Cardio/Renal 29 - Solute and Water Handling II (Dr. Olgun)
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
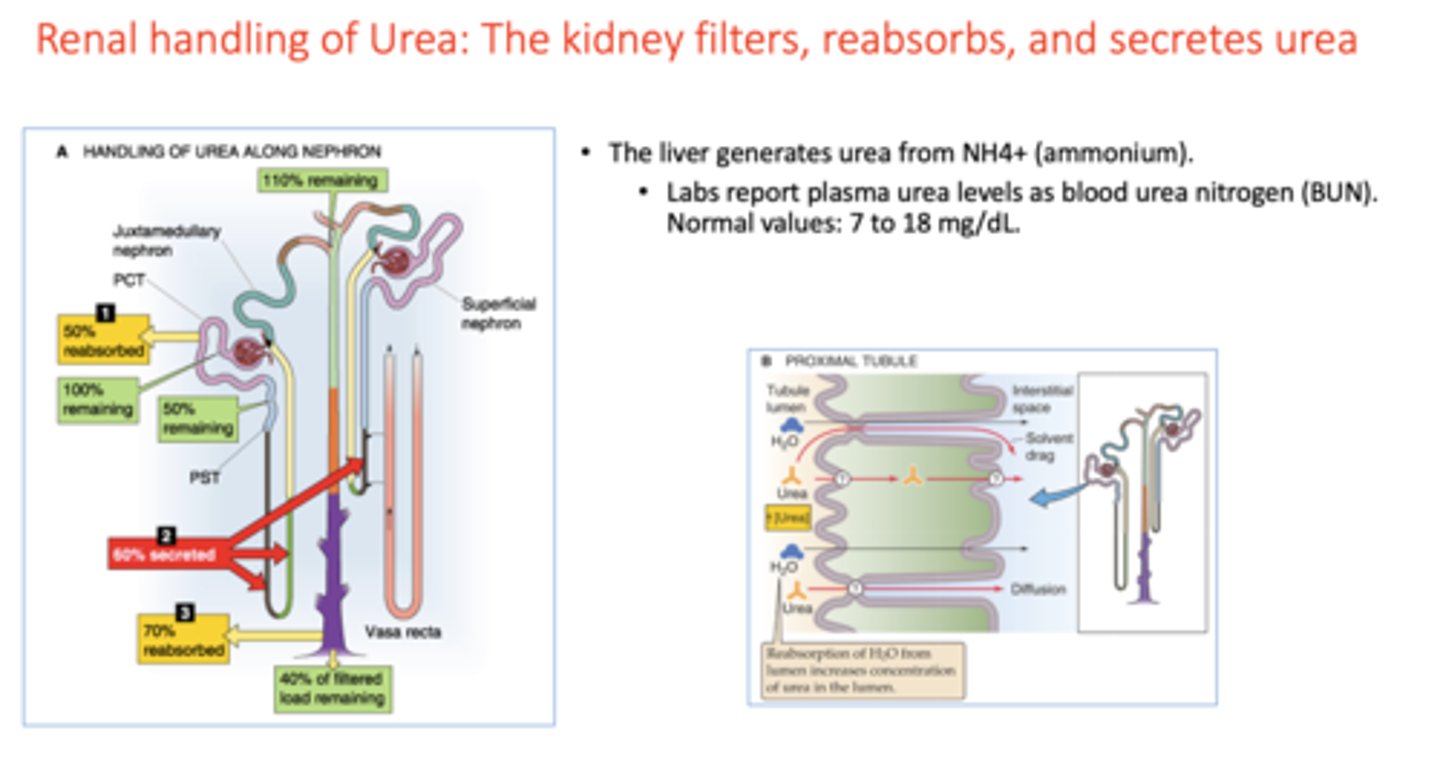
Of the 3 kidneys functions, urea normally experiences:
filtration
reabsorption
secretion
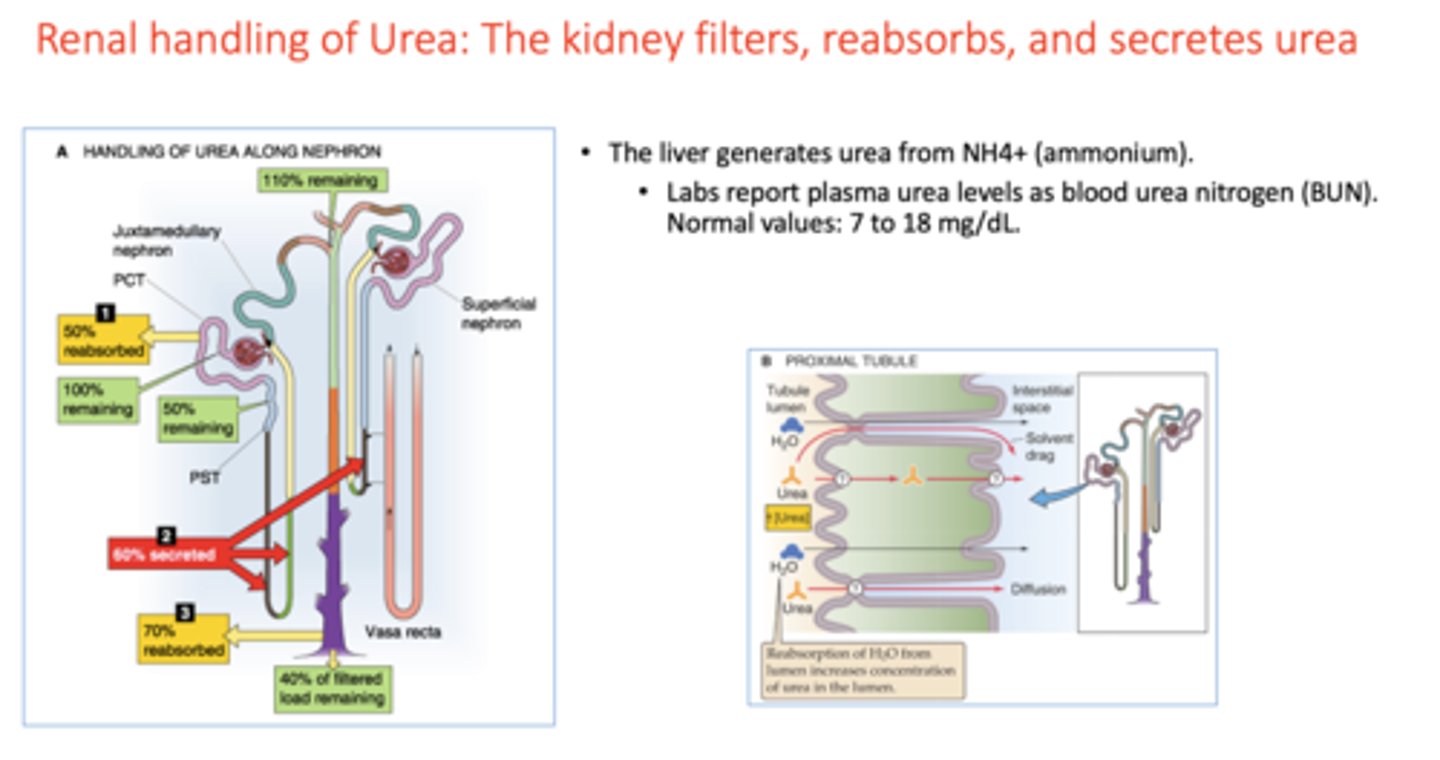
liver generates urea from
NH4+ (ammonium)
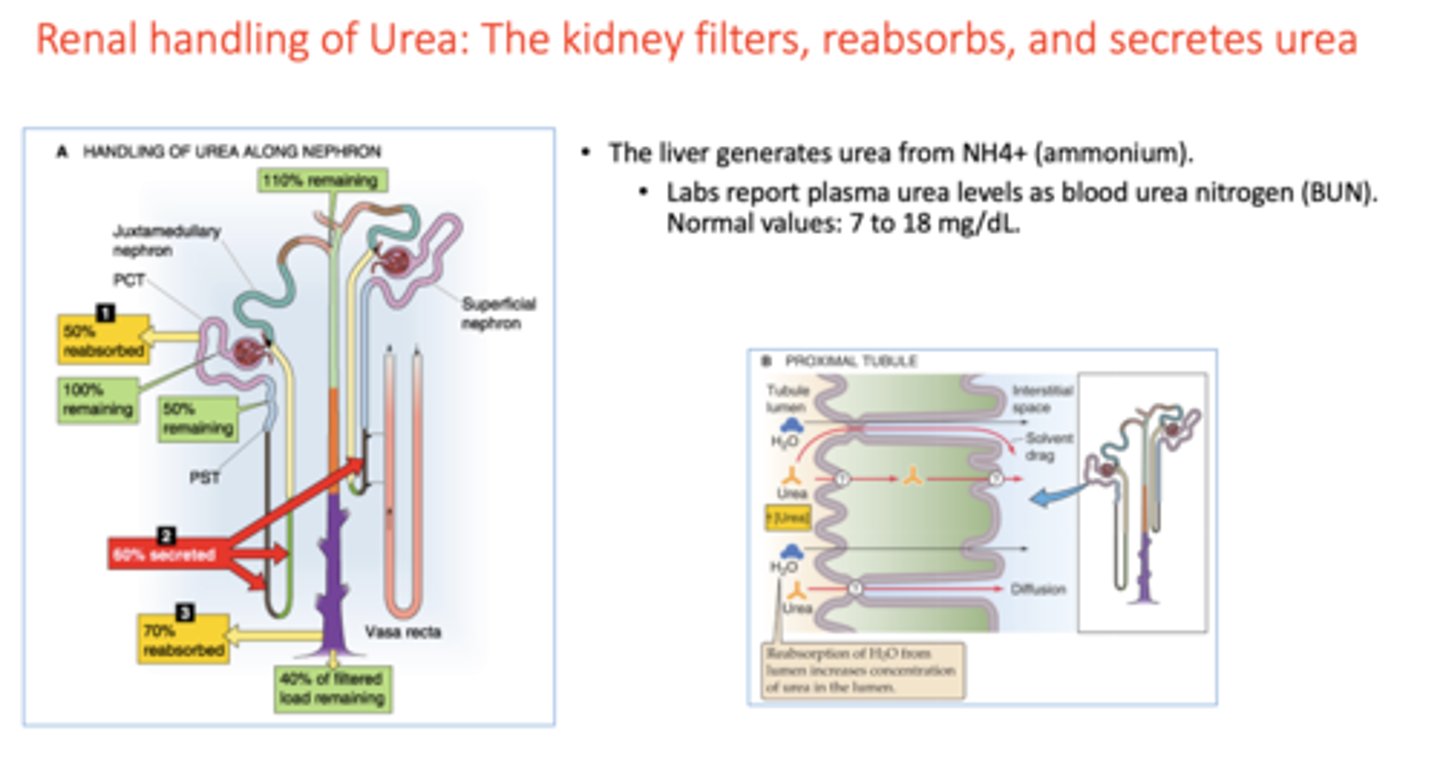
What is the normal blood urea nitrogen levels?
7-18 mg/dL
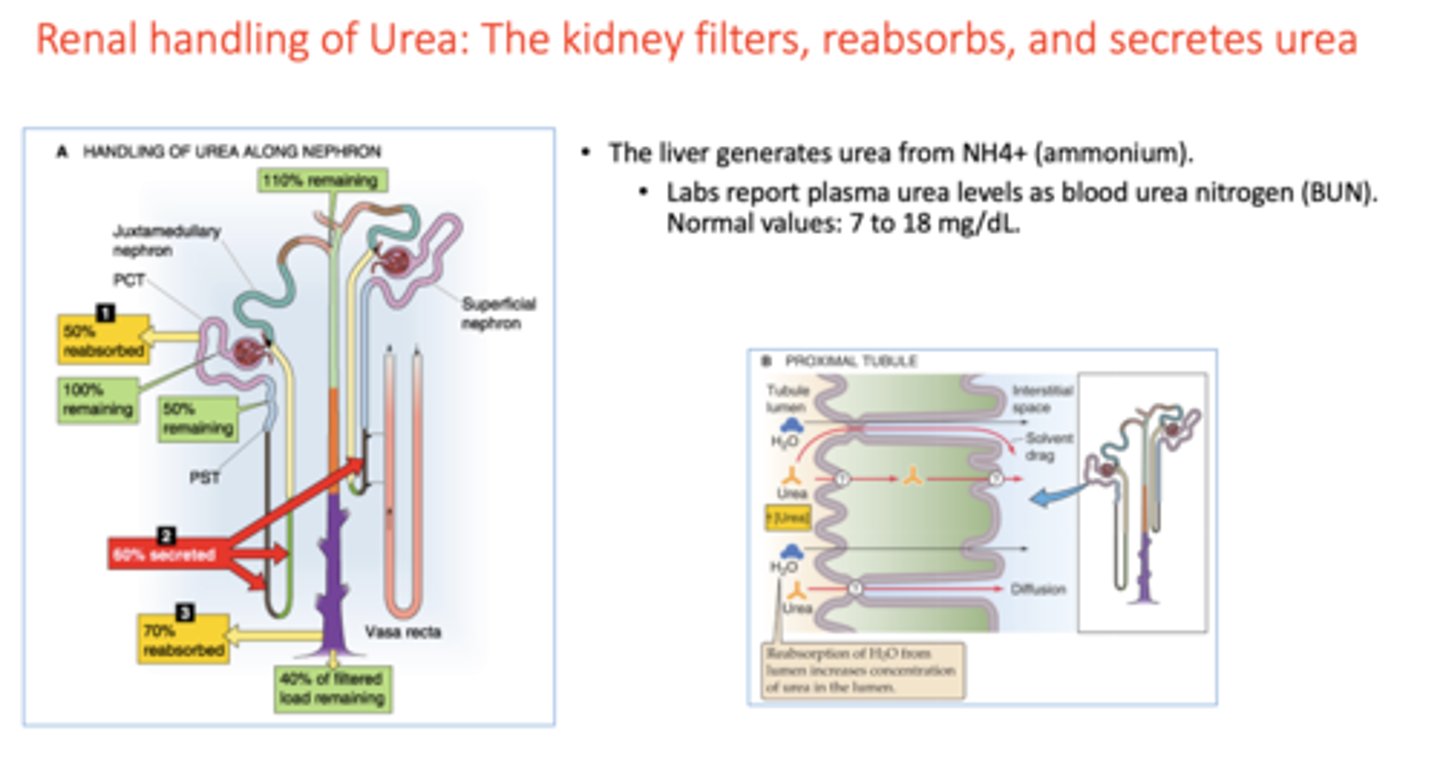
in the proximal tubule, urea is reabsorbed via ______
solvent drag/diffusion
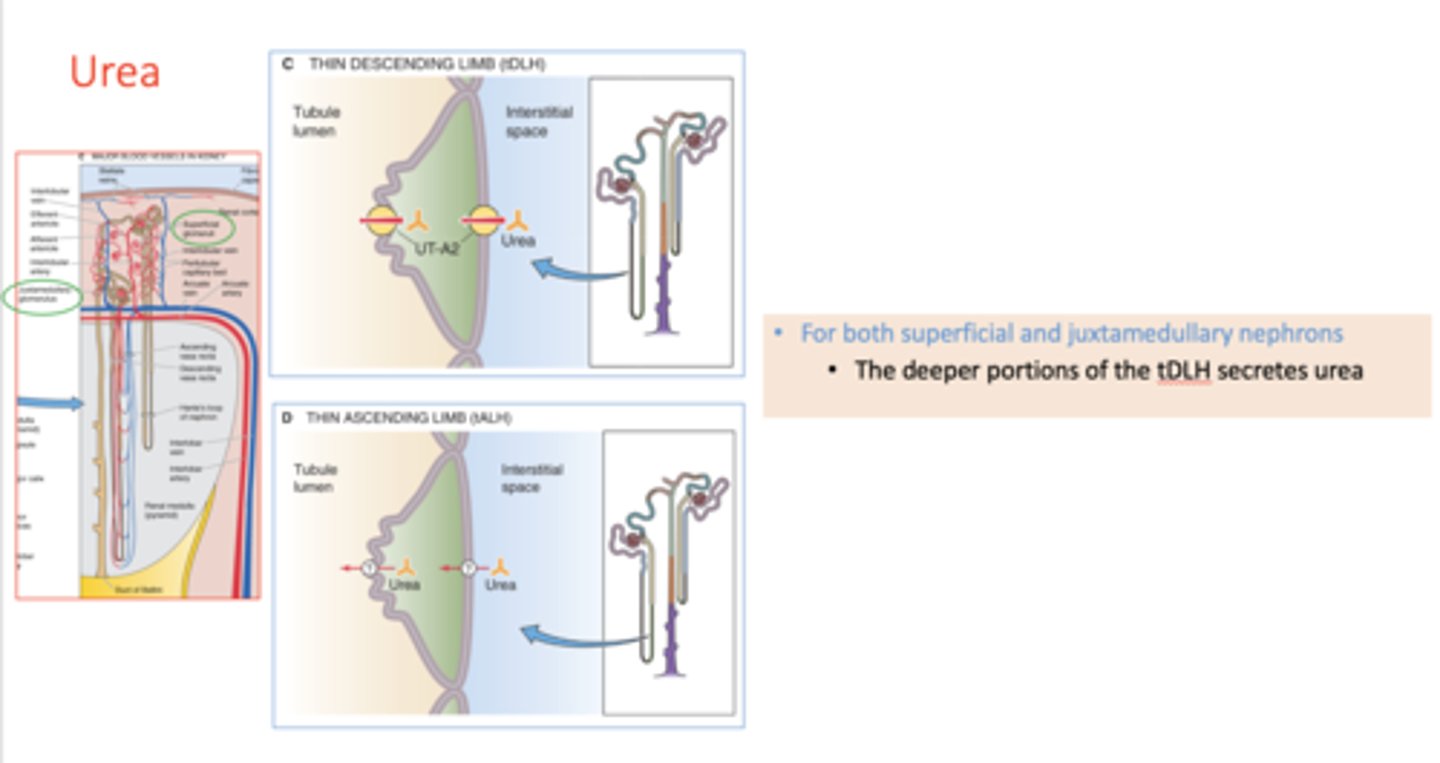
For both superficial and juxtamedullary nephrons, the deeper portions of the thin descending loop of henle secretes ________
urea
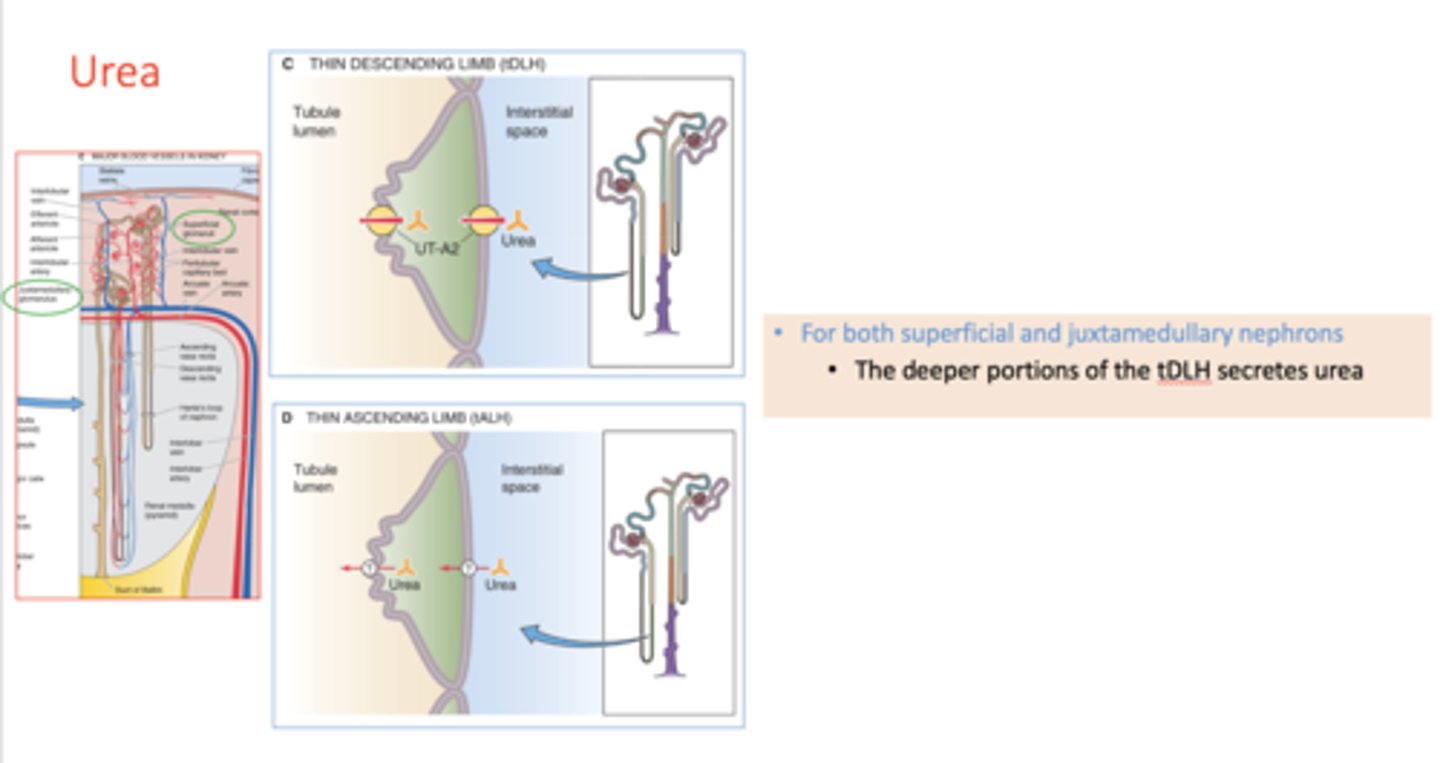
what part of the nephron secretes the most urea?
thin descending loop of Henle
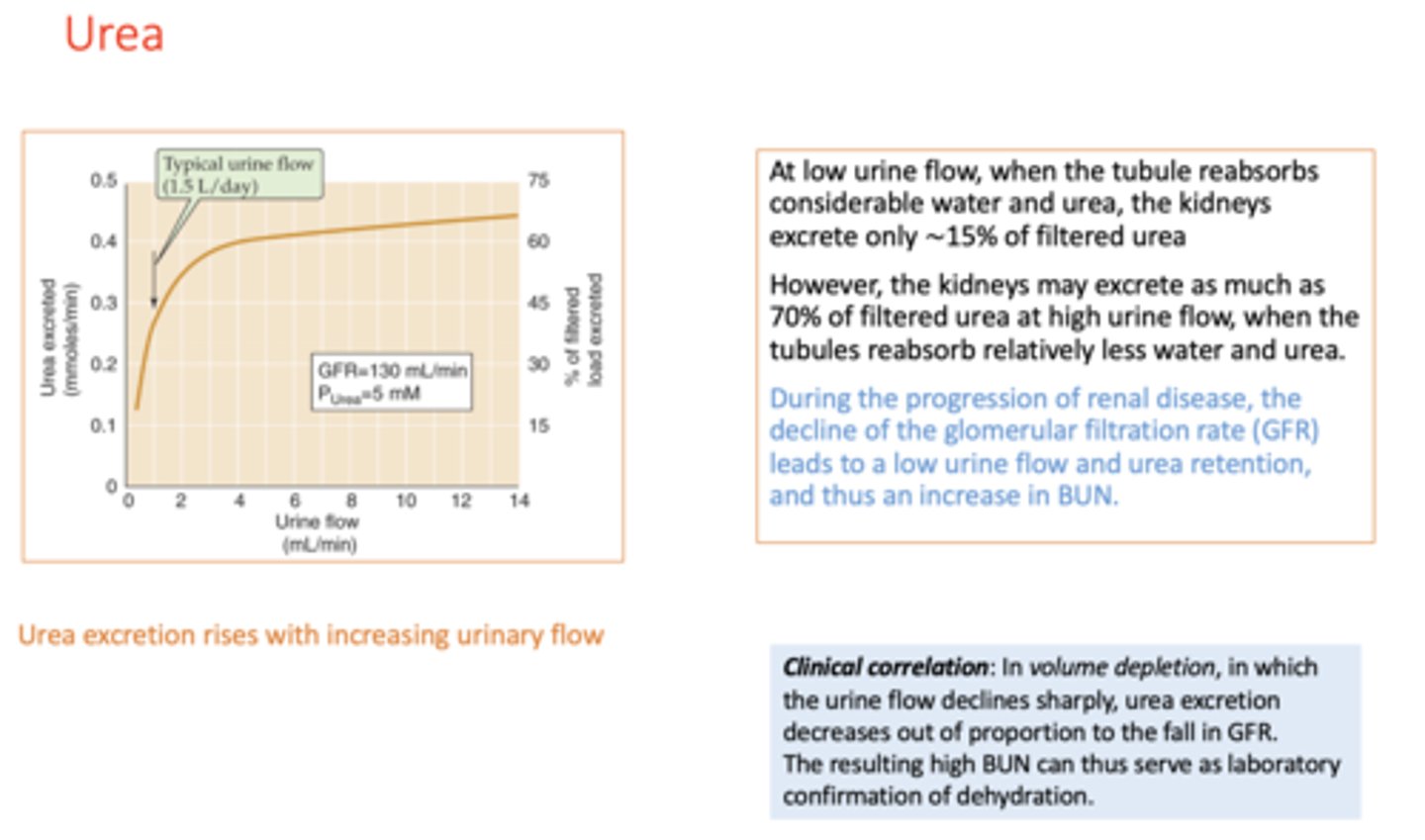
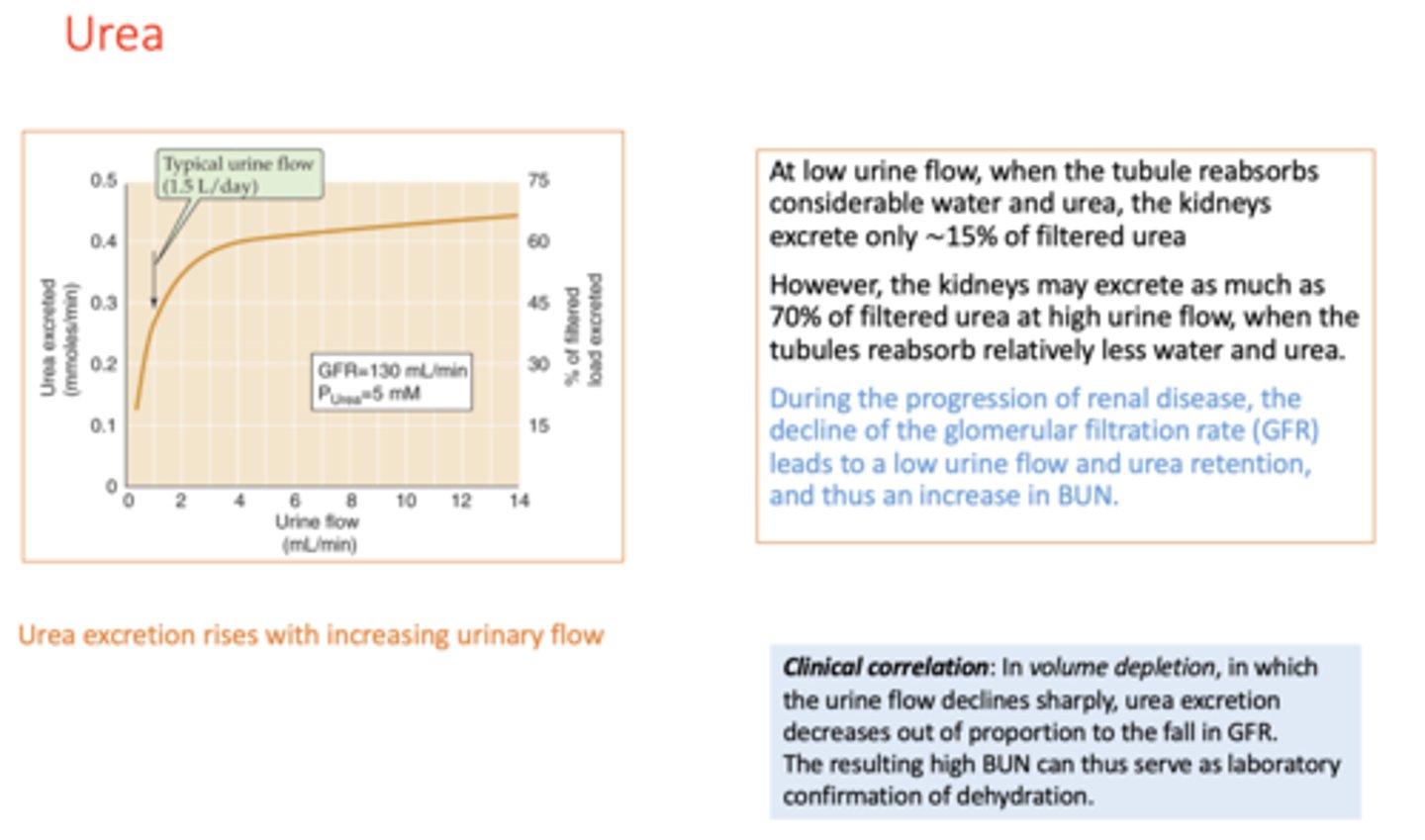
Urea excretion will _______ with increasing urinary flow
increase
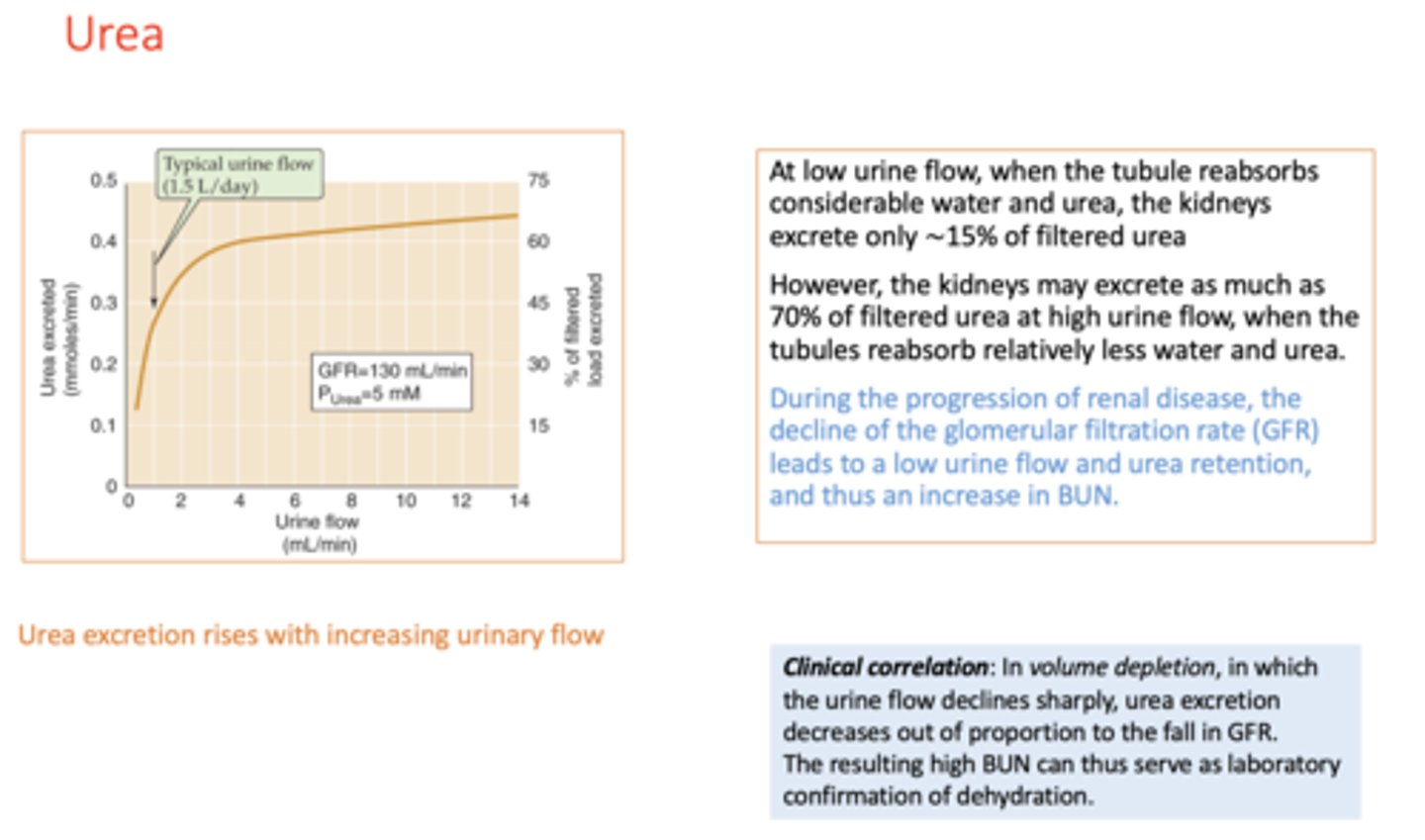
During the progression of renal disease, the decline of the glomerular filtration rate (GFR) leads to a low urine flow and urea retention, and thus an _______ in Blood Urea Nitrogen (BUN).
increase
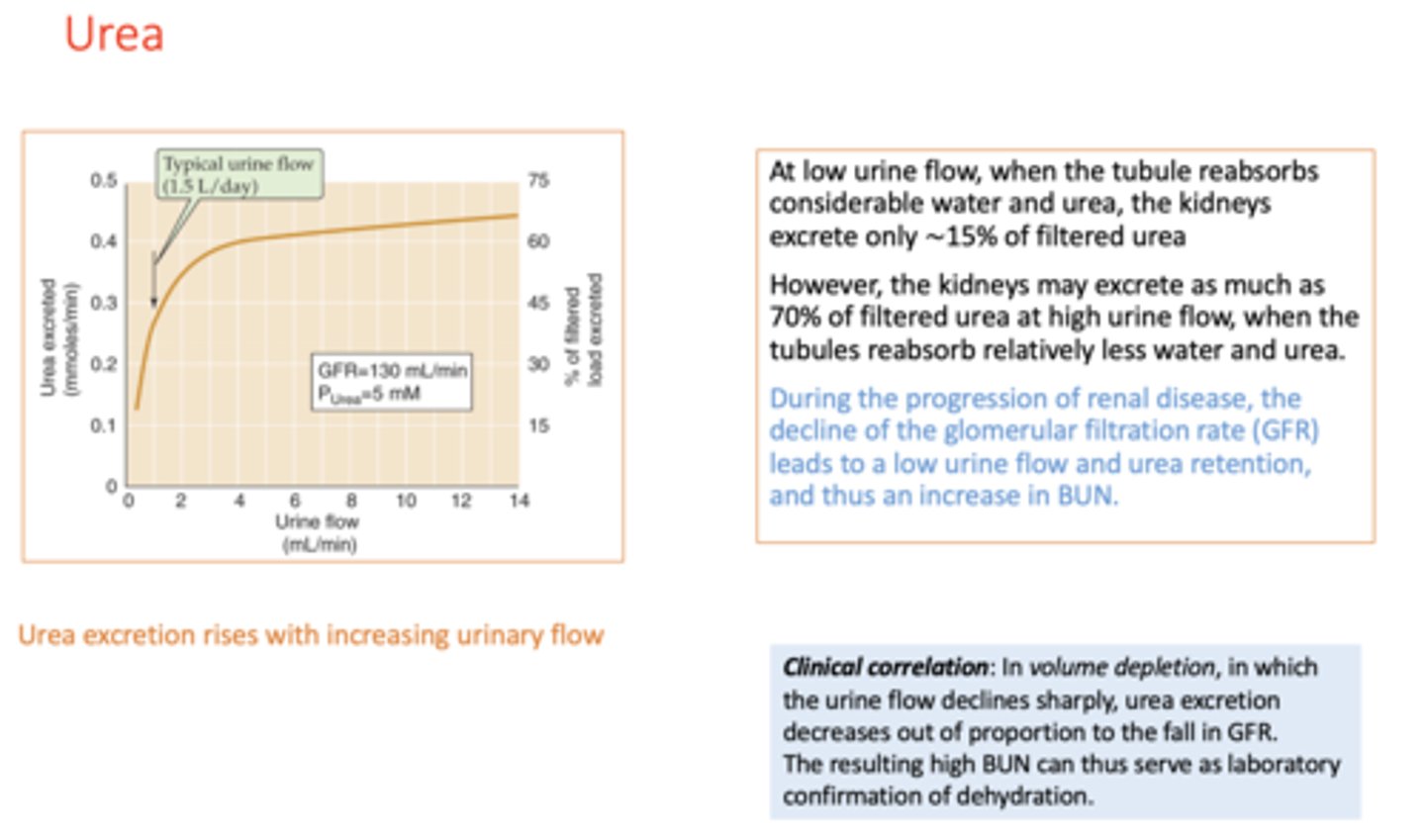
Clinically, in volume depletion, in which the urine flow declines sharply, urea excretion decreases out of proportion to the fall in GFR. The resulting high BUN can thus serve as laboratory confirmation of ___________
dehydration
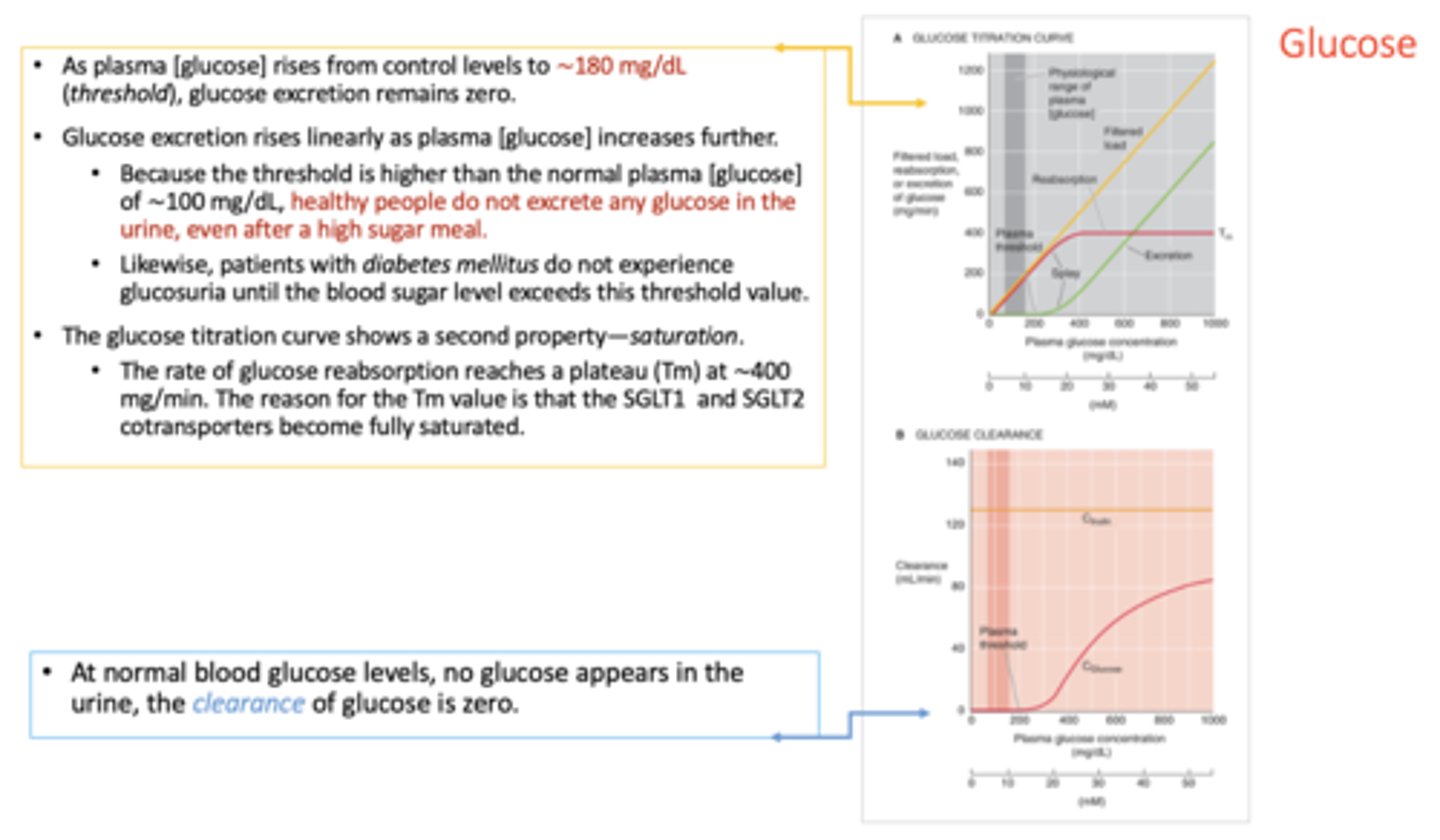
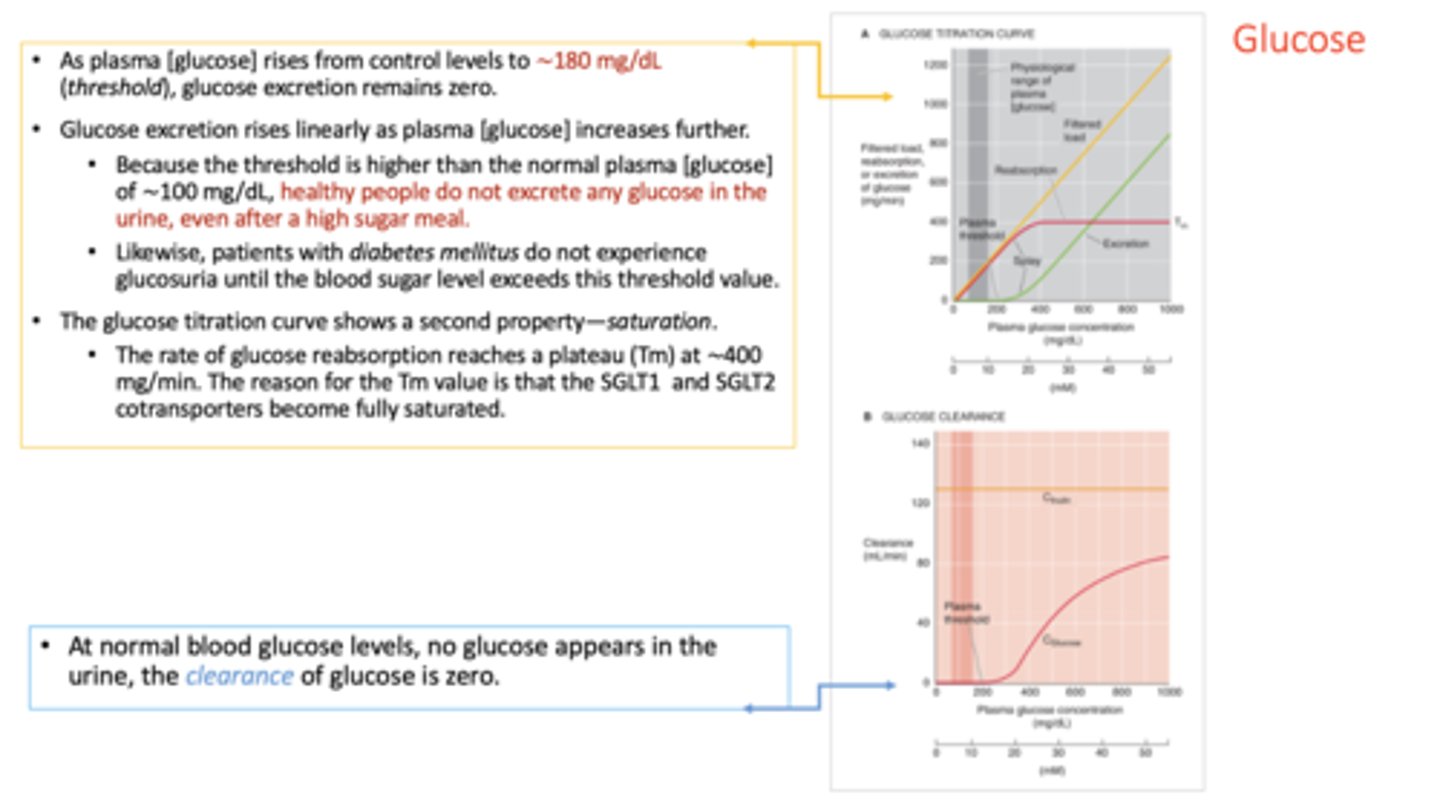
t/f: glucose is normally found in the urine
false
of the 3 kidneys functions, glucose normally experiences:
filtration
reabsorption
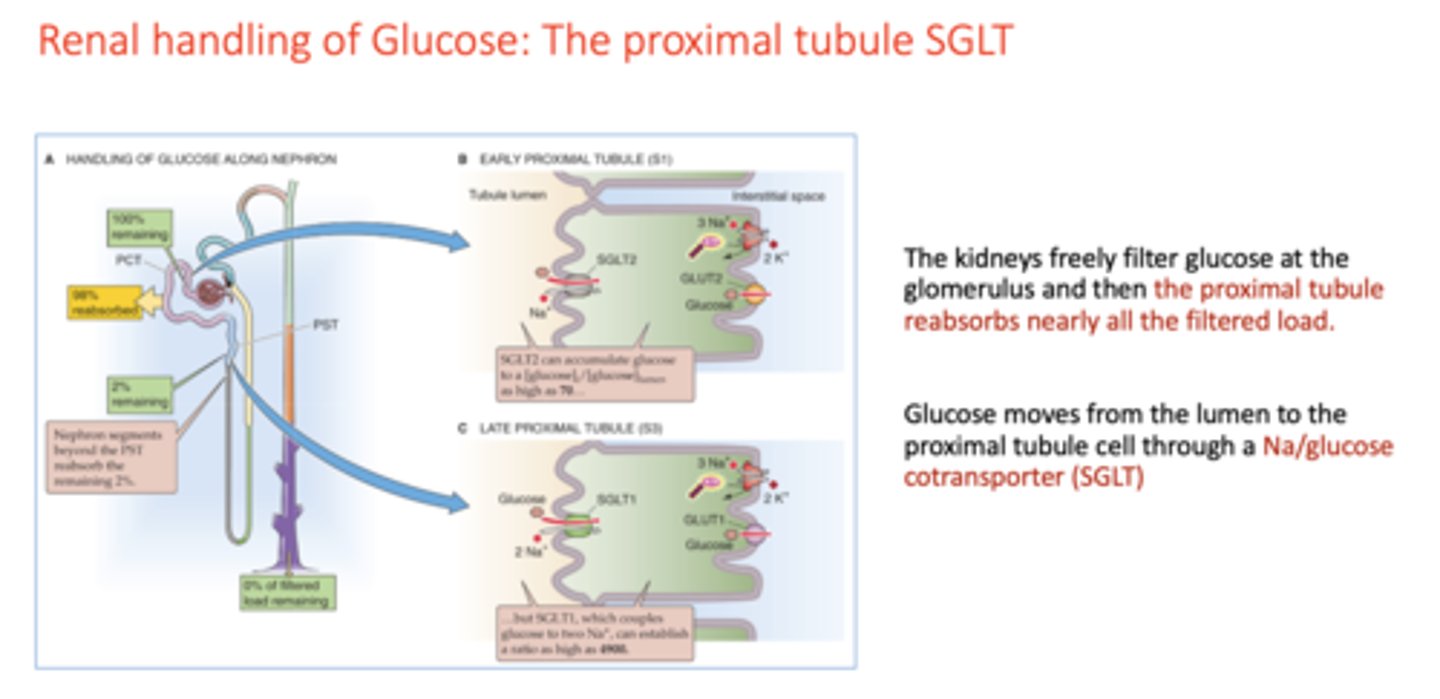
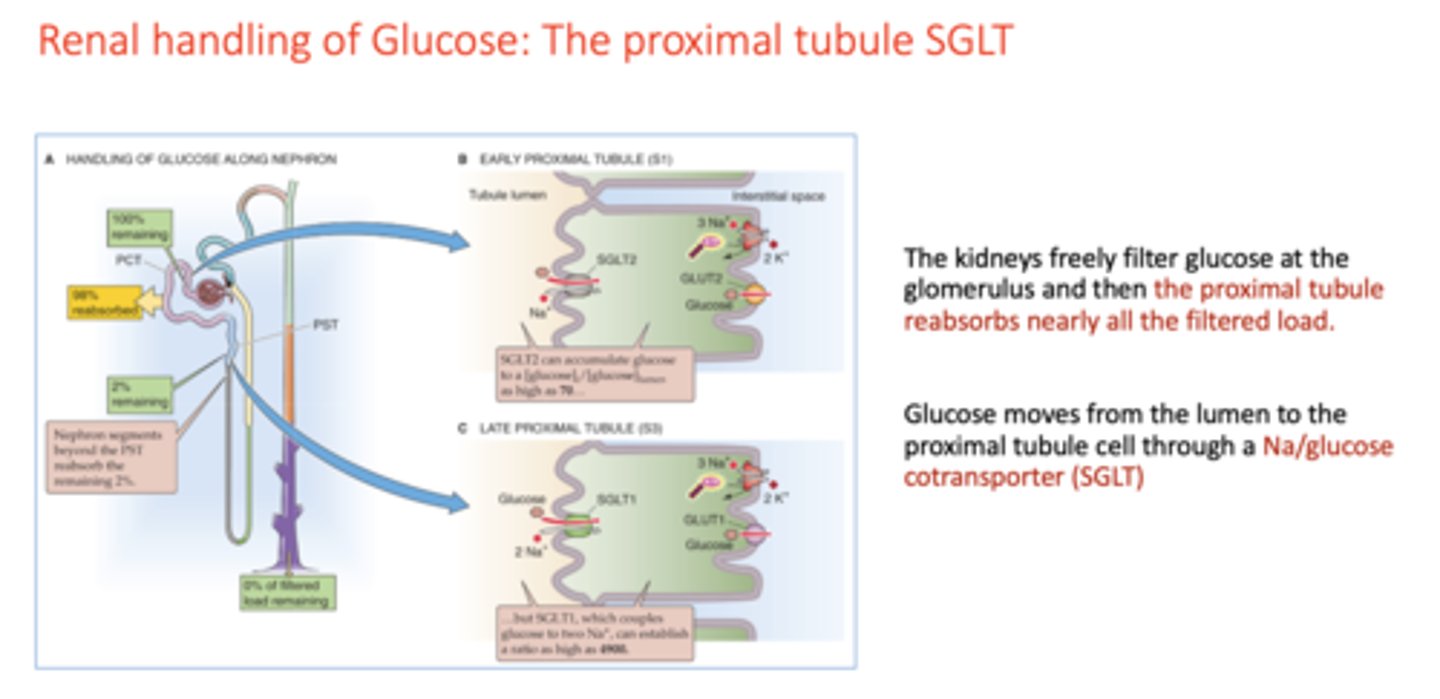
the kidneys freely filter glucose at the glomerulus and then the __________ reabsorbs nearly all the filtered load
proximal tubule
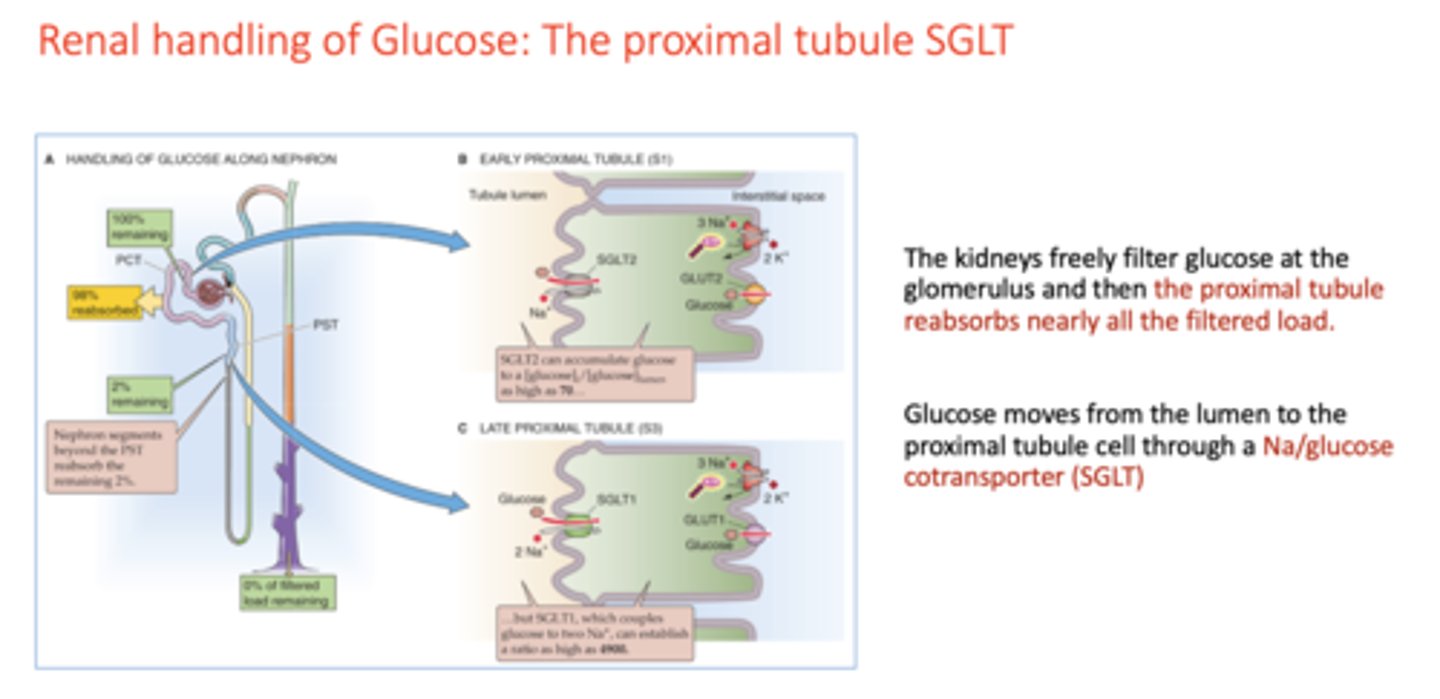
Glucose moves from the lumen to the proximal tubule cell through a _________
Na/glucose cotransporter (SGLT)
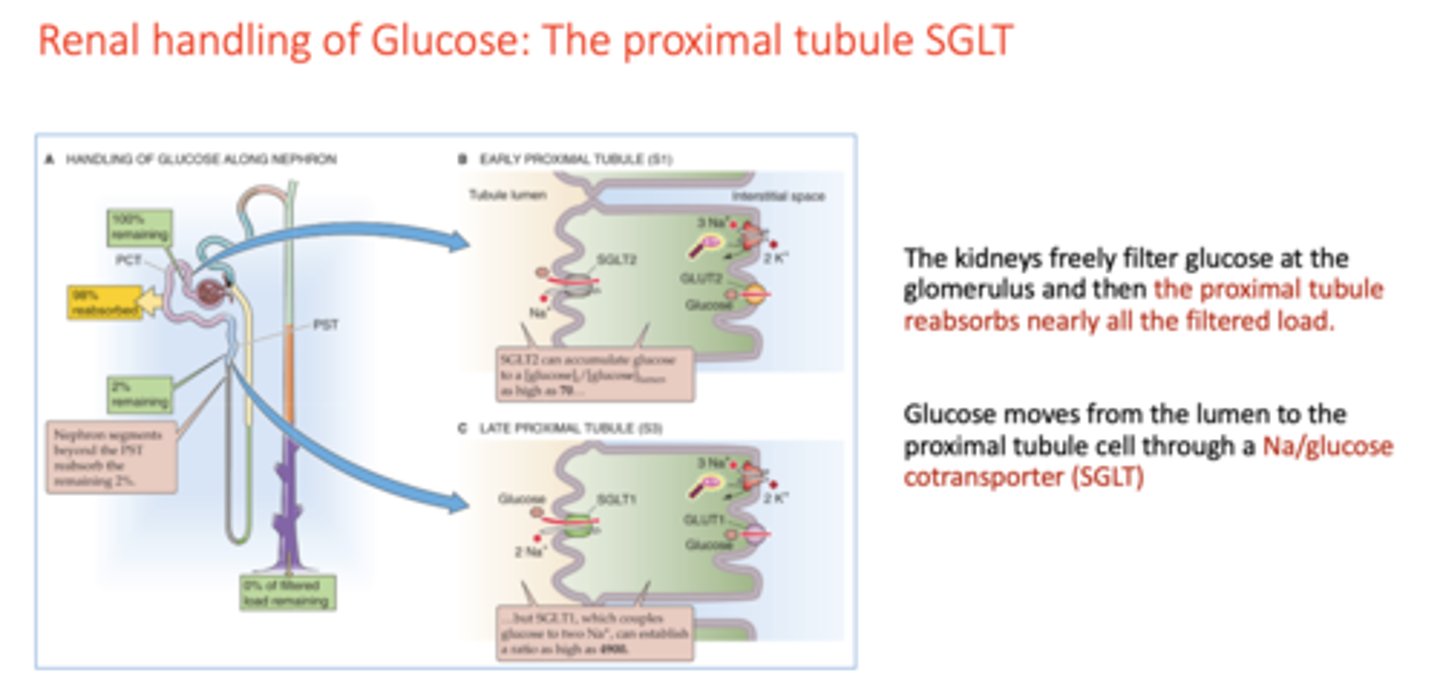
In the early proximal tubule, SGLT2 can accumulate glucose to a [gluocse]i/[glucose]lumen as high as ________. In the late proximal tubule, SGLT1, which couples glucose to two Na+, can establish a ratio as high as _________
70, 4900
what is the plasma [glucose] level threshold that allows glucose excretion to remain zero?
180mg/dL
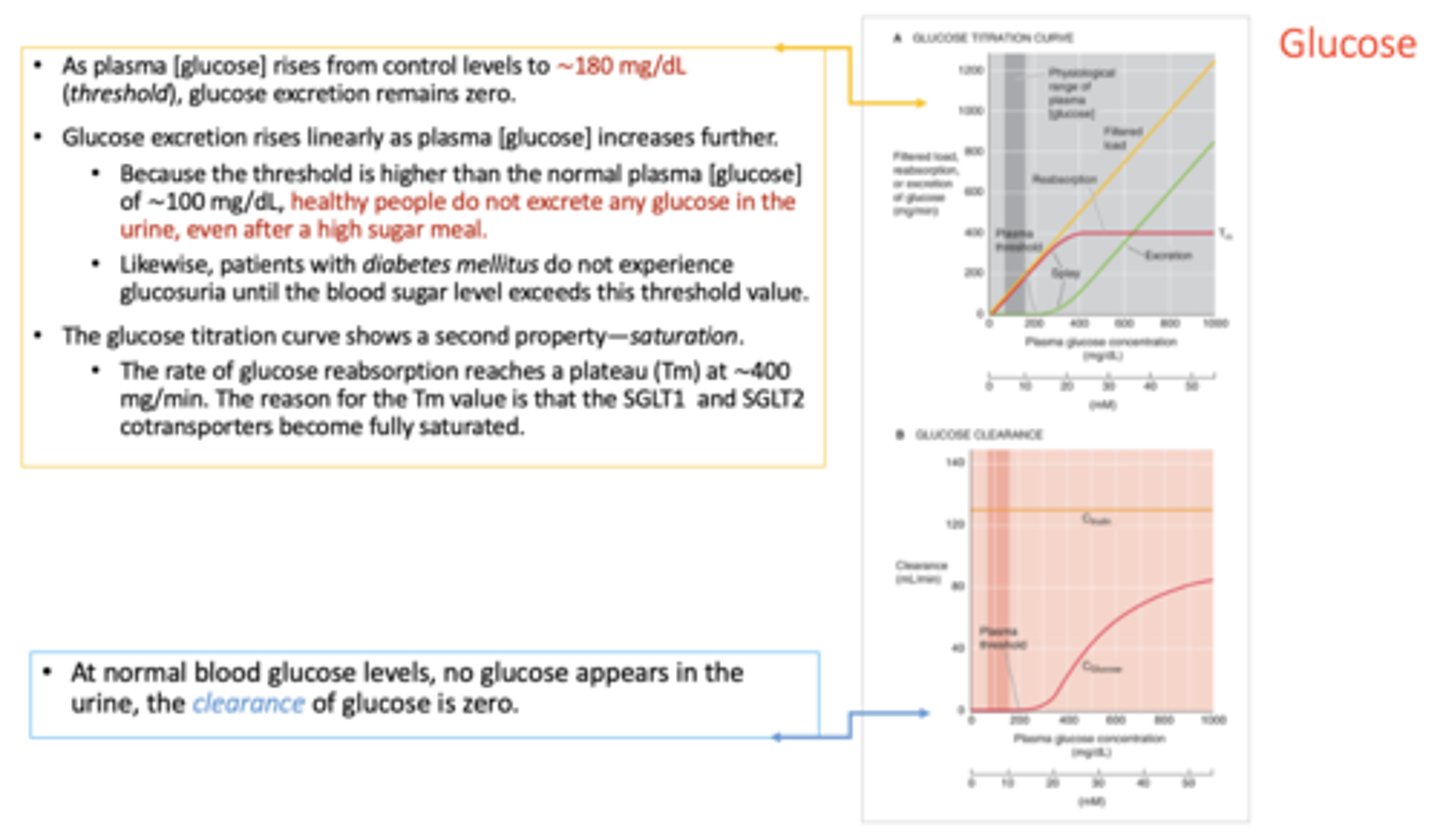
T/F: Because the threshold is higher than the normal plasma [glucose] of ∼100 mg/dL, healthy people do not excrete any glucose in the urine, even after a high sugar meal.
True
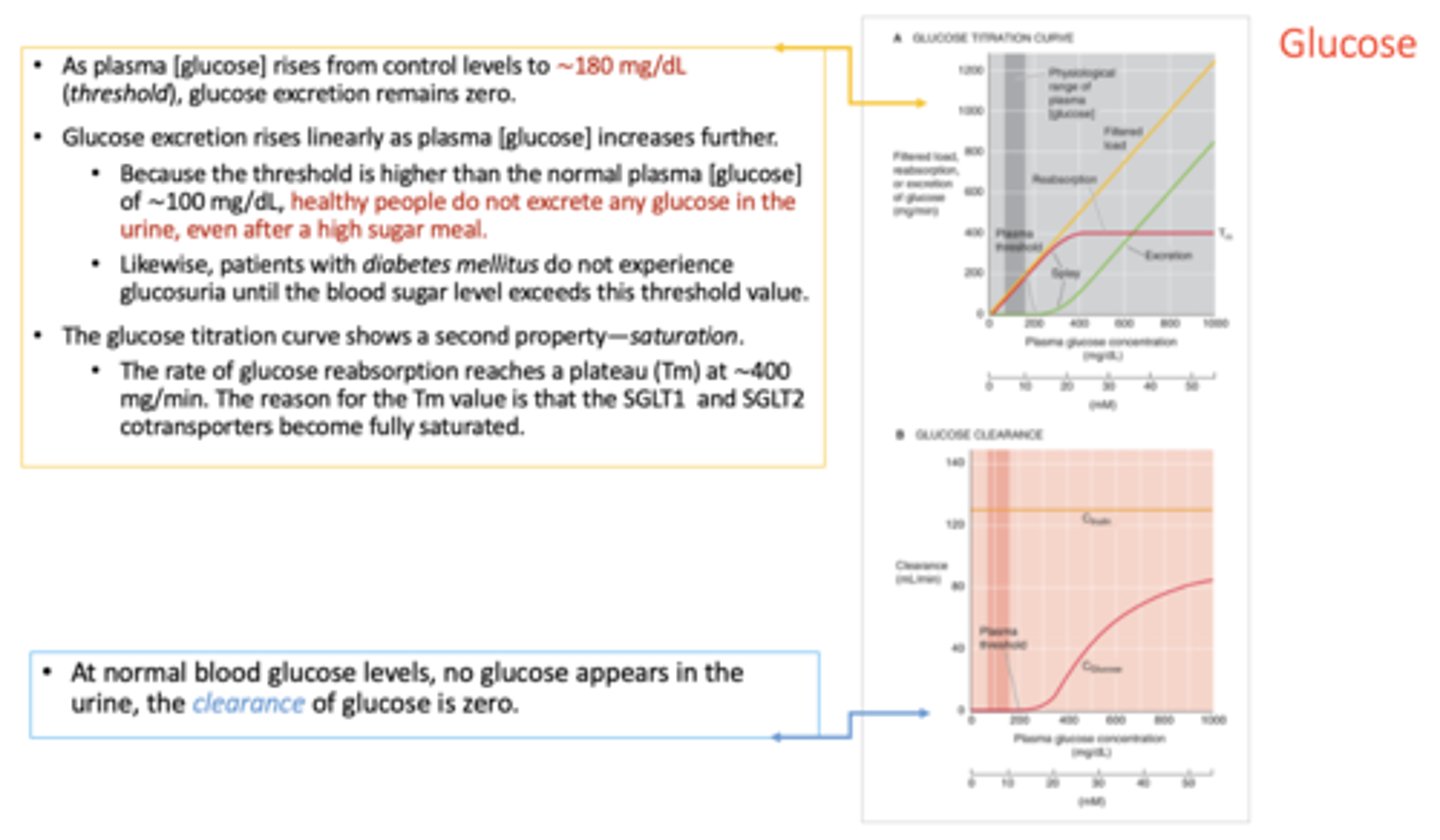
The rate of glucose reabsorption reaches a plateau (Tm) at ∼___________. The reason for the Tm value is that the SGLT1 and SGLT2 cotransporters become fully saturated.
400 mg/min
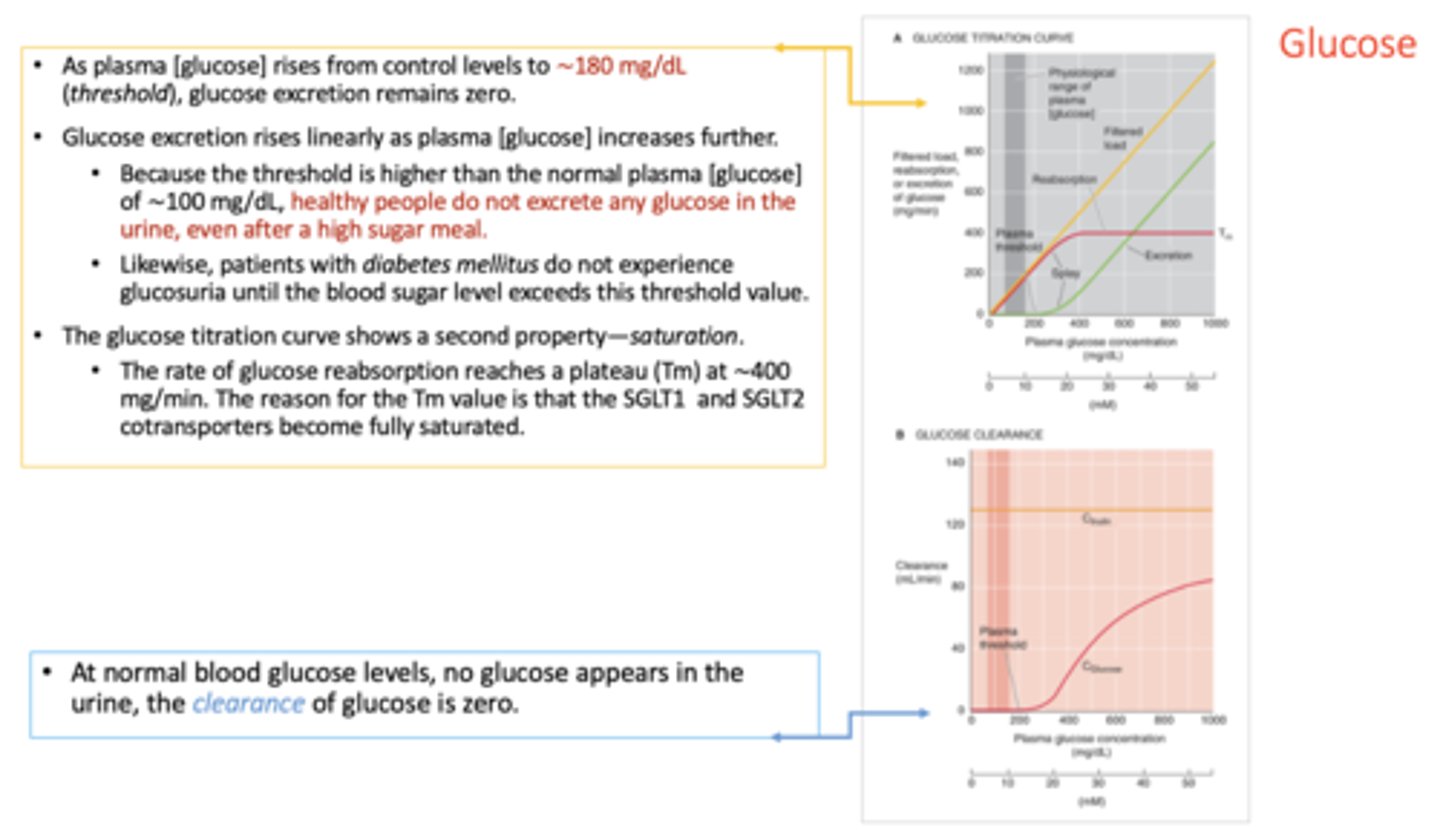
At normal blood glucose loads, when no glucose appears in the urine, the clearance of glucose is ____
Zero
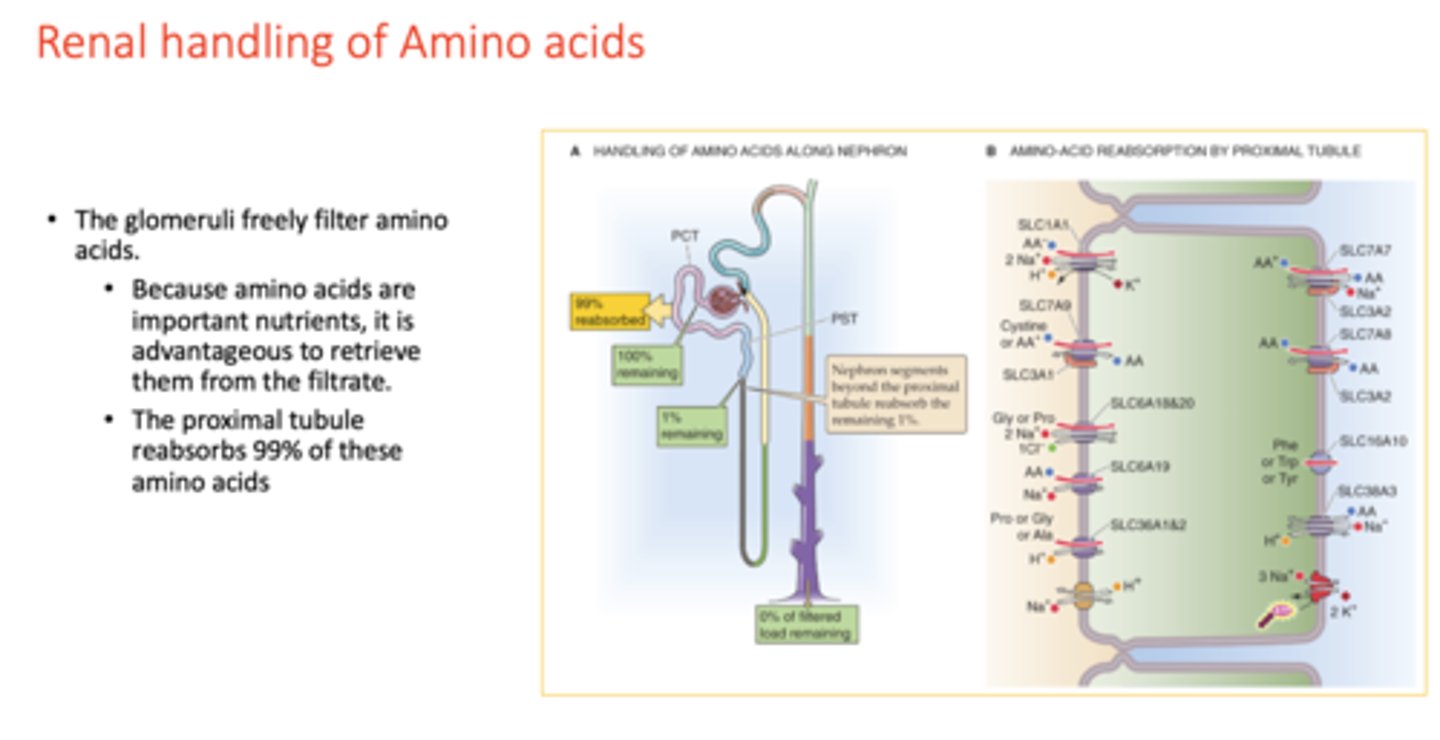
t/f: the glomeruli freely filter amino acids
true
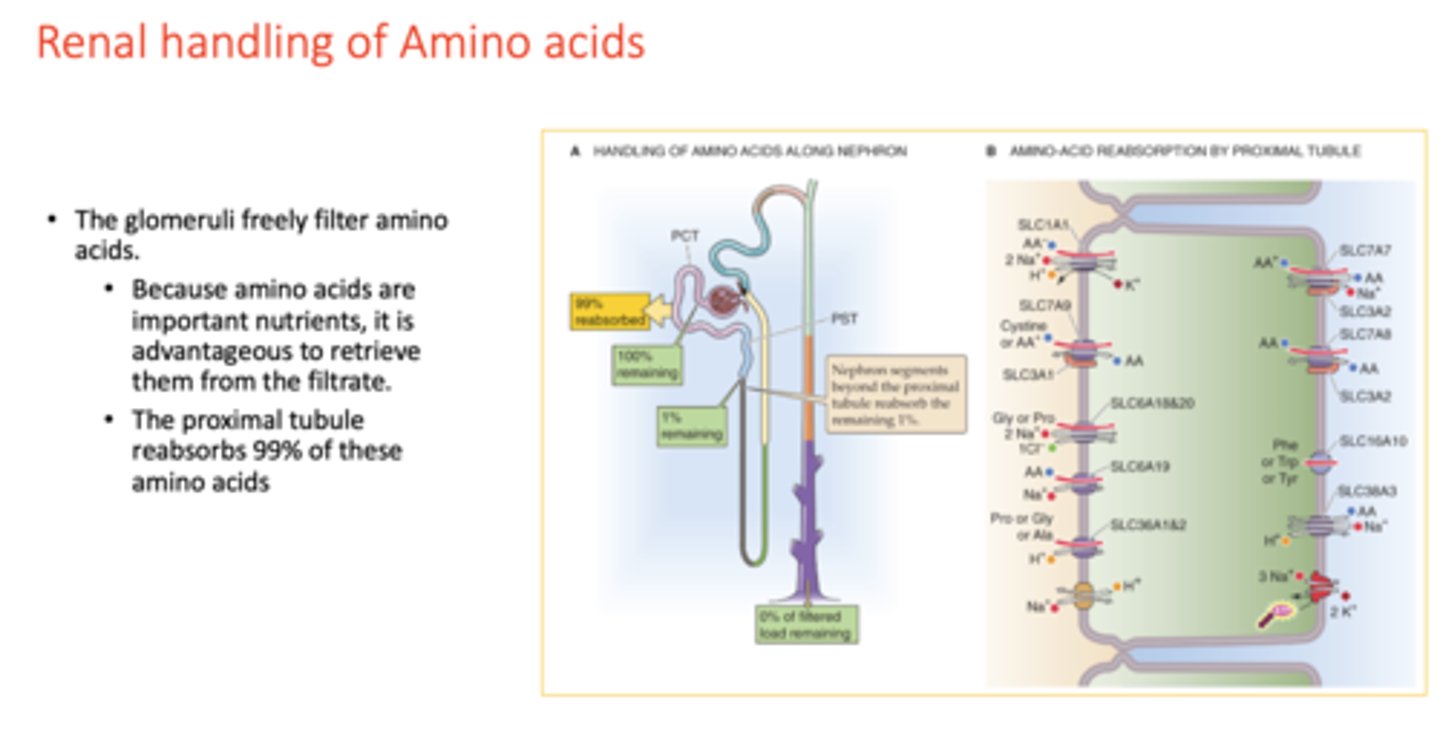
proximal tubule reabsorbs more than ___ of these amino acids
99%
What disease is the following:
- Amino acids: Neutral and ring-structure amino acids (e.g. phenylalanine)
- MOA: Defective SLC6A19; Autosomal recessive disease
Hartnup disease (neutral aminoaciduria)
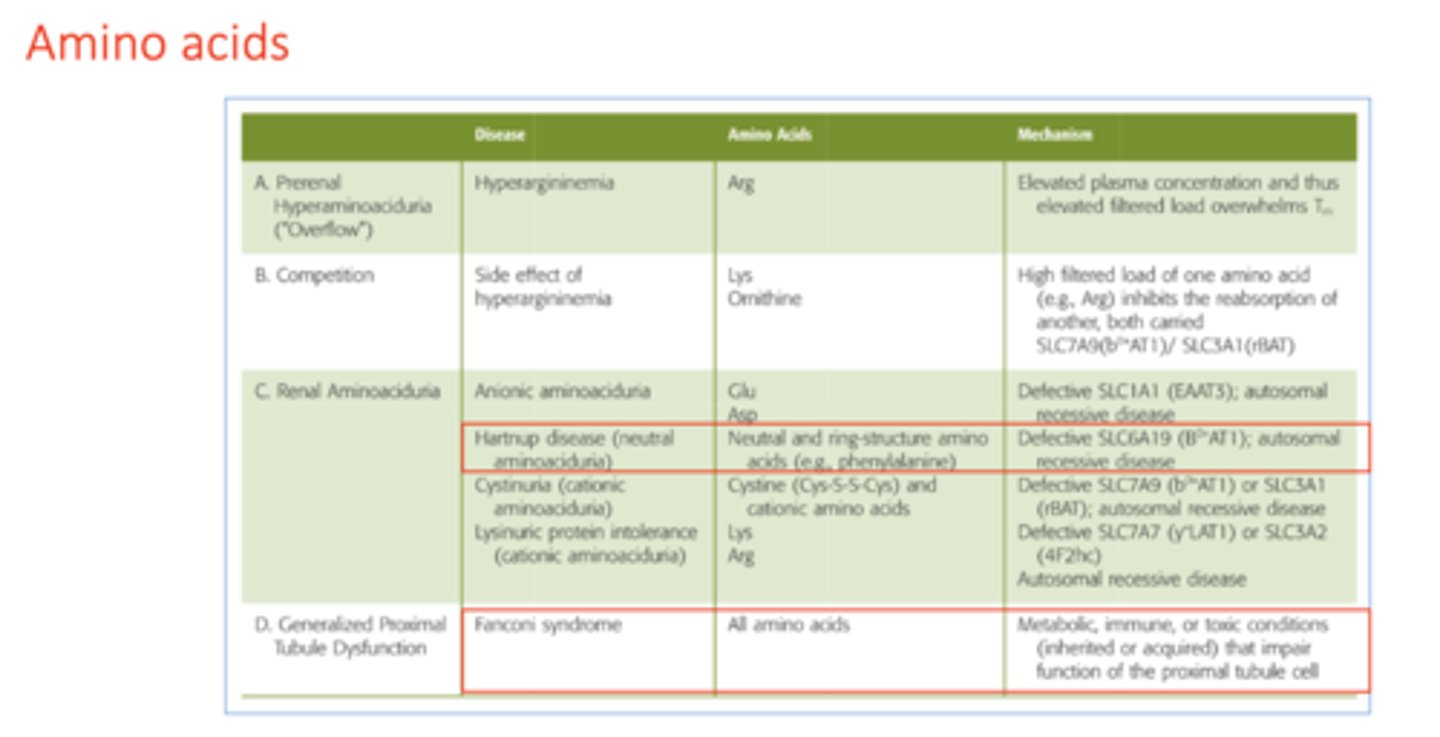
What disease is the following:
- Amino acids: All amino acids
- MOA: Metabolic, immune, or toxic conditions (inherited or acquired) that impair function of the proximal tubule cell
Fanconi syndrome
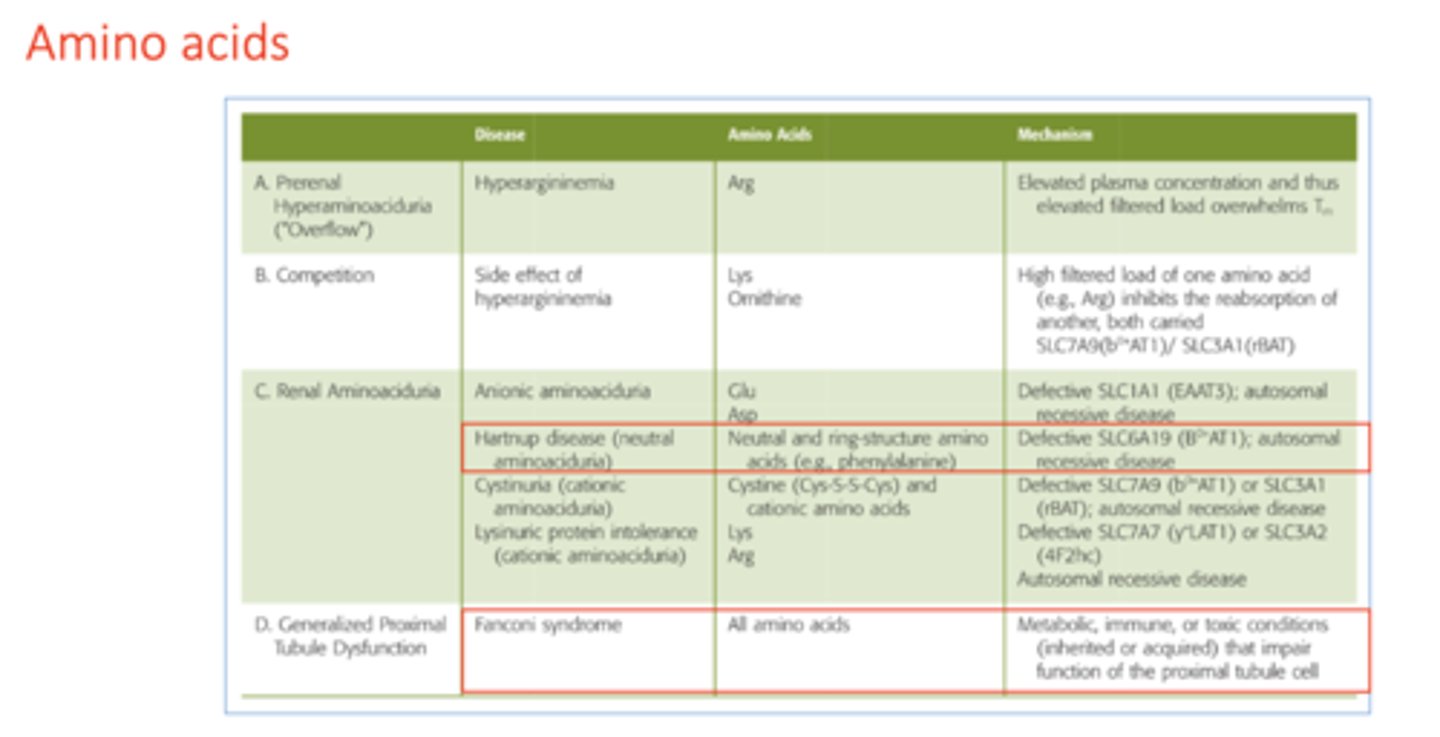
disease where neutral and ring structured amino acids are secreted in to the urine:
Hartnup disease
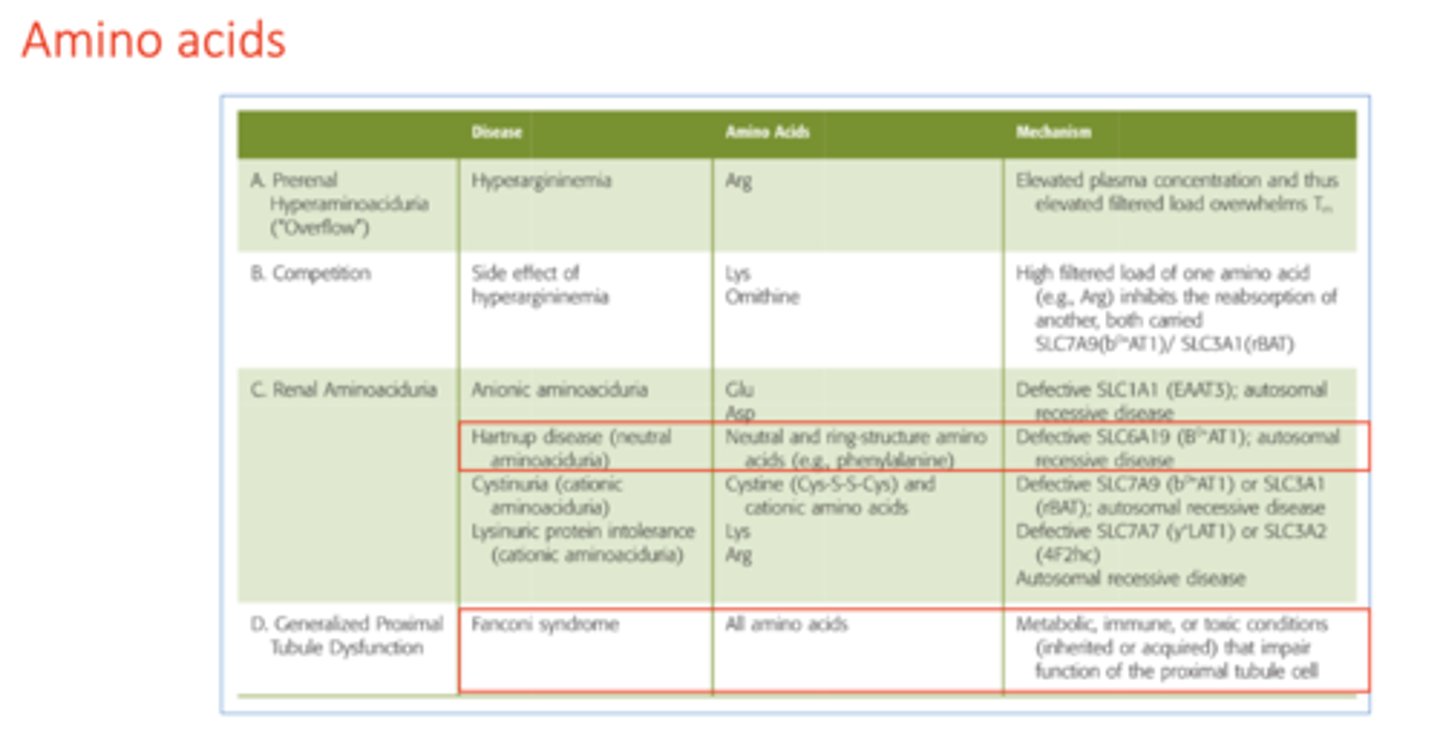
disease where all amino acids are secreted into the urine:
Fanconi syndrome
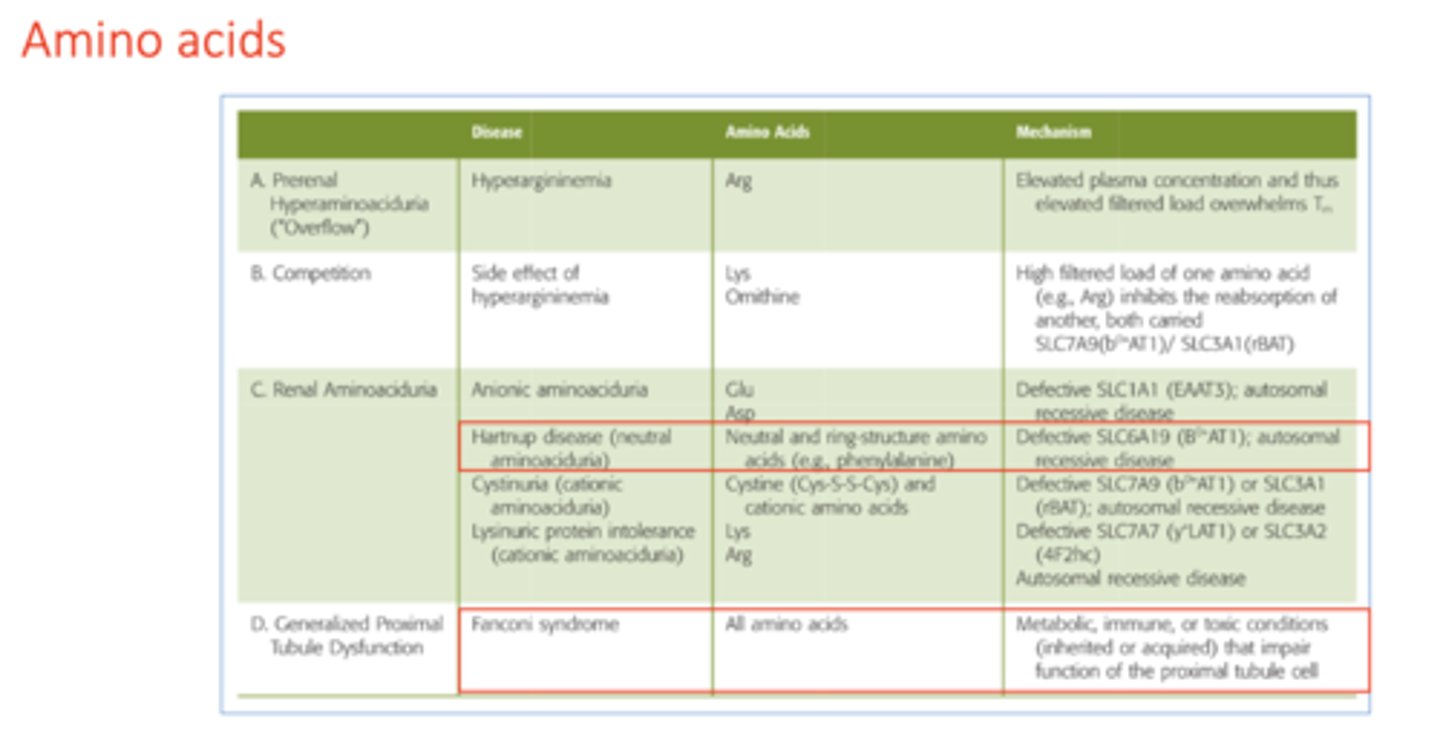
what is the cause of Fanconi syndrome?
impaired function of proximal tubule cells
of the 3 kidneys functions, Amino Acids normally experiences:
filtration
reabsorption

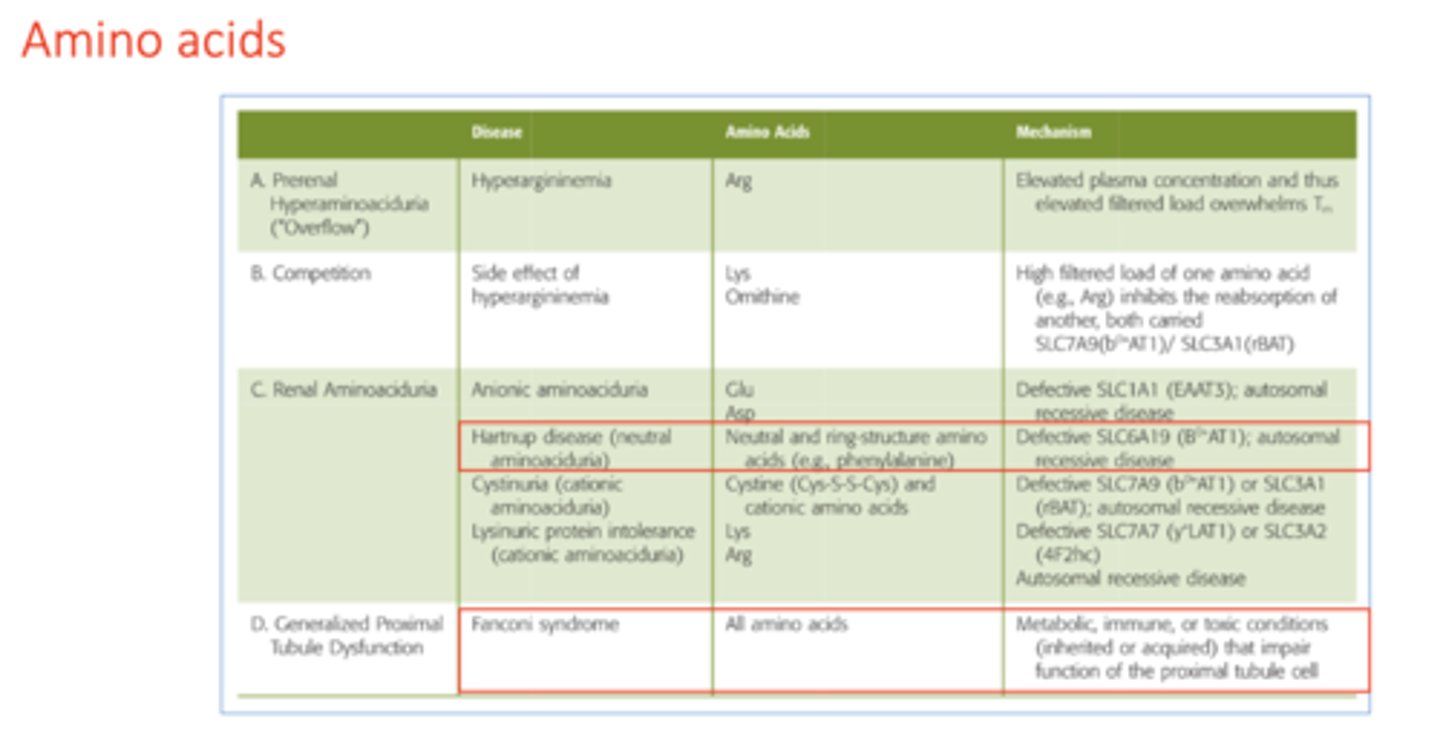
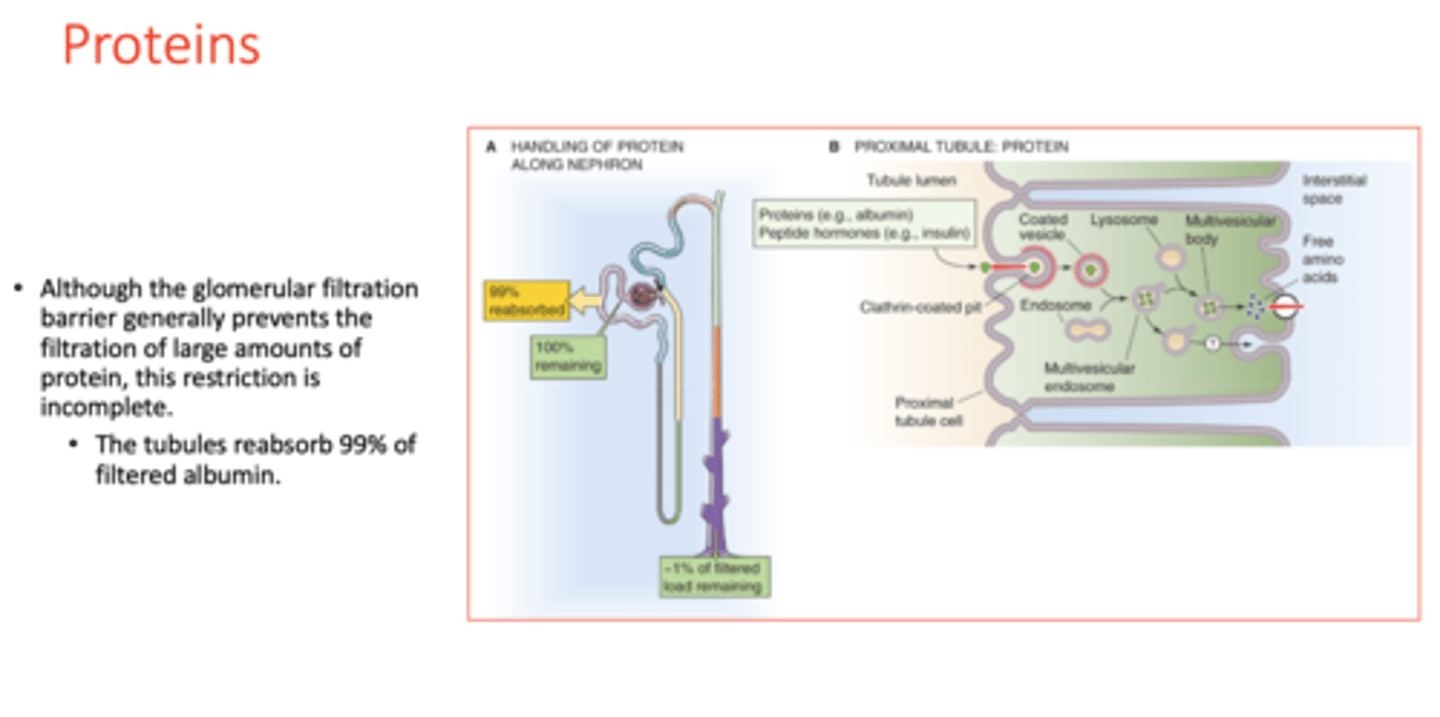
the tubules reabsorb ________ of filtered albumin
99%
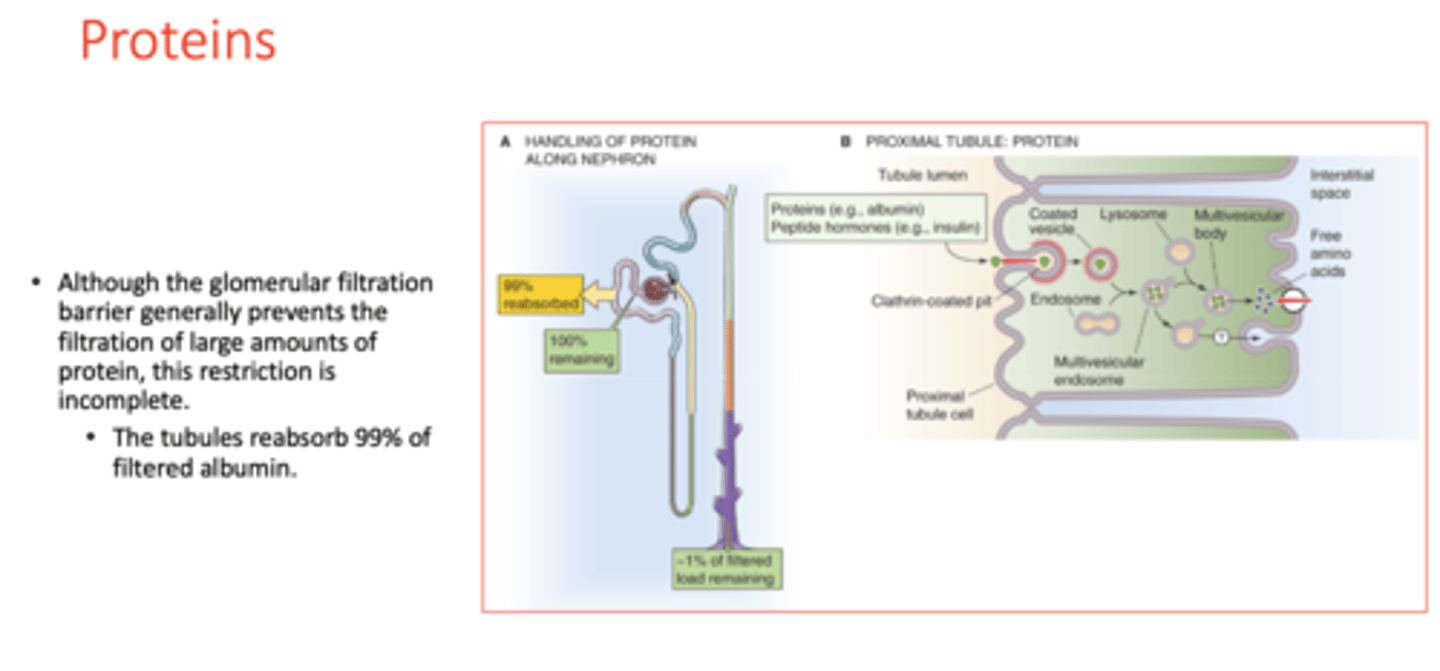
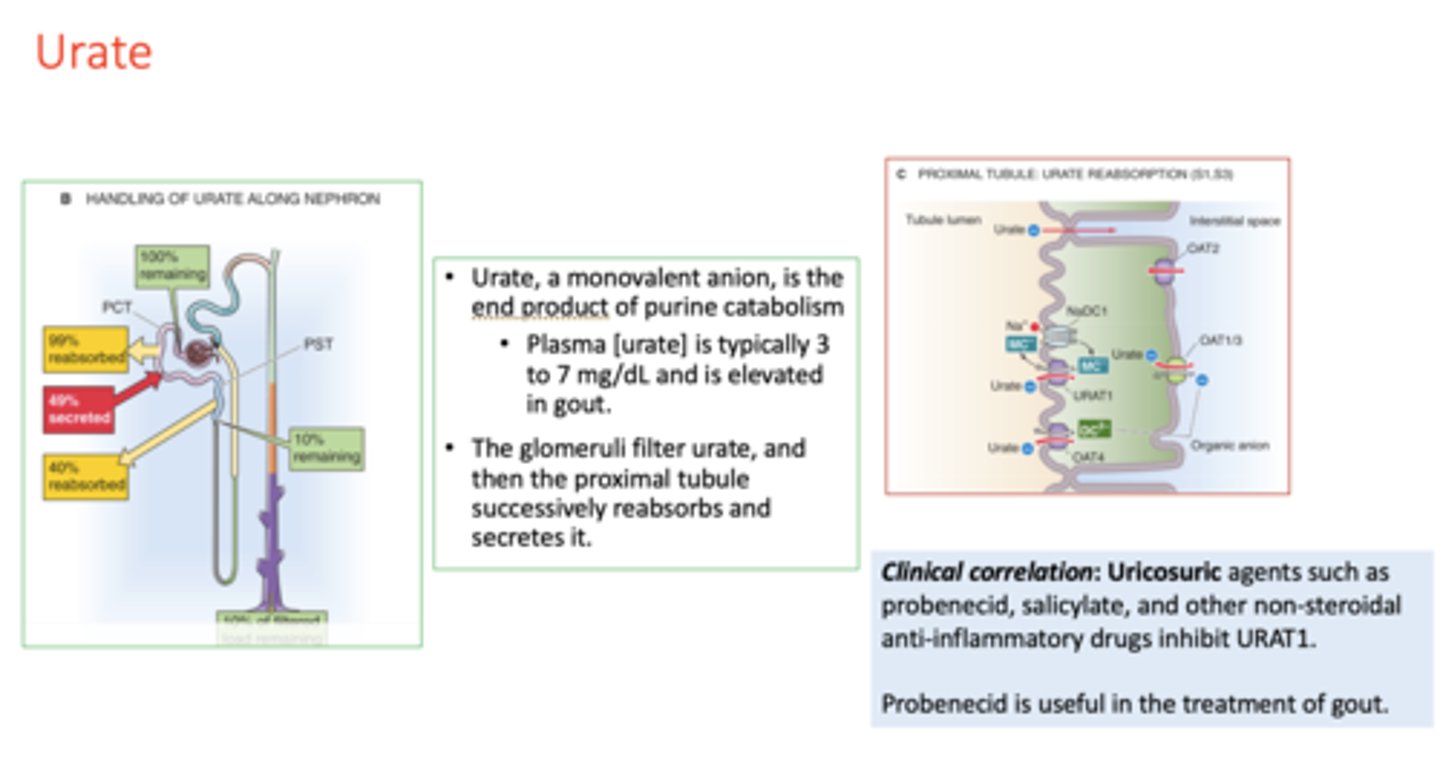
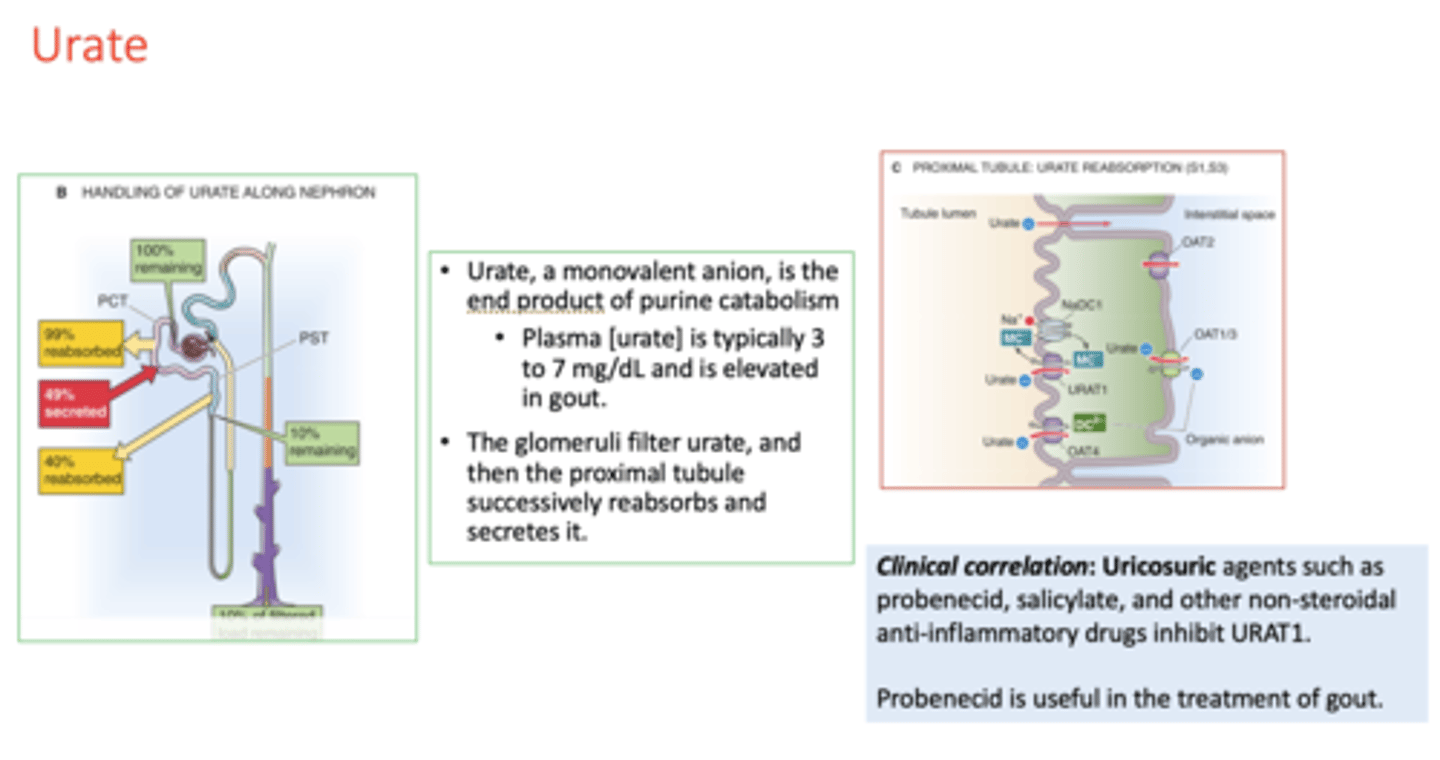
Plasma [urate] is typically ______ to ______ mg/dL
3 to 7 mg/dL
this plasma concentration is elevated in patients w/ gout:
urate
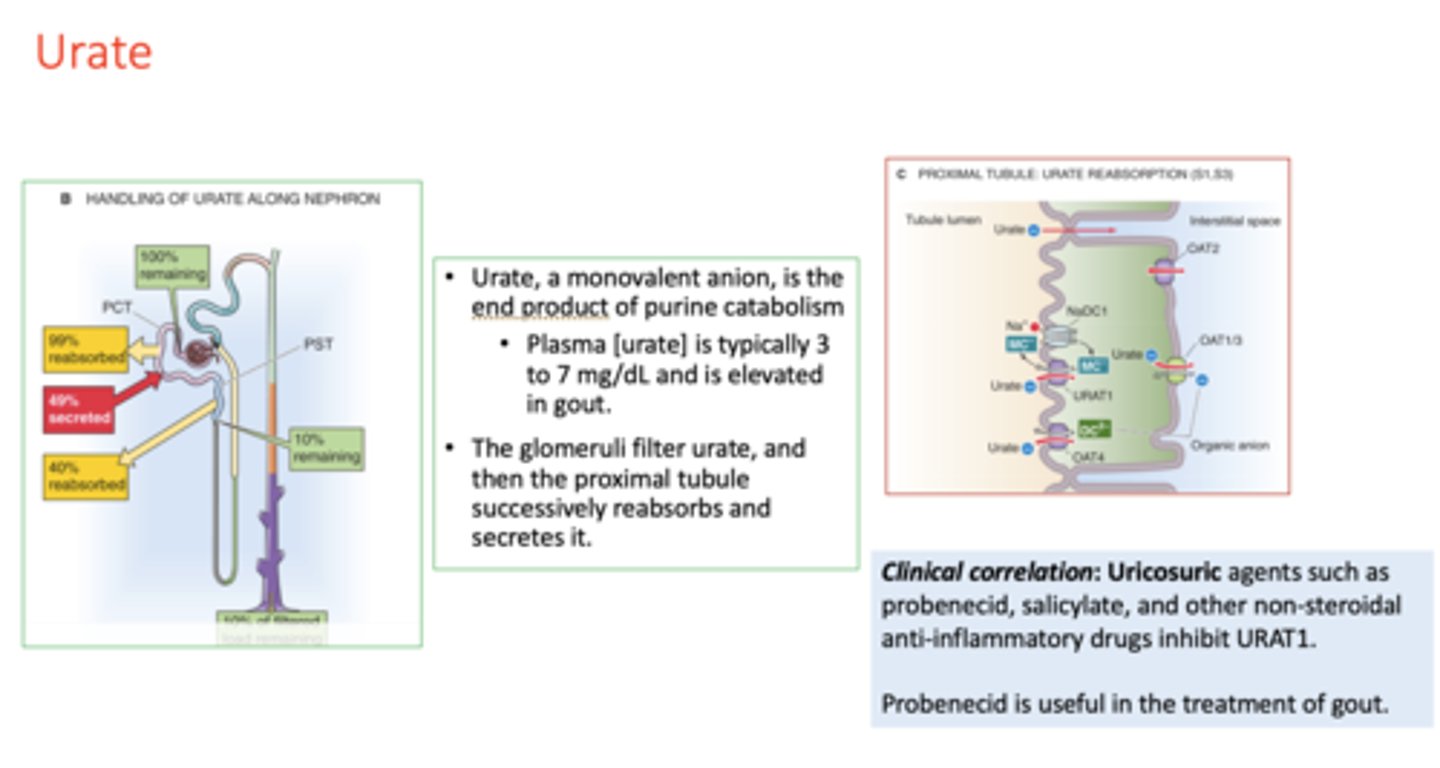
___________ agents such asprobenecid, salicylate, and other non-steroidalanti-inflammatory drugs inhibit URAT1
uricosuric
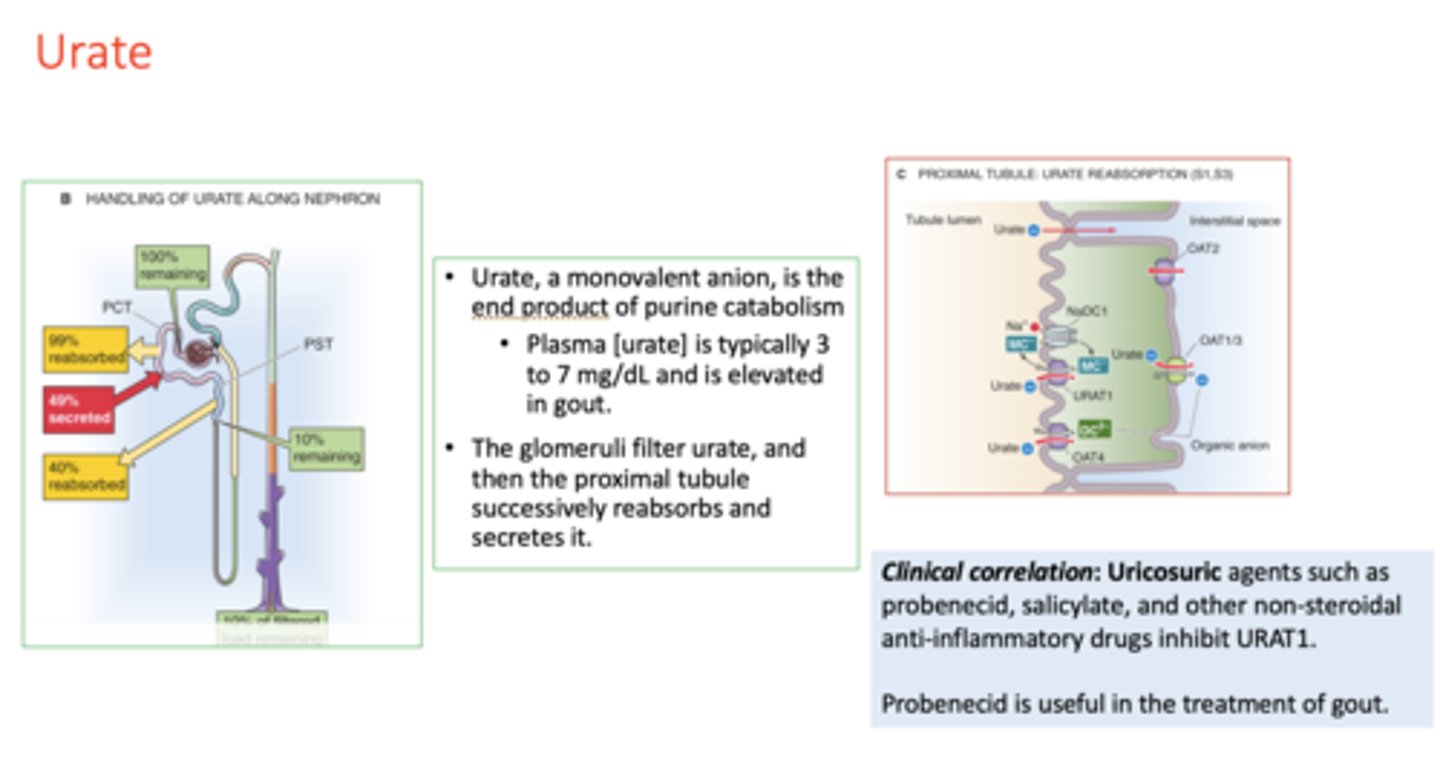
What drug is useful in the treatment of gout?
probenecid
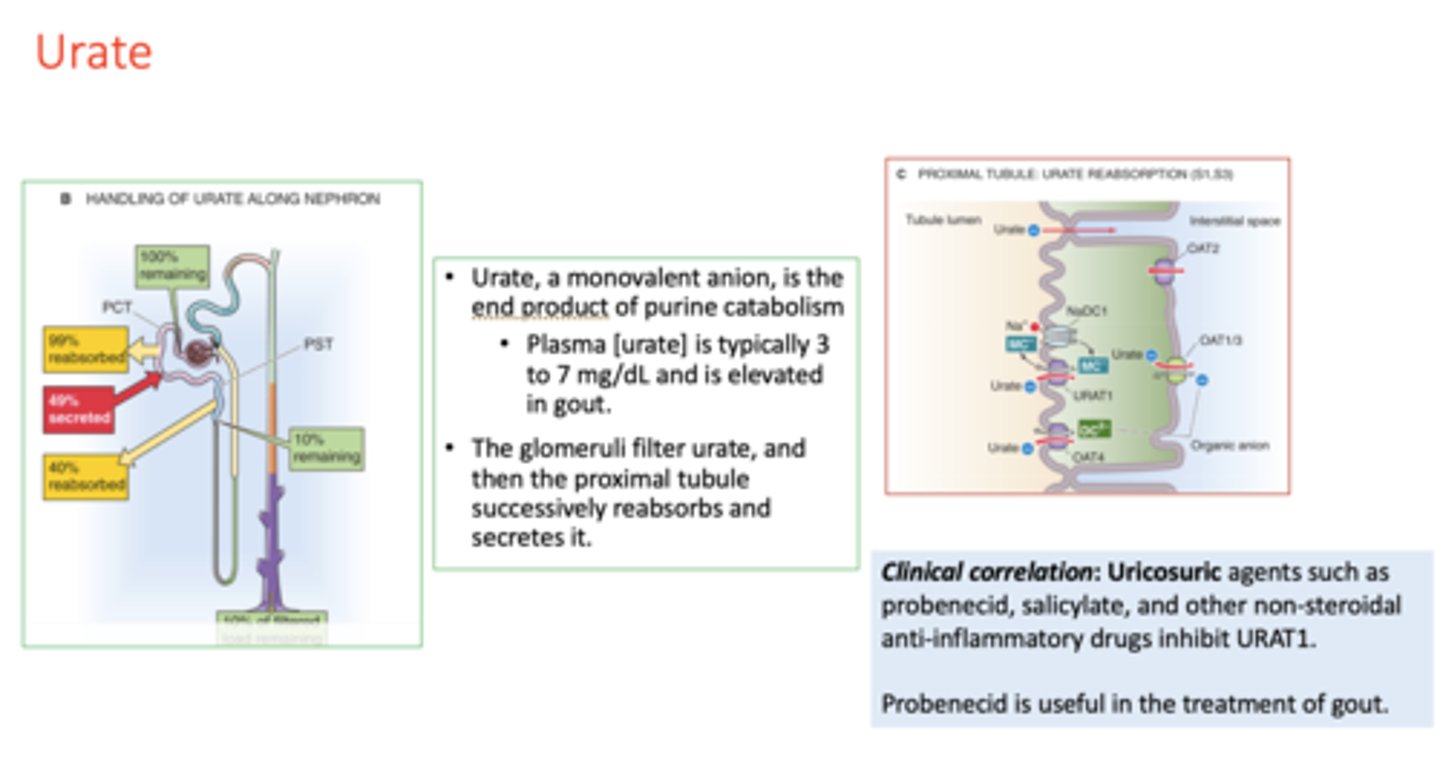
t/f: The glomeruli filter urate, and then the proximal tubule successively reabsorbs and secretes it
true
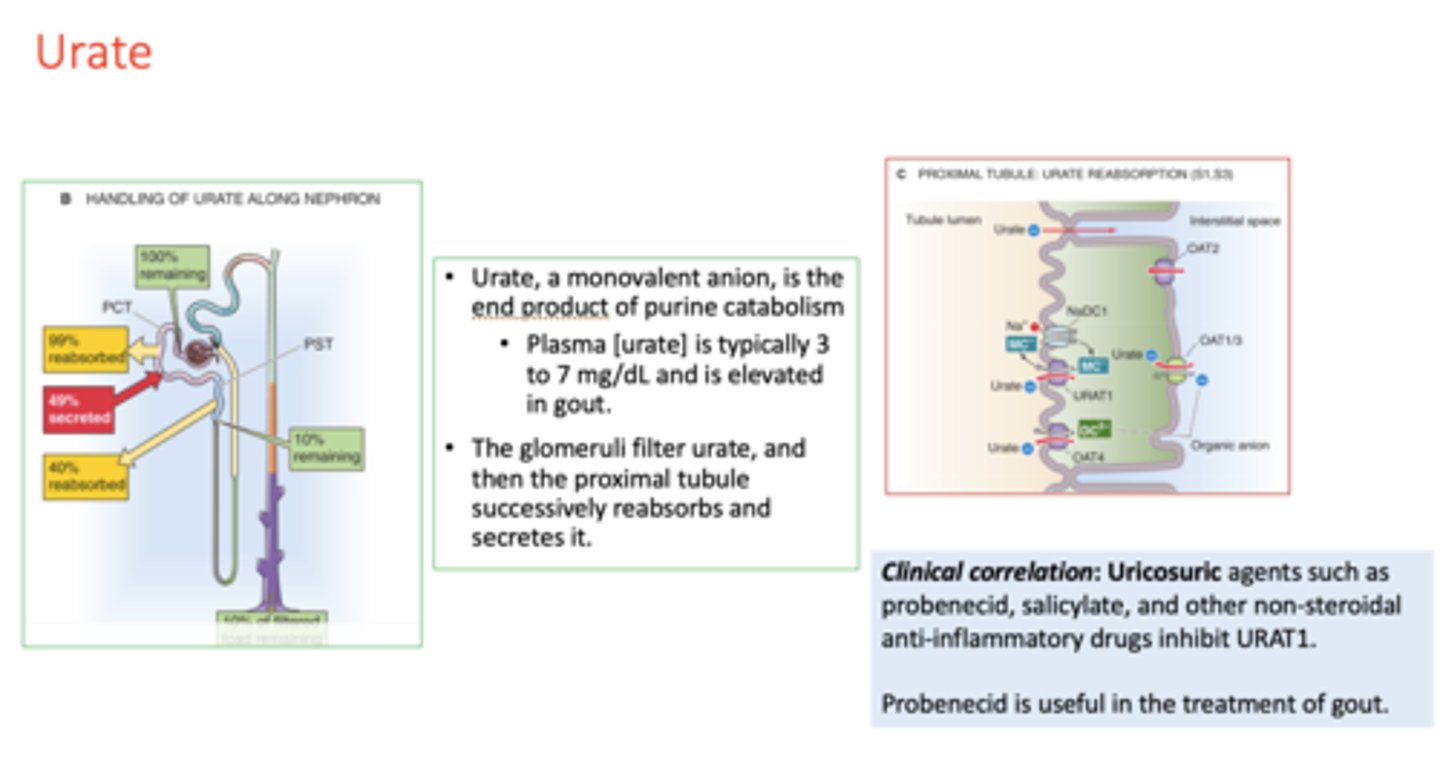
Uricosuric agents such as probenecid, salicylate, and other non-steroidal anti-inflammatory drugs inhibit _____
URAT1
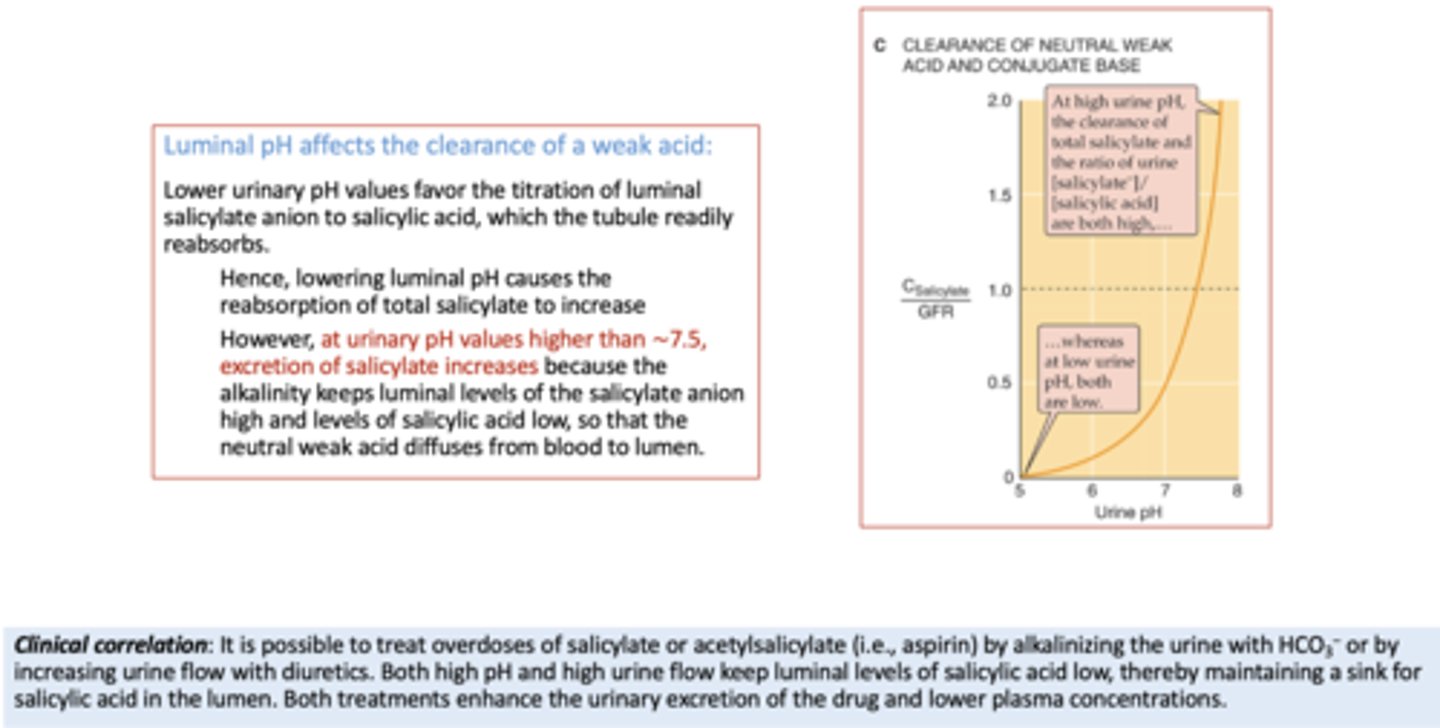
acidifying the tubule lumen promotes the reabsorption of a neutral _________ and secretion of a neutral weak base
weak acid
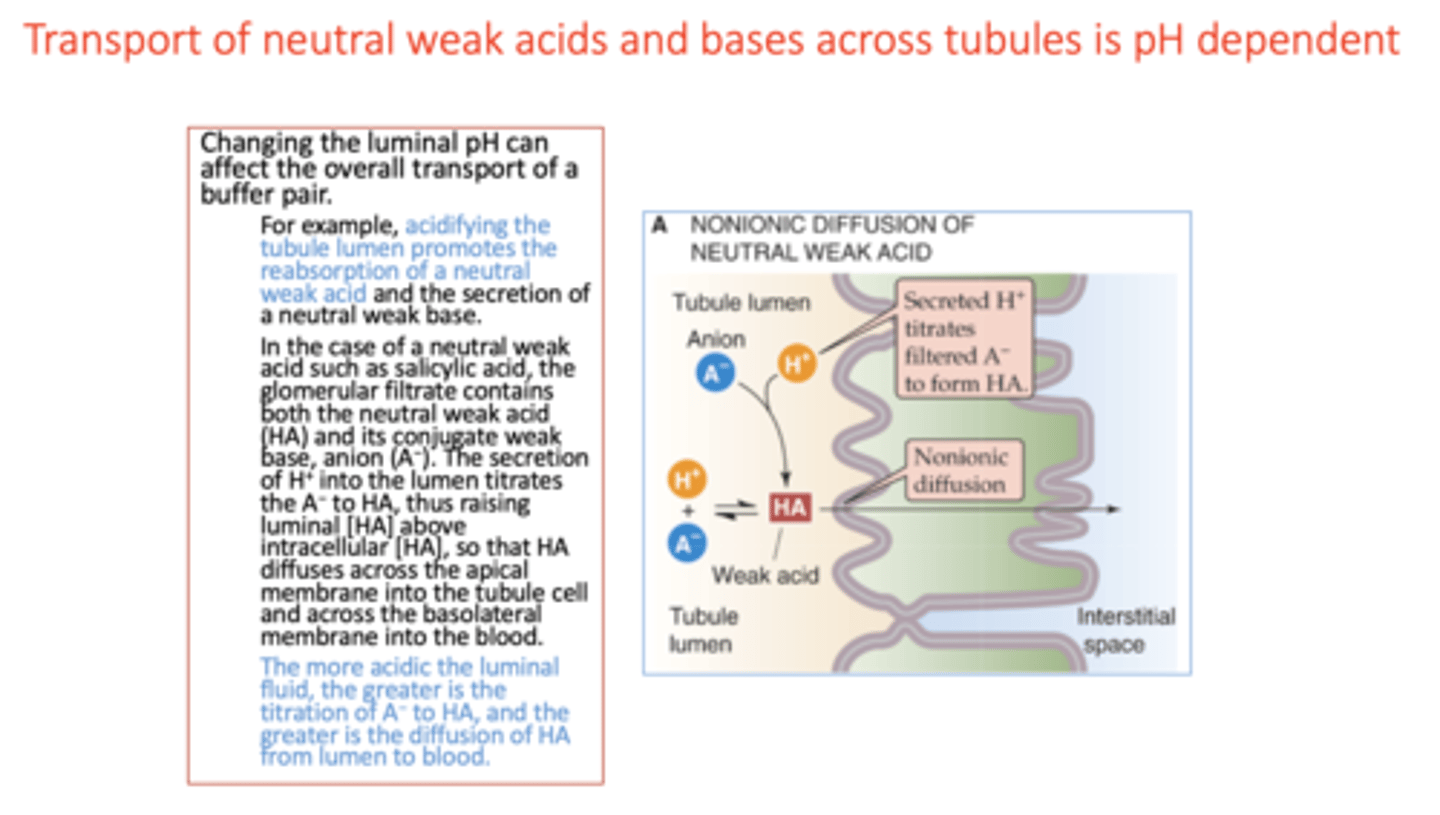
transport of neutral weak acids and bases across tubules is ______ dependent
pH
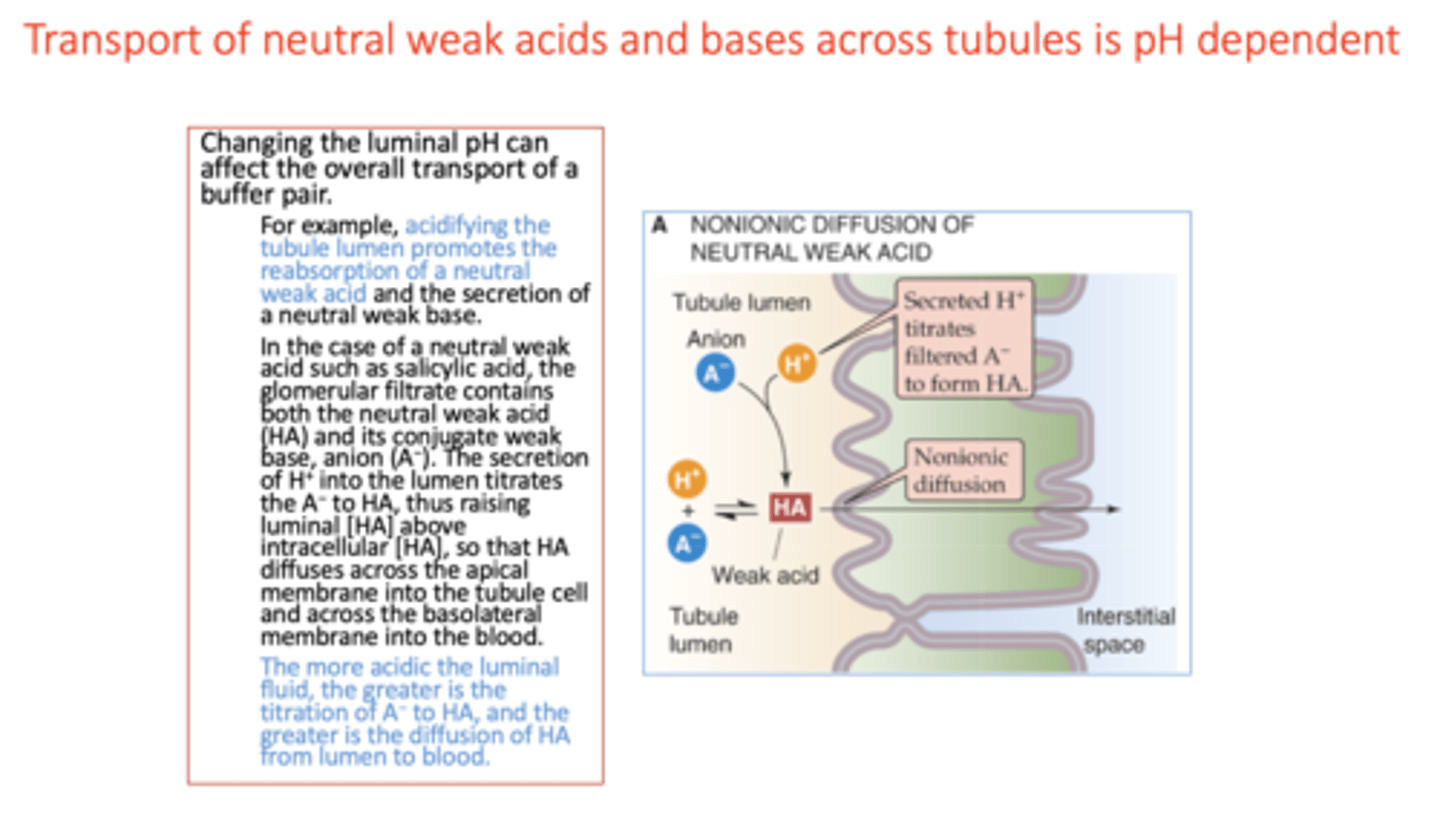
The more _________ the luminal fluid, the greater is the titration of A− to HA, and the greater is the diffusion of HA from lumen to blood.
acidic

lowering luminal pH causes the reabsorption of salicylate to ____
increases
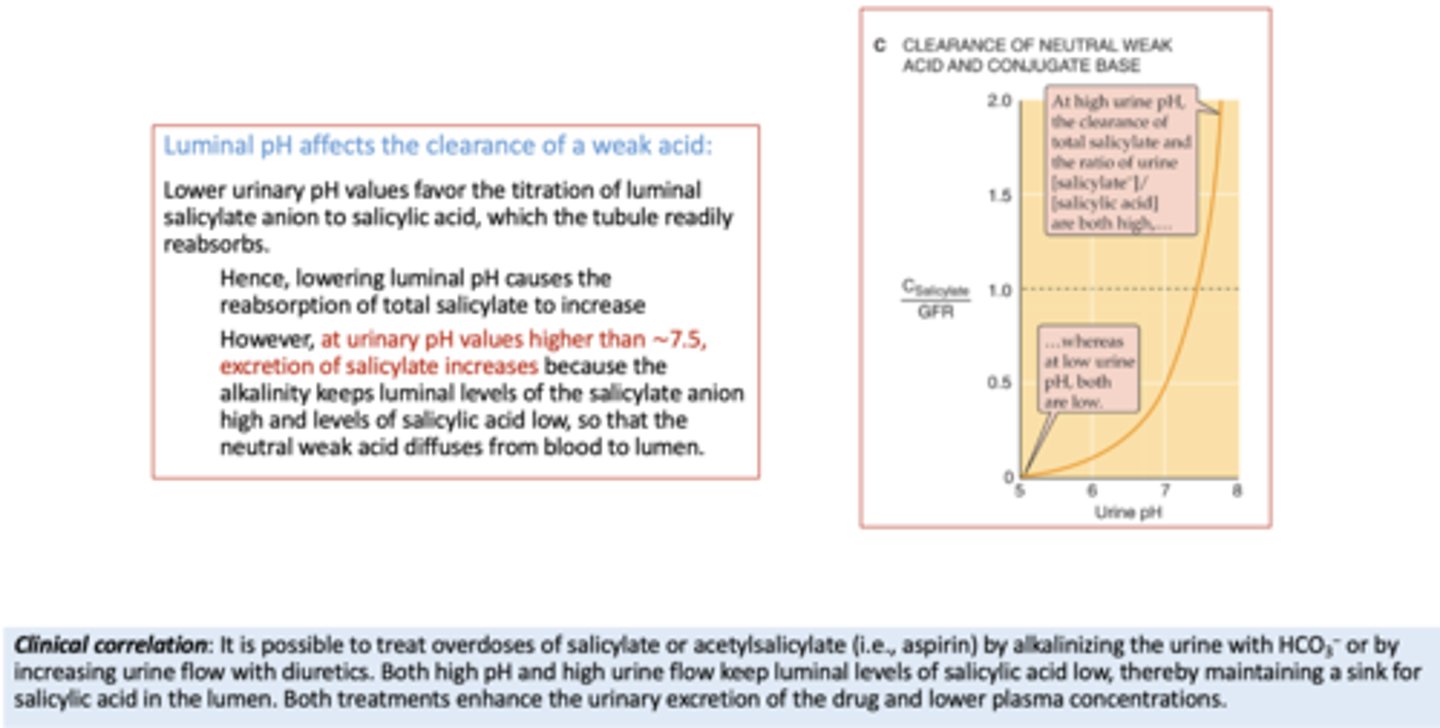
With urinary pH values higher than ∼7.5, excretion of salicylate ___________
increases
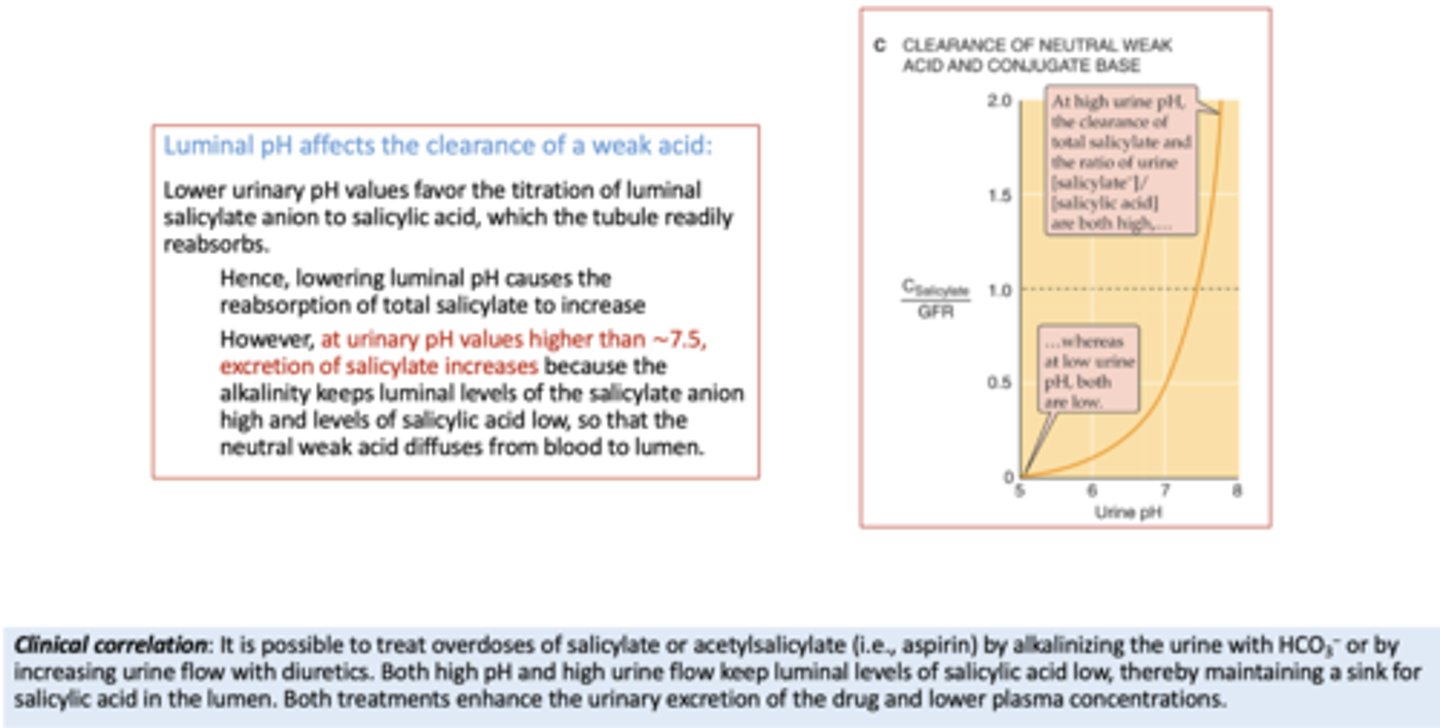
Luminal pH affects the clearance of a ___________
weak acid
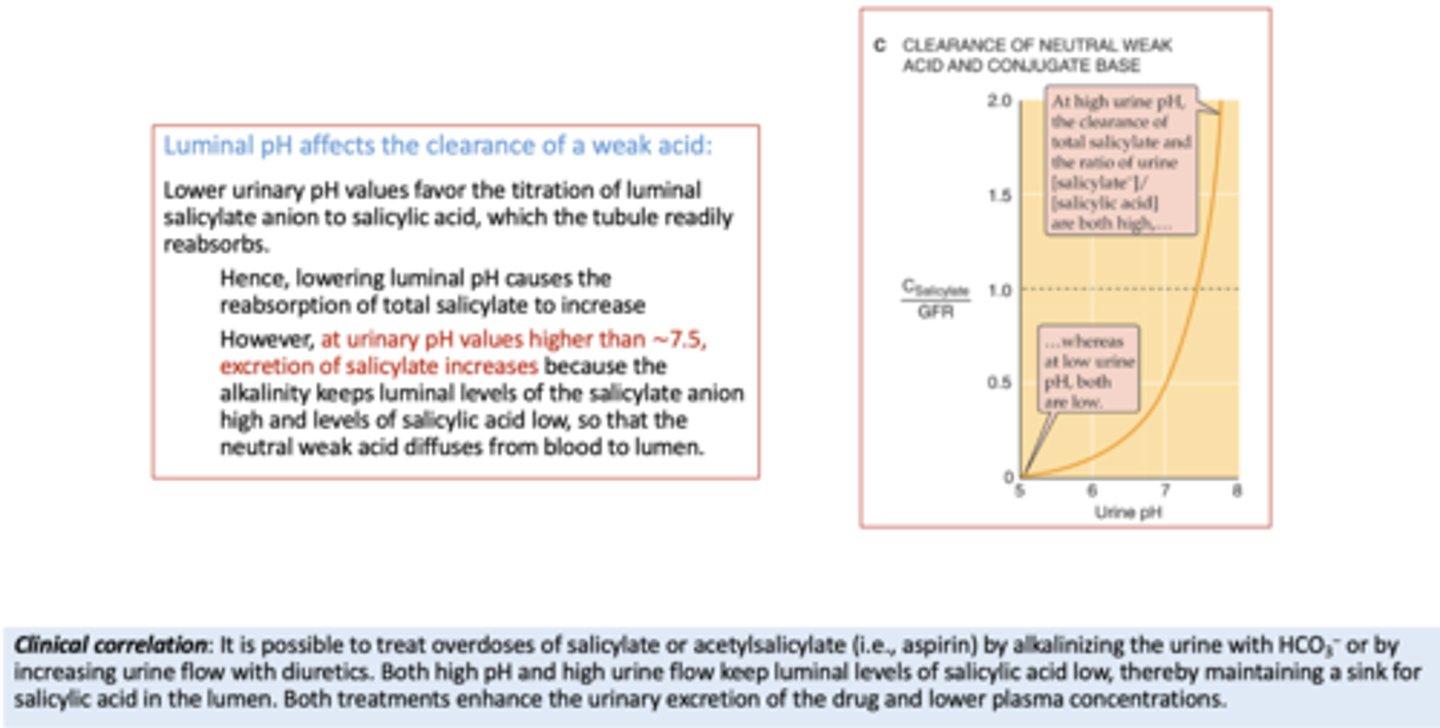
It is possible to treat overdoses of salicylate or acetylsalicylate (i.e., aspirin) by (2)
- Alkalinizing the urine with HCO3−
- Diuretics
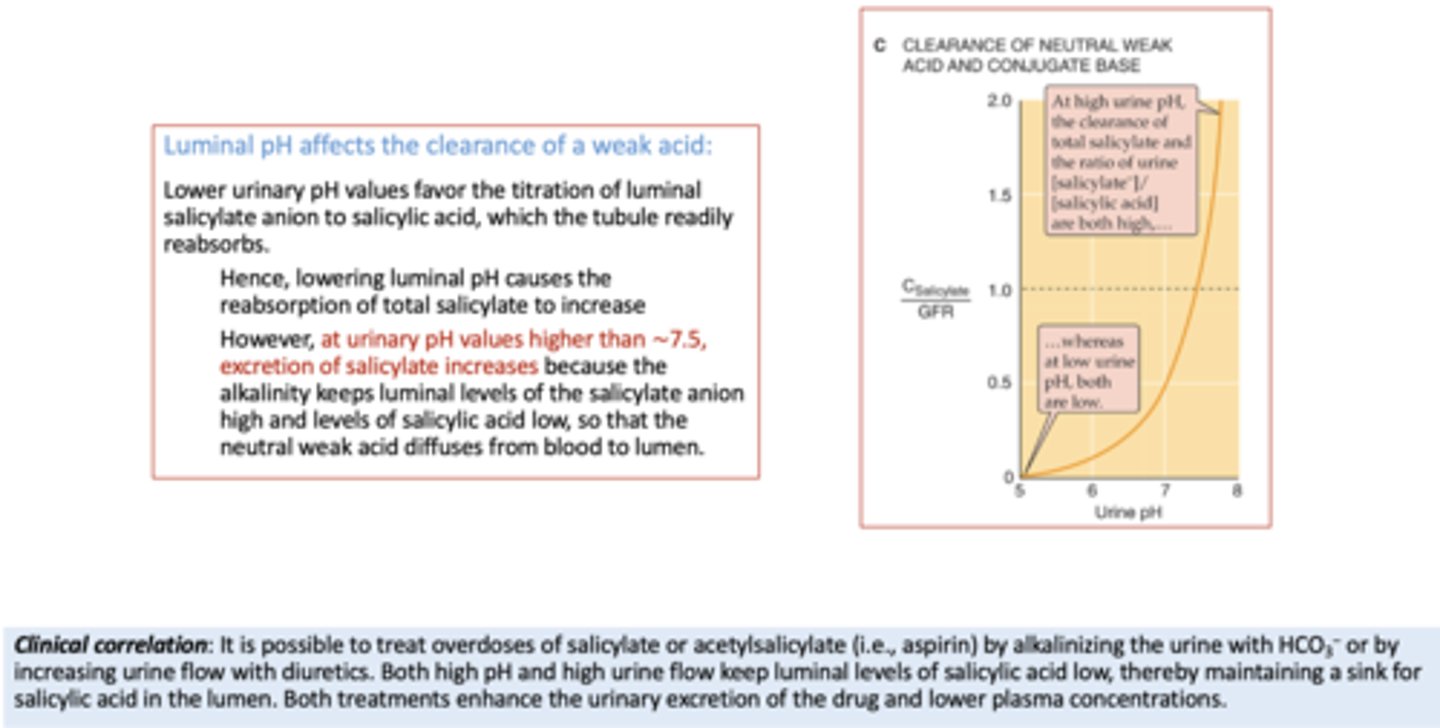
a _____ pH will increase salicyate acid absorption
low
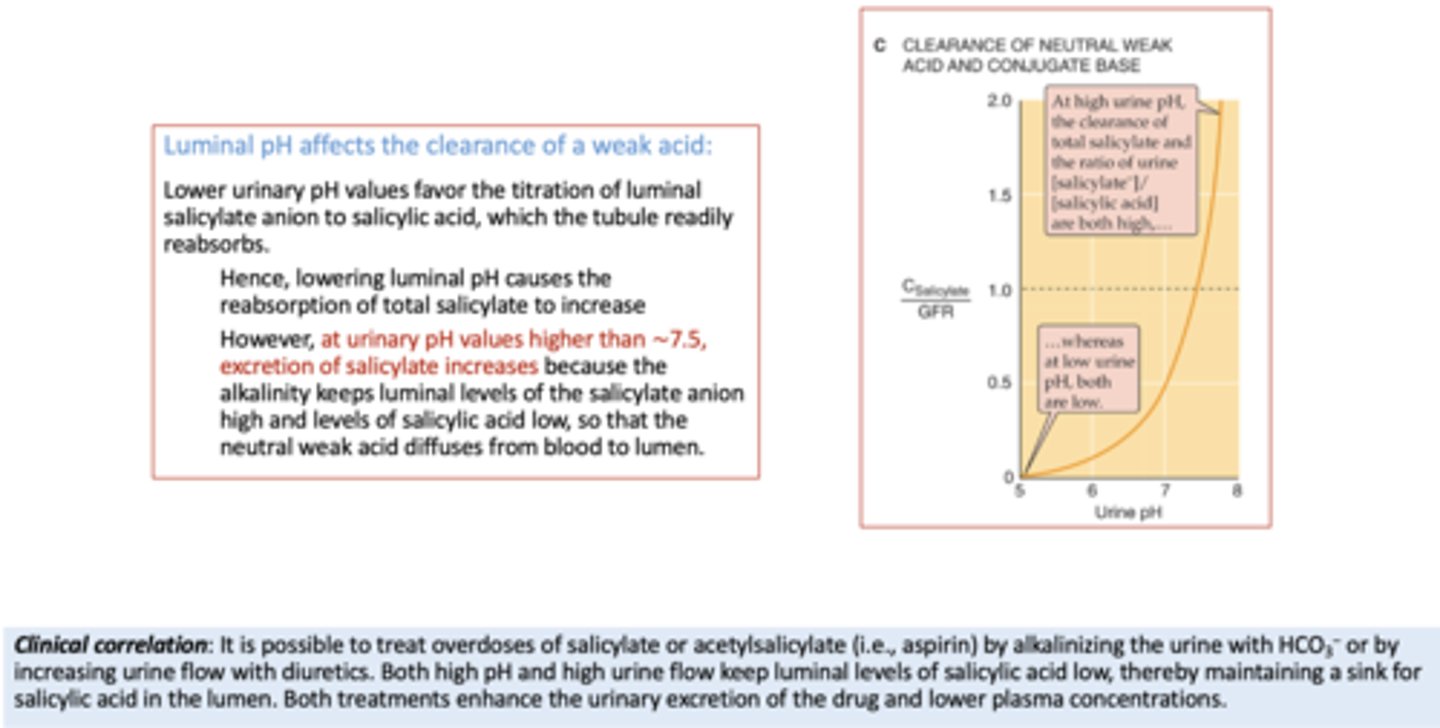
a _____ pH will decrease salicyate acid absorption
high
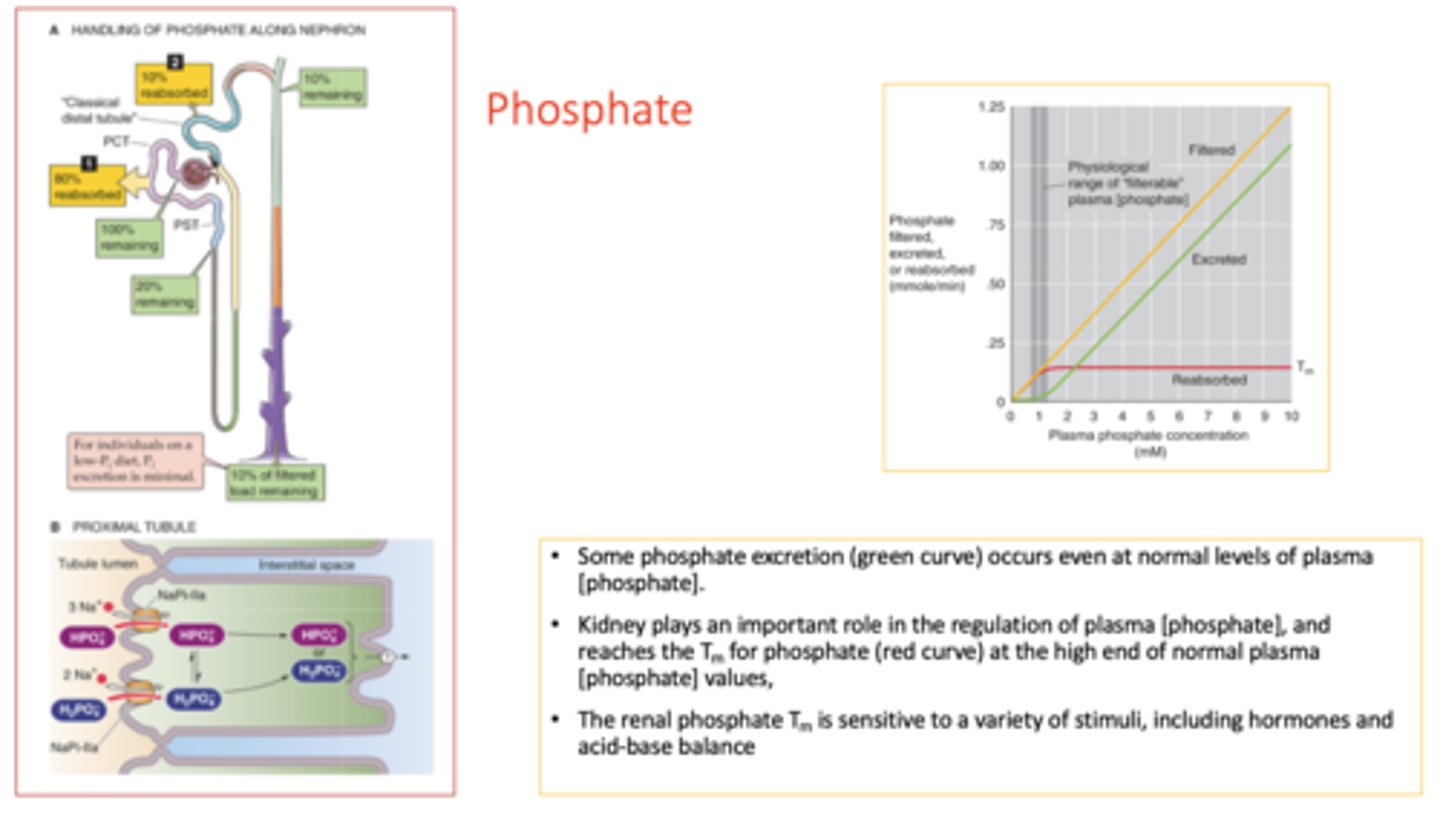
The __________ plays an important role in the regulation of plasma [phosphate], and reaches the Tm for phosphate (red curve) at the high end of normal plasma [phosphate] values
Kidney
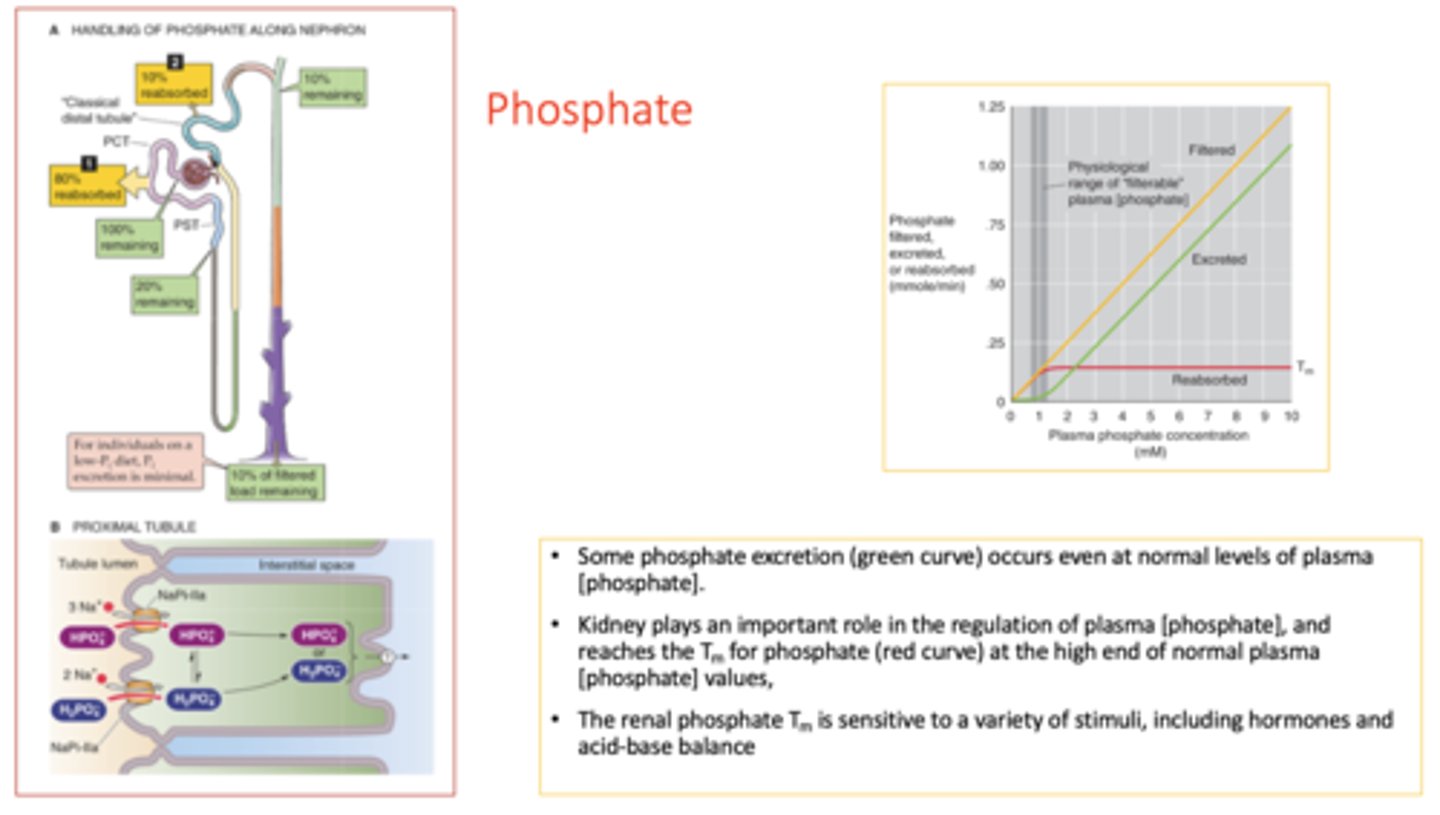
The renal phosphate Tm is sensitive to a variety of stimuli, including...
hormones and acid-base balance
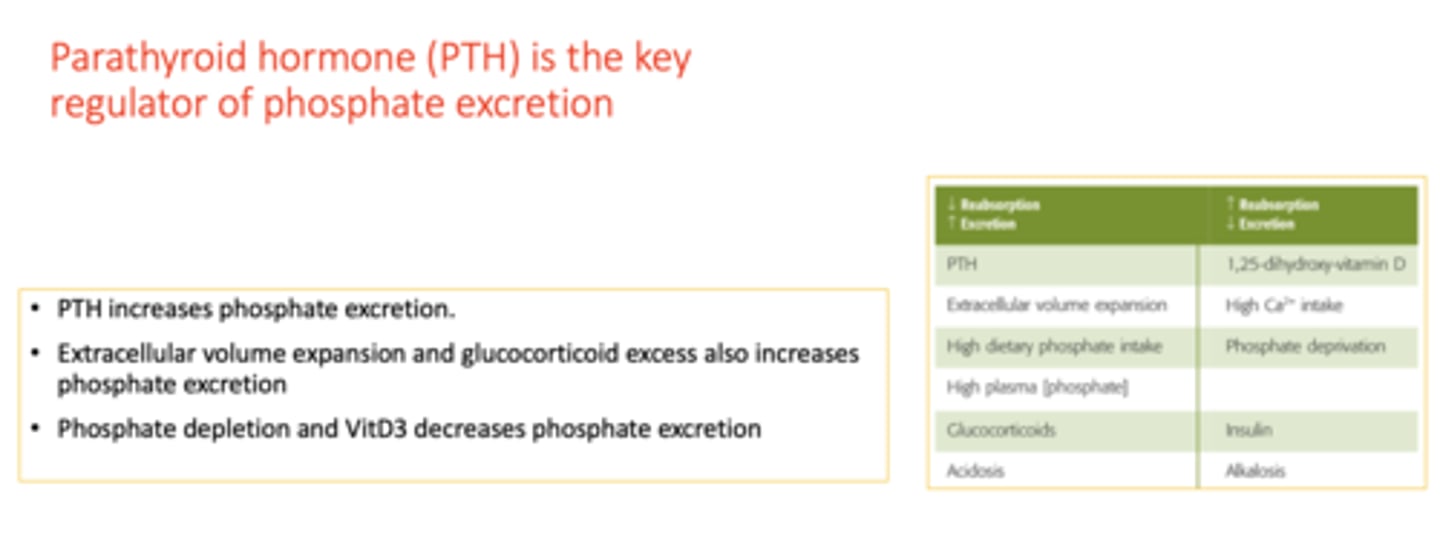
_________ is the key regulator of phosphate excretion
parathyroid hormone
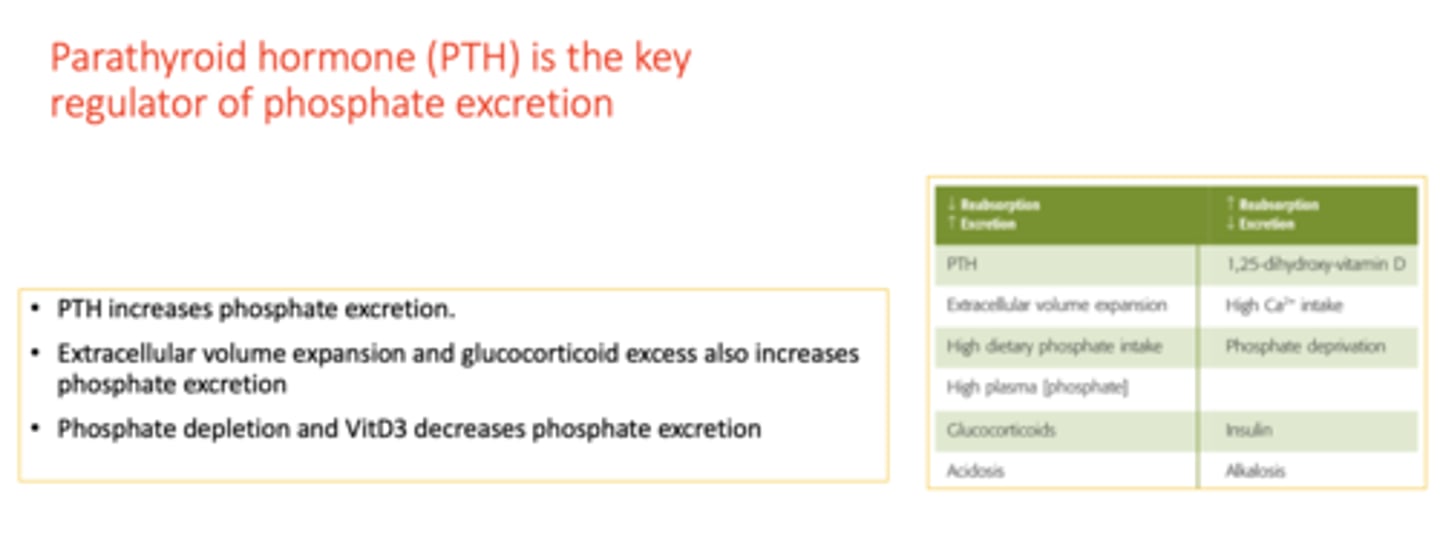
Both PTH and atrial natriuretic peptide (ANP) _______ phosphate excretion.
increase
PTH _______ phosphate reabsorption
Decreases
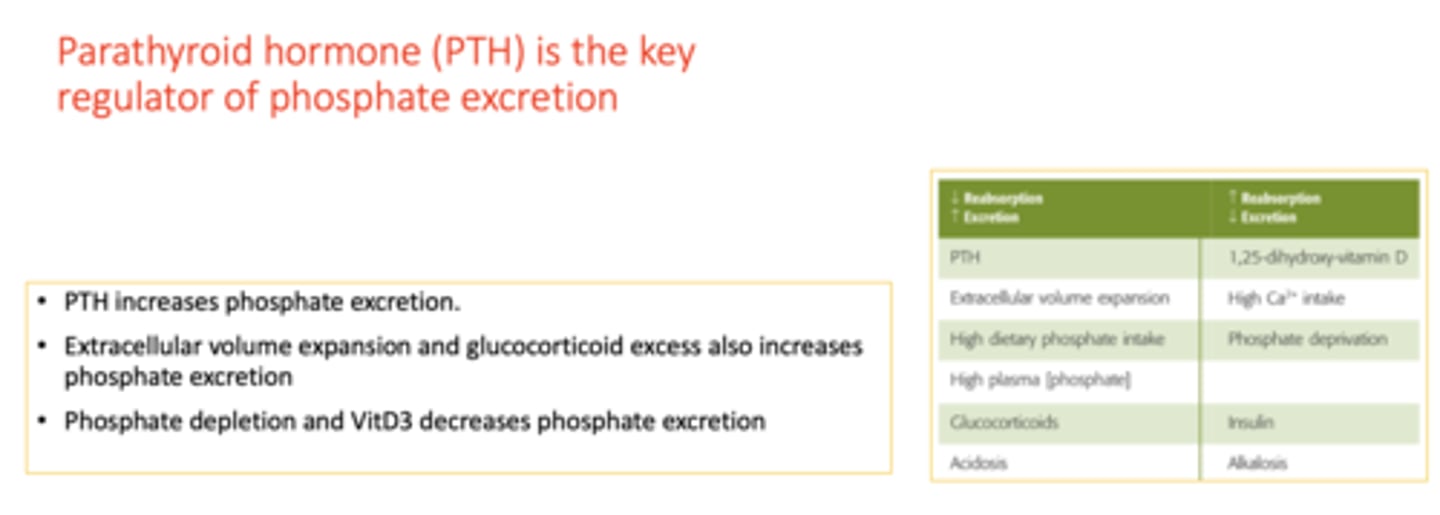
Extracellular volume expansion ________ phosphate excretion
increase
phosphate depletion ________ phosphate excretion
decreases
VitD3 ________ phosphate excretion
decreases
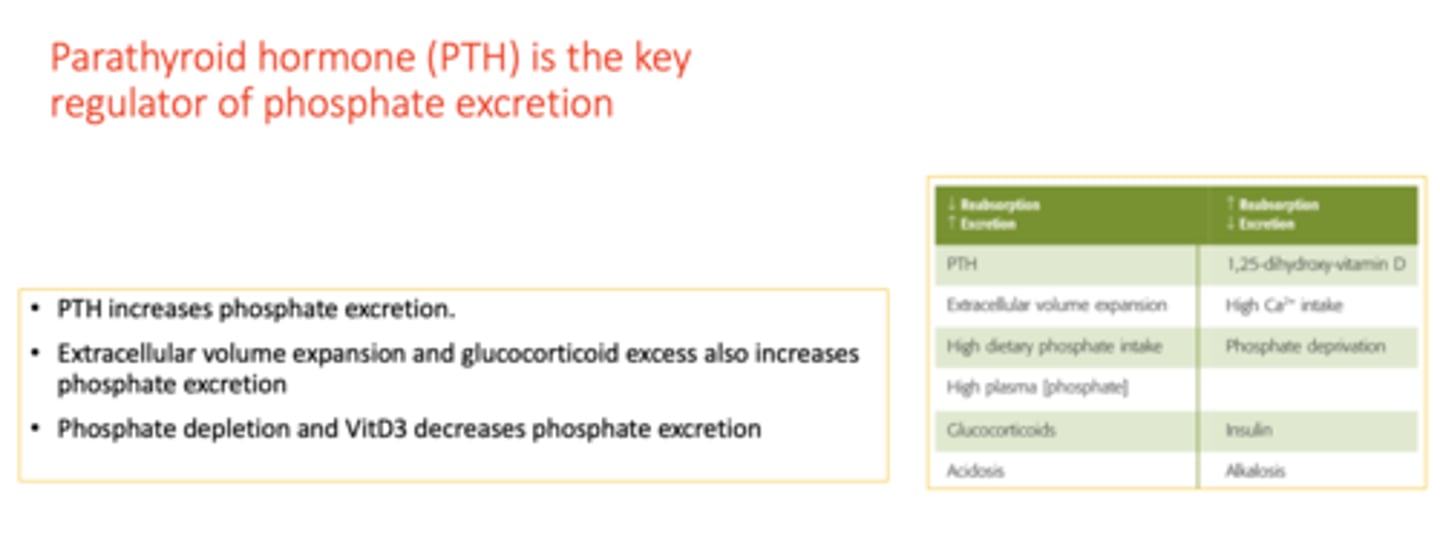
glucocorticoid excess ________ phosphate excretion
increases
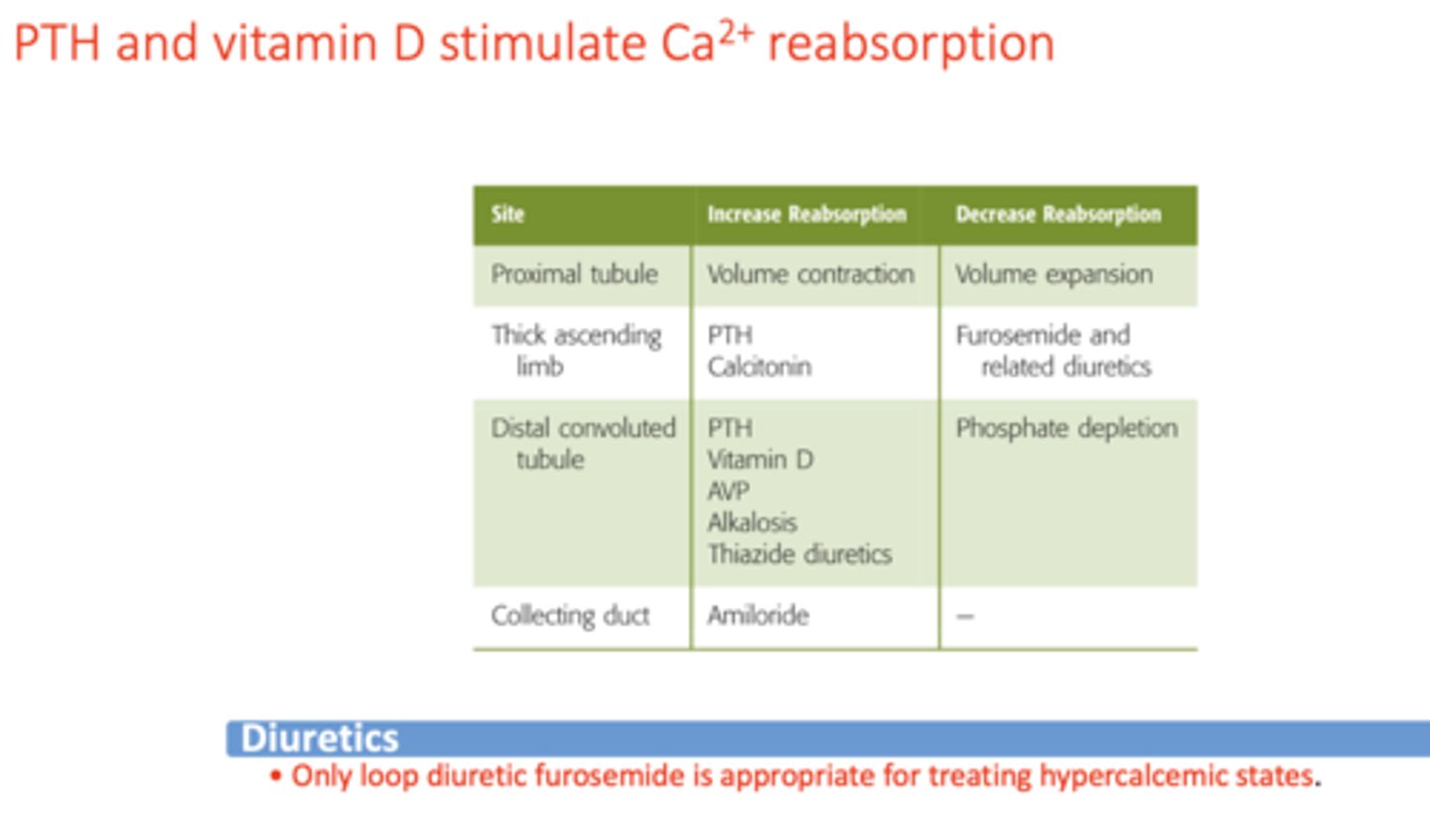
concentration of Ca2+ in plasma is normally ____ to ____
8.8 to 10.6 mg/dL
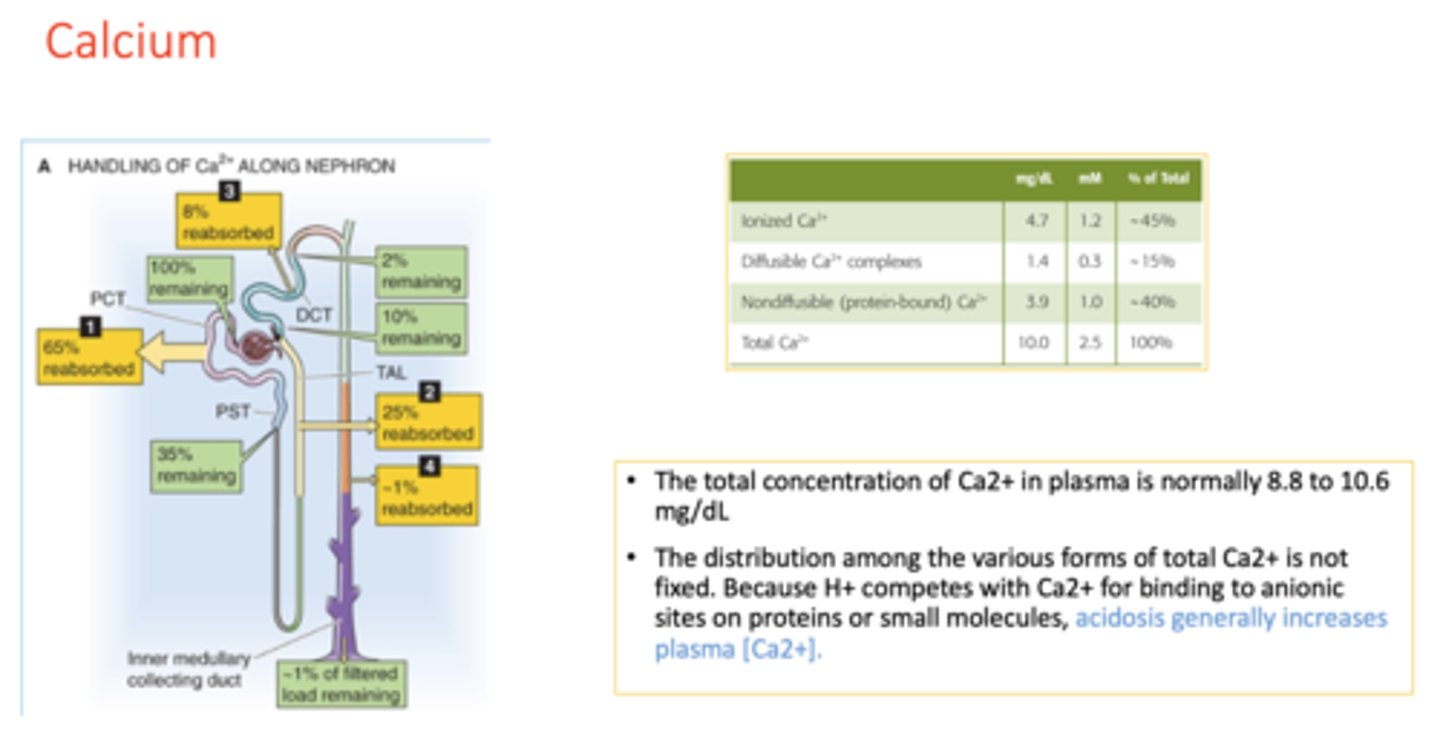
acidosis generally will ________ plasma [Ca2+].
increase
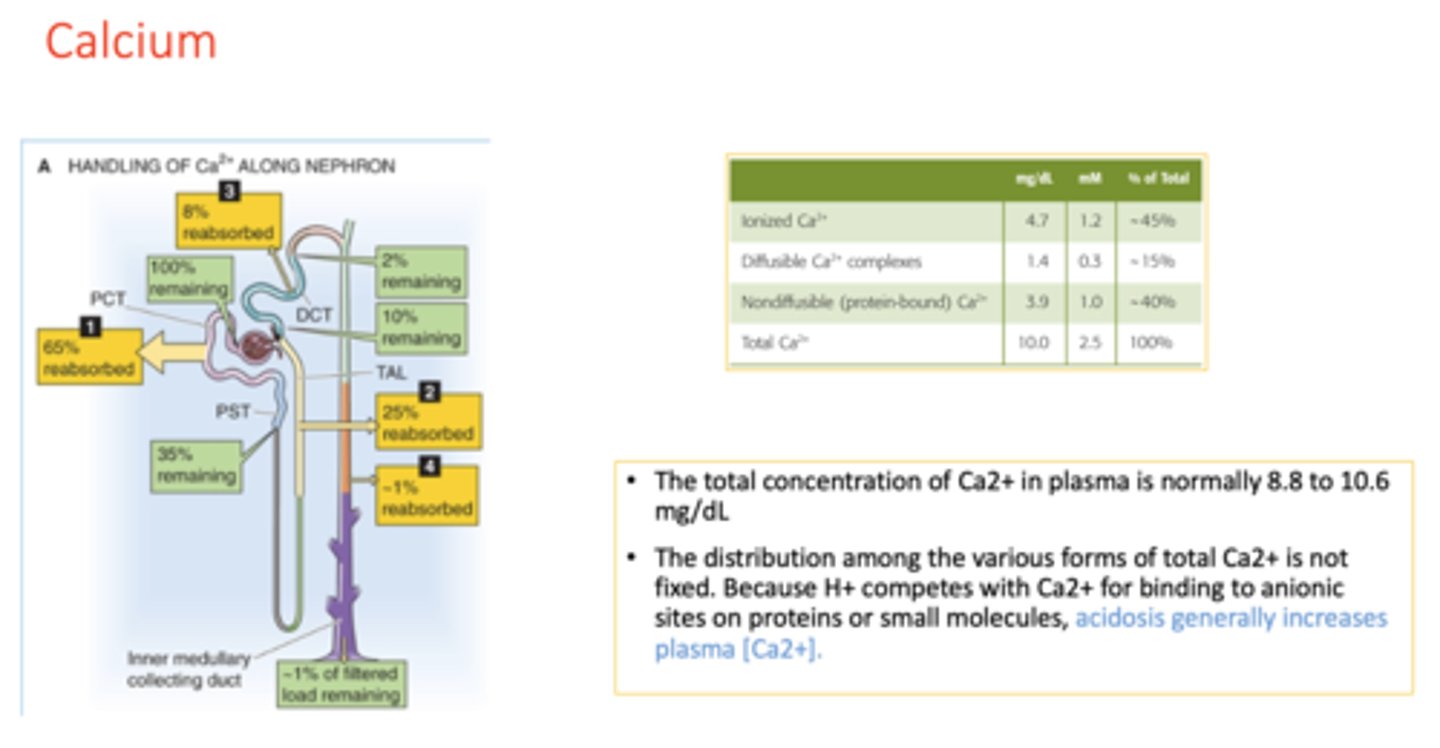
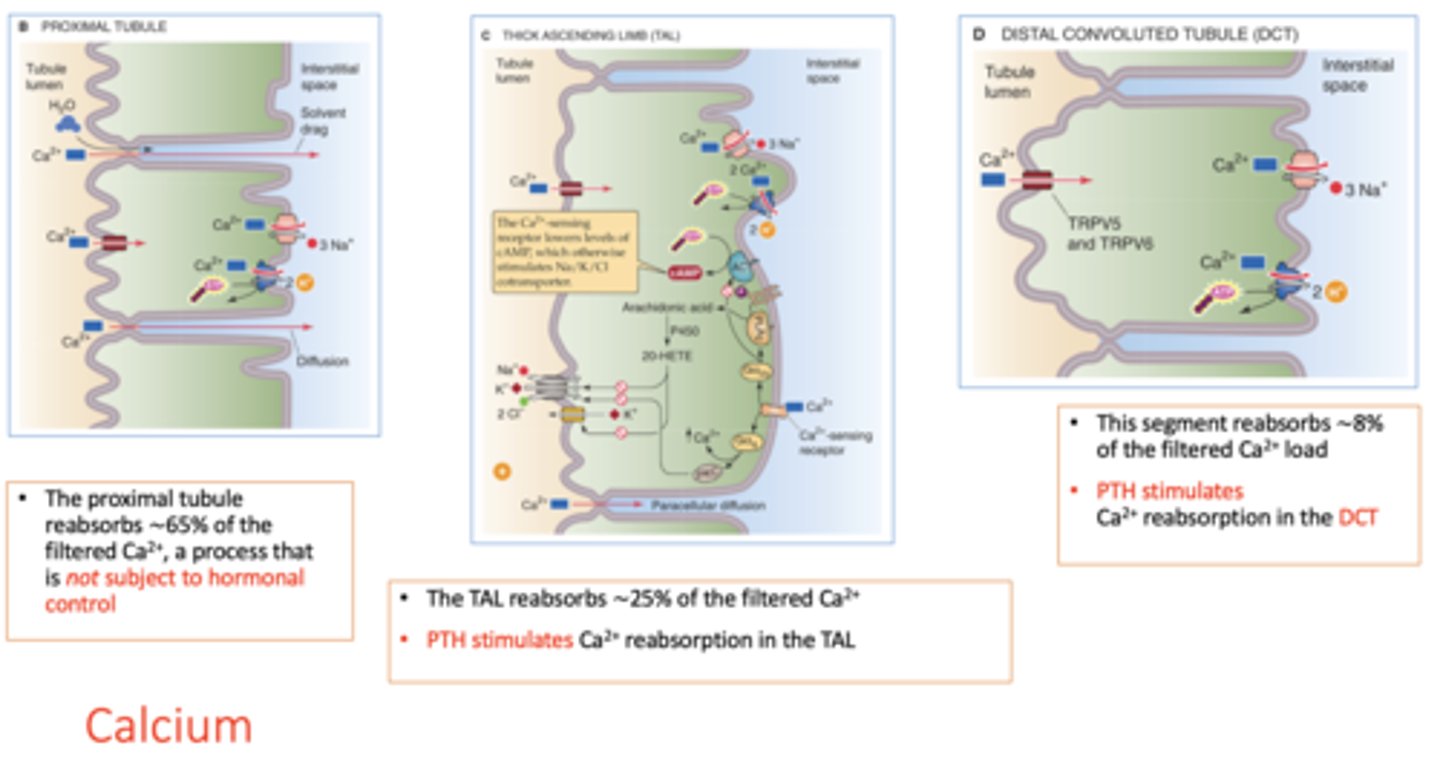
The proximal tubule reabsorbs ∼65% of the filtered Ca2+, a process that is regulated by a ____________
concentration gradient
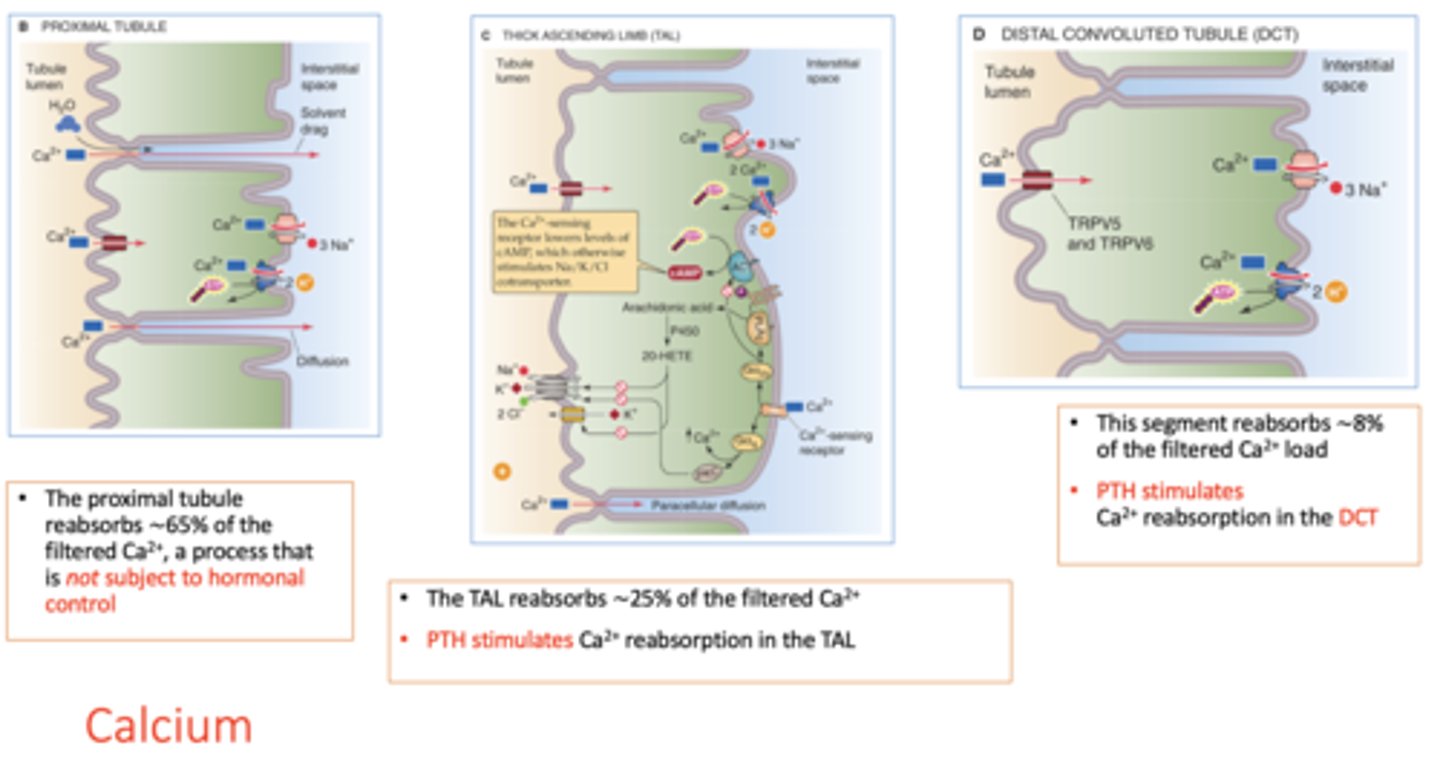
The proximal tubule reabsorbs ∼_____ of the filtered Ca2+
65%
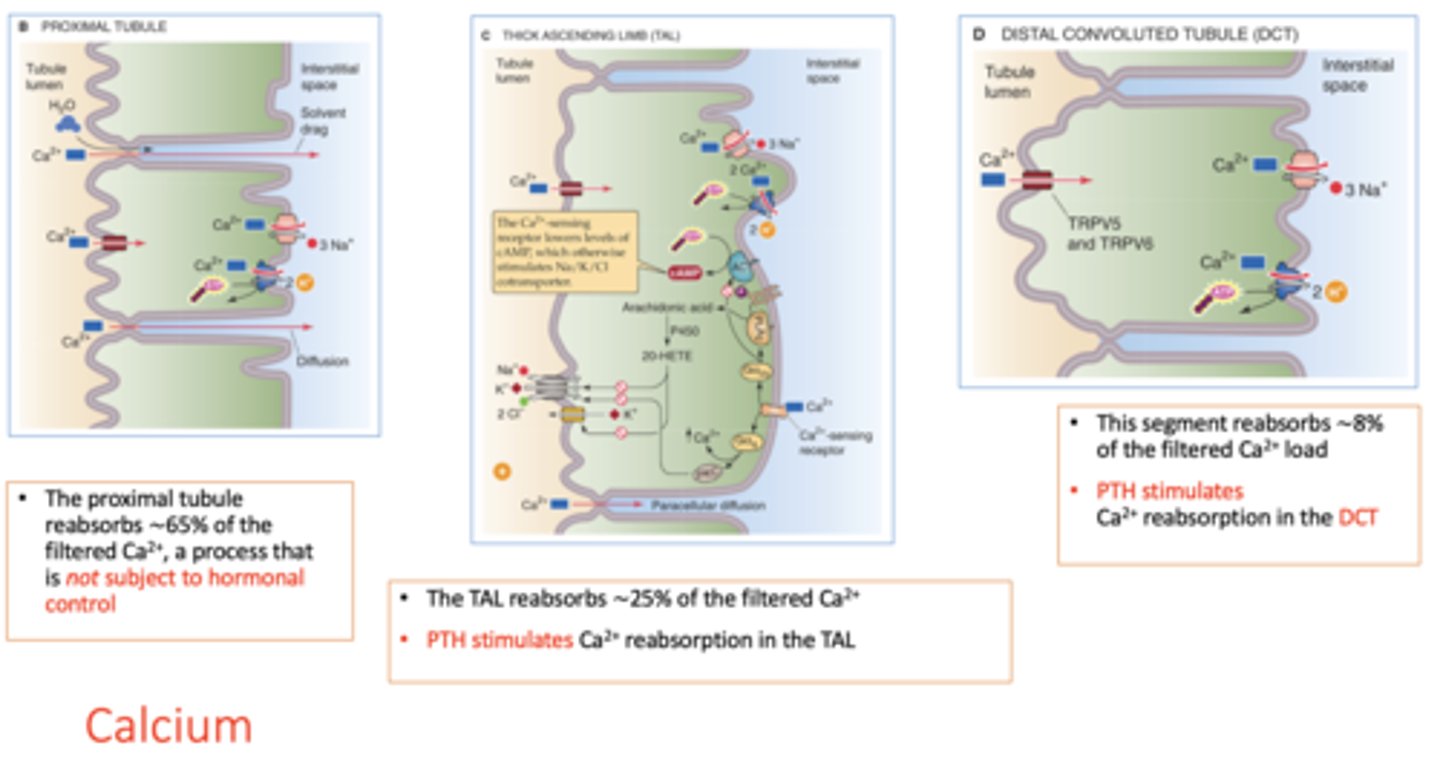
The _____________ reabsorbs ∼65% of the filtered Ca2+, a process that is not subject to hormonal control
proximal tubule
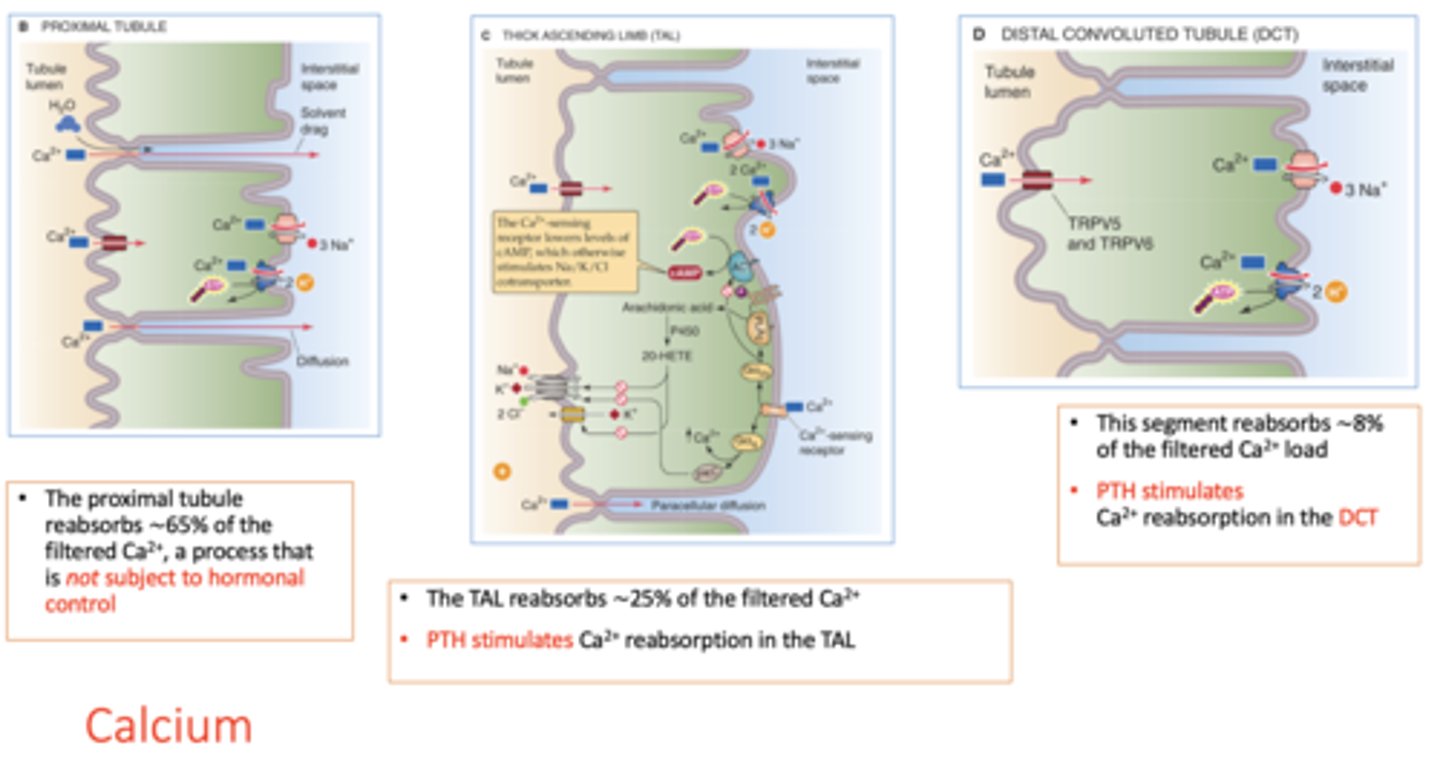
The _______ reabsorbs ∼25% of the filtered Ca2+
thick ascending loop of Henle
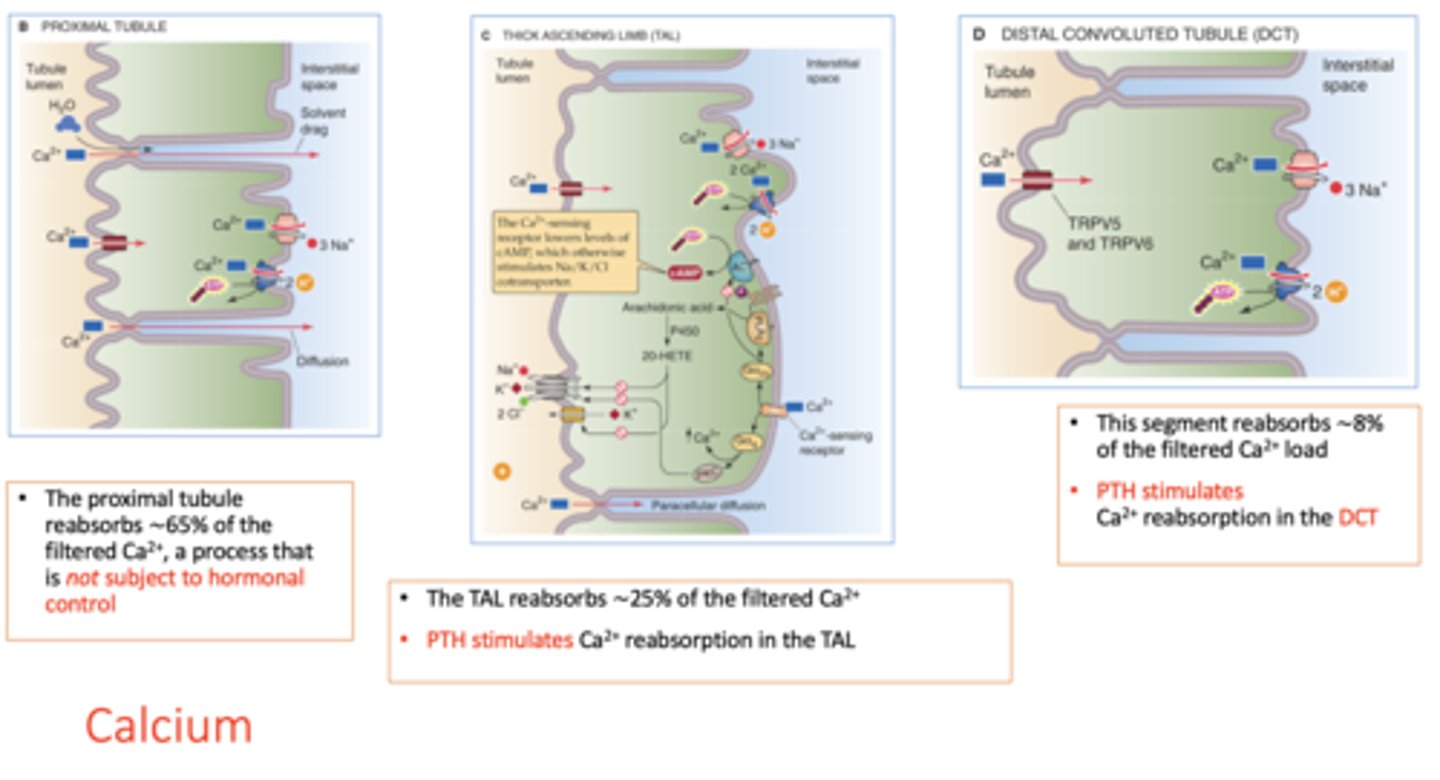
______ stimulates Ca2+ reabsorption in the TAL
PTH
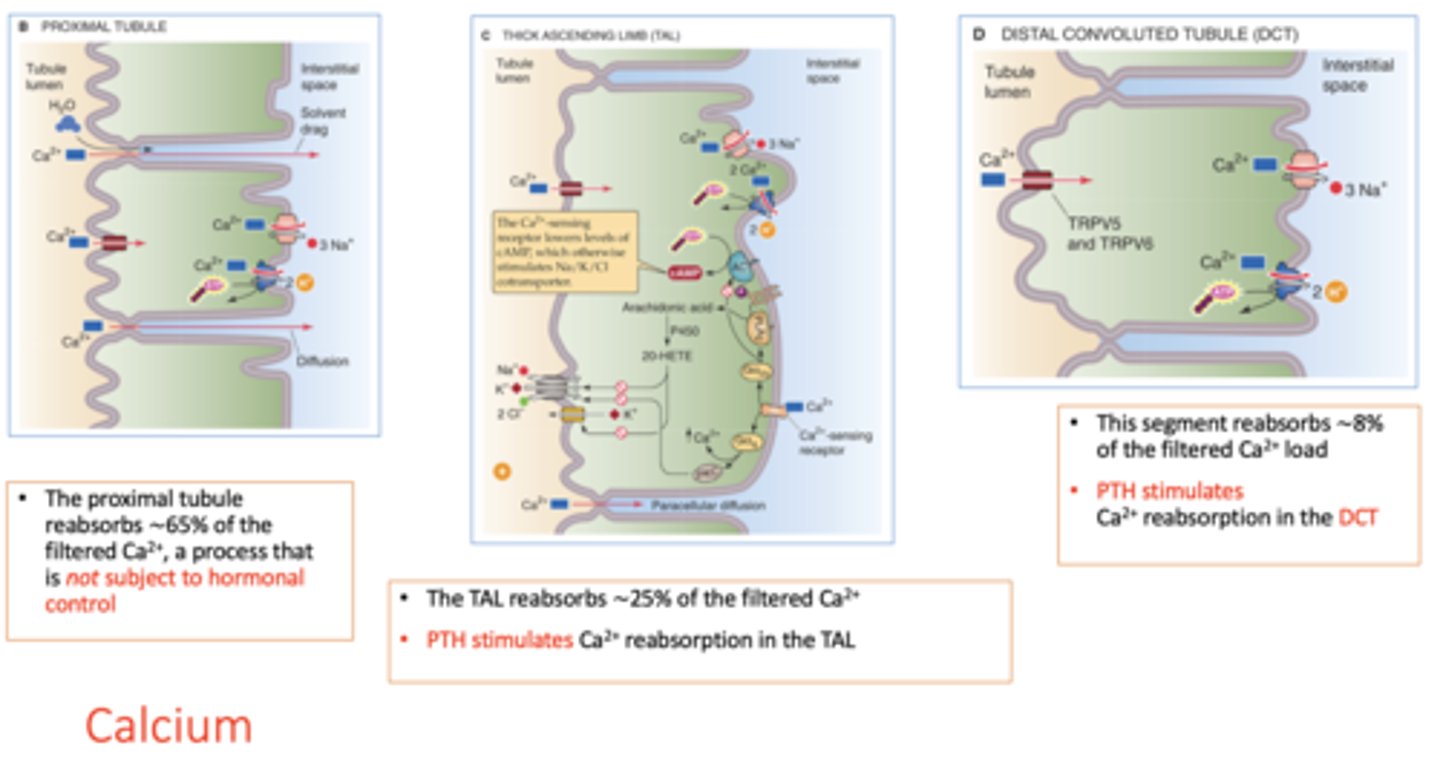
What segment reabsorbs ∼8% of the filtered Ca2+ load?
distal convoluted tubule (DCT)
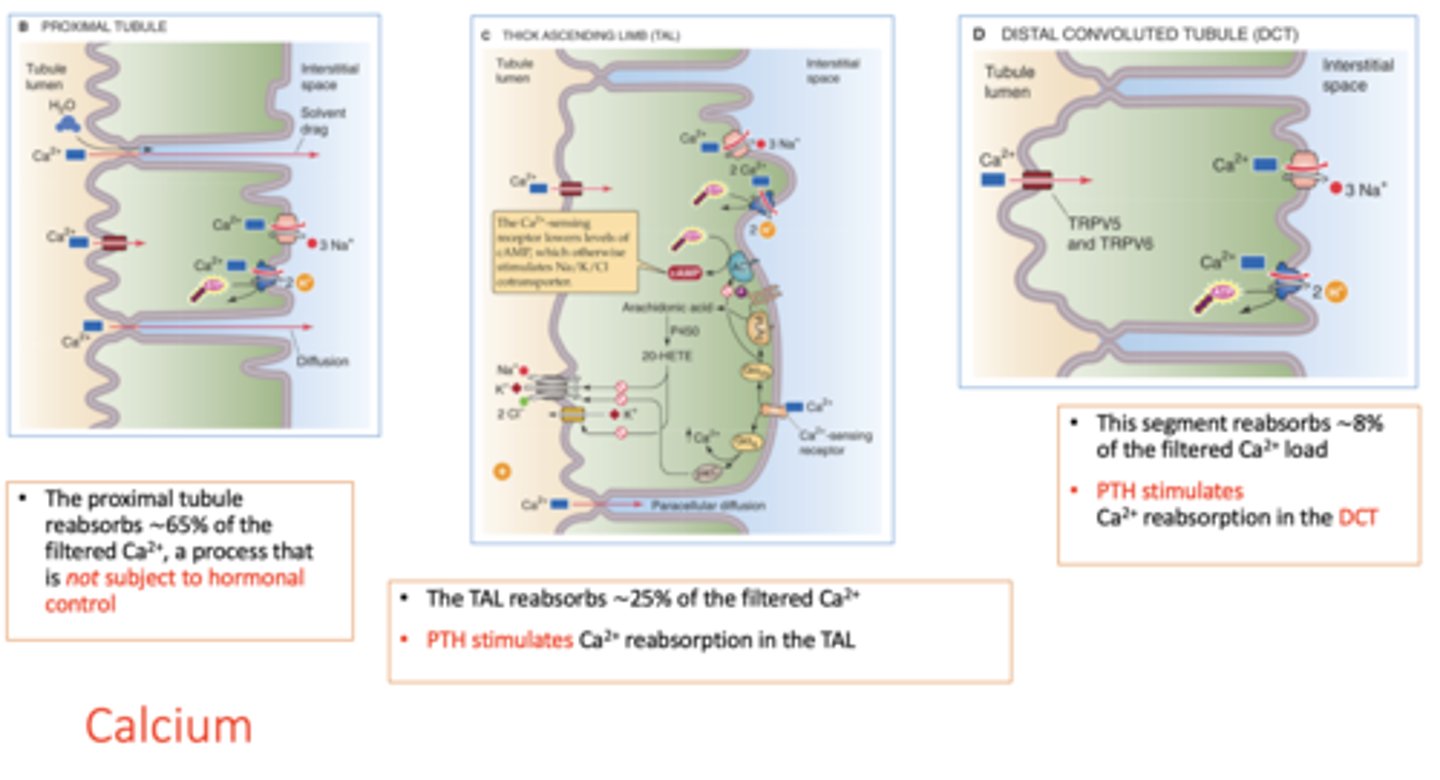
________ stimulates Ca2+ reabsorption in the DCT
PTH
t/f: vitamin D stimulate Ca2+ reabsorption
true
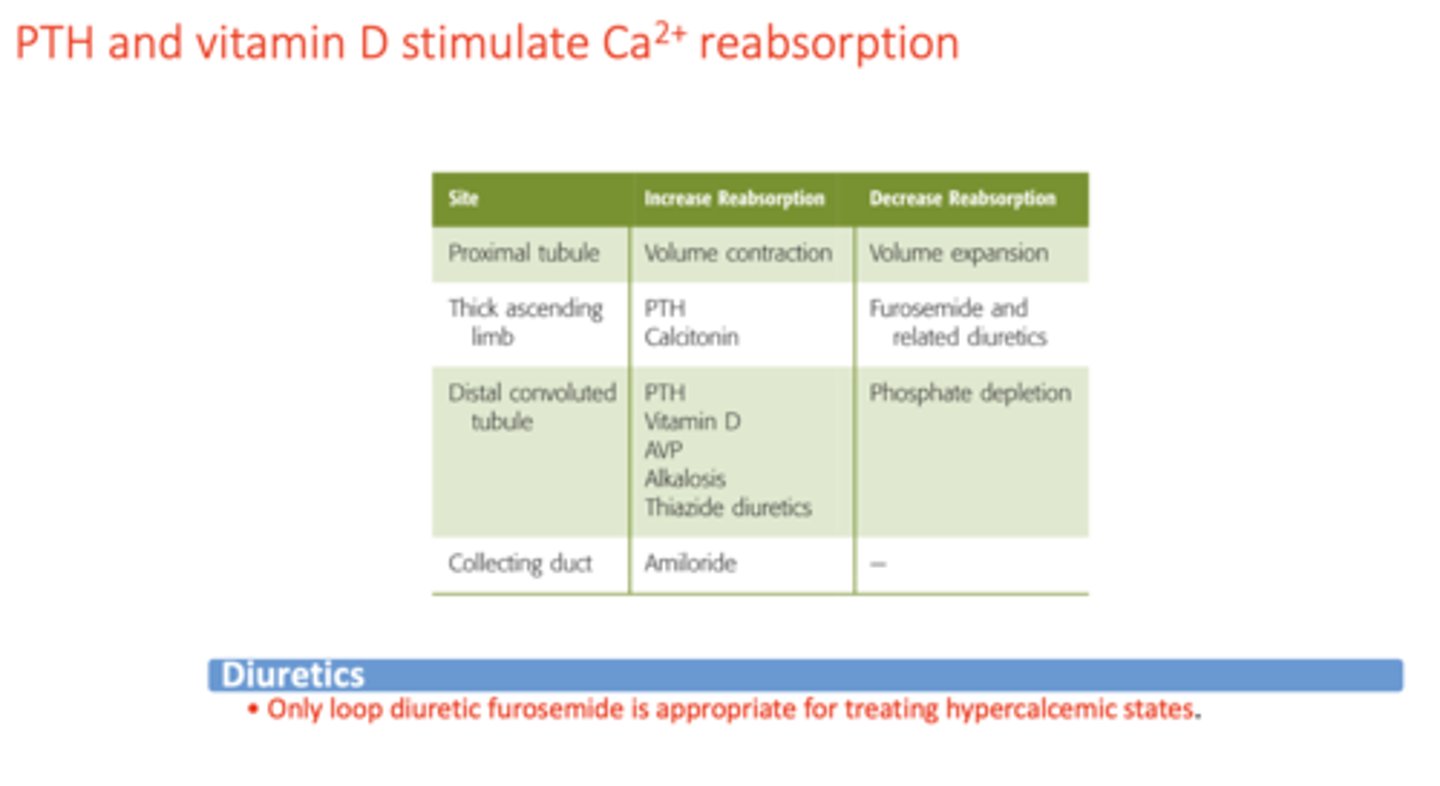
What is the only diuretic appropriate for treating hypercalcemic states?
loop diuretic (i.e. furosemide)
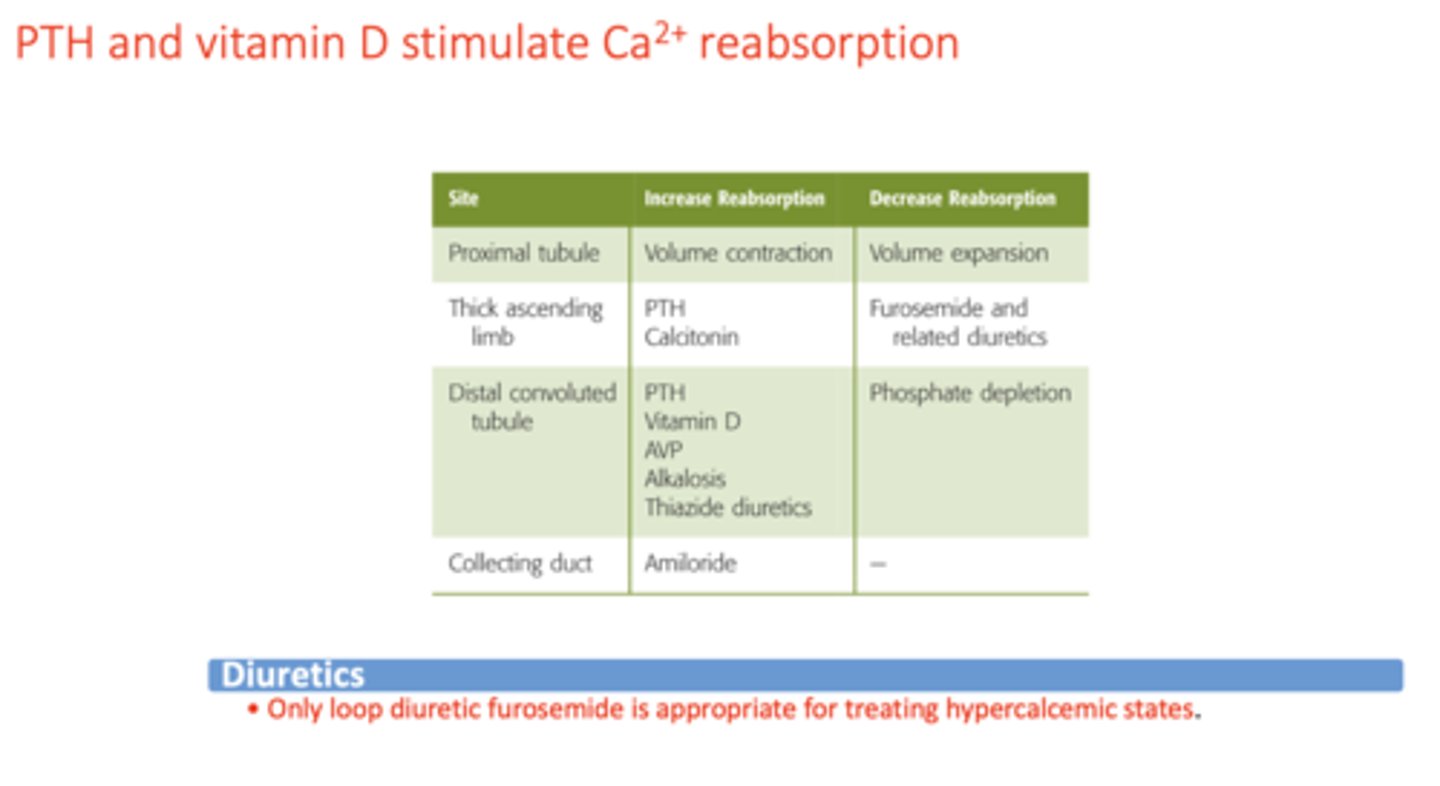
The most important regulator of renal Ca2+ reabsorption is ____
parathyroid hormone
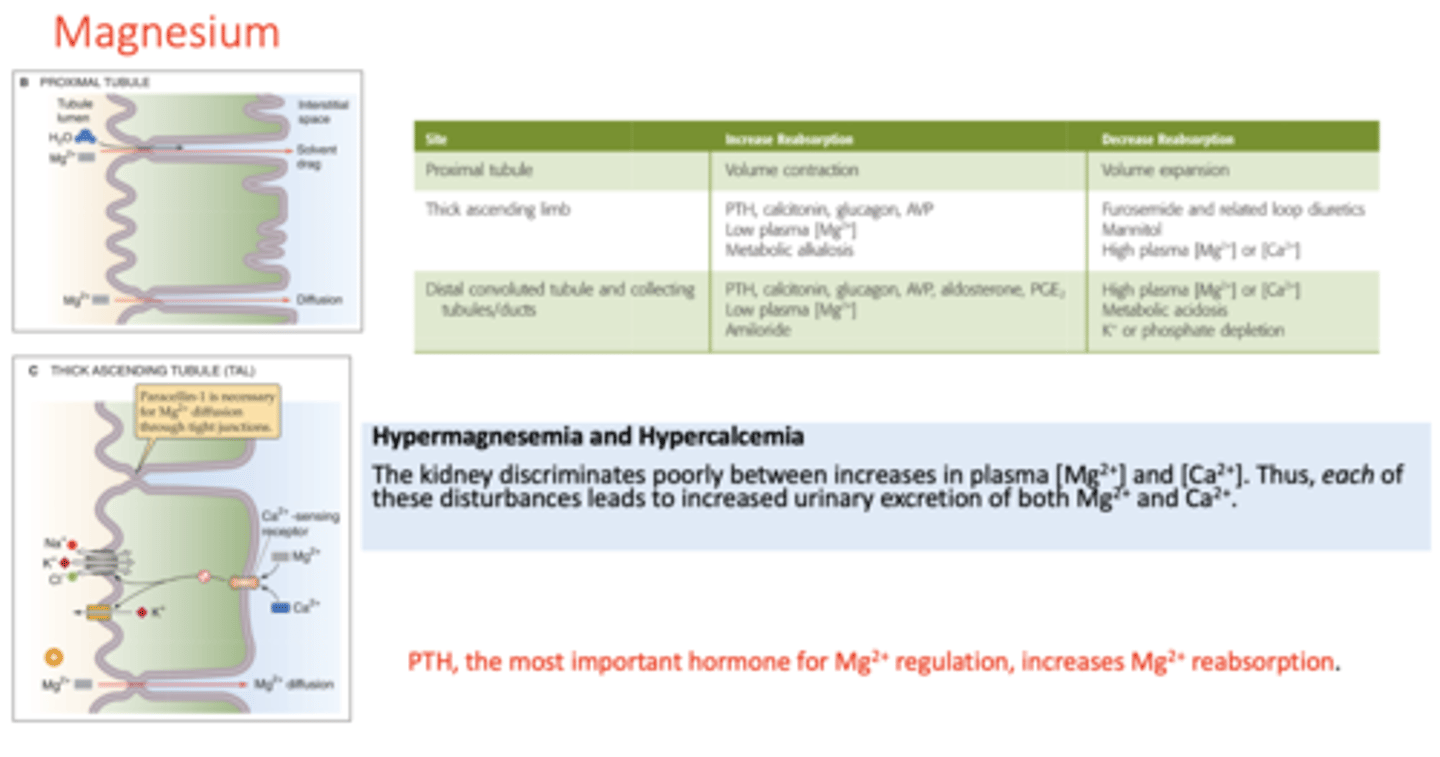
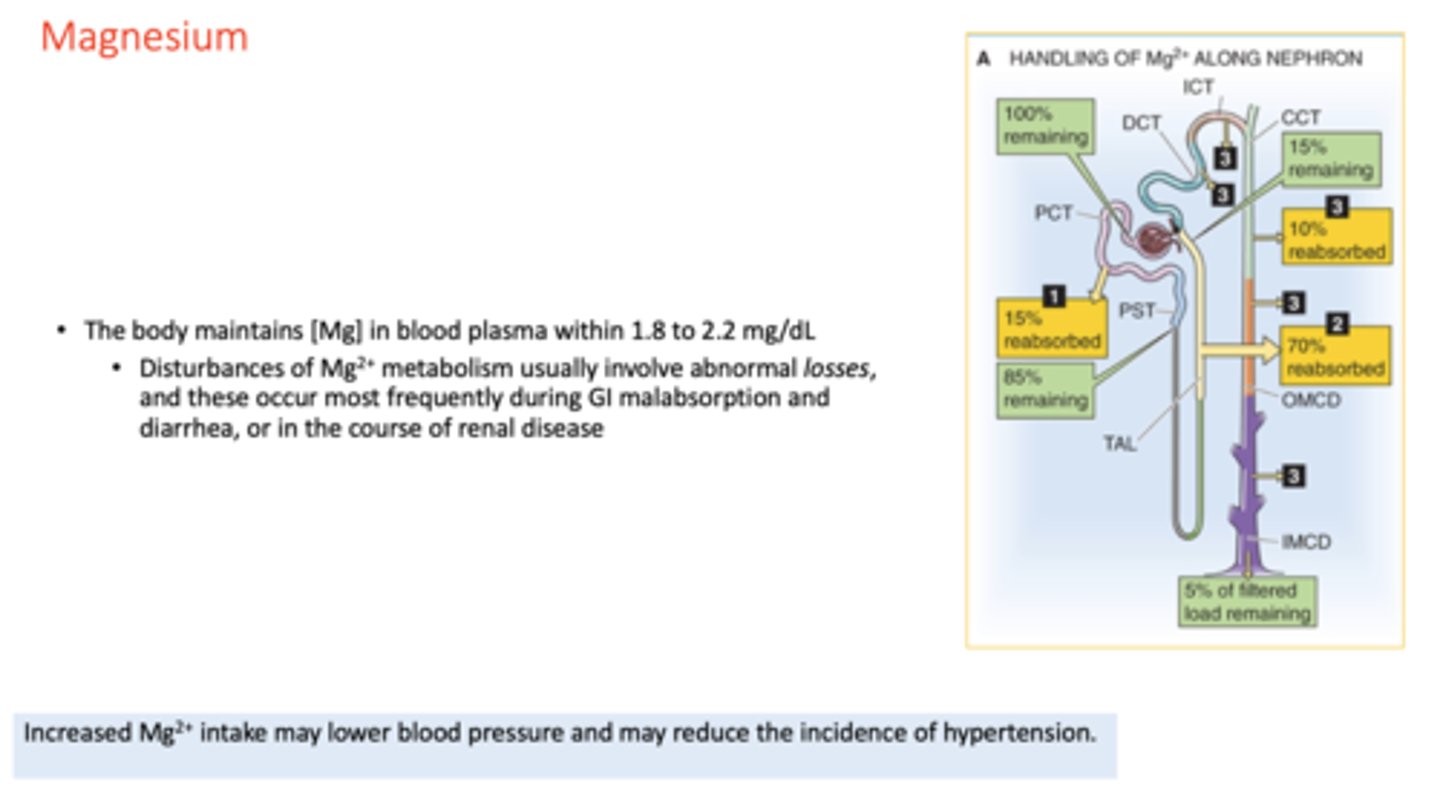
The most important regulator of renal Mg2+ reabsorption is ____
parathyroid hormone
parathyroid hormone increase Ca2+ reabsorption in the _______ (2)
- Thick ascending loop of Henle
- Distal convoluted tubule
Vitamin D increase Ca2+ reabsorption in the _______
distal convoluted tubule (DCT)
Regular body [Mg] in blood plasma is ________ to ________ mg/dL
1.8 to 2.2 mg/dL
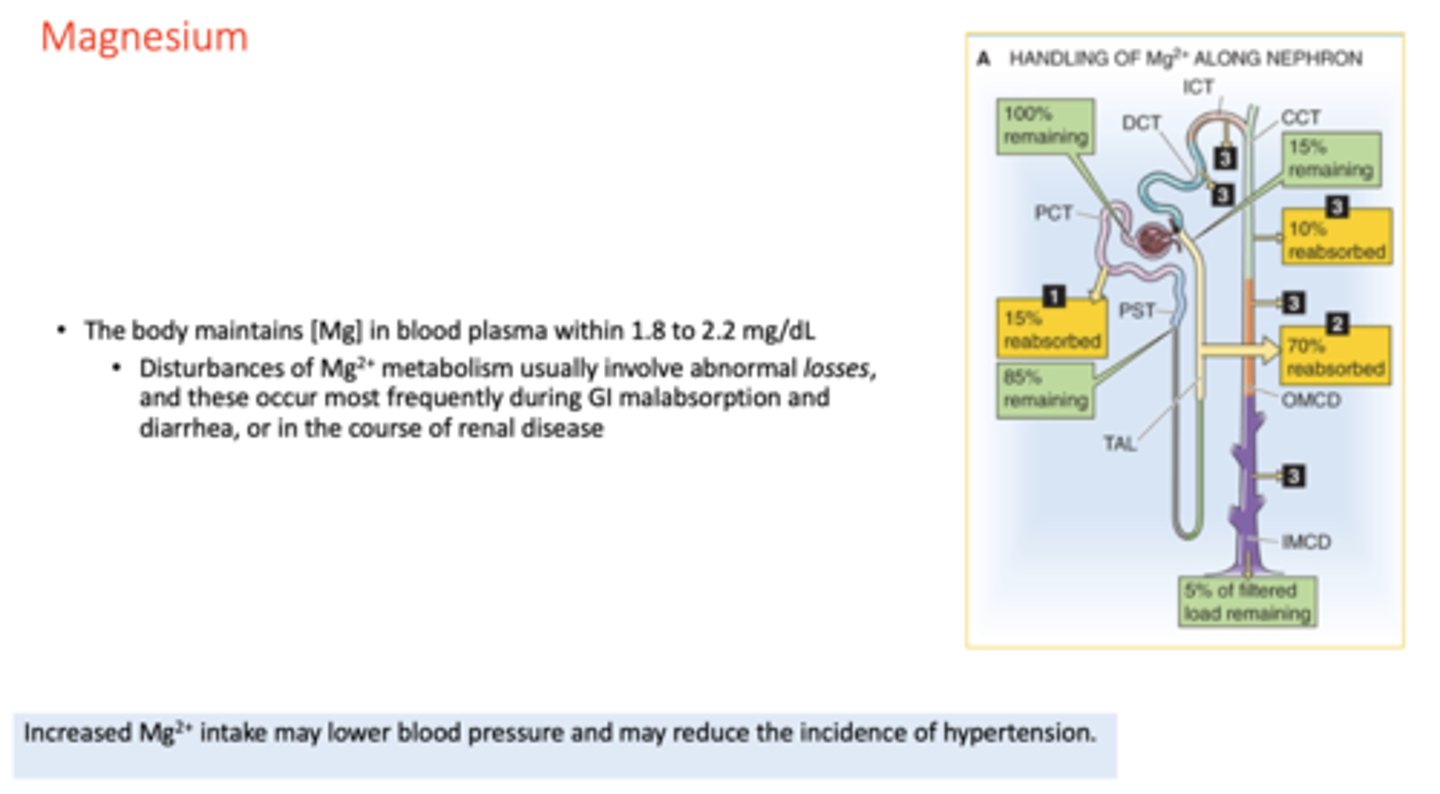
__________ Mg2+ intake may lower blood pressure and may reduce the incidence of hypertension
Increased
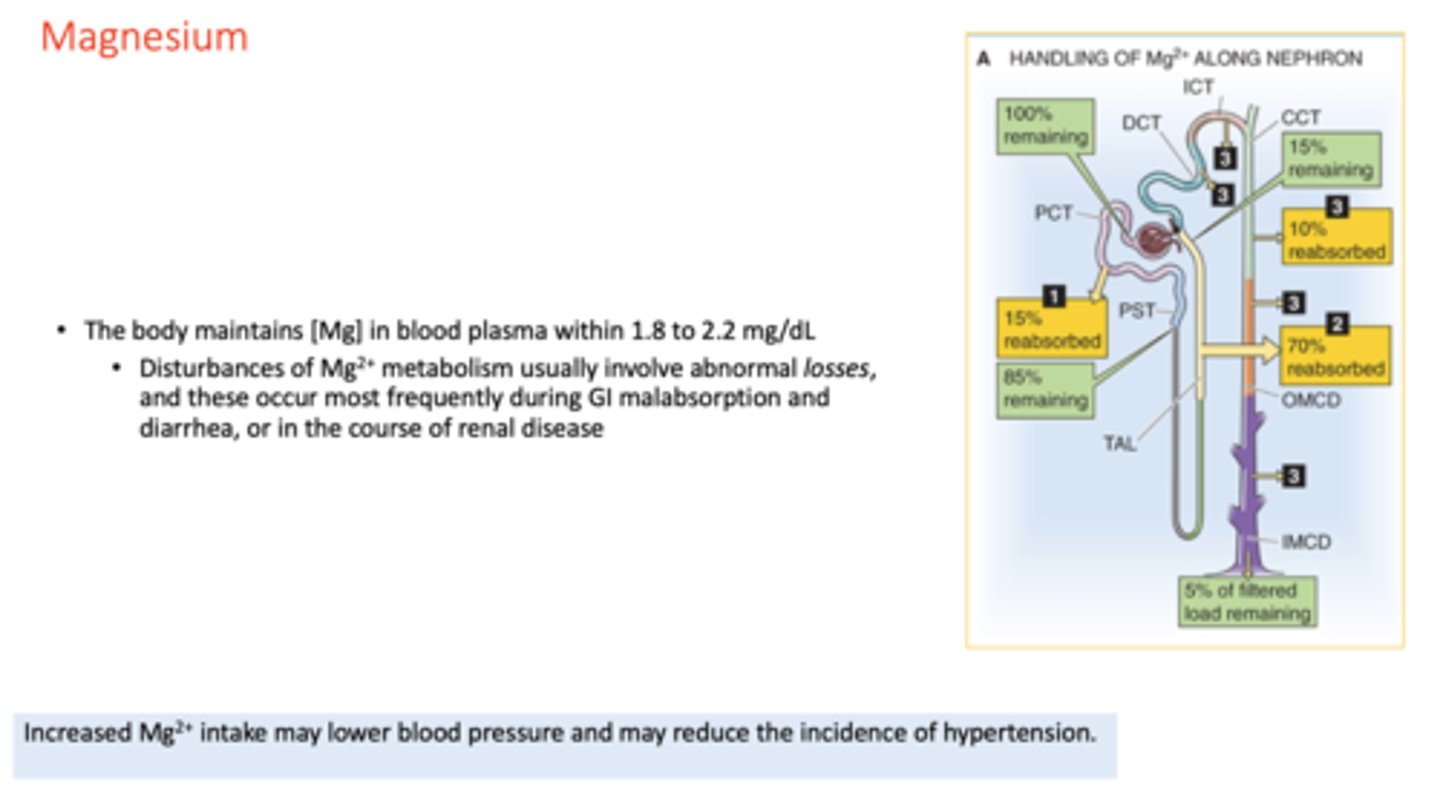
Disturbances of Mg2+ metabolism usually involve abnormal ___________, and these occur most frequently during GI malabsorption and diarrhea, or in the course of renal disease
losses
What conditions are the following:
The kidney discriminates poorly between increases in plasma [Mg2+] and [Ca2+]. Thus, these disturbances leads to increased urinary excretion of both Mg2+ and Ca2+
Hypermagnesemia; Hypercalcemia

the end product of purine catabolism is __________
urate
proteins should not be filtered, but if they escape into filtrate, they will be reabsorbed via ______
clathrin coated endosomes
rate of glucose reabsorption reaches plateau (Tm) at ________. Once Tm is reached, glucose will be excreted into the urine
400mg/min
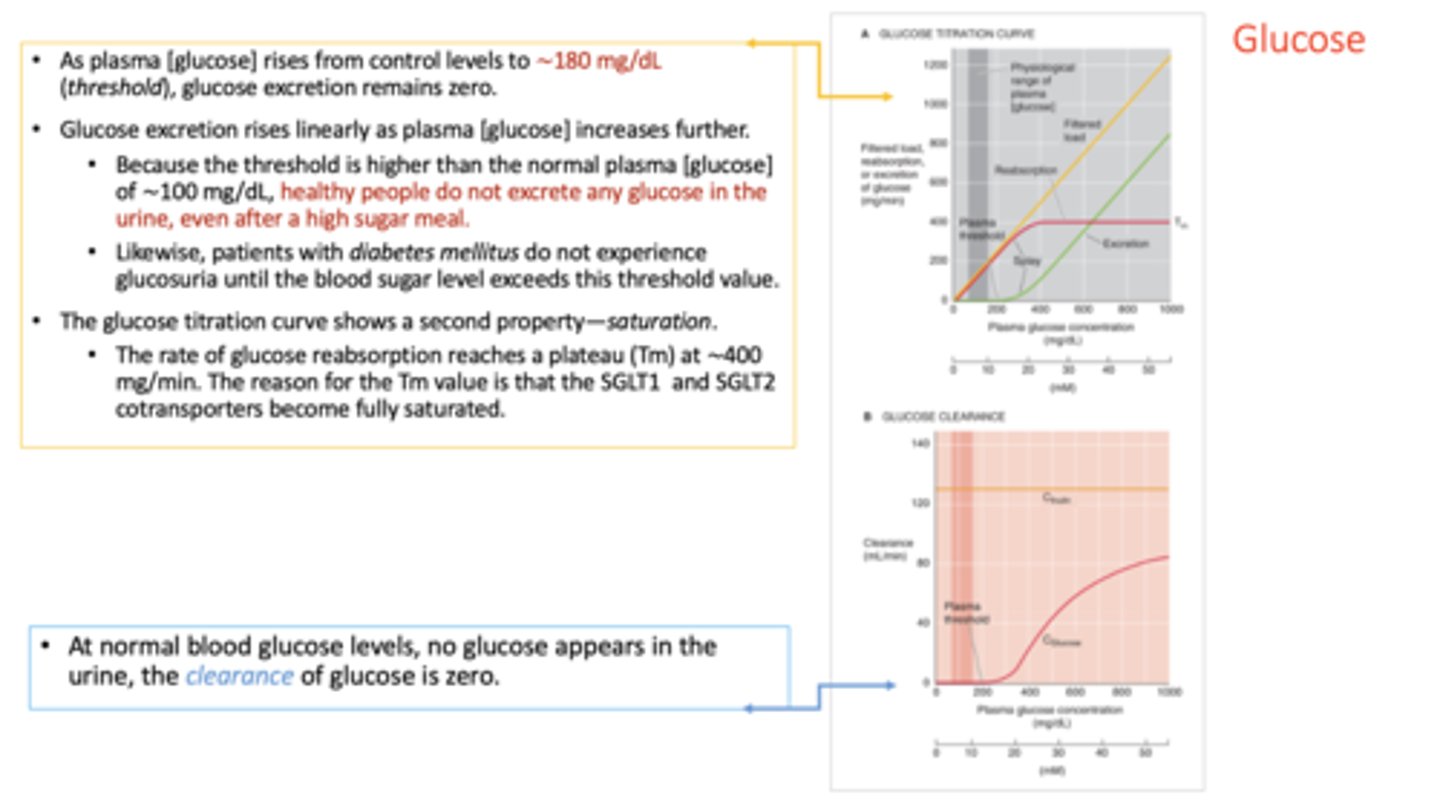
At what Tm value of glucose reabsorption indicates that the SGLT1 and SGLT2 cotransporters are fully saturated?
400 mg/min
Urine flow rate = 1 ml/min
Urine inulin concentration = 100 mg/ml
Plasma inulin concentration = 2 mg/ml
Urine urea concentration = 50 mg/ml
Plasma urea concentration = 2.5 mg/ml
What is the glomerular filtration rate (GFR)?
A) 25ml/min
B) 50 ml/min
C) 100 ml/min
D) 125ml/min
E) None of the above
B) 50 ml/min
Urine flow rate = 1 ml/min
Urine inulin concentration = 100 mg/ml
Plasma inulin concentration = 2 mg/ml
Urine urea concentration = 50 mg/ml
Plasma urea concentration = 2.5 mg/ml
What is the net urea reabsorption rate?
A) 0 mg/min
B) 25 mg/min
C) 50 mg/min
D) 75 mg/min
E) 100 mg/min
D) 75 mg/min
In normal kidneys, which of the following is true of the osmolarity of renal tubular fluid that flows through the early distal tubule in the region of the macula densa?
A) Usually isotonic compared with plasma
B) Usually hypotonic compared with plasma
C) Usually hypertonic compared with plasma
D) Hypertonic, compared with plasma, in antidiuresis
B) Usually hypotonic compared with plasma
After receiving a renal transplant, a patient develops severe hypertension (170/110 mm Hg). A renal arteriogram indicates severe renal artery stenosis in his single remaining kidney, with a reduction in GFR to 25% of normal. Which of the following changes, compared with normal, would be expected in this patient, assuming steady-state conditions?
A) Large increase in plasma sodium concentration
B) Reduction in urinary sodium excretion to 25% of normal
C) Reduction in urinary creatinine excretion to 25% of normal
D) Increase in serum creatinine to about four times normal
E) Normal renal blood flow in the stenotic kidney due to autoregulation
D) Increase in serum creatinine to about four times normal
If a patient has a creatinine clearance of 90 ml/min, a urine flow rate of 1 ml/min, a plasma K+ concentration of 4 mEq/L, and a urine K+ concentration of 60 mEq/L, what is the approximate rate of K+ excretion?
A) 0.06 mEq/min
B) 0.30 mEq/min
C) 0.36 mEq/min
D) 3.6 mEq/min
E) 60 mEq/min
A) 0.06 mEq/min
Which of the following changes would you expect to find after administering a vasodilator drug that caused a 50% decrease in afferent arteriolar resistance and no change in arterial pressure?
A) Decreased renal blood flow, decreased GFR, and decreased peritubular capillary hydrostatic pressure
B) Decreased renal blood flow, decreased GFR, and increased peritubular capillary hydrostatic pressure
C) Increased renal blood flow, increased GFR, and increased peritubular capillary hydrostatic pressure
D) Increased renal blood flow, increased GFR, and no change in peritubular capillary hydrostatic pressure
E) Increased renal blood flow, increased GFR, and decreased peritubular capillary hydrostatic pressure
C) Increased renal blood flow, increased GFR, and increased peritubular capillary hydrostatic pressure
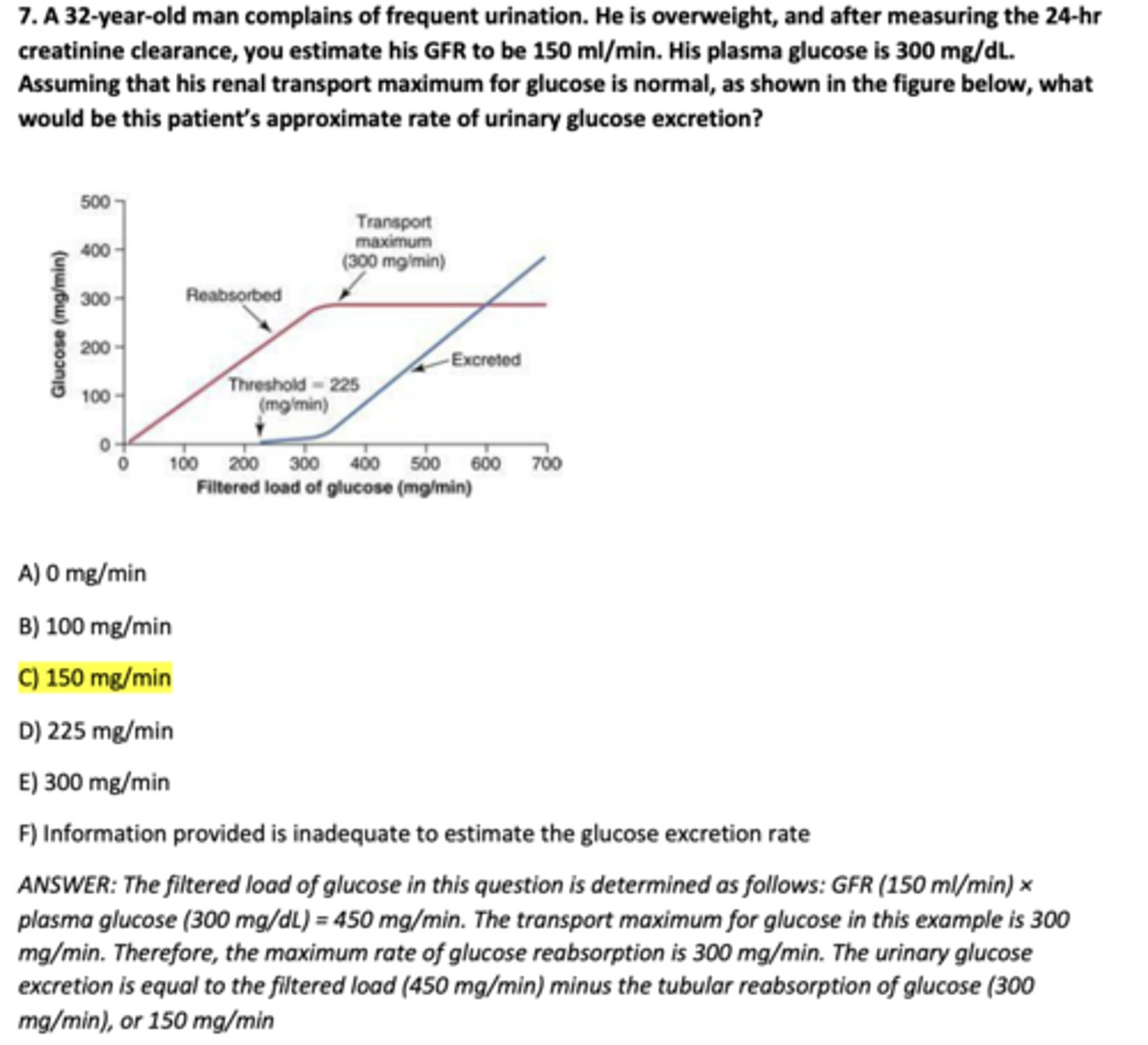
A 32-year-old man complains of frequent urination. He is overweight, and after measuring the 24-hr creatinine clearance, you estimate his GFR to be 150 ml/min. His plasma glucose is 300 mg/dL. Assuming that his renal transport maximum for glucose is normal, as shown in the figure below, what would be this patient's approximate rate of urinary glucose excretion? (Image shows transport maximum is 300 mg/min)
A) 0 mg/min
B) 100 mg/min
C) 150 mg/min
D) 225 mg/min
E) 300 mg/min
F) Information provided is inadequate to estimate the glucose excretion rate
C) 150 mg/min
Which of the following changes tends to increase peritubular capillary fluid reabsorption?
A) Increased blood pressure
B) Decreased filtration fraction
C) Increased efferent arteriolar resistance
D) Decreased angiotensin II
E) Increased renal blood flow
C) Increased efferent arteriolar resistance
Which of the following is filtered most readily by the glomerular capillaries?
A) Albumin in plasma
B) Neutral dextran with a molecular weight of 25 kDa
C) Polycationic dextran with a molecular weight of 25 kDa
D) Polyanionic dextran with a molecular weight of 25 kDa
E) Red blood cells
C) Polycationic dextran with a molecular weight of 25 kDa
Which of the following changes tends to increase GFR?
A) Increased afferent arteriolar resistance
B) Increased glomerular capillary filtration coefficient
C) Increased Bowman's capsule hydrostatic pressure
D) Decreased glomerular capillary hydrostatic pressure
B) Increased glomerular capillary filtration coefficient
The maximum clearance rate possible for a substance that is totally cleared from the plasma is equal to which of the following?
A) GFR
B) Filtered load of that substance
C) Urinary excretion rate of that substance
D) Renal plasma flow
E) Filtration fraction
D) Renal plasma flow
If the average hydrostatic pressure in the glomerular capillaries is 50 mm Hg, the hydrostatic pressure in the Bowman's space is 12 mm Hg, the average colloid osmotic pressure in the glomerular capillaries is 30 mm Hg, and there is no protein in the glomerular ultrafiltrate, what is the net pressure driving glomerular filtration?
A) 8 mm Hg
B) 32 mm Hg
C) 48 mm Hg
D) 60 mm Hg
E) 92 mm Hg
A) 8 mm Hg
Furosemide (Lasix) is a diuretic that also produces natriuresis. Which of the following is an undesirable side effect of furosemide due to its site of action on the renal tubule?
A) Edema
B) Hyperkalemia
C) Hypercalcemia
D) Decreased ability to concentrate the urine
E) Heart failure
D) Decreased ability to concentrate the urine
A previously healthy 12-year-old boy is brought to the Emergency Department with vomiting and severe abdominal cramps after a prolonged period of exercise. Elevated levels of serum creatinine and blood urea nitrogen suggest acute renal failure. Following treatment and recovery, his serum uric acid concentration (0.6 mg/dL) remains consistently below normal. To determine if his low serum uric acid level is related to renal dysfunction, uric acid clearance studies are conducted, and the following data are obtained:
Urine volume = 1 mL/min
Urine uric acid concentration = 36 mg/dL
Which of the following is this patient’s uric acid clearance?
A) 12 mL/min
B) 24 mL/min
C) 60 mL/min
D) 216 mL/min
c. 60 mL/min
An individual is known to be suffering from diabetes mellitus. Recently, he has developed hypertension. His doctor suspects that the patient may be developing renal insufficiency that is leading to a reduced glomerular filtration and, as a result, hypervolemia and hypertension. The doctor wishes to evaluate kidney function by measuring the glomerular filtration rate. She can estimate GFR best by performing a urine clearance study of which of the following substances?
A) Creatinine
B) Para-aminohippuric acid (PAH)
C) Urea
D) Glucose
A) Creatinine
Administration of a thiazide diuretic (e.g., chlorothiazide) would be expected to cause which of the following effects as its primary mechanism of action?
A) Inhibition of NaCl co-transport in the early distal tubules
B) Inhibition of NaCl co-transport in the proximal tubules
C) Inhibition of Na+-2Cl−-K+ co-transport in the loop of Henle
D) Inhibition of Na+-2Cl−-K+ co-transport in the collecting tubules
E) Inhibition of the renal tubular actions of aldosterone
A) Inhibition of NaCl co-transport in the early distal tubules
Which of the following would likely lead to hyponatremia?
A) Excessive antidiuretic hormone secretion
B) Restriction of fluid intake
C) Excess aldosterone secretion
D) Administration of 2 L of 3% sodium chloride solution
E) Administration of 2 L of 0.9% sodium chloride solution
A) Excessive antidiuretic hormone secretion
If a person has a kidney transport maximum for glucose of 350 mg/min, a GFR of 100 ml/min, a plasma glucose of 150 mg/dL, a urine flow rate of 2 ml/min, and no detectable glucose in the urine, what would be the approximate rate of glucose reabsorption, assuming normal kidneys?
A) Glucose reabsorption cannot be estimated from these data
B) 0 mg/min
C) 50 mg/min
D) 150 mg/min
E) 350 mg/min
D) 150 mg/min
A healthy 29-year-old man runs a 10-km race on a hot day and becomes very dehydrated. Assuming that his antidiuretic hormone levels are very high, in which part of the renal tubule is the most water reabsorbed?
A) Proximal tubule
B) Loop of Henle
C) Distal tubule
D) Cortical collecting tubule
E) Medullary collecting duct
A) Proximal tubule
A patient's one remaining kidney has moderate renal artery stenosis that reduces renal artery pressure distal to the stenosis to 85 mm Hg, compared with the normal level of 100 mm Hg. Which of the following is most likely decreased in this patient 2 weeks after the stenosis has occurred, assuming that his diet is unchanged?
A) Efferent arteriolar resistance
B) Afferent arteriolar resistance
C) Renin secretion
D) Sodium reabsorption rate
E) Plasma aldosterone concentration
B) Afferent arteriolar resistance