed with heterogenous enhancement on imaging
You treat them based on their size and imaging characteristics
1) Small (less than 3 cm) you observe
2) > 4 cm you should surgically resect due to risk of adrenocortical carcinoma
3) in between 3-4 cm you should surveillance with imaging and labs
→ you can resect if good candidate
What is the staging and treatment of adrenocortical carcinoma?
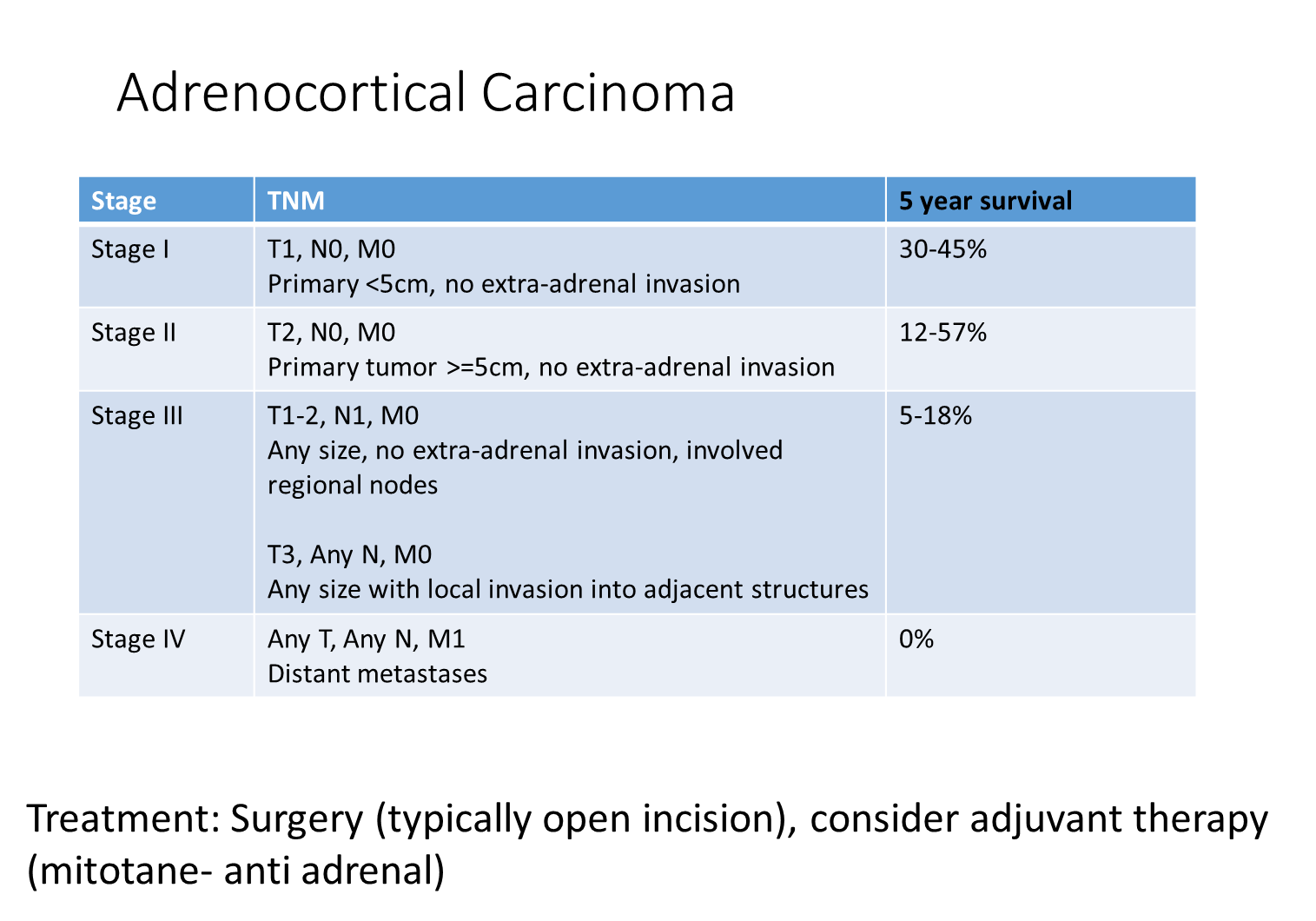
Adrenocortical Carcinoma is staged based on the TNM into four stages
1) Stage I
→ less than 5 cm in size with no extra-adrenal invasion
2) Stage II
→ larger than 5 cm, no extra-adrenal invasion
3) Stage III
→ local invasion
4) Stage IV
→ distant metastasis
Treated with surgery (open incision) and mitotane which is an anti-adrenal chemotherapy
When should you biopsy and treat an adrenal incidentaloma?
Biopsies for incidentalomas have a high false negative and false positive rate for adrenocortical carcinoma
1) You only biopsy if you are concerned for metastatic disease to the adrenal gland
→ commonly seen in patients that have had lung cancer or something that randomly present with a mass in the adrenal gland
2) If the metastatic disease is isolated or only in the adrenal gland you should resect
→ if metastasis occurs to multiple areas you should not resect
What is Addison’s Disease?
Addison’s Disease is a intrinsic failure of the adrenal cortex and results in a failure of cholesterol from being converted to steroid hormones of the cortex
1) Can be primary or secondary/tertiary
2) Patients will commonly present with weight loss and decreased appetite
→ patients are often hypotensive and hypoglycemic
→ often present with GI issues such as nausea and vomiting
→ are hyponatremic
3) Patients can be hyperpigmented due to excess cleavage of POMC
What is Congenital Adrenal Hyperplasia
Congenital Adrenal Hyperplasia is a group of autosomal recessive disorders that causes enzyme deficiencies in adrenal steroidogenesis
1) Patients most commonly have 21-hydroxylase deficiency which is necessary for cortisol and aldosterone synthesis
→ leads to elevated ACTH and high androgen levels leading to virilization or increase in male sex-characteristics
2) Tested with an ACTH stimulation test which measures an appropriate cortisol increase in response to ACTH
What is Waterhouse-Friedrichsen Syndrome?

Waterhouse Friedrichsen Syndrome is a bilateral hemorrhage of the adrenal glands secondary to shock or disseminated intravascular coagulation following some septic infection
1) Most commonly occurs secondary to Neisseria Meningitides infection
→ and presents with complete and sudden collapse of cortical function
What are the identifiable features of aldosteronomas on histology?
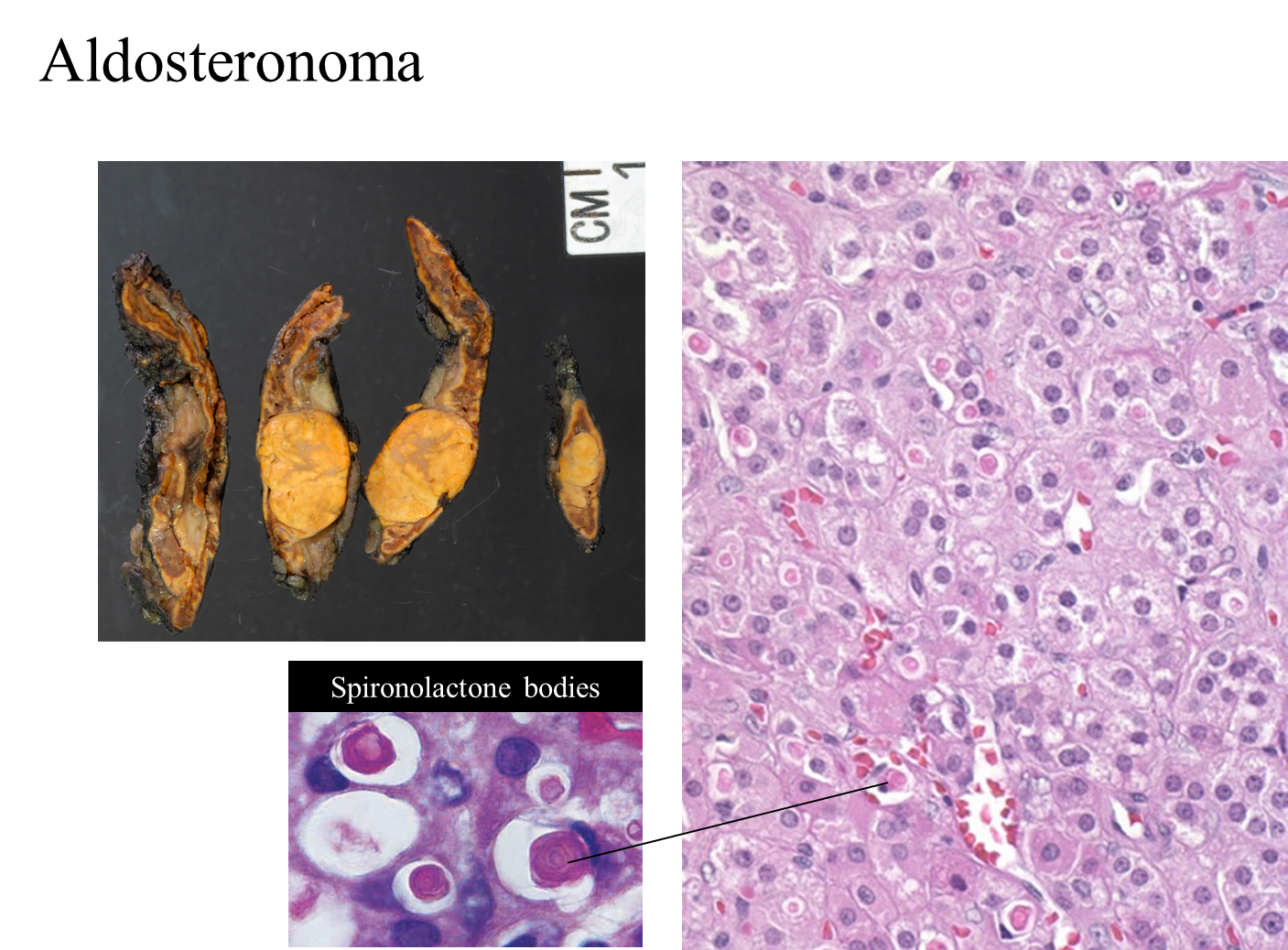
Aldosteronomas are identifiable by the presence of spironolactone bodies following treatment of spironolactone
1) Spironolactone is an aldosterone antagonist and cause unusual inclusions within the zona glomerulosa
What are the histological features of pheochromocytoma?
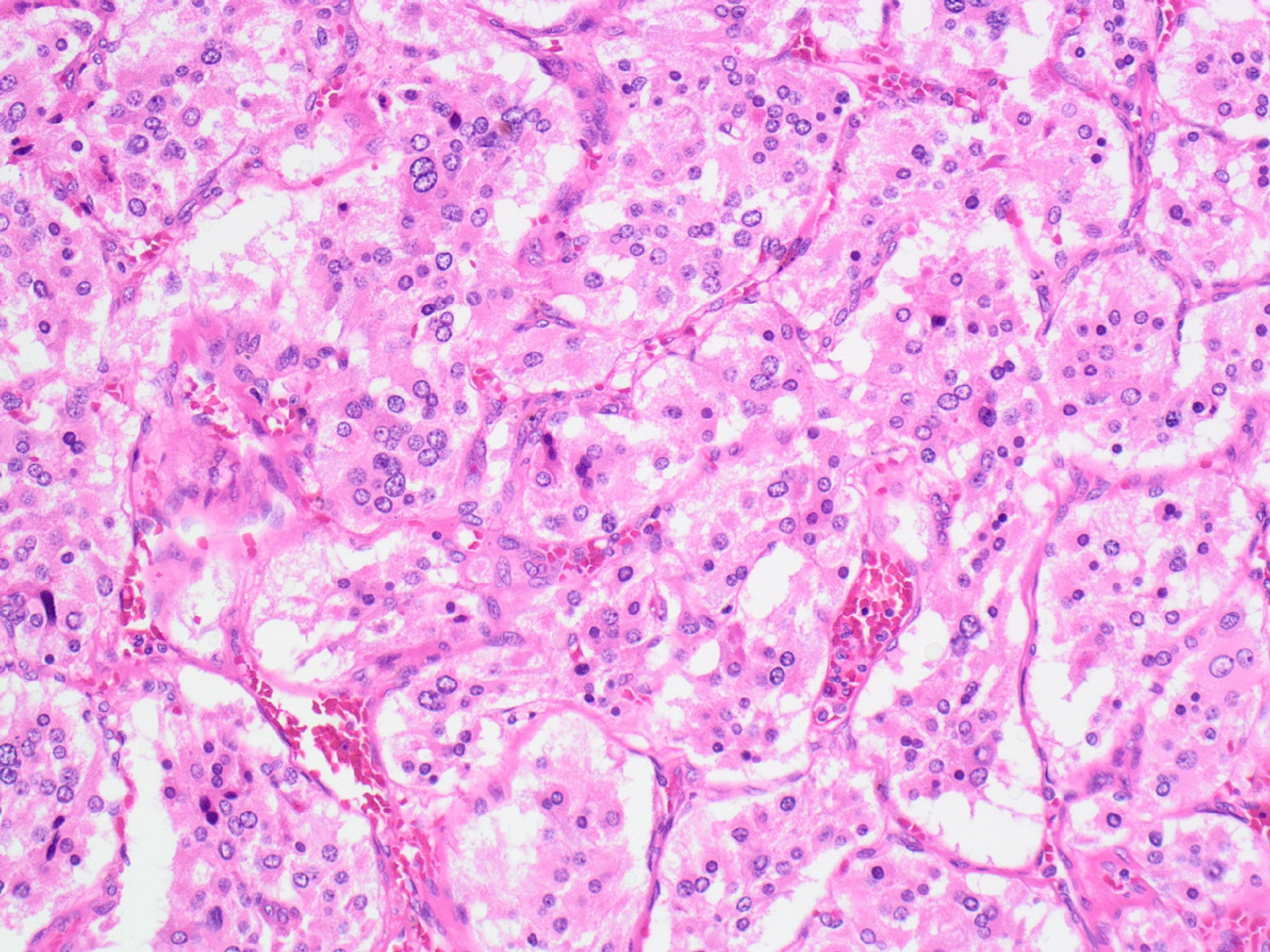
Pheochromocytoma are identified on histology by Zellballen patterns
→ tumor cells arranged in a nested/zellballen architecture and separated by stroma
1) Also have salt and pepper chromatin within the nuclei due to its origin as a neuroendocrine neoplasm