Bacterial Meningitis and Anthrax
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
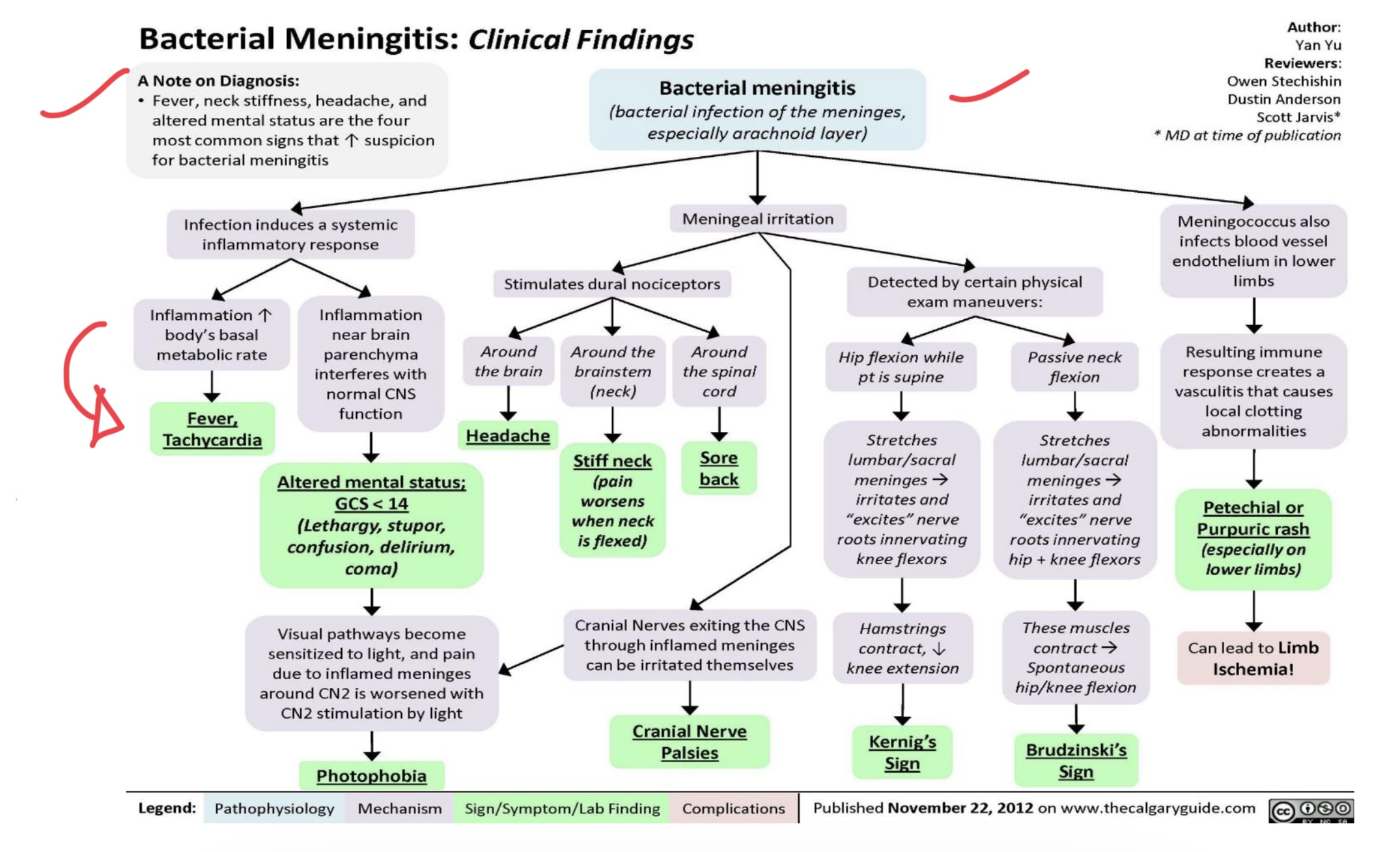
Bacterial Meningitis
life-threatening infection of the meninges caused by bacterial pathogens
Streptococcus pneumoniae
Neisseria meningitidis
Haemophilus influenzae type B
Listeria monocytogenes
BACTERIAL PATHOGENS
Most common in adults
Common in young adults and outbreaks
Common in unvaccinated children
in neonates, elderly, and immunocompromised
5
Bacterial Meningitis highest in children under _____ years and elderly
Bacterial Meningitis
Bacteria colonize the nasopharynx, invade the bloodstream, and cross the blood- brain barrier
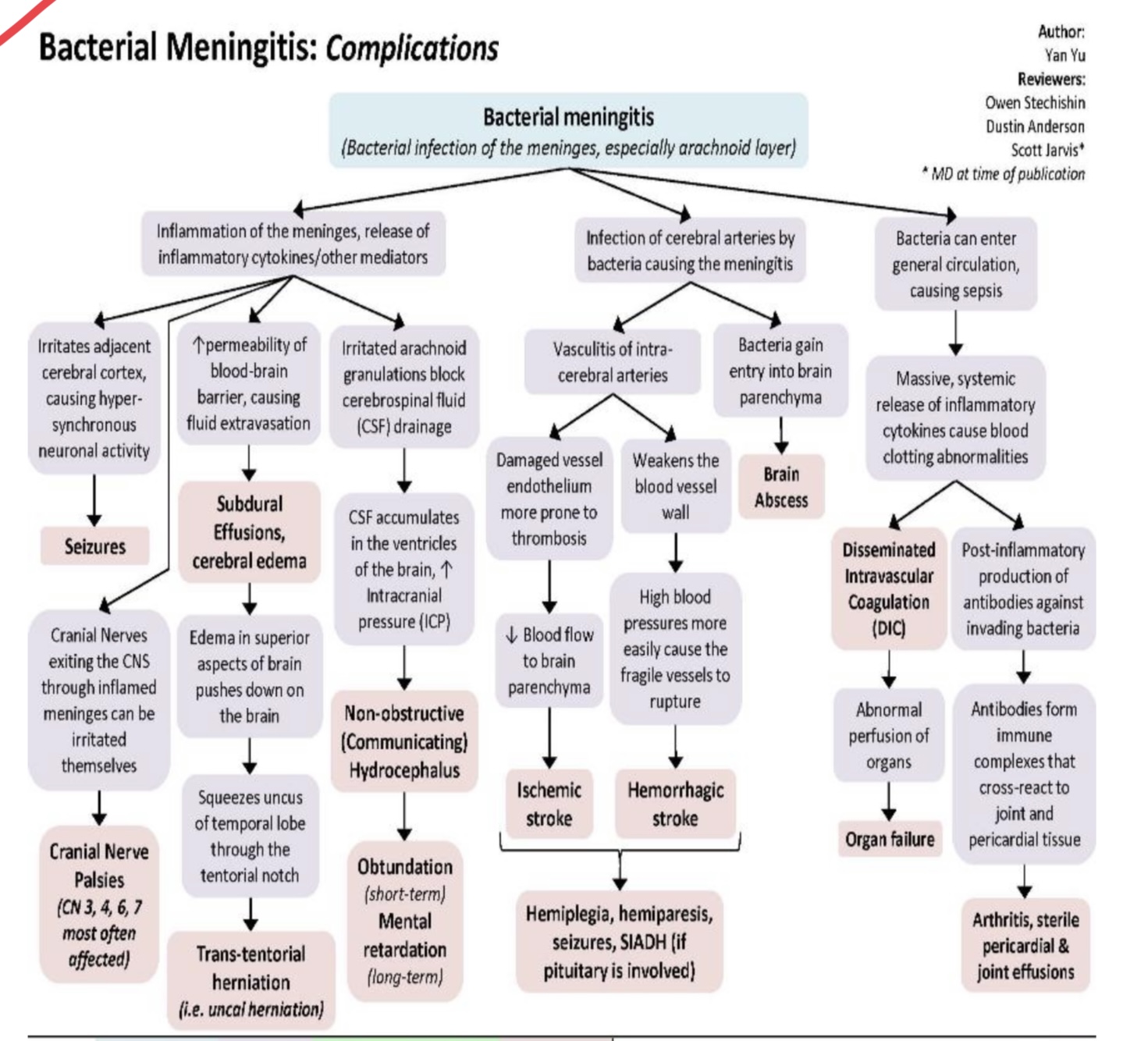
Leads to inflammation, increased intracranial pressure (ICP), and neuronal damage.
Brain edema
hydrocephalus
septic shock
neurological sequelae (hearing loss, cognitive impairment).
Major Complications of Bacterial Meningitis (4)
Fever
Neck Stiffness
Altered Mental Status
Bacterial Meningitis Classic Triad
Bacterial Meningitis
An infection of the membranes that protect the brain and spinal cord.
During Childbirth
Coughing or sneezing
Sharing Saliva
Eating contaminated food
How does it spread? (4)
Meningococcal vaccine (MenACEY and MenB)
Pneumococcal Vaccine (PCV15 or PCV20)
Haemophilus influenzae serotype B (Hib) Vaccines
Bacille Calmette-Guerin (BCg) vaccine
Bacterial Meningitis Vaccine (4)
Meningococcal vaccine (MenACEY and MenB)
Helps protect against N. meningitidis
Pneumococcal Vaccine (PCV15 or PCV20)
Help protect against S. pneumoniae
Bacille Calmette-Guerin (BCg) vaccine
Helps protect against tuberculosis disease, but is not widely used in the United States.
Lumbar Puncture and CSF
Gram stain and culture
Blood culture
CT scan
Diagnostic Test (4)
↑ WBCs (neutrophilic predominance)
↓ Glucose
↑ Protein
Bacterial meningitis CSF findings (3)
Adults: Ceftriaxone + Vancomycin (for S. pneumoniae resistance)
Infants: Ampicillin + Cefotaxime (for Listeria coverage)
Immunocompromised: Add Ampicillin (covers Listeria monocytogenes)
Steroids (Dexamethasone): Reduces inflammation and risk of
neurological complications.
Management
Adults
Infants
Immunocompromised
Steroids
Mass Chemoprophylaxis (Rifam or Cipro)
Public Awareness campaign
Strengthening Infection Control
DOH Guidelines for Outbreak Management: (3)
Anthrax
Caused by Bacillus anthracis, a Gram-positive spore-forming bacterium.
Anthrax
Spread through contact with infected animals, contaminated
animal products, or inhalation of spores.
Agricultural regions (e.g.,Cagayan Valley, Central Luzon).
Anthrax is common in
Public Health Threat
Anthrax was classified by DOF as a
Cutaneous Anthrax
Most Common
Painless Black Eschar
Local edema and Lymphadenopathy
Inhalational Anthrax
Most Severe
Flu-like symptoms progressing to severe respiratory distress, shock, and death.
Gastrointestinal Anthrax
Severe abdominal pain, bloody diarrhea, and vomiting.
Injection Anthrax
Occurs in drug users (rare).
Culture and Gram stain of lesion, blood, or sputum
PCR or ELISA to detect anthrax toxin
Chest X-ray/CT scan
Anthrax Diagnosis (3)
Ciprofloxacin or Doxycycline (60 days)
Anthrax Management
First line Antibiotics
Raxibacumab (severe cases)
Antitoxin therapy
60-day antibiotic therapy + Anthrax vaccine.
Post-Exposure Prophylaxis