Block 5 - Genitourinary Cancers
1/181
Earn XP
Description and Tags
ONCOL 309 - Clinical Oncology I. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
182 Terms
What is the bladder?
A sac-like organ that stores urine produced by the kidneys
can hold up to 500 mL of fluid: will push up agaisnt the umbilibus when full and will lie behind the pubic symphysis when empty
What do ureters do?
drain the urine from the kidneys into the bladder
what does the urethra do
drains the urine for elimination from the body
does the bladder sit in-front or behind the pelvic bone, and where does the rectum sit
The bladder sits behind the pubic bone, while the rectum is located posterior to the bladder.
what is the lining of the urinary tract called?
the urothelium
extends from the renal pelvis to the urethra and is lined by transitional epithelium
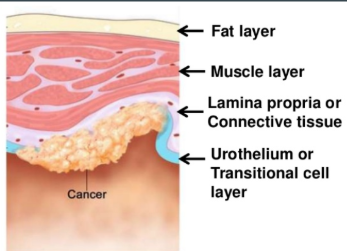
what are the 4 different layers of the bladder
transitional epithellium
in contact with urine
lamina propria
a layer of connective tissue and blood vessels
detrusor muscle
deep muscle layer made of thick smooth musle to form the wall of the bladder
perivascular fat
outer most layer: fat, fibrous tissue, and blood vessels
is bladder cancer more common in males or females?
males: 3x more likely
females will get the more aggressive form of the disease though
how does bladder cancer risk increase with age; and what percent of patients are older than 60
risk increases with age
80% of case are over the age of 60
What type of bladder cancer is most common in developed countries, what about developing countries?
transitional cell carcinoma (TCC) = developed countries
squamous cell carcinoma (SCC) = developing countries
what is the number one risk factor for bladder cancer
smoking tobacco
smokers are 2-3 times more likely to develop bladder cancer compared to non-smokers
smokers account for what percent of bladder cancers
approximately 50% of cases
etiological risk factors of bladder cancer
arsenic
aromatic amines from occupational exposure (diesel engines, paintin, rubber)
race (white is twice more likely to get disease, black is twice more likely to die)
prior exposure to abdo/pelvic RT
cyclophosphamide chemo
bladder birth defects
irritation and infection
lynch syndrome
what is lynch syndrome
a hereditary condition that increases the risk of various cancers, including colorectal and endometrial cancer. It is caused by mutations in DNA mismatch repair genes.
what are the three natural histories of bladder cancer
non-muscle invasive
muscle invasive
metastatic disease
Non-muscle invasive bladder cancer
70-80% of tumors are superfical and non life threatening
these tumors tend to recur often and is a chronic condition
can progress to muscle invasion
Muscle Invasive bladder cancer
20-30% of tumors that have grown in to deep muscle layers
poor prognosis and higher rate of metastatic disease at diagnosis
Metastatic bladder cancer
most patietns who have had prior treatment for localized disease
median survival is 12-18 months, depending on the disease extent and patient’s health status
Local presentation of bladder cancer
painless hematuria (80-90% of cases)
increased bladder irritability: frequency, incontinence, dysuria, urgency
locally advanced presentaiton of bladder cancer
pelvic pain, lymphedema, and renal poor function
metastatic bladder cancer presentation
bone pain
palpable abdomen or pelvic mass
flank pain from ureter obstruction
edema of lower extremeities
respiratory symptoms: coughing, dyspnea, hemoptysis
What screening is done for bladder cancer
no current screening exits
no evidence that early treatment of bladder cancer leads to better health outcomes and less mortality
describe the lymphatic trail from the bladder to the thoracic duct
internal iliac —> external iliac —> common iliac —> para-aortic —> cisterna chyli —> thoracic duct
what is the lymphatic spread risk for superficial tumours, detrusor muscle tumors, and deep tumors
superficial tumors: <5%
detrusor muscle: 20%
deep tumors: 20-40%
what three sites does bladder cancer generally spread to
bone
liver
lungs
poor prognostic factors of bladder cancer
depth of tumor invasion into bladder wall
the deeper the dx, the less favourable
grade
high grade tumors tend to grow into muscle walls and metastasize
carcinoma in-situ
associated with poor prognosis and a higher chance of recurrence
type of tumor
SCC is worse than TCC, papillary urothelial have best prognosis
multiple tumors is no good
size of tumor
recurrent tumors
LN invasion
what are the three types of bladder cancers
urothelial (transitional cell) (90%)
squamous cell tumors (3-8%)
adenocarcinomas
Transitional Cell tumors
tumors in the lining of the bladder wall, these cells can change shape and stretch without breaking apart
tend to spread in head to toe direction: renal pelvis to ureter
Squamous Cell Tumors
more common in developing countries, worse prognosis
due to chronic infections, bladder stones, schistosomiasis
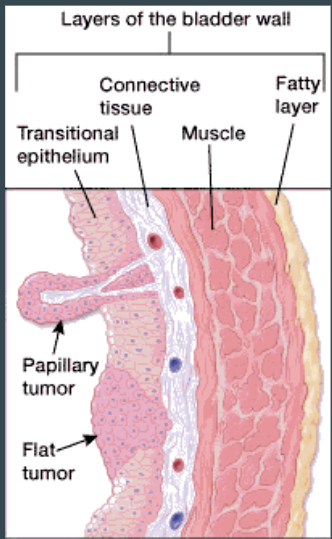
what are the two subtypes of Transitional Cell tumors
Papilary (Ta)
finger like projecitons that grow from inner surface towards hollow part of bladder
do no grow deep into muscle layers
non-invasive, slow growing tumors
tend to have good outcomes
Flat (Tis)
do not grow towards the hollow area of bladder, and are only found on the surface of the bladder
high recurrence rate
What are the 7 steps to diagnosing bladder cancer
history and physical
including smoking history and occupational exposures
urinalysis - rule out UTIs
cytology - examine bladder cells under microscope
identify high grade tumors, cancer recurrences
blood work
CCC, electrolytes, CBC, CEA
cytoscopy
assess size and mobility of palpable masses: location, size, appearance extent of dx
can do bx at same time
intravenous pyelography or ultrasound-
size of tumor and extension along bladder wall
CT/MRI (assess LN and appearance)
what is the gold standard for diagnosing bladder cancer
Cystoscopy with biopsy
to obtain tissue samples for histological examination. and to assess masses
why are CT and MRI not main choices to diagnose bladder cancer
underestimates extent of the tumor with respect to more deeply invasive tumors
what is a transurethral resection of bladder (TUR)
A surgical procedure used to remove bladder tumors or abnormal tissue through the urethra, often performed to treat bladder cancer.
removes tumor for early stage dx
bx and assess muscle invasion
if there is muscle invasion at the time of TUR for bladder cancer, what imaging is then done?
CT abdo/pelvis to see LN involvement
What is an intravenous pyelogram and what is it used for
Opaque medium is injected into a vein and the excretion of the kidneys can be radiographed
Used to show renal or ureteral disease or for localization
Has been replaced as a means of localization in RT with the use of the CT scanner which is less invasive.

What is the most important stage for bladder cancer
Stage muscle invasion (T2)
muscle invasion determines what treatment is done
TNM staging for bladder cancer - T
Tx = primary tumor cannot be assess
T0 = no evidence of primary tumor
Ta = non-invasive papillary carcinoma
Tis = carcinoma in situ = flat tumor
T1 = tumor involves subepithelial connective tissue
T2a = tumor invades superficial muscle
T2b = tumr invades deep muscle
T3a = tumor invades perivesical tissue microscopically
T3b - tumor invades perivesical tissue macroscopically
T4a = tumor invades prostate, uterus, or vagina
T4b = tumor invades pelvic or abdominal wall
TNM Staging for bladder cancer - N
Nx = regional LN cannot be assessed
N0 = no regional LN mets
N1 = single regional LN (<2 cm) in true pelvis
N2 = multiple regional LN in true pelvis
N3 = mets. to common iliac nodes
TNM staging for bladder cancer - M
Mx = distant mets cannot be assessed
M0 = no distant mets
M1 = distant mets
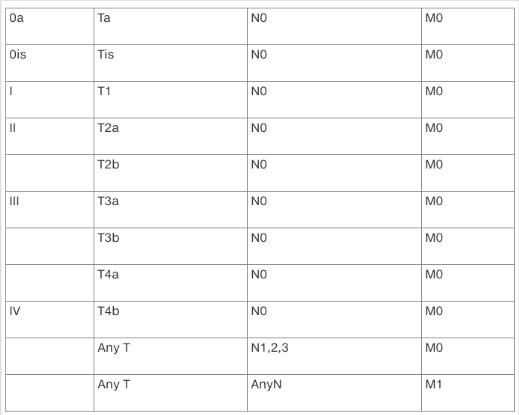
Stage groupings
Stage 0a: early cancer, surface of the inner lining of the bladder, No invasion of the muscle or connective tissue of the bladder wall. Noninvasive papillary urothelial carcinoma (Ta, N0, M0).
Stage 0is: A flat tumor or carcinoma in situ (CIS), only on the inner lining of the bladder. No growth toward the hollow part of the bladder, no spread to muscle or connective tissue of the bladder (Tis, N0, M0). High-grade cancer - aggressive disease because it can often lead to muscle-invasive disease.
Stage I: The cancer has grown through the inner lining of the bladder and into the lamina propria. It has not spread to the thick layer of muscle in the bladder wall or to lymph nodes or other organs (T1, N0, M0).
Stage II: The cancer has spread into the thick muscle wall of the bladder - muscle-invasive cancer. The tumor has not reached the fatty tissue surrounding the bladder and has not spread to the lymph nodes or other organs (T2, N0, M0).
Stage III: The cancer has spread throughout the muscle wall to the fatty layer of tissue surrounding the bladder (perivesical tissue) or to the prostate in a man or the uterus and vagina in a woman. Or, the cancer has spread to the regional lymph nodes.
Stage IIIA: The tumor has grown into the perivesical tissue or has spread to the prostate, uterus, or vagina, but has not spread to the lymph nodes or other organs (T3a, T3b, or T4a; N0; M0), or the cancer has spread to a single regional lymph node (T1 to T4a, N1, M0).
Stage IIIB: The cancer has spread to 2 or more regional lymph nodes or to the common iliac lymph nodes (T1 to T4a, N2 or N3, M0).
Stage IV: The tumor has spread into the pelvic wall or abdominal wall, or the cancer has spread to lymph nodes outside of the pelvis or to other parts of the body.
Stage IVA: The tumor has spread to the pelvic wall or the abdominal wall but not to other parts of the body (T4b, any N, M0), or the cancer has spread to lymph nodes located outside of the pelvis (any T, any N, M1a).
Stage IVB: The cancer has spread other parts of the body (any T, any N, M1b).
Bladder Cancer grading (G1,2,3)
G1 = well differentiated
G2 = moderately differentiated
G3 - poorly differentiated
What are the management categories for bladder cancer
superfical bladder cancer (T1s, Ta, T1)
muscle-invasive bladder cancer (stage T2a)
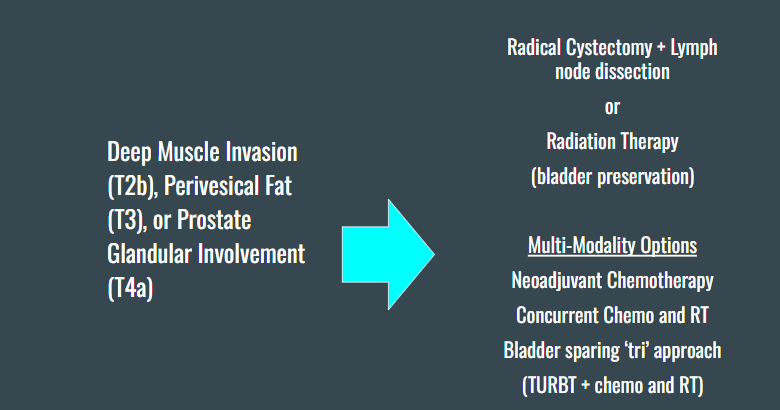
deep muscle invasion, perivesical fat, prostate involvement (T2b, T3, T4a)
locally advanced bladder cancer (T4b)
metastatic
what is a radical cystectomy
removal of the entire bladder, nearby LN, part of the urethra and nearby organs containing cancer cells
male – prostate, seminal vesicles, and proximal urethra
female – urethra, uterus, ovaries, fallopian tubes, anterior vaginal wall
can preserve sexual function/potency
5 year overall survival is 50% after a radical cystectomy
What is a segmental cystectomy
removal of part of bladder wall
high recurrence rate of 50-70% (will invade bladder musculature)
<5% of patients are candidates
if tumour is solitary and localized to the bladder dome and NOT associated with CIS + able to be removed with 3 cm margins
After a cystectomy, what are the three different ways to reconstruct the urinary tract
ileal conduit
a piece of small intestine is used to create a tube that connect your ureters and kidneys to an opening in your abdominal wall (stoma).
A exterior bag will continuously drain the urine from the stoma
neobladder reconstruction
Using a larger piece of bowel the surgeon creates a new bladder and attaches it to your ureters and urethra to drain urine. Sometimes a catheter is still required to drain the bladder.
conduit urinary reservoir
Using a piece of bowel, the surgeon creates a small reservoir inside your abdominal wall. It is drained with a catheter. No collection bag needed.
what is Bacilus Calmette-Guerin (BCG) intravesical therapy
an immunotherapy treatment to treat early stage tumors
drug is given directly into your bladder (germ that is related to TB), this will activate the immune system to attack cancer cells
leads to a 70-80% 5YS in T1 tumors
Side effects of BCG therapy
flu like symptoms, hematuria, urinary frequency, burning sensation while urinating
what class of chemo drug is considered the standard of care for bladder cancer
Platinum-based chemotherapeutics
5% survival benefit and helps patients become eligable for bladder sparing
What is the new combo regiment chemotherapy for bladder cancer
Gemcitabine + cisplatin
shows good response rate for fewer side effects
Old chemo regime for bladder cancer
MVAC
methotrexate
vinblastine
Doxorubicin/adriamycin
cisplatin
intravesical chemotherapy for bladder cancer
mitomycin C
gemcitabine (less side effects than MC and less blood absorption)
Valrubin (same side effects as BCG)
why does giving chemo right to the bladder decrease side effects?
Delivering chemotherapy directly to the bladder minimizes systemic exposure, thereby reducing side effects while targeting the tumor more effectively.
Cyclophosphamide for bladder cancer
Alkylating agent (Nitrogen mustard derivative)
Can enhance radiation damage to tissues, know as a ‘recall radiation reaction’
Acute inflammatory reaction confined to irradiation tissue
is radiation therapy used for superficial bladder tumors?
no
when is RT used for bladder cancer
typically used post-op for bladder preservation
T3b, T4 or positive surgical margins
is RT indicated for node positive disease?
no, not generally indicated as distant mets are the concern, not local recurrence
What is the treatment protocol for low grade superficial bladder cancers (Ta or T1)
Transurethral resection with bx
then re-resection within 4 weeks (since tumors are often understaged in bladder)
if the Bx are positive following TUr for low grade superficial bladder cancers, what is the next treatment steps
T1: BCG intravesical injection
Ta: mitomycin C intravesical chemo
Is RT involved in the treatment of low grade superficial bladder cancer?
no
What is the treatment protocol for high grade superfical bladder cancer?
Transurethral resection + mitomycin C chemo
4 weeks later: BCG intravesical injection
cystectomy if BCG fails
is there RT involved in the treatment for high grade superficial bladder cancer?
no, does not respond reliably to therapy
What is the treatment protocol for muscle invasive bladder cancer (Stage T2a)
cystectomy
radiation therapy ± chemotherapy (bladder sparing)
what is the treatment protocol for deep muscle, perivesical fat, or prostate involvement (T2b, T3, T4a)?
radical cystectomy + LN dissection
or RT (for bladder preservation)
we also have multimodality options for concurrent chemo and RT or tri approach
what is the treatment protocol for locally advanced bladder cancer (metastatic T4b)?
initial treatment is with chemo, but then rest of treatment is case by case
palliative RT or Pt based chemo may then be used
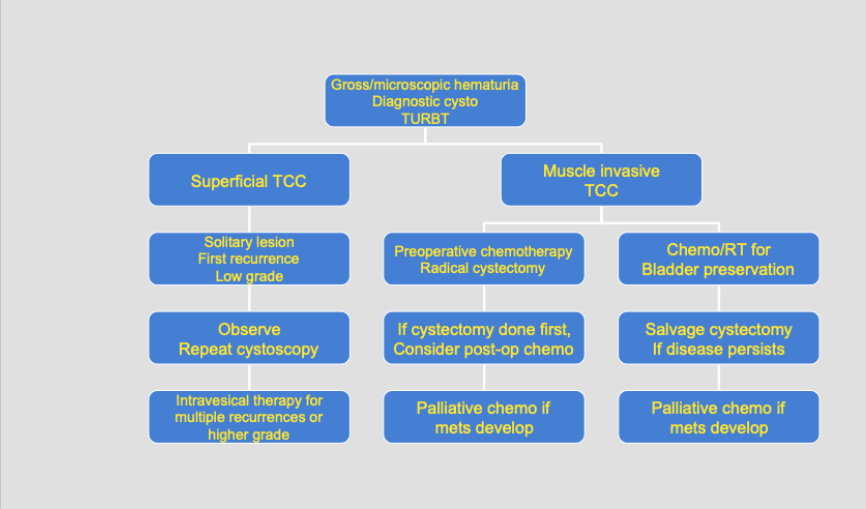
Bladder Cancer Treatment Pathway
good for studying
Bladder Cancer Radical Radiation Therapy - Phase 1: treatment energy, technique, dose / fractionation and margins,
10 MV or greater
4 Field Box
45 Gy / 25 fraction
treat entire pelvis, including external/internal iliac nodes, bladder, and margin around bladder and prostate.
we want bladder full if possible but empty is an option
why are the common iliac nodes not targeted in phase 1 bladder cancer treatment
higher risk of disease in internal/external and to limit bowel toxicity
what does bladder filling for bladder cancer treatment depend on
patient condition - if patient can hold their bladder, if they have a bladder
doctor preference
Full bladder is the ideal option for whole pelvis tx to reduce small bowel toxicity
May involve clamping/locking a patient’s catheter ahead of treatment to have a consistent bladder volume
This must be followed for successive treatment phases or re-sim patient with an empty bladder for boost fields
Empty bladder - reduces size of bladder and therefore we can have smaller treatment fields
consistent way to ensure internal anatomy is localized for treatment
why do we plan patient with bladder cancer for RT with both a full and empty bladder
allows for evaluation of best plan and can use either set-up for boost
Bladder cancer phase 1 treatment volumes - superior
L5/S1
include internal and external iliacs
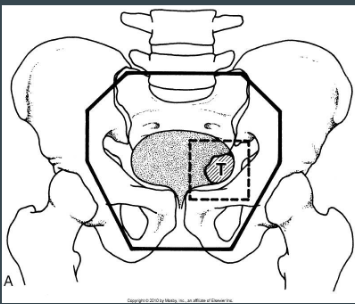
Bladder cancer phase 1 treatment volumes - inferior
bottom of obturator foraman or 2 cm below tumor
men: coverage of prostate
women: proximal 2 cm or urethra
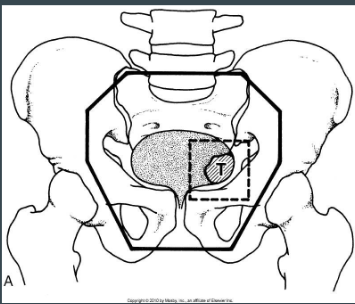
Bladder cancer phase 1 treatment volumes - laterally
1.5 - 2 cm lateral to pelvic brim
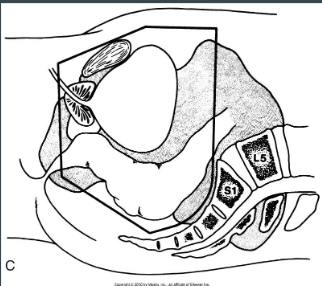
Bladder cancer phase 1 treatment volumes - anterior
extend 2 cm anterior to bladder and pubic symphysis
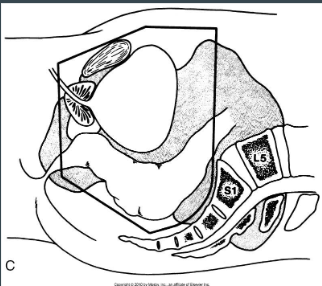
Bladder cancer phase 1 treatment volumes - posterior
extend 2 cm beyond bladder or any visable tumor/iliac nodes
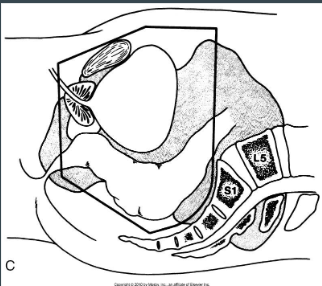
Radical Bladder Cancer RT Phase 2 - technique and dose fractionation
4 field box with/without oblique combination
20 Gy / 10 fraction (so total treatment with phase 1 = 65 Gy / 35)
8 Gy to entire bladder
12 Gy to tumor + 2 cm margin
When is palliaitve EBRT used for bladder cancer
for patients who are not eligble for cystectomy or have metastatic disease
Palliative bladder cancer treatment technique and dose fractionation
large pelvic POP
30 Gy / 10 Fractions
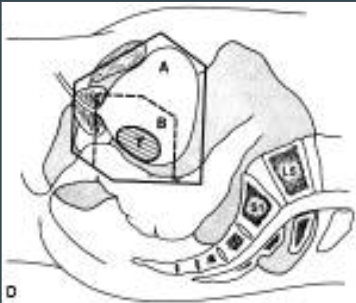
5 OARs for bladder cancer treatment
bladder
rectum
small bowel
large bowel
femoral heads
review TD5/5s and max doses
what is the acute reaciton of the bladder to 30 Gy
cystitis
acute side effects for RT to bladder
fatigue
skin erythema
radiation cystitis (freq, urgency, dysuria)
mild diarrhea and tenusmus (persistent, often painful, sensation of rectal fullness and the urgent need to pass stool, even when the bowel is empty)
hair loss in Tx area
chronic side effects for RT to bladder
cystitis
decreased bladder capacity = 30 Gy
increased frequency = 70 Gy
painless hematuria
Fibrosis
bleeding
ulcerations
surgical complications from bladder cancer
blood loss, rectal injuries, importence, urinary infection, obstruction
chemo reactions from bladder cancer
chemical cystitis
myelosuppression
why is patient follow up and cytology so important for bladder cancer
This is a very aggressive disease with a poor prognosis. If disease left untreated:
50 % die within one year
75 % die within 2.5 years
do cytology and cyscopy every 3-6 months for 2 years after tx completetion
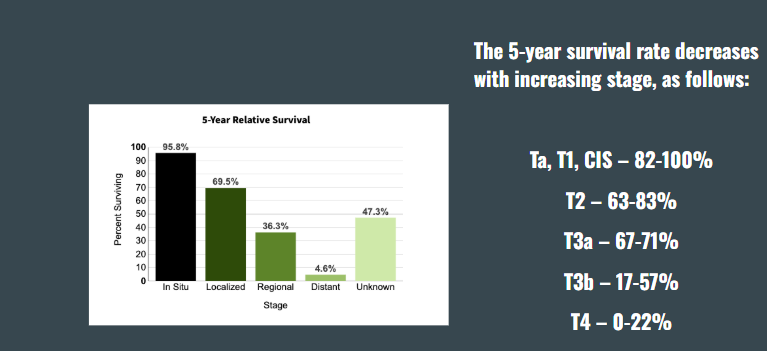
5 year survival rates for bladder cancer
emerging technology for bladder cancer treatment
hexaminovulinate blue light cytoscopy
Presence of missed tumour could link to high recurrence rate
Photosensitizer injected right into bladder before cystoscopy
Photosensitizer accumulates in rapidly dividing cells, usually malignant cells, and shows red when under blue light
Improves visualization of the bladder - more accurate staging and reducing tumour recurrences
Penile Cancer Epidemiology
rare; occurs <1% of cancer in men
occurs in men aged 60 and older
peakts at 80
south america, china, africa have higher incidence
Etiological factors of penile cancer
poor personal hygiene
HPV infection
many sexual partners
smokers
phymosis (the inability to retract the skin (foreskin or prepuce) covering the head (glans) of the penis)
Prognostic indicators of penile cancer
location and size of tumor
stage (status of nodes)
tumor differentiation
incidence of nodal involvement
why is nodal invovement relvant to prognostic factors of penile cancer
tumor free regional nodes = excellent long term survival
inguinal node involvement = 40-50% 5YS
pelvic node involement = <20% 5YS
what are the two carcinoma in-site premalignant lesions of penile cancer
bowen’s disease (SCC in situ)
erythroplasia of queyrat (Bowen’s of penis)
what is the name of the precancerous dermatolgic lesion of penile cancer
leukoplakia
what is the histology of penile cancers
mostly well-differentiated SCC
melanoma, sarcoma, and metastatic dx are possible but rare
where do most penile carcinomas start?
in the preputial area; arising in the glands, coronal sulcus or the prepuce
what is the most common LN penile cancer will go to
the inguinal lymph nodes
what is the most common metastatic site for penile cancer
lungs
what is the clinical presentaiton of penile cancer
redness, sores on penis
bloody discharge
warty growths/ulcers (like SCC of skin)
dysuria
hematuria
diagnosis and detection of penile cancers
Urinalysis
CBC
CXR
Clinical exam
primary lesion
inguinal node (30% are palpable at presentation)
Biopsy under local anesthetic
CT – to determine LN involvement
MRI & US of penis
what are the four pathological types of penile cancer
SCC (most common)
Verroucous cancer (a slow-growing, rare, low-grade variant of squamous cell carcinoma)
Warty and basaloid carcinoma (HPV associated)
neuroendocrine (rare)
TNM staging of Penile Cancer - T
T1 - Tumor invades subepithelial connective tissue
T2 - Tumor invades corpus spongiosum or cavernosum
T3 - Tumor invades urethra
T4 - Tumor invades other adjacent structures