Primer on Musculoskeletal Outcome Measures and Instruments
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
48 Terms
APTA Vision statement
Transforming society by optimizing movement to improve the human experience
Evidence Based Practice (EBP): patient values
are unique preferences, concerns and expectations each patient brings to a clinical encounter and which must be integrated into clinical decisions if they are to serve the patient
Evidence Based practice (EBP)
integration of:
current best research evidence
your clinical expertise
patient values
formulation of an answerable clinical question:
PICO
patient (or population, or problem)
intervention (or comparison)
outcomes
the triple aim
better case, better health, and lower costs
guide to physical therapist practice
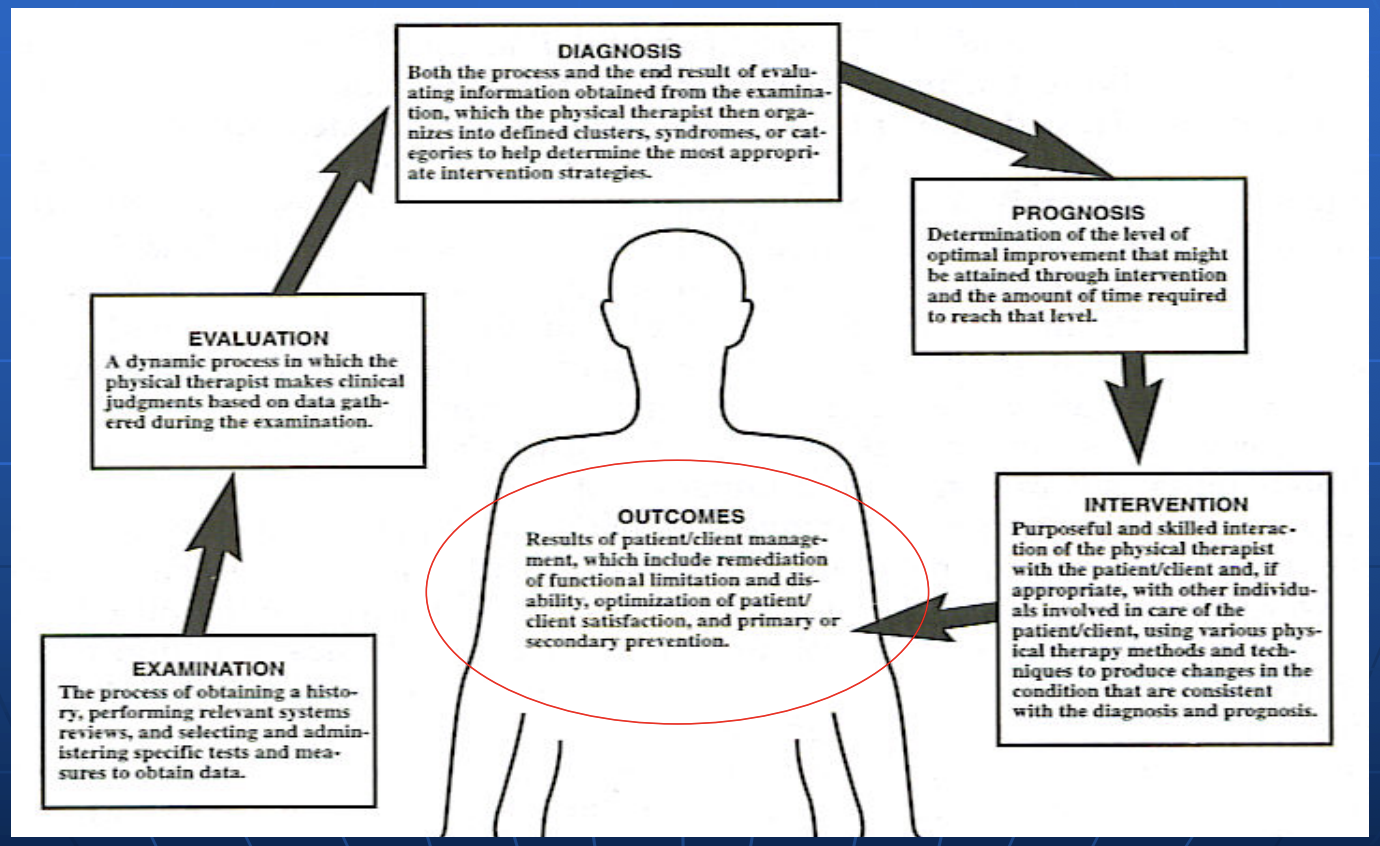
Outcomes research: guide to physical therapist practice
“PT determines expected outcomes and engages in outcomes data collection and analysis… statistical reports for internal or external use”
Traditional research
impairments: ROM, strength
physiological parameters: HR, radiographs, etc
function/performance: gait speed, functional performance, return to work
outcomes research
covers what the patient thinks of the results of the care given
meant to enhance evaluation, not replace the usual methods
barriers to outcomes research
attitudes, paradigms, lack of understanding
time pressures
unseen value by some *time vs productivity”
“End Result” Idea
the common-sense notion that every hospital should follow every patient it treats, long enough to determine whether or not the treatment has been successful, and then to inquire ‘if not, why not'?’ with a view to preventing similar failures in the future
Ernest Armory Codman, M.D.
“End result Idea”
founder of joint commission on accreditation of healthcare organizations
Codman’s Pendulums
Codman’s Paradox
Codman’s triangle
MIPS
Medicare program that awards providers for tracking outcomes
initial
discharge pairings
Why use an outcome measure
impairments measures alone are inadequate
enhances patient care → assists in goal setting
substantiates improvement in QOL from our interventions
may improve shared/clinical decision making
communication
patients
physicians/surgeons/referral sources
research/standardization for intra-group comparisons
scrutiny by 3rd party payers/recognition of external benchmarks
ensuing “pay for performance” models
standardized outcome measures are one indicator
What makes a quality outcomes instrument
components:
content
psychometric (clinimetric) properties
reliability, validity, responsiveness
clinical utility
Content
Type:
generic, condition-specific, patient specific
clinician based (CBO)
patient reported (PRO)
Scale:
what measures or questions make up the instrument
how are they scored
Interpretation
do higher scores indicate a better outcome
do certain scores pertain to excellent or poor outcomes
clinician based outcomes (CBO)
measured by clinician
joint ROM, strength, alignment, stability
considered “objective” inferring functional ability
patient reported outcomes (PRO)
patient perceptions of sx’s, abilities, and quality of life
considered more “subjective”
emphasis now greater on patient perceptions
psychometric properties: validity
extent to which the instrument measures what it is supposed to measure
psychometric properties: reliability
ability of the instrument to measure something the same way twice (or repeatedly)
psychometric properties: responsiveness
ability of the instrument to change as the status of the patient changes (referred to as “sensitivity to valid change”)
Validity
Construct (refers to items like pain or disability)
Divergent
Convergent
Content (refers to comprehensiveness of scale)
Face
Criterion (correlates with some “gold standard”)
predictive
concurrent
divergent
two similar tools do not correlate highly if they measure different attributes (i.e. social/emotion vs physical)
convergent
high correlation between two different tools measuring similar attributes
face
inferred from content experts
Reliability: internal consistency
how consistent are the questions in measuring the same outcome
Reliability: test-retest
how close are the results of an instrument given to the same patient on two different occasions
Reliability: inter-observer
how closely does observer 1 agree with observer 2 using the same instrument on the same patient
responsiveness
another psychometric property
what is the functional status of a patient at a given point in time (baseline)?
has a patient’s functional status truly changed
AND, is this change important
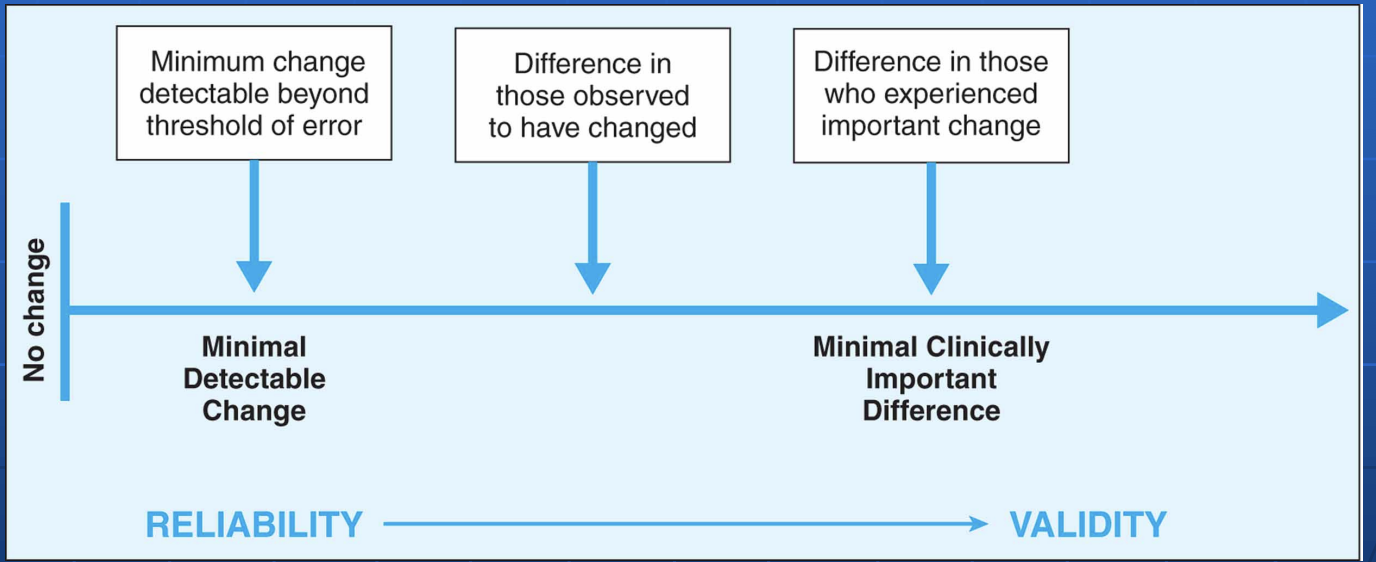
MDC or MCID
MDC: minimal detactable change
error estimate of change of an instrument
MCID, minimal clinically important difference
minimal change in score, indicative of change in function, that is truly important to a patient
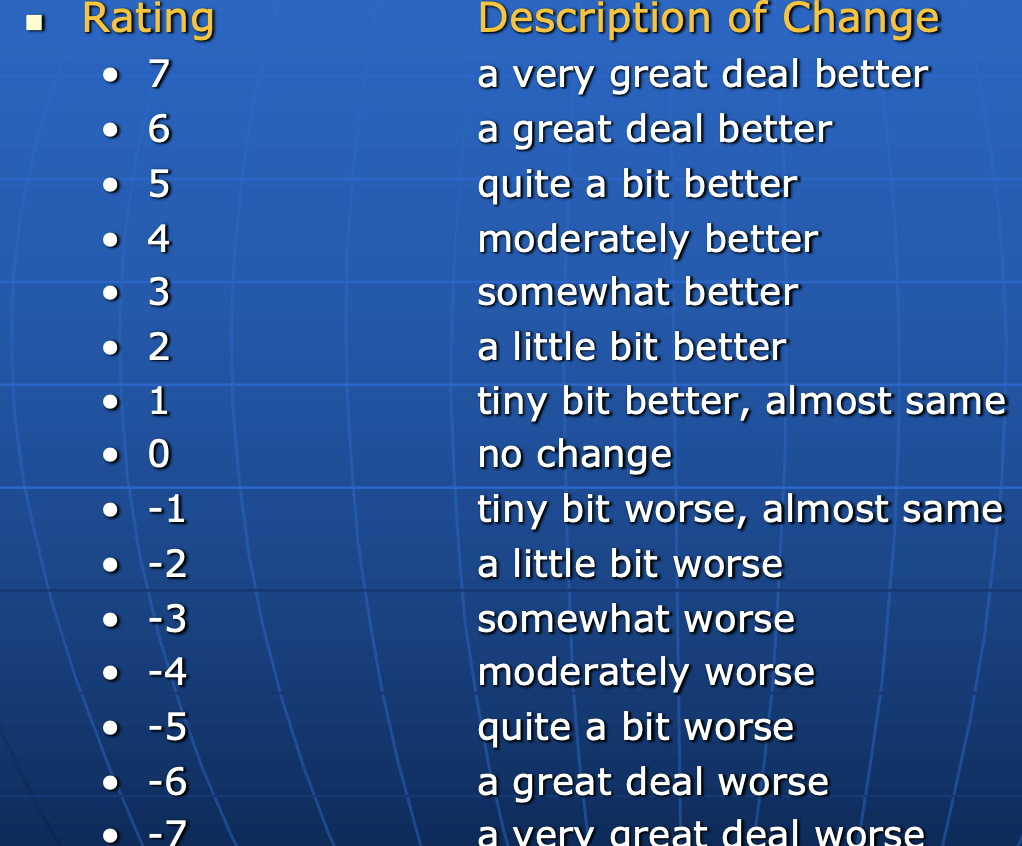
MCID
first described in 1989 (Jaeschke et al)
“the smallest difference.. which patients perceive as beneficial and which would mandate,,,, a change in patient management”
Vary widely, no standard as how to calculate MCID
9 different calculation methods
Global Rating of Change (GRoC)
MDC and MCID
Floor and Ceiling effects
useful measures must provide room for clients to demonstrate improvement or deterioration
ceiling effect
“top out” on scale, achieving normal function when some disability remains
floor effect
“bottom out” on scale, unable to detect a decline in status
patient friendly clinical utility
time to administer
clear, concise, easy to understand questions
patient comfort in answering questions
clinician friendly clinical utility
staff vs. self administered
staff effort/cost in administering, recording, and analyzing
scoring time (30-60 seconds)
Individual Common Barriers
time
knowledge
resources
competence
attitude
organizational common barriers
time and cost
policy
culture
individual common facilitators
positive attitude
flexibility
practicality
external common facilitators
access to resources
support from colleagues and organization
guidance in selection, administration, scoring and interpretation
WHO internal classification of Function (ICF) model
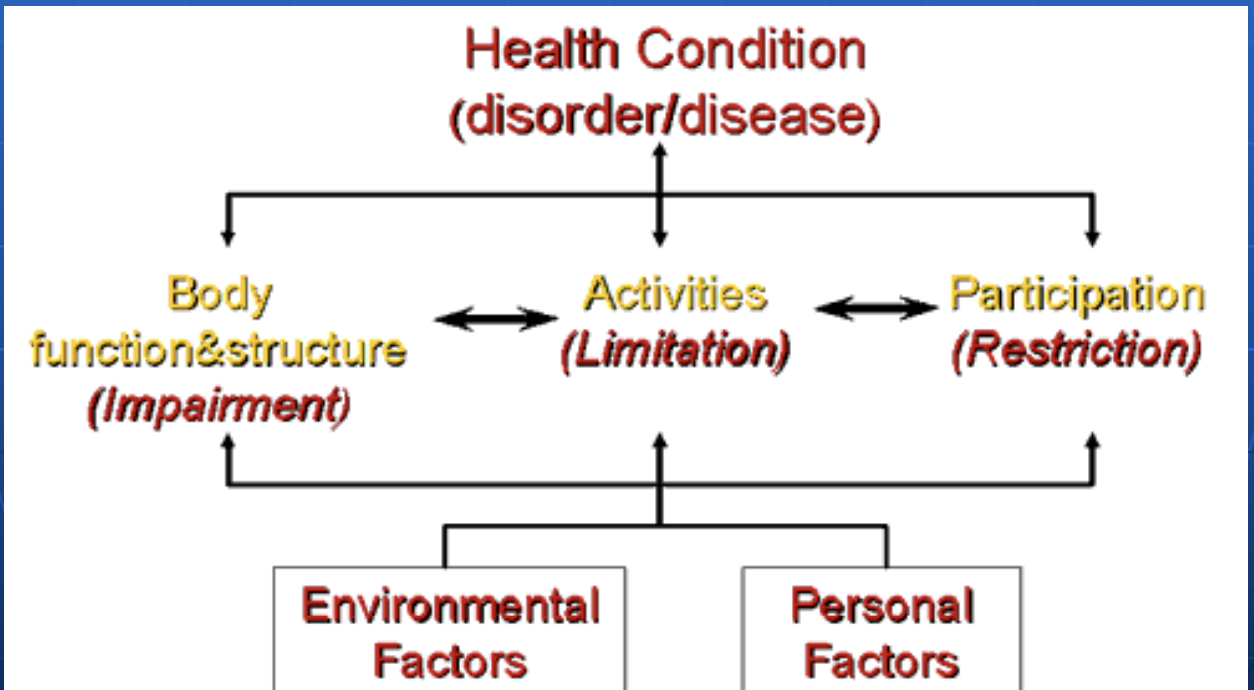
Which outcome measure to use?
the WHO ICF framework provides direction and options for choosing a variety of outcomes measures to capture multiple constructs or characteristics
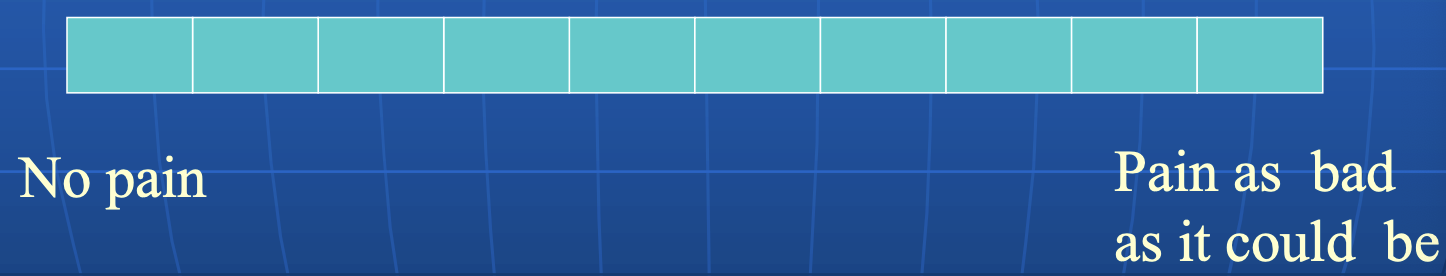
Visual Analog Scale (VAS)
100 mm vertical or horizontal line
continuous line, replaced by continuous boxes
self—administrated, easy to administer/score
reliability: test-retest (.71-.99)
Validity: correlations with McGill Pain Questionnaire, Numeric Pain Rating scale: .30-.95
Limitations: elderly and less literate populations and errors associated with photocopying/scoring
Interpretability: score >30mm equal t or greater than “moderate” pain or score > 54mm equal to or greater than “severe” pain
Responsiveness: MDC 30 mm
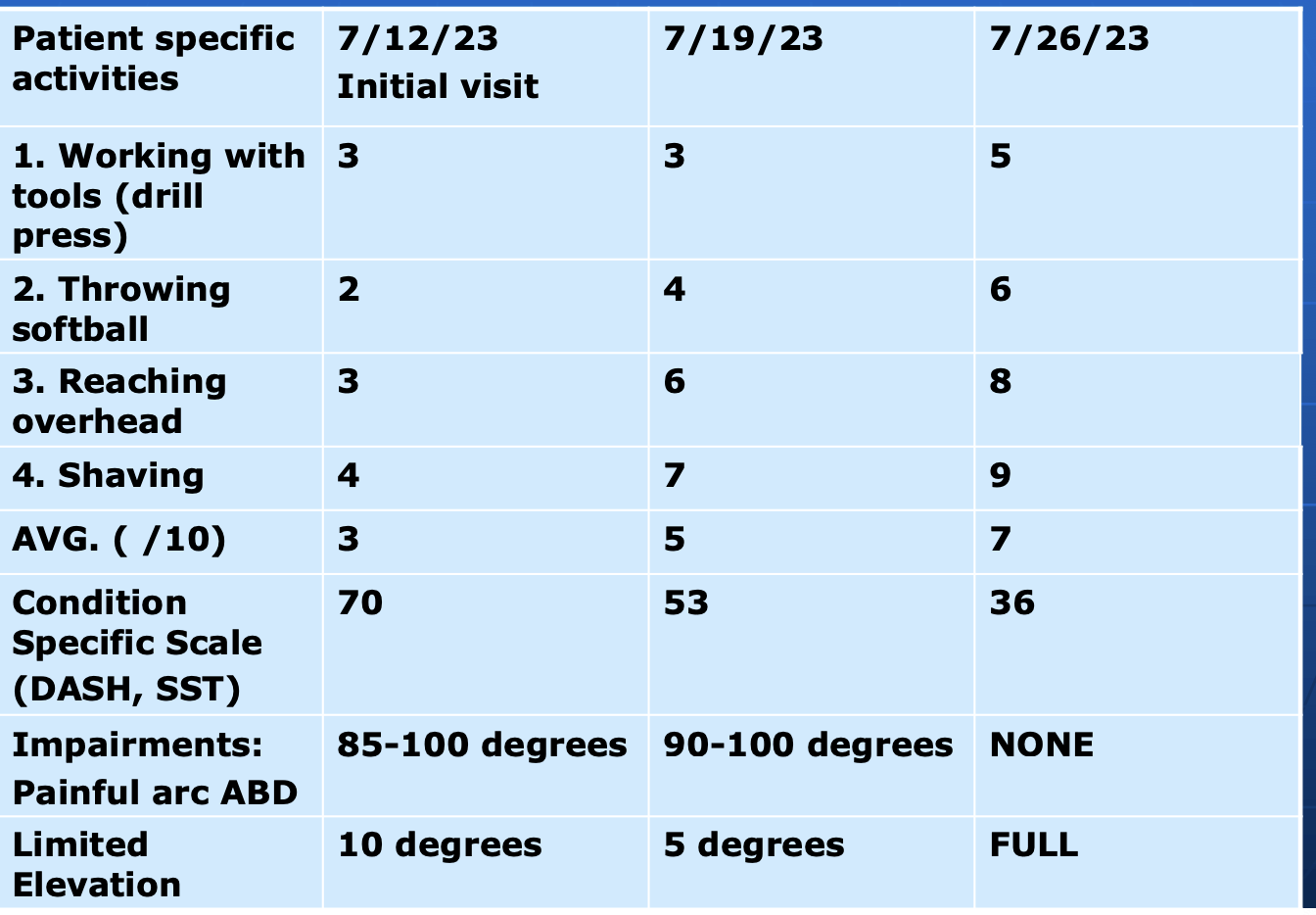
Patient Specific Functional Scale (PSFS)
type: PRO, patient specific
client asked to identify up 3 to 5 activities at initial visit before their examination
scale: rates ability to complete each one on 11 pt. scale
0 = unable to perform
10 = able to perform with no problem
time to administer: 5-15 minutes
psychometrics: MDC and MCID: 3 points
comment: not advocated for between-client comparsions
may be one of most responsive of all health-related quality of life tools