Unit Three- Venous History and Physical/Pharmacology
1/127
Earn XP
Description and Tags
Unit Three- Venous History and Physical/Pharmacology
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
128 Terms
DVT: Etiology
Virchow’s Triad
Virchow’s Triad (2)
Causes of clot formation within the intact venous system
“Discovered” by Rudolf Virchow in 1856
Virchow's Triad describes the 3 main factors that contribute to thrombosis:
Stasis
Vein wall injury
Hypercoagulability
Why do we do venous testing? (4)
Presence of thrombus
Evaluate valve competence
Vein Mapping
Pre-Op AV Fistula
Presence of thrombus (3)
R/O DVT
R/O SVT
Assess embolism risk
What does SVT stand for
Superficial Thrombophlebitis
ALL HISTORY AND PHYSICAL QUESTIONS RELATED TO DVT/VENOUS STUDIES SHOULD ALL REVOLVE AROUND THESE THREE THINGS!!
1. Stasis
2. Vein wall injury
3. Hypercoagulability
STASIS
Blood that remains stagnant for any period will clot with minimal stimulus
Examples of Stasis (4)
Immobilization
Obstruction/Extrinsic Compression
Previous DVT History
CHF
Stasis
Slowed Blood Flow
Hypercoagulability
Increased Clotting Tendency
Vein Wall Injury
Damage to Blood Vessel Lining
Immobilization (6)
Surgery
Acute Stroke
Bedrest
Obesity
Paraplegic
Etc.
Obstruction/Extrinsic Compression (7)
Tumors
Late Trimester Pregnancy
Hematomas
Trauma
Paget-Schroetter Syndrome
May-Thurner Syndrome
Nutcracker Syndrome
PAGET-SCHROTTER DISEASE:
Effort Thrombosis
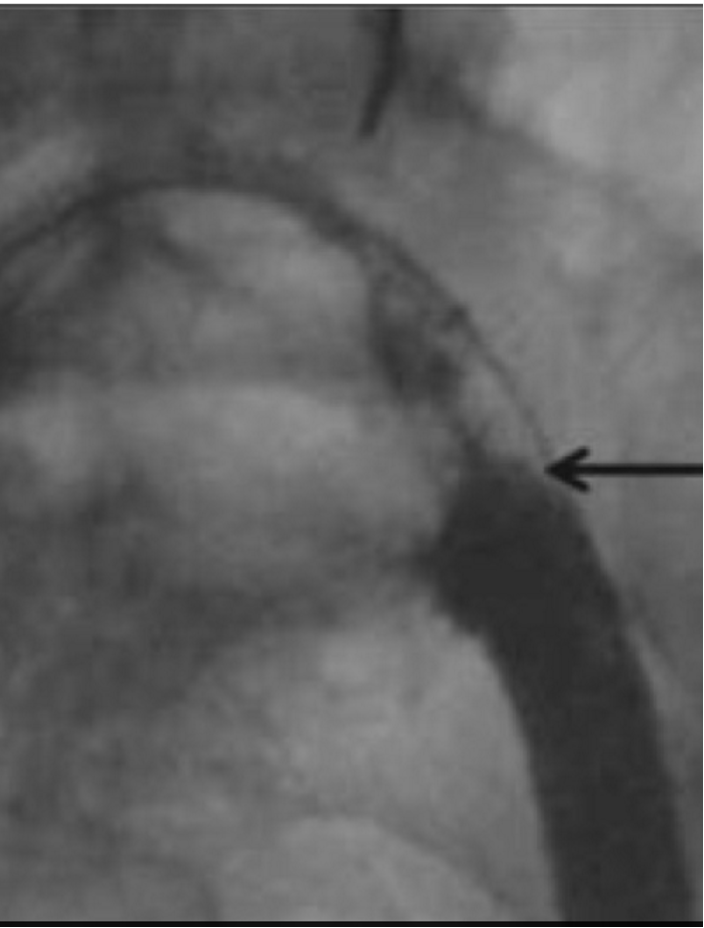
Effort Thrombosis Causes DVT Where?
Subclavian Vein
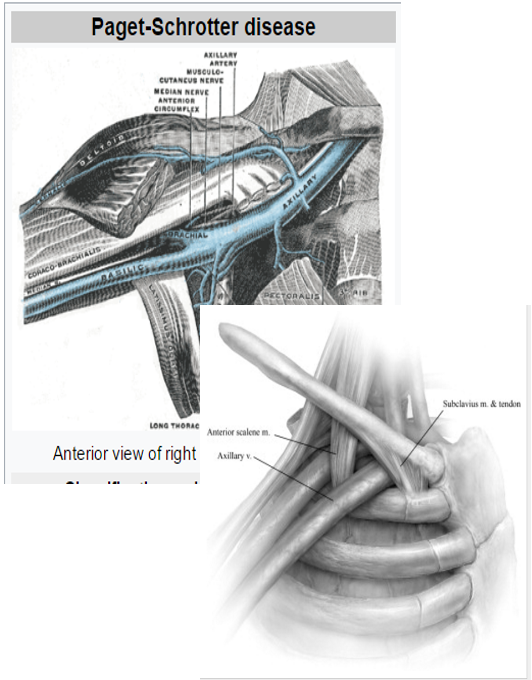
Paget-Schrotter Disease (4)
Blood clot occurring in the Subclavian Vein under the Collarbone
Extrinsic compression of the vein
Annual Incidence: 1 and 2 out of 100,000
Continuous flow would be demonstrated distally
Effort Thrombosis: Extrinsic compression of the vein
Aching, numbness, or tiredness with positional changes of the shoulder
MAY-THURNER SYNDROME:
Iliac Vein Compression Syndrome
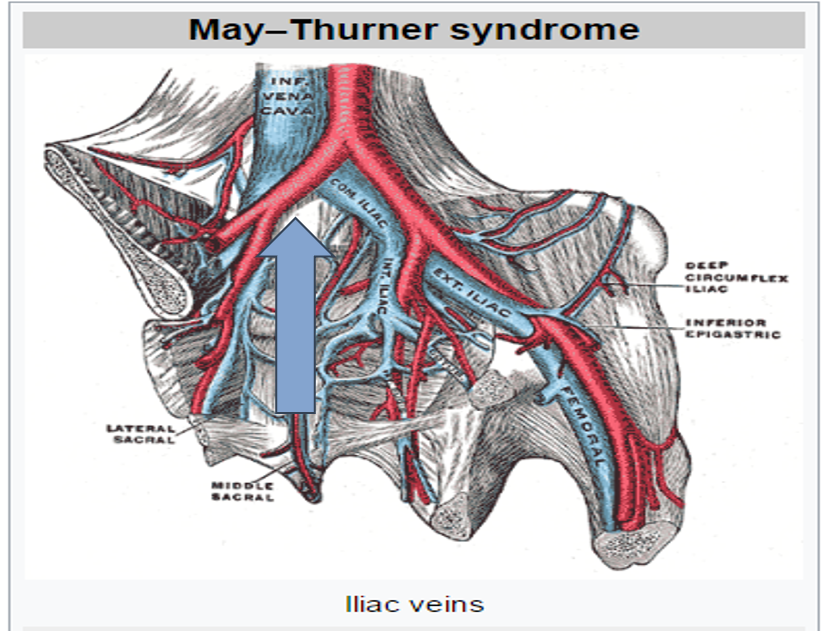
Iliac Vein Compression Syndrome (3)
The left Iliac Vein is compressed by the Right Common Iliac Artery
Increased risk of endothelial injury to Iliac Vein
Undetected until pathology is present
MTS
May-Thurner Syndrome
MTS: (2)
*Endovenous stenting to treat MTS
*Early thrombus removal would be beneficial in reducing the development of post thrombotic syndrome
VEIN WALL INJURY (3)
Normal Venous Endothelium
Luminal surface of these cells contain various substances in their membrane to prevent adhesion of platelets and clotting factors
Mild to moderate injury can alter this
Normal Venous Endothelium
Intact single layer of non-thrombogenic cells
VEIN WALL INJURY DUE TO: (5)
Indwelling catheters (most common in upper extremity)
Venography
Stretching or twisting injuries
Blunt trauma
Chemical injury
HYPERCOAGUABILITY
Increase in clotting factors and platelets/Condition that causes blood to clot more easily
HYPERCOAGUABILITY: Causes (2)
Congenital
Acquired
Congenital (5)
Decreased antithrombin III
Protein C Deficiency
Protein S Deficiency
Disorders of plasminogen and plasminogen activator
Factor V Leiden
Acquired (7)
Carcinoma (Cancer)
Estrogen Replacements
Oral Contraceptives
Pregnancy and Postpartum
Liver Disease
Smoking
Nephrotic Syndrome
Once Thrombus Has Formed… (3)
Stabilize
Propagate
Embolize
STABILIZE
Adhere to wall without changing location or propagating
PROPAGATE
Growth in size and location
EMBOLIZE
A portion breaks free and travels elsewhere within vascular system
Signs and Symptoms of Acute DVT: (3)
Non-specific symptoms
Symptoms are NOT reliable (<50% chance)
ASYMPTOMATIC!!
Symptoms are NOT reliable (<50% chance)
Pain, Swelling, Erythema
ASYMPTOMATIC
Due to the CAPACITANCE of the venous system and its ability to form collaterals around obstruction
Acute DVT: Pain and Tenderness (3) (most common)
Most common symptom
Ranges from mild to severe
Does NOT necessarily correlate with size of the thrombus
Acute DVT: Swelling (4)
Caused by obstruction of venous circulation
Due to an increase in venous volume and pressure
Ranges from mild to severe
Dependent on collateral circulation and size/extent of clot
Acute DVT: Distended Superficial Veins (3)
Veins respond as collaterals and dilate in presence of significant DVT
Commonly seen across the pelvis with Iliofemoral DVT
Upper extremity in anterior shoulder region with proximal Subclavian DVT
CRITICAL ACUTE DVT: (2)
Phlegmasia Cerulea Dolens
Phlegmasia Alba Dolens
Phlegmasia Cerulea Dolens
Cyanosis (blue)
Phlegmasia Alba Dolens
Pallor (white)
PHLEGMASIA CERULEA DOLENS (5)
Extensive lower extremity DVT
Severe pain, swelling, cyanosis, and decreased limb temperature
“Blue Leg”
Arterial perfusion is also compromised
May lead to VENOUS GANGRENE
Extensive lower extremity DVT
Deep and Superficial System
PHLEGMASIA ALBA DOLENS (4)
Acute Iliofemoral Deep Vein Thrombosis
Painful, swollen white leg
“Milk Leg”
Superficial Veins are still patent (deep system involved only)
Acute Iliofemoral Deep Vein Thrombosis; More common in which leg and why?
Left leg
Because of May-Thurner Anatomical Position
ACUTE DEEP VEIN THROMBOSIS: Complication
PULMONARY EMBOLISM/EMBOLUS (PE)
PULMONARY EMBOLISM/EMBOLUS (PE) (3)
Complication from DVT
Obstruction of pulmonary circulation from emboli
Sudden onset
SIGNS AND SYMPTOMS OF PE: (7)
Dyspnea
Pleuritic chest pain
Tachypnea
Tachycardia
Hemoptysis
Right Side Heart Failure
Respiratory Arrest → Cardiac Arrest
Dyspnea
Hard time breathing
Pleuritic chest pain
Chest pain in that area of your lungs
Tachypnea
Breathing really quickly
Tachycardia
Really fast heart rate
Hemoptysis
Coughing up blood
SVT Which vessels would this affect?! (Upper Extremity)
Superficial Vessels; Basilic and Cephalic
SVT Which vessels would this affect?! (Lower Extremity)
Superficial Vessels; Greater Saphenous Vein (GSV), Smaller Saphenous Vein (SSV) and Accessory Veins.
SVT (3)
Local Erythema
Local Inflammation
Palpable Subcutaneous Cord
Local Erythema
Reddish discoloration of the skin due to dilation of superficial blood vessels, secondary to inflammation
Local Inflammation
Redness, warmth, pain in area of thrombus
Palpable Subcutaneous Cord
Feel area of vein that has thrombus in it
CVI
Chronic Venous Insufficiency
General CVI Signs and Symptoms (8)
Spider Veins
Reticular Veins (Telangiectasias)
Varicose Veins
Edema
Skin Changes (Hyperpigmentation)
Ulceration (Wet/”Weepy”)
Heaviness/tightness
Achiness
Other CVI signs and symptoms
Heaviness, tension, achiness, burning or itching, tightness
Hyperpigmentation
Brownish, broany skin tone

Reticular Veins measure , while spider veins are less than in size; many texts say Reticular Veins=
1-3 mm; 1 mm; 2mm
CVI Causes: (4)
“Post-Phlebotic Syndrome”- Recanalization!
Chronic venous obstruction and/or venous valve insufficiency
Frequency of symptoms in CVI is related to site of anatomic involvement and severity of the disease
Pressure the greatest during muscle contraction
Symptoms and Cascade of Events
Venous Obstruction and/or Valvular Insufficiency
Venous Obstruction and/or Valvular Insufficiency (5)
Venous HTN
Capillary Distension
Fibrin Deposition
Lipodermatosclerosis
Cell Death
Venous HTN
Normal: 90 mmHg when standing, 20-30 mmHg when walking
Capillary Distension (4)
Edema
Pain, Achy, Heaviness
Venous Claudication
Stasis Dermatitis
SWELLING (EDEMA) (4)
Begins distally at level of the malleoli
Can progress to mid calf
Worsens with dependency
Relieved with limb elevation

Pitting Edema
Apply pressure to swollen area with finger– it’s pitting edema if the depression stays
Achiness and/or Pain (3)
C/O heaviness or achiness in the limb along with period of standing
Relieved with walking or limb elevation
Typically seen with patients with insufficiency of superficial system
Venous Claudication (3)
Intense burning or cramping in the calf with walking
Caused by rapid increase in both superficial and deep venous pressure due to increase resistance to venous flow
Patients with Iliofemoral DVT and inadequate collaterals are most likely to experience venous claudication
What is claudication most often associated with?! (at least ___________)
peripheral artery disease ???
HYPERPIGMENTATION (3)
Brownish, discolored skin due to VENOUS INSUFFICIENCY
“Brawny” skin changes at the ankle
High venous pressure causes blood cells to be trapped within the tissue
“Brawny” skin changes at the ankle
Most likely to represent CVI
Stasis Dermatitis (2)
Dry, flakey skin located along the inner aspect of the leg above the medial malleolus, may spread to the entire leg
May become inflamed
Lipodermatosclerosis (Induration) (2)
Hardening of the skin
Chronic inflammatory condition characterized by subcutaneous fibrosis and hardening of the skin of the lower legs
Varicose Veins (3)
Due to increase venous pressure
Elongated, tortuous, dilated, and thickened veins
Two Types
Varicose Veins: Due to increase venous pressure (2)
Chronic CVT
Venous Insufficiency
Varicose Veins: Two Types (2)
Primary
Secondary
Primary Varicose Veins (3)
Involves insufficiency of the Superficial Veins Only
Hereditary
Pressure
Primary Varicose Veins: Hereditary (2)
Congenital absence or weakness of the valves
Most common cause of CVI
Primary Varicose Veins: Pressure
Caused by increase in intraluminal pressure on veins: Pregnancy, prolonged standing, obesity
Secondary Varicose Veins (2)
Develop secondary to a disease process
Involves both superficial and deep veins
Develop secondary to a disease process (2)
DVT
Congenital Absence
Congenital Absence:
Klippel Trenaunay Syndrome (KTS)
Klippel Trenaunay Syndrome (KTS)
Absence or atresia of the deep veins
CEAP Classification: Used to classify patients:
C→ Clinical
E→ Etiologic
A→ Anatomic
P→ Pathophysiologic
CEAP– Clinical Classification (6)
C0: no venous insufficiency signs or symptoms
C1: telangiectasias and/or reticular veins (<3 mm in diameter)
C2: varicose veins (≥3 mm in diameter)
C3: edema
C4: skin changes, presently subdivided into
C4A: minor skin changes
C4B: major skin changes such as lipodermatosclerosis
C5: healed skin ulcers
C6: open skin ulcers
CEAP- Etiological Classification (4)
Ep: CVVI is the major cause of clinical manifestations.
Es: CVI or CVVI is secondary to deep venous thrombosis or other pathology.
Ec: CVI or CVVI has a congenital origin (venous malformation or lack of valves).
En: unknown etiology, no venous etiology identified.
CEAP- Anatomical Classification (5)
Ad: CVI or CVVI affects deep veins.
As: CVI or CVVI affects superficial veins.
Ap: CVI or CVVI affects perforating veins.
Ads, Adp, Asp, and Adsp are multiple combinations.
An: no venous anatomy identified.
CEAP- Pathophysiologic Classification (4)
Pr: reflux or reverse venous flow
Po: chronic venous obstruction
Pro: a pathologic combination
Pn: no venous pathophysiology identified
VENOUS STASIS ULCERS (2)
Due to CVI!
Most common type of ulcer you will see!
VENOUS STASIS ULCERS: Onset
Trauma
VENOUS STASIS ULCERS: Course
Chronic
VENOUS STASIS ULCERS: Pain
NONE (unless inflected)
VENOUS STASIS ULCERS: Location
Medial Leg/ankle “Gaiter Zone”
VENOUS STASIS ULCERS: Skin Temperature
Warm