Breast Disorders (Fibrocystic Breast Changers, Fibroadenoma, and Breast Cancer) | NURS230
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
89 Terms
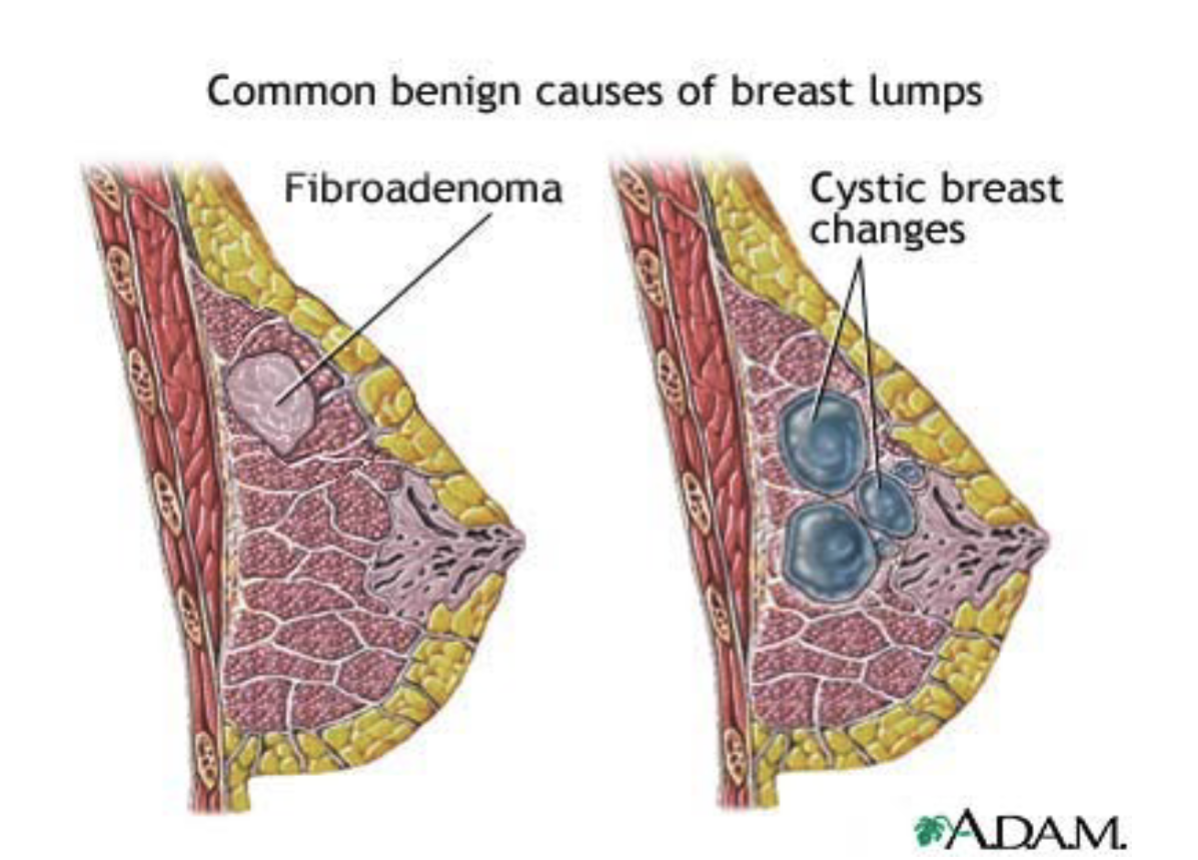
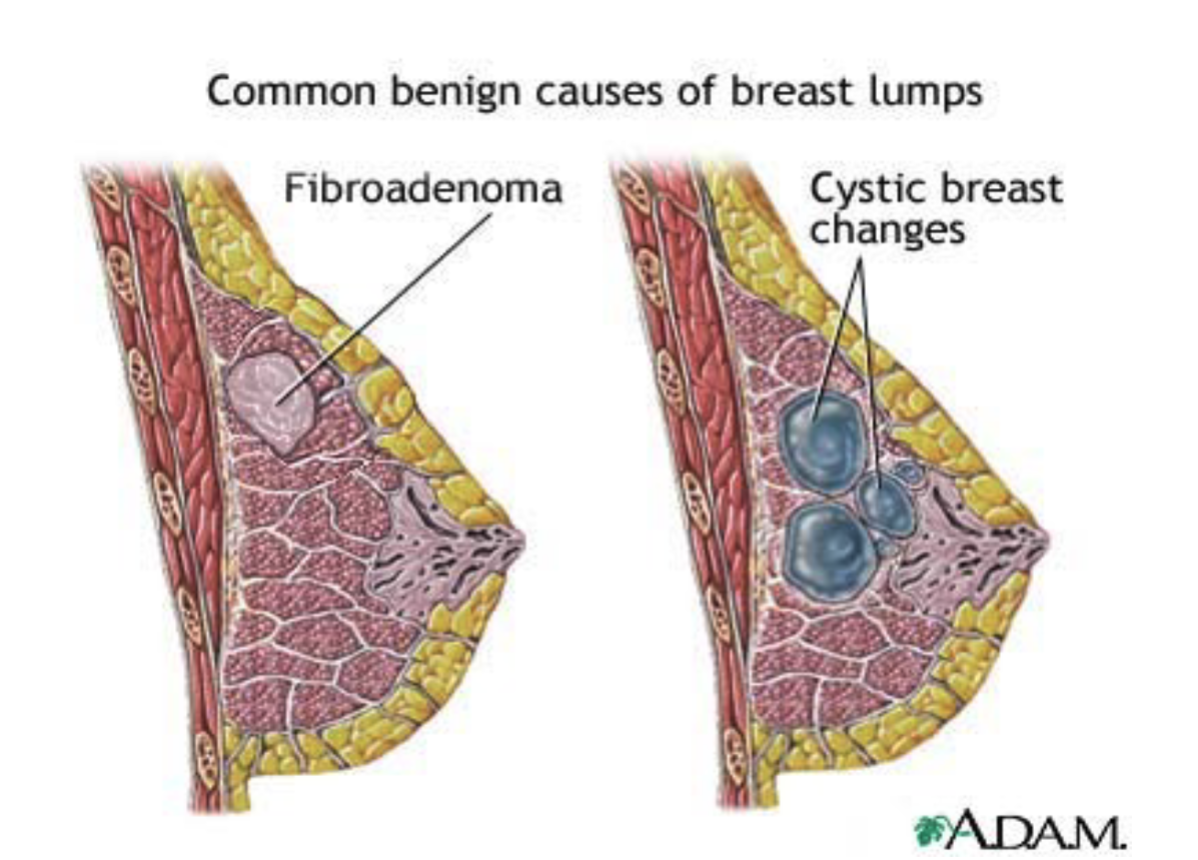
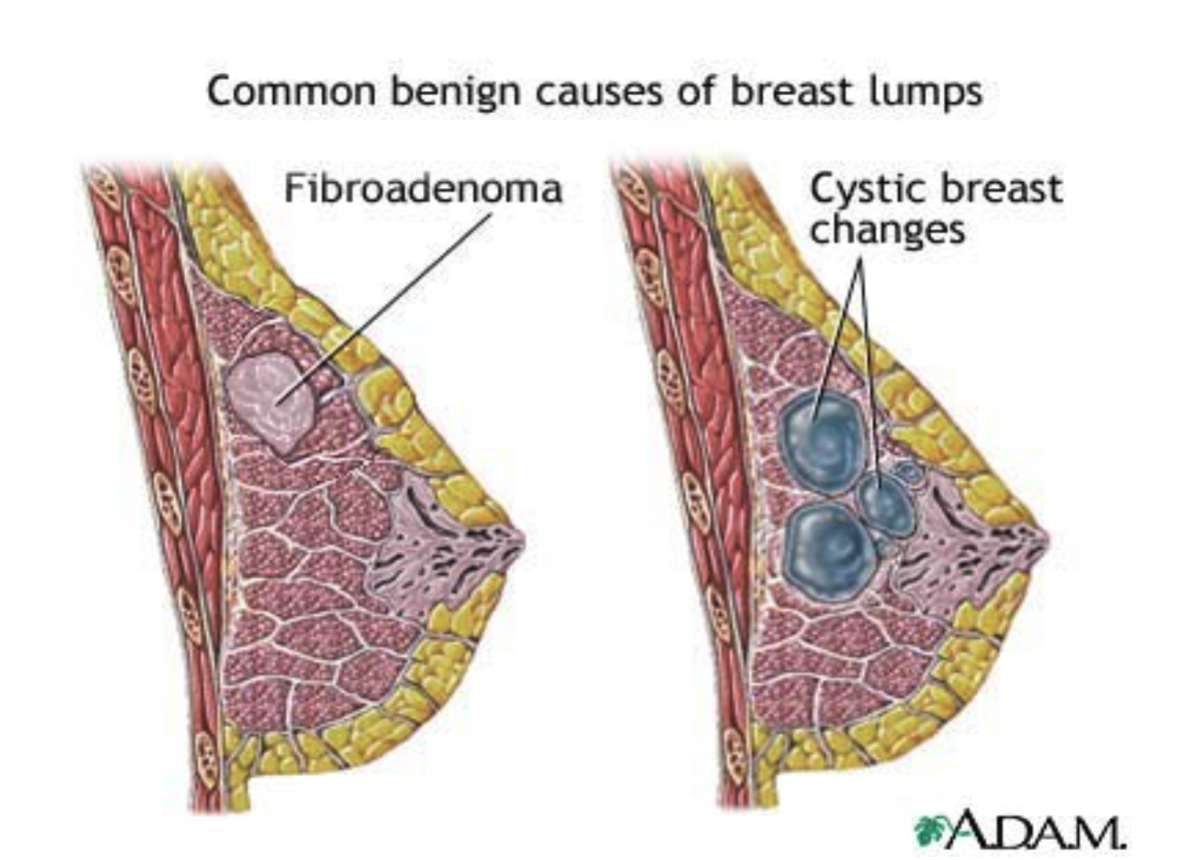
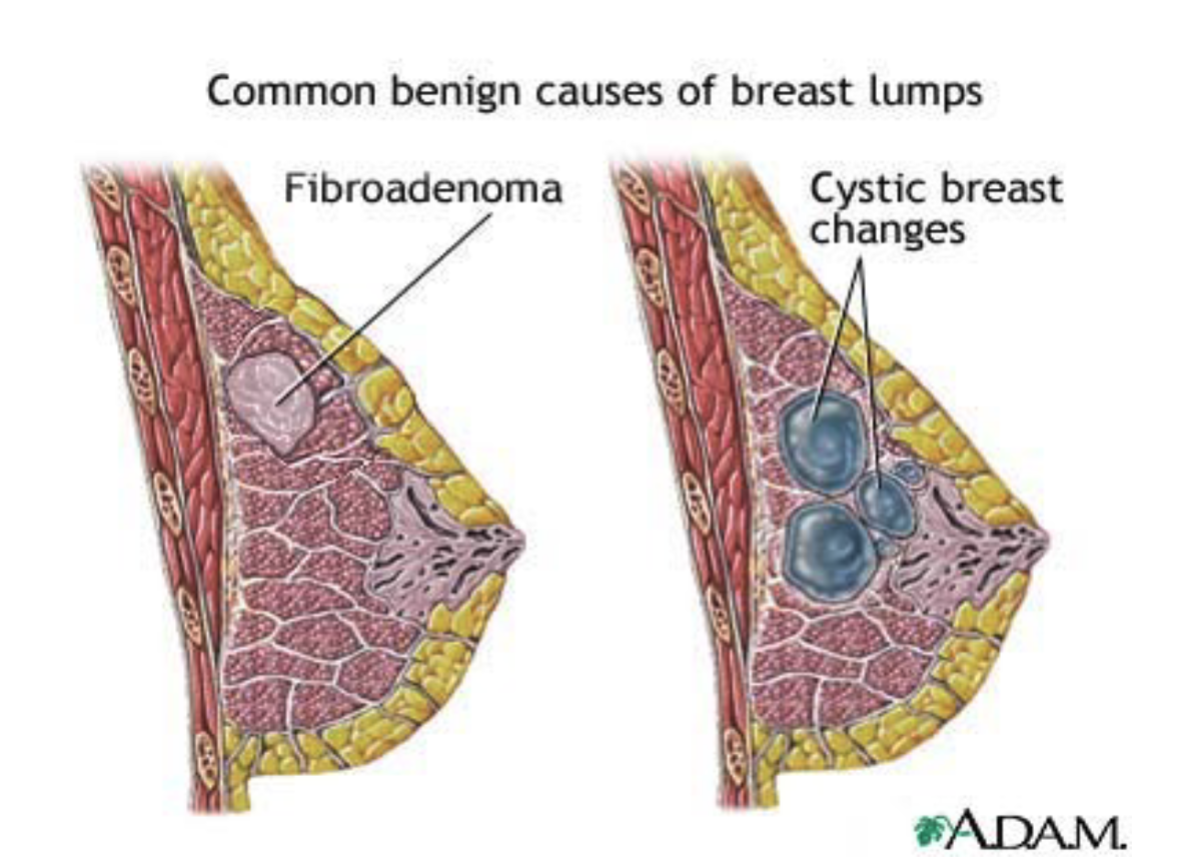
what are fibrocystic breast changes?
benign (non-cancerous breast changes caused by hormonal fluctation that create cysts, fibrosis, and tissue thickening
who is the most likely to experience fibrocystic breast changes?
premenopausal women ages 20-50
what causes fibrocystic breast changes?
monthly estrogen fluctuations during the menstrual cycle
what breast tissue changes occur in fibrocystic breast disease?
development of cysts, fibrosis, hyperplasia
what is the typical pattern of fibrocystic cysts?
usually multifocal, bilateral, and can be micro (tiny) or macro (1-2 inches)
do fibrocystic breast changes increase breast cancer risk?
no, they do not increase cancer risk
what are the key clinical presentation of fibrocystic breast changes?
breast pain
rubbery, ill-defined, tender lumps
usually in the upper-outer quadrant
often multifocal and bilateral
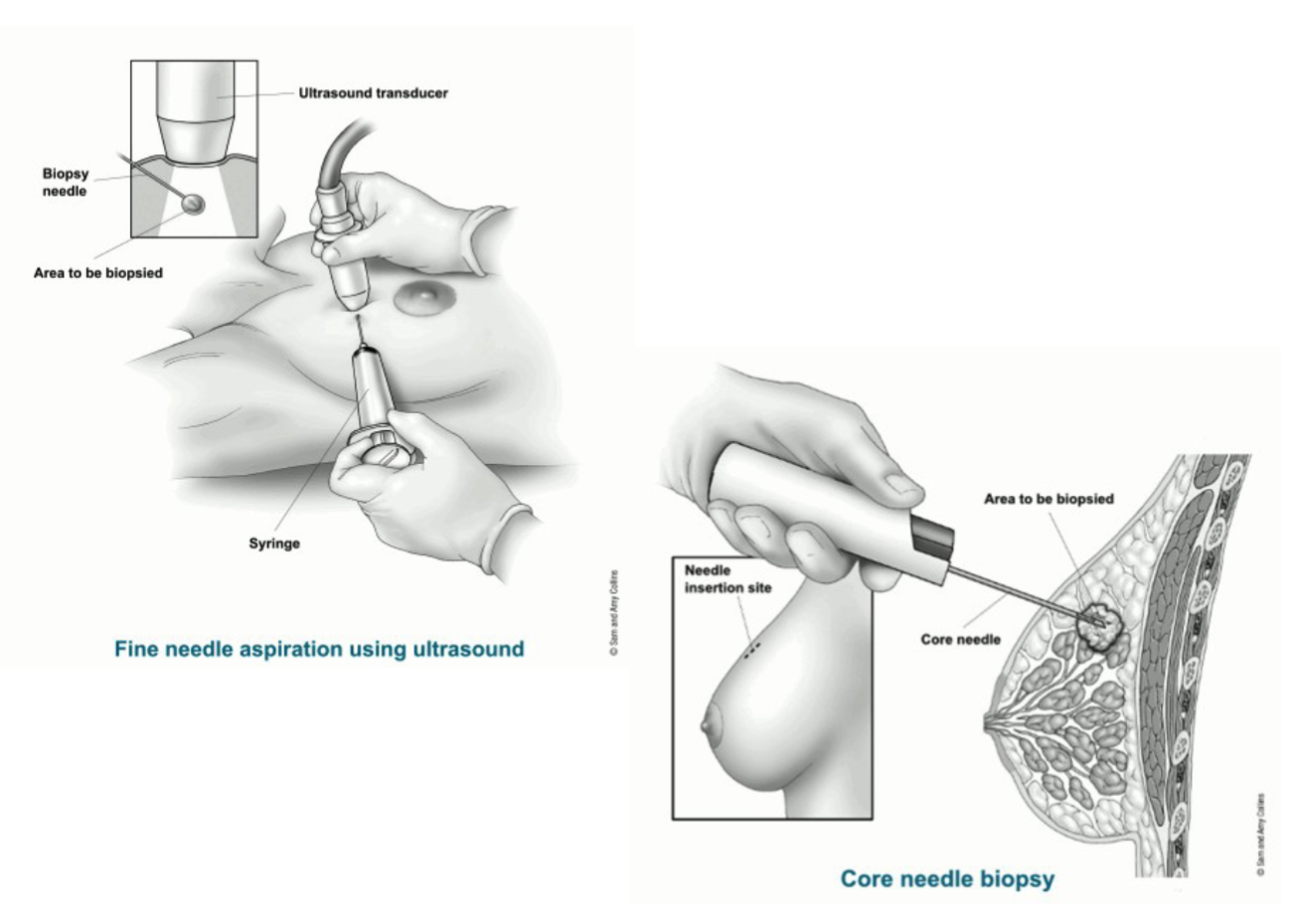
how are fibrocystic breast changes diagnosed?
breast ultrasound to confirm
may also need a mammogram or fine-needle biopsy with aspiration
what are the treatments options for fibrocystic breast changes?
oral contraceptive → stabilize estrogen levels which reduces the hormonal fluctuation that trigger cyst formation and breast pain
vitamins supplements - can reduce breast tenderness and improve symptoms related to cyclic changes
diuretics - decrease fluid retention, which helps reduce breast swelling and discomfort around the menstrual cycle
supportive bra and breast support

what is a fibroadenoma? what is the key physical features of a fibroadenoma?
a common benign breast lesion made of glandular and stromal tissues
glandular tissues are the tissues that make milk
stromal tissue is the tissue that provides support - basically the padding and the scaffolding around the milk system
key characteristics - a solid mass that is unattached to surrouunding tisse (moves easily on exam; mobile)
who most commonly develops fibroadenomas?
women in their 20s-30s, though they can occur at any age
what hormonal factor is linked to fibroadenoma development?
changes in estrogen levels
how are fibroadenomas evalulated/diagnosed?
ultrasound or needle aspiration may be done to rule out cancer
is a fibroadenoma a form of fibrocystic breast changes?
No.
Fibroadenoma = one solid, benign tumor (mobile, made of glandular + stromal tissue).
Fibrocystic breast changes = multiple cysts and tissue changes due to hormones (tender, often bilateral).
Both are benign, but they are different conditions.
what is the malignancy risk of a fibroadenoma?
less than 1% malignant
what does a fibroadenoma typically look/feel like on exam?
a discrete, solitary lump (usually 1-15 cm), round, firm, freely moveable, and non-tender; commonly in the upper outer quadrant
what can happen to a fibroadenoma over time
it may stop growing or shrink on its own; providers usually monitor it once cancer is ruled out.
when is treatment/excision indicated for a fibroadenoma?
tt can be excised under local anesthesia if it grows, becomes large, or changes breast shape.
what is the ranking of breast cancer as a cause of cancer death in U.S. women?
It is the 2nd leading cause of cancer death in U.S. women.
what is a woman’s lifetime risk of developing breast cancer?
1 in 8, and the risk increases with age.
what percentage of breast cancer cases occur after age 50?
75%.
what are the two main categories of breast cancer?
non-invasive and invasive.
what percentage of breast cancers are non-invasive?
20%
what defines non-invasive breast cancer?
malignant cells remain within the ducts (do not invade surrounding tissue).
what is the most common type of non-invasive breast cancer?
ductal carcinoma in situ (DCIS).
what is another form of non-invasive breast cancer besides DCIS?
lobular carcinoma in situ (LCIS)
what percentage of breast cancers are invasive?
80%
what defines invasive breast cancer?
malignant cells start in the epithelial lining of ducts or lobules, then penetrate surrounding breast tissue.
what is the most common type of invasive breast cancer?
Infiltrating ductal carcinoma
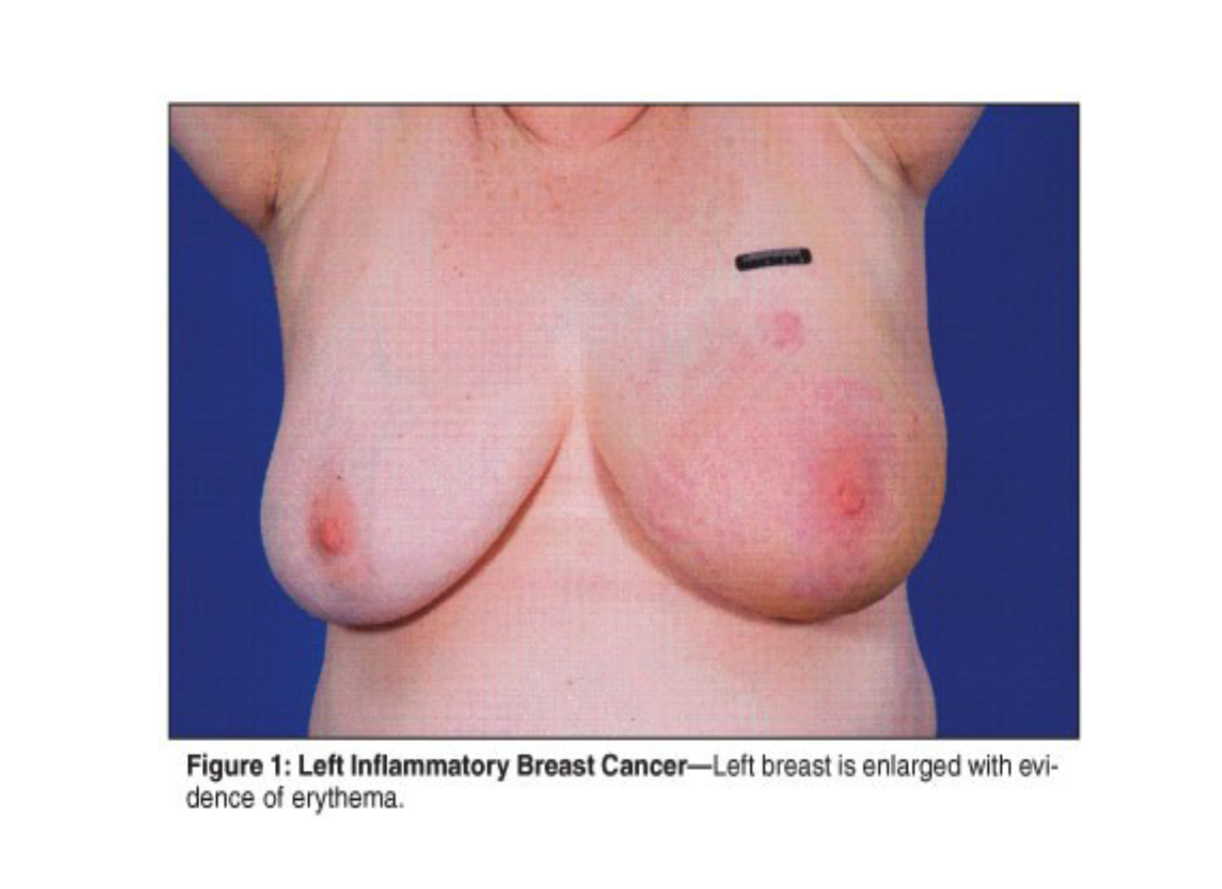
what is the most malignant type of breast cancer?
inflammatory breast cancer
what hormone receptors are used in breast cancer classification?
estrogen receptor (ER) and progesterone receptor (PR) — classified as positive (+) or negative (−)
what does HER2 (+) or (−) mean in breast cancer?
it refers to the presence or absence of human epidermal growth factor receptor 2, which can affect growth and treatment response.
what is triple-positive breast cancer?
cancer that is estrogen receptor (+), progesterone receptor (+), and HER2 (+).
what is triple-negative breast cancer?
cancer that is estrogen receptor (−), progesterone receptor (−), and HER2 (−) — more aggressive and harder to treat.
is triple positive or triple negative more aggressive?
triple negative
Because it lacks estrogen receptors, progesterone receptors, and HER2, meaning:
No targeted therapies (like hormone therapy or HER2-targeted drugs) work on it
Tends to grow faster and spread earlier
Has a higher risk of recurrence
what is the biggest risk factor for breast cancer?
being female
how does age affect breast cancer risk?
risk increases with age, specially, more than 65
what genetic factors increase breast cancer risk?
family history and BRCA1/BRCA2 mutations
how does breast density affect breast cancer risk?
dense breast tissue increase risks by making mammograms harder to interpet thus making it harder to catch actual cancer growth
what environmental ecposure increase risk for breast cancer?
radiation exposureh
ow do menstrual factors affect breast cancer risks?
early menarche or late menopause = longer estrogen exposure, leading to increased risk
how does pregnancy history affect breast cancer risk?
nulliparity or having the first child after the age of 30 increases risk due to higher exposure to estrogen at an older age
what lifestyle factors increase breast cancer risk?
obesity and alcohol use
what is the ACS screening recommendation for women ages 40–44?
they should have the option to start annual mammograms.
how often should women ages 45–54 be screened?
Annually (like the main difference from 40-44 is that unlike that the people in 40-44 can do it if they want ot not while 45-54 they should do it!!)
What is the screening recommendation for women 55 and older?
What is the screening recommendation for women 55 and older? Why is mammogram screening no longer annual after age 55?
Transition to biennial (every 2 years) screening or continue annual screening if preferred.
Because after menopause, breast tissue becomes less dense, and breast cancer tends to grow more slowly, so screening every 2 years is still effective—but women can continue annual screening if they prefer.
when should women stop screening mammography?
Continue as long as they are in good health and have a 10+ year life expectancy.
what is the first step in a breast cancer assessment?
assess risk factors (age, family history, BRCA, radiation exposure, reproductive history, lifestyle, etc.).
Why ask about past history of breast masses during breast assessment?
To identify previous lumps, biopsies, or breast diseases that may increase risk or guide evaluation.
what does “health maintenance practices” include in breast cancer assessment?
Screening behaviors: mammograms, self-breast exams, clinical breast exams, and follow-up history.
what is included in the breast cancer physical exam?
Inspection and palpation of the breasts and lymph nodes (axillary, supraclavicular, infraclavicular)
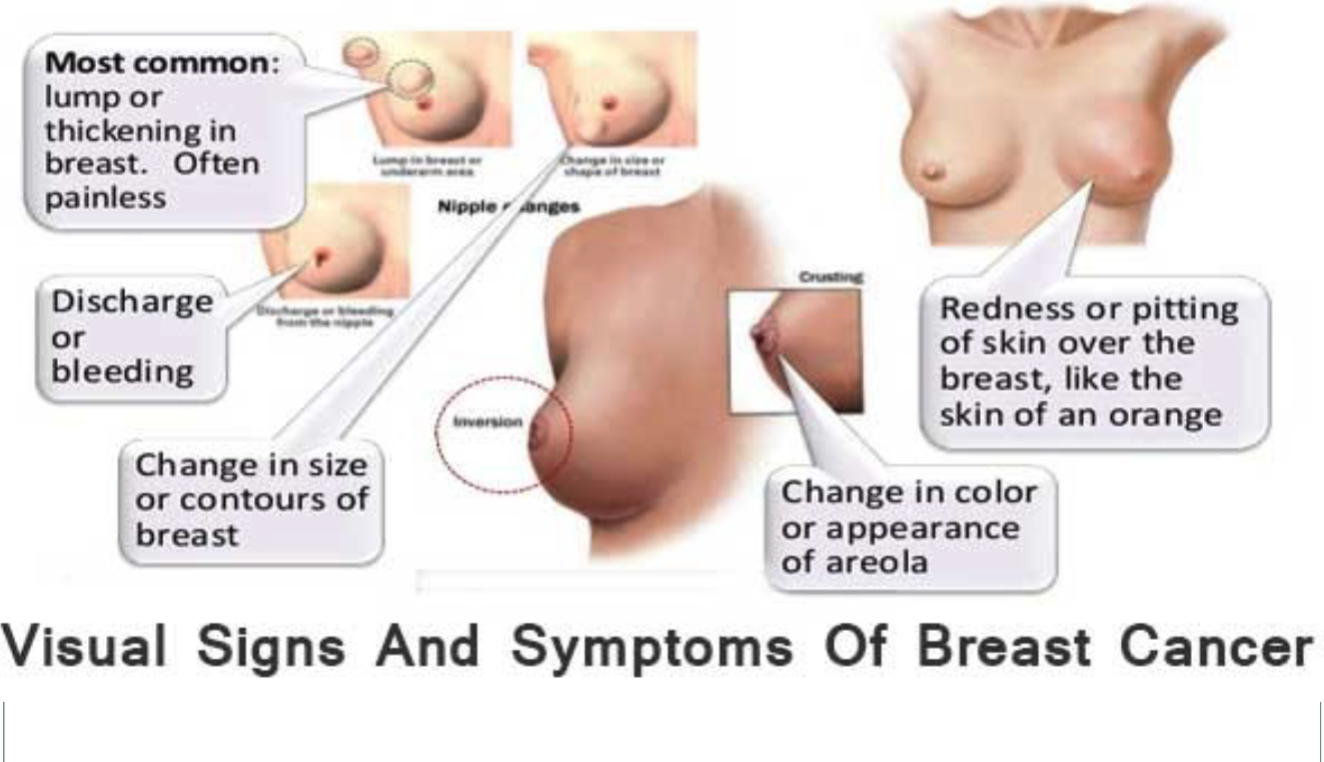
what are the visual signs and symptoms of breast cancer?
lump or thickening in breast (often painless)
discharge or bleeding
change in contour of breast =
redness or pitting of skin over the breast, like the skin of an orange”
change in color or appearance of areola
why are tumor markers used in breast cancer?
they help track the cancer over time — like checking if treatment is working or if cancer has come back.
(Not good for screening, but good for monitoring.)
why is a mammogram important in breast cancer?
It’s the main screening tool because it can catch tiny calcifications or lumps before they can be felt.
why use an ultrasound in breast cancer workup?
It tells you what type of lump it is —
Fluid-filled = cyst
Solid = possible tumor
It’s like asking, “Is the lump squishy or solid?”
what’s the difference between a mammogram, ultrasound, MRI, PET scan, CT scan, and chest X-ray in breast cancer evaluation? (when to use what?)
🟦 Mammogram — Best for Screening
First-line test for most women
Detects tiny calcifications and early changes
Works best when breast tissue is not too dense
Think: “Standard screening test.”
🟩 Ultrasound — Tells You What the Lump Is
Helps differentiate solid vs. cyst
Used when a lump is found or breast tissue is dense
Think: “Is this lump fluid or solid?”
🟪 MRI — Detailed View, Dense Breasts
Very sensitive, picks up changes mammograms might miss
Best for dense breasts, high-risk patients, or unclear findings
Think: “Super-detailed camera.”
🟧 PET Scan — Looks for Active Cancer
Detects metabolically active (fast-growing) cancer cells
Used for staging (seeing how far it has spread)
Think: “Where is the cancer active in the body?”
⬛ CT Scan — Checks for Organ Metastasis
Used to look for spread to bone, liver, brain
Not a primary breast imaging tool
Think: “Where has it traveled?”
⬜ Chest X-ray — Checks the Lungs
Looks for lung metastasis
Quick and simple
Think: “Has it gone to the lungs?”
⭐ Mini-Memory Trick
Mammogram = first look
Ultrasound = what kind of lump?
MRI = dense breasts / very detailed
PET/CT = staging for spread
CXR = lungs
why use MRI or PET scans?
They give a more detailed look, especially in dense breasts, where mammograms are harder to read.
Also good for checking how far cancer may have spread.
why get a chest X-ray for breast cancer?
To check if the cancer has spread to the lungs—a common metastasis site.
why is a CT scan done in breast cancer workup?
To look for spread to major organs:
Bone
Liver
Brain
It’s like “full-body staging.”
Why check estrogen/progesterone receptor status during an assessment of the breast?
It tells whether the cancer feeds on hormones.
If it’s ER/PR positive → hormone therapy will work (like shutting off the tumor’s food supply).
what does Grade 1 breast cancer mean?
Score: 3–5
Cells look more like normal breast cells (well differentiated)
Slow-growing
Less likely to spread
what does Grade 2 breast cancer mean?
Score: 6–7
Moderately differentiated
Intermediate growth and behavior
what does Grade 3 breast cancer mean?
Score: 8–9
Cells look very abnormal (poorly differentiated)
Fast-growing
More likely to spread
what pieces of information are used in breast cancer staging?
T = Tumor size
N = Lymph node involvement
M = Metastasis
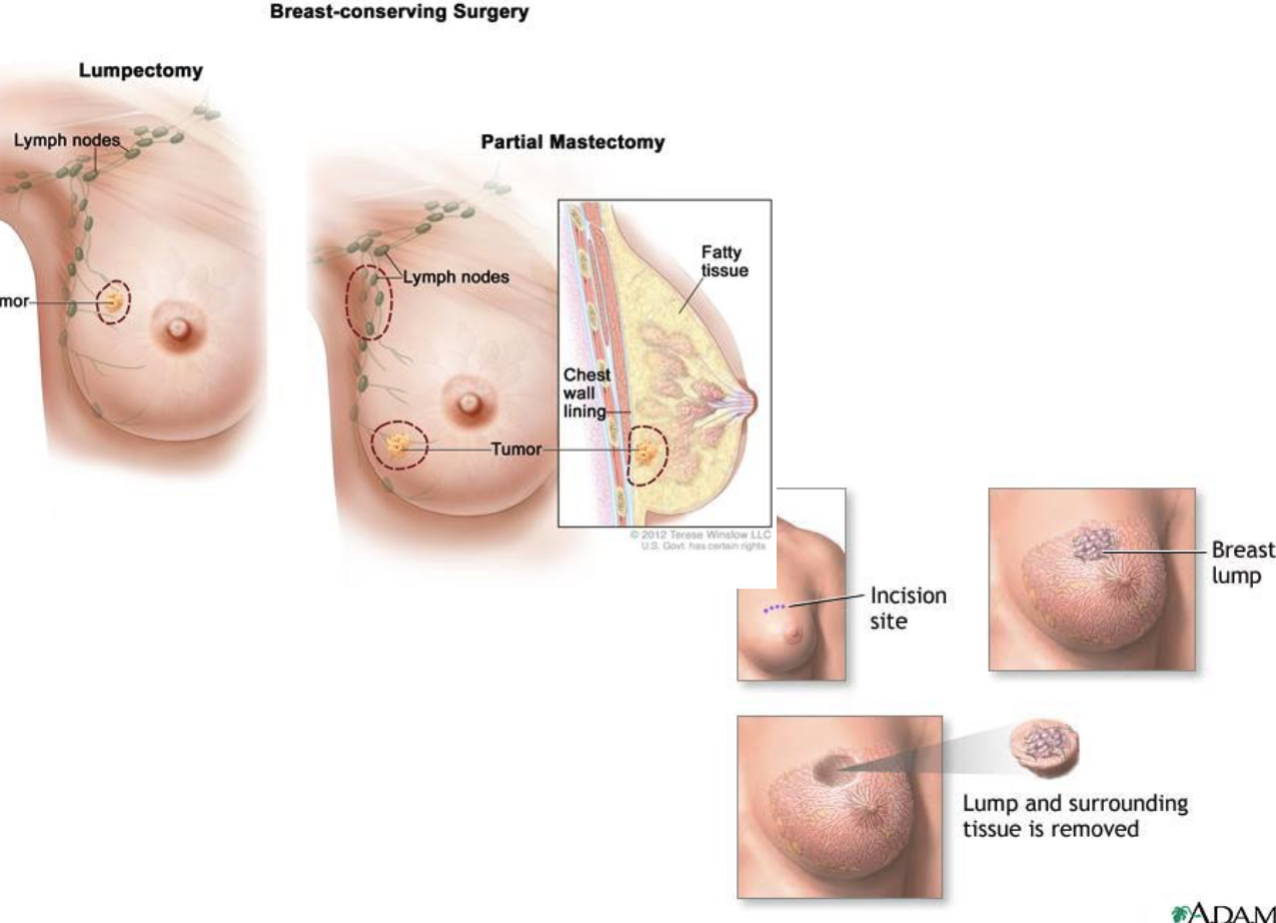
what is breast-conserving surgery (lumpectomy)?
removal of only the tumor + a small rim of tissue, keeping most of the breast.
May be done with or without:
Axillary lymph node dissection (LND)
Sentinel lymph node biopsy (SLND)
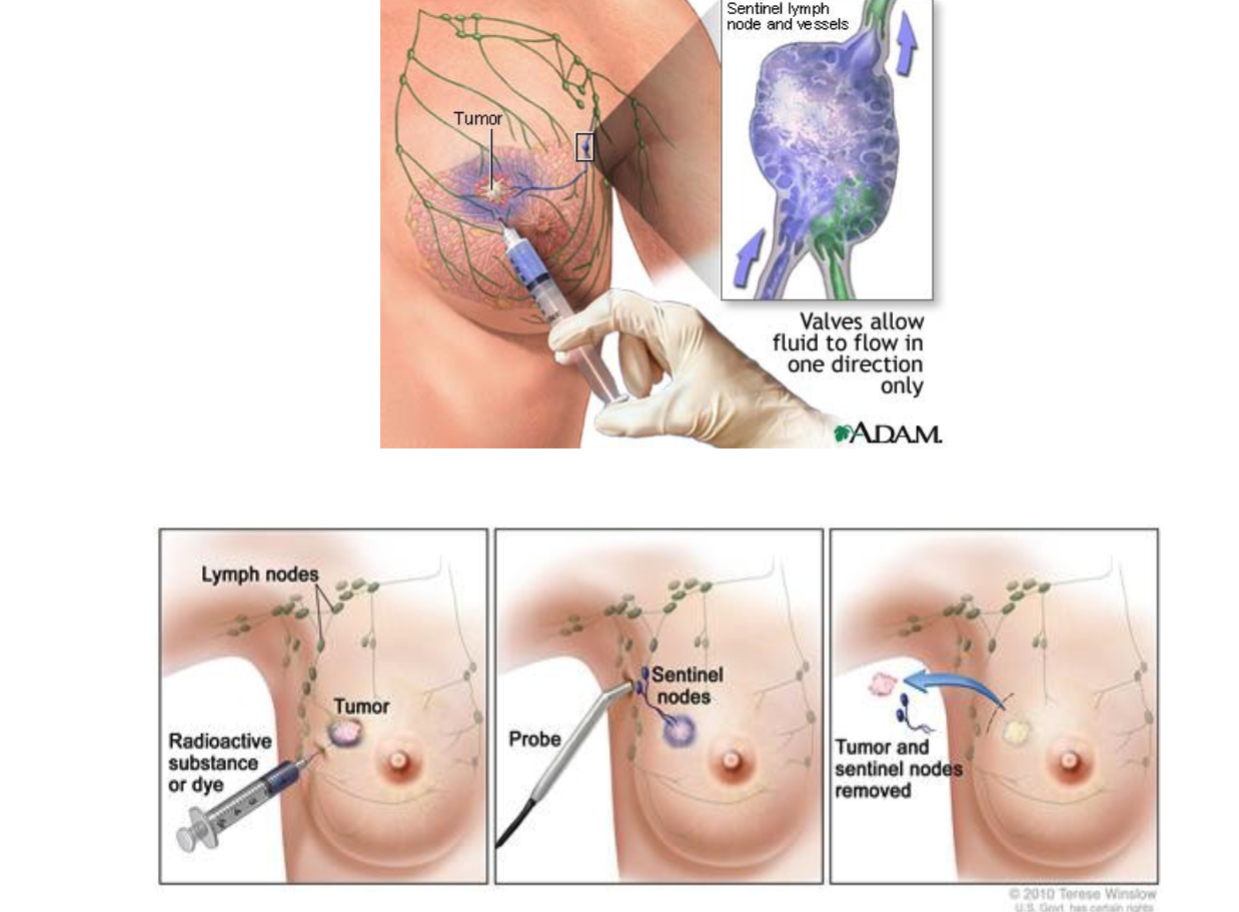
why perform a sentinel lymph node biopsy?
to check if cancer has spread to the first draining lymph node, which helps avoid removing unnecessary nodes.
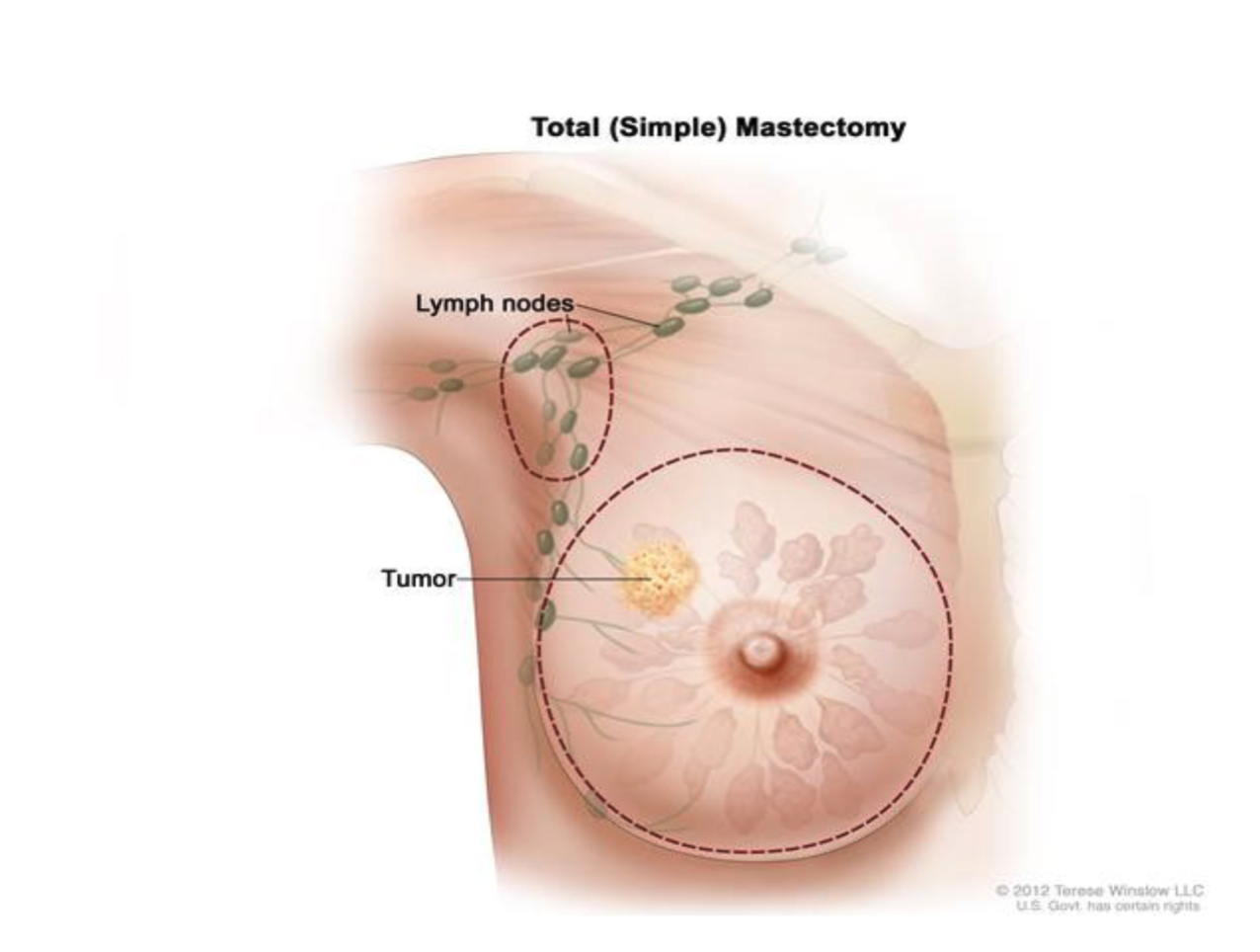
what is a simple mastectomy?
removal of the entire breast, but no lymph nodes and no muscle removed.
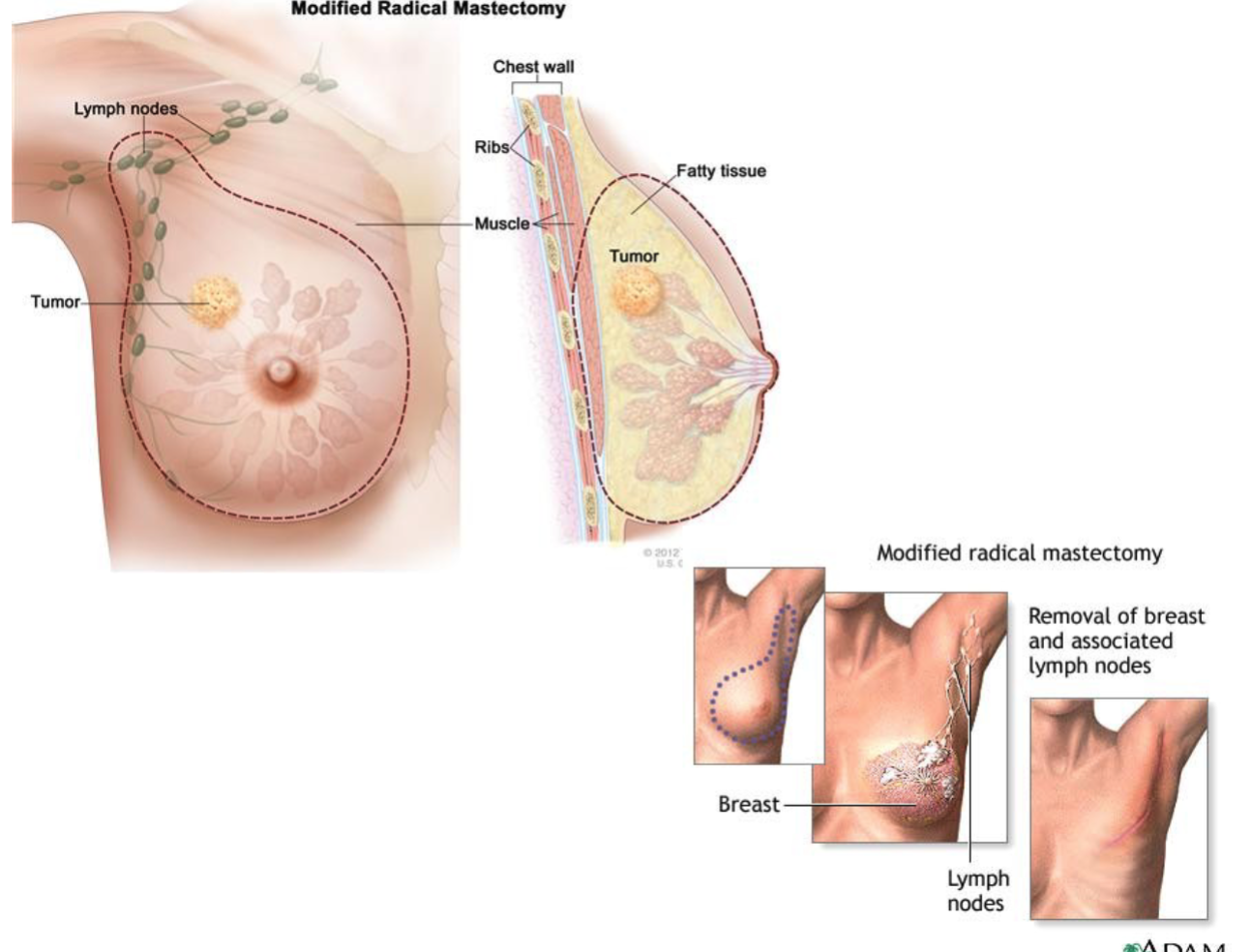
what is a modified radical mastectomy?
Removal of:
The entire breast
Axillary lymph nodes
But chest muscles are left in place.
what is the main focus of pre-op teaching before breast cancer surgery?
Preparing the patient for what to expect (procedure, drains, pain, mobility limits, follow-up care).
why refer the patient to “Reach for Recovery” before surgery?
provides emotional support, peer mentors, and practical info from women who had similar surgery.
what is the nursing priority for post-op dressings?
monitor for bleeding, drainage, and signs of infection.
why are drains needed after breast surgery?
To prevent fluid buildup (seroma/hematoma).
Nursing role: empty, measure, and record output.
what’s the goal of post-op pain management?
Keep pain controlled so the patient can move the arm, breathe deeply, and recover safely.
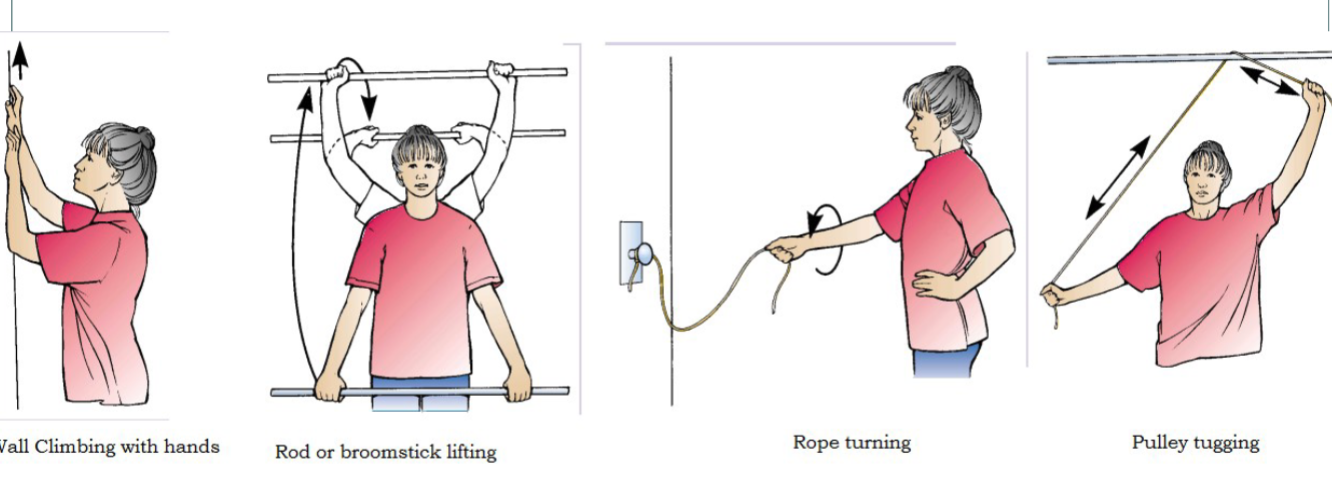
why are ROM exercises important after breast cancer surgery?
Prevent arm stiffness, improve lymph drainage, and reduce risk of lymphedema.
why is psychosocial support essential after breast surgery?
Body image changes, fear of cancer recurrence, and emotional distress are common.
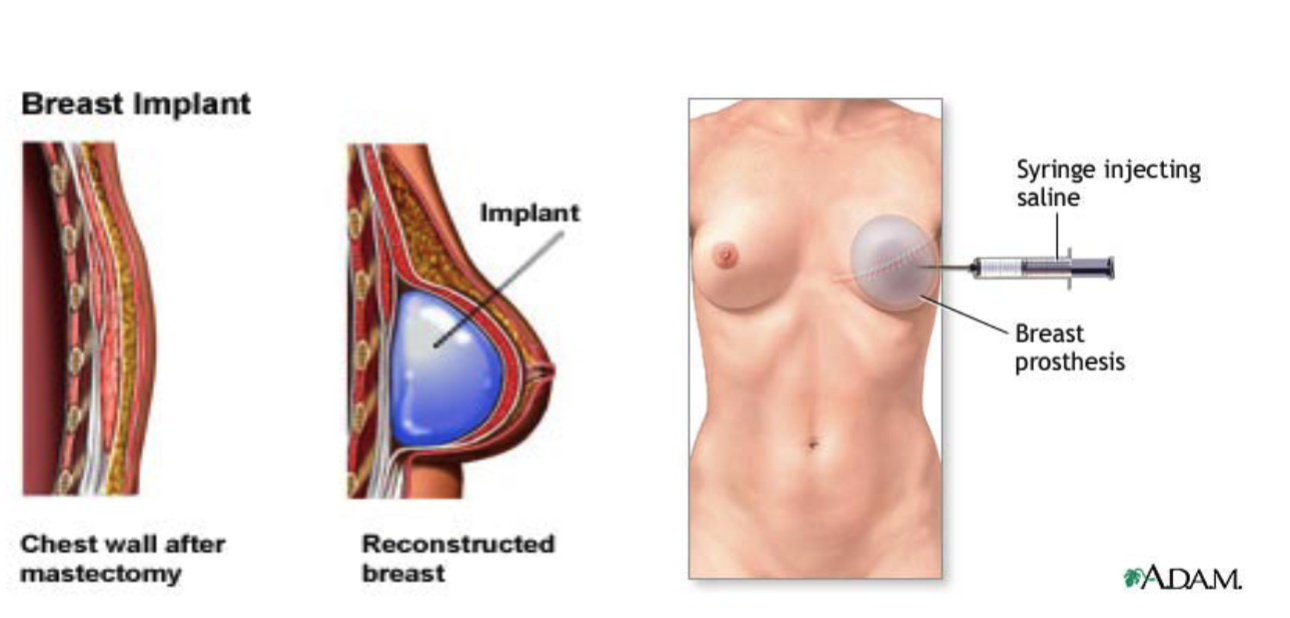
what is a breast prosthesis?
a removable artificial breast placed inside the bra.
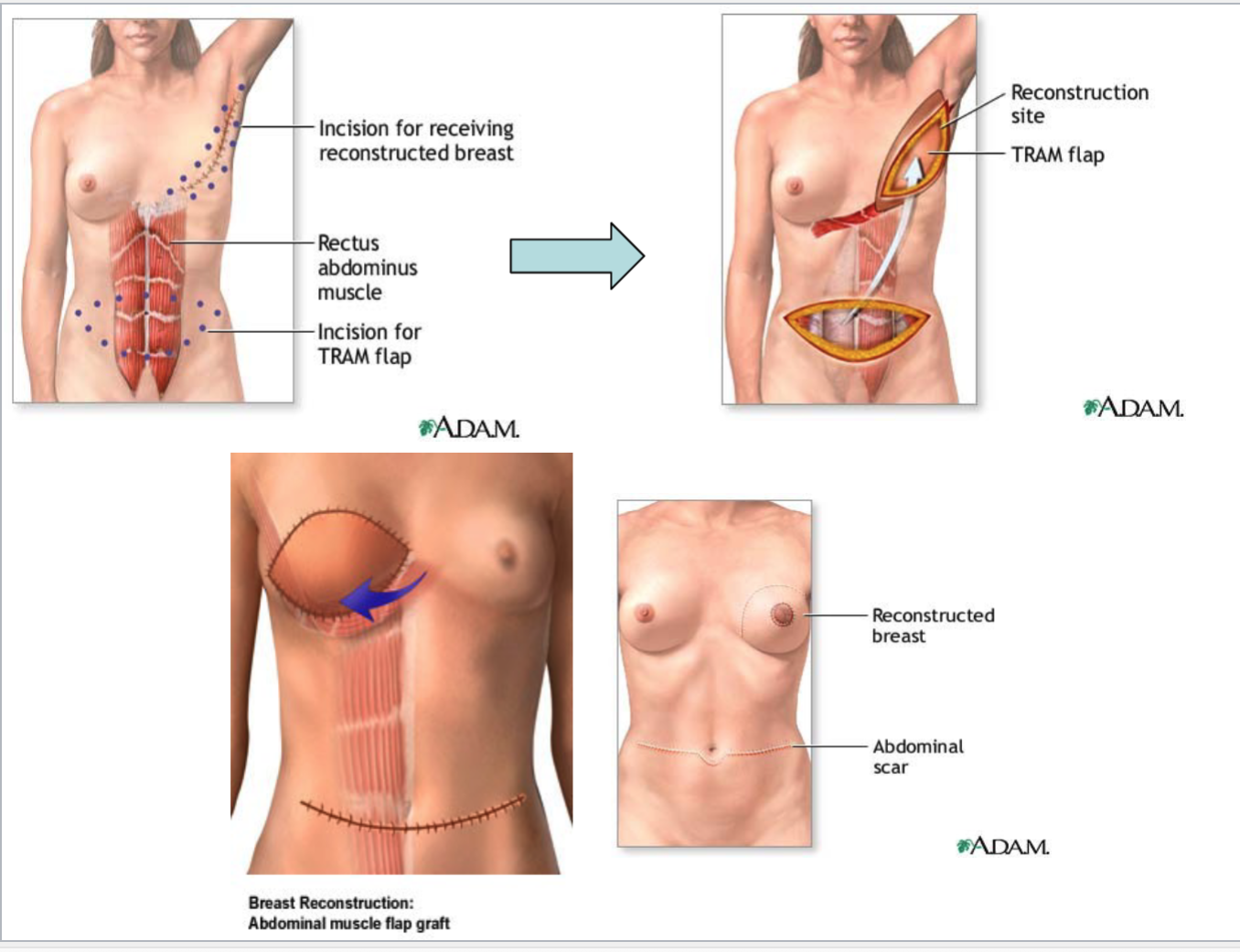
what are myocutaneous flap procedures for breast reconstruction?
Using the patient’s own skin, fat, and muscle from another body area to create a breast mound.
Common types:
TRAM flap — tissue from the abdomen
Latissimus dorsi flap — tissue from the upper back
what is a tissue expander?
a temporary device placed under the skin and gradually filled with saline to stretch the tissue before placing a permanent implant.
what is nipple reconstruction?
Surgery to rebuild the nipple and areola using skin grafts or tattooing.
what is the purpose of targeted therapy in breast cancer?
To target specific characteristics of cancer cells (HER2, hormone receptors, BRCA mutations) so treatment hits the cancer without harming as many normal cells.
what drugs treat HER2 (+) breast cancer?
Trastuzumab (Herceptin) and Pertuzumab (Perjeta).
what targeted therapies are used for ER/PR (+) but HER2 (–) cancers?
Ibrance, Kisqali, Verzenio (CDK4/6 inhibitors).
what drug is used for breast cancer with BRCA mutations?
Olaparib (Lynparza), a PARP inhibitor.
what is the purpose of hormonal therapy for breast cancer?
to reduce estrogen available to ER/PR (+) tumors, starving them of their growth signal.
why is chemotherapy used in breast cancer?
To kill rapidly dividing cancer cells—especially used in early-stage cancers to reduce recurrence and in advanced cancers to control spread.
what anthracyclines are used for early breast cancer?
Doxorubicin (Adriamycin) and Epirubicin (Ellence).
what taxanes are used for early breast cancer?
Paclitaxel (Taxol) and Docetaxel (Taxotere).
what symptoms do nurses help manage during breast cancer treatment?
Side effects from surgery, chemotherapy, radiation, hormonal therapy, or targeted therapy (e.g., pain, nausea, fatigue, skin changes, neuropathy).