NPB101: Cardiovascular Physiology II
1/65
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
Compared to the resting state, which is true of the cardiac cycle during exercise?
both systole and diastole decrease, but there is a greater decrease in diastole
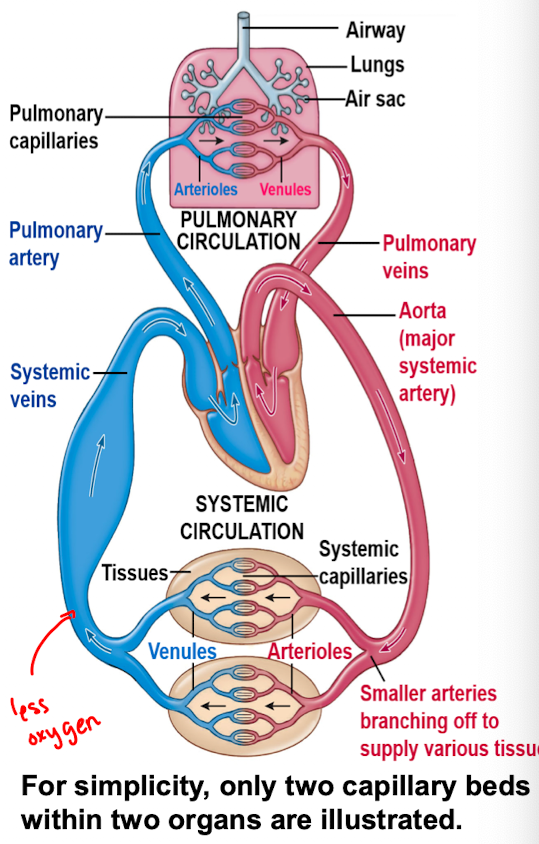
Circulation and blood pressure
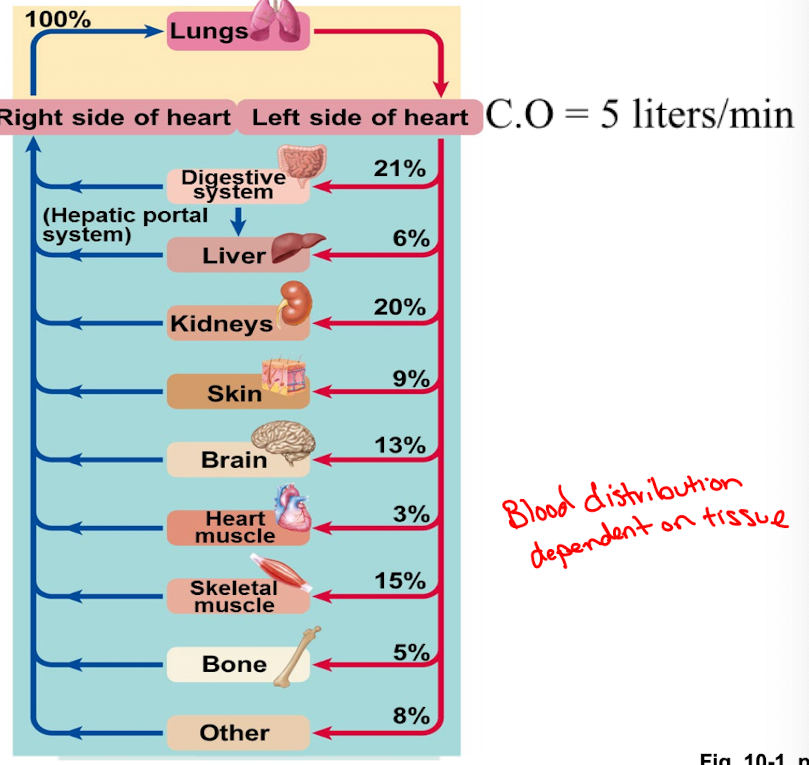
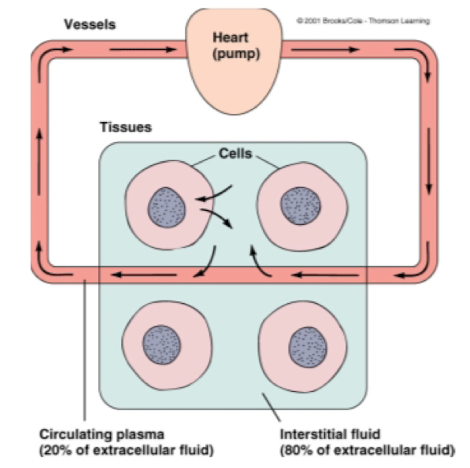
Systemic and pulmonary circulation each consist of a closed system of vessels that transport blood to the tissues in parallel
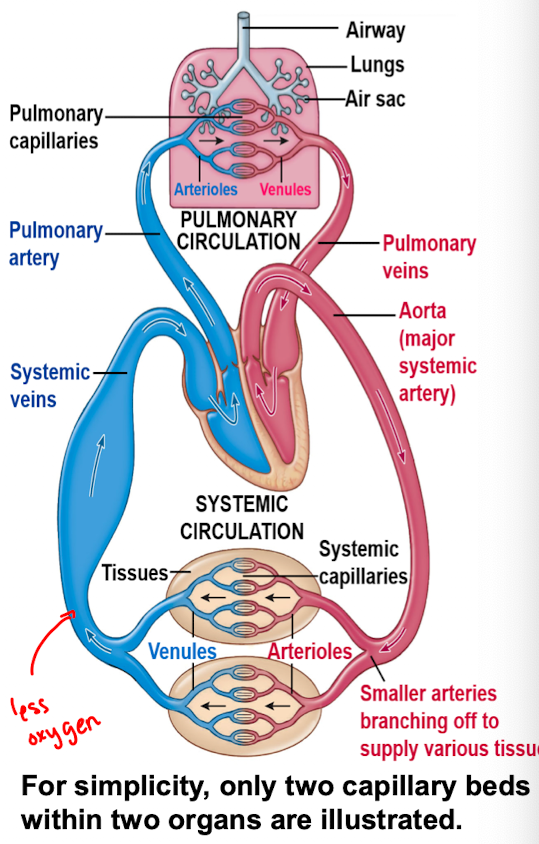
Arteries
Composed of large vessels that carry blood from the heart
Arterioles
small diameter vessels that arise form the branching of arteries when they reach the organs they are supplying
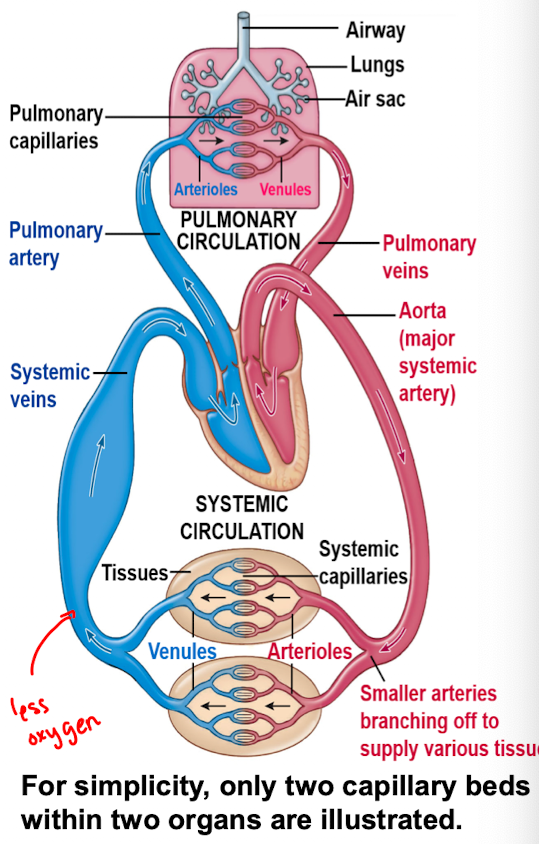
Capillaries
the smallest diameter vessels that are formed when arterioles branch
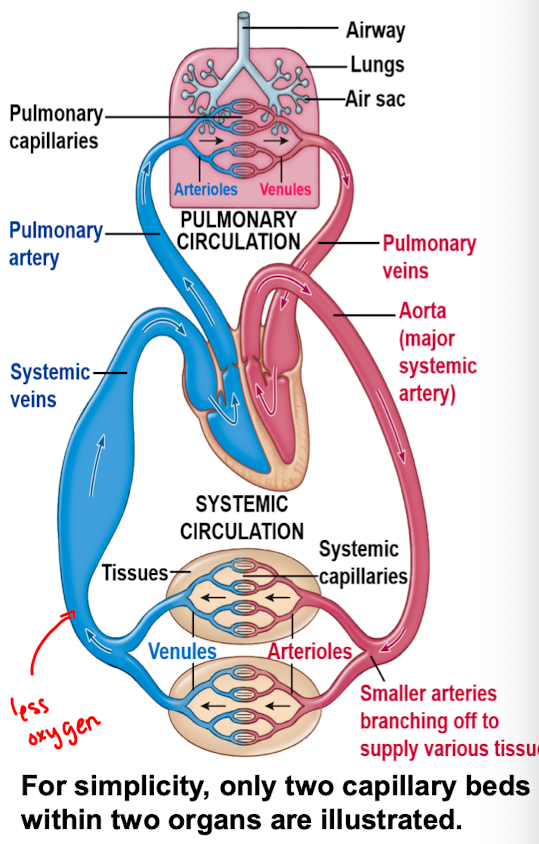
venules
the vessels that form when capillaries join together
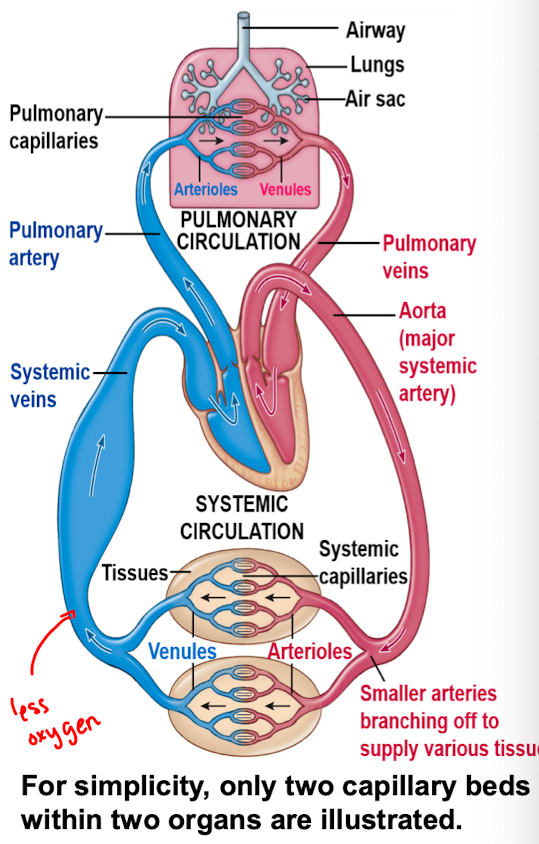
veins
large diameter vessels formed by the merging of venules
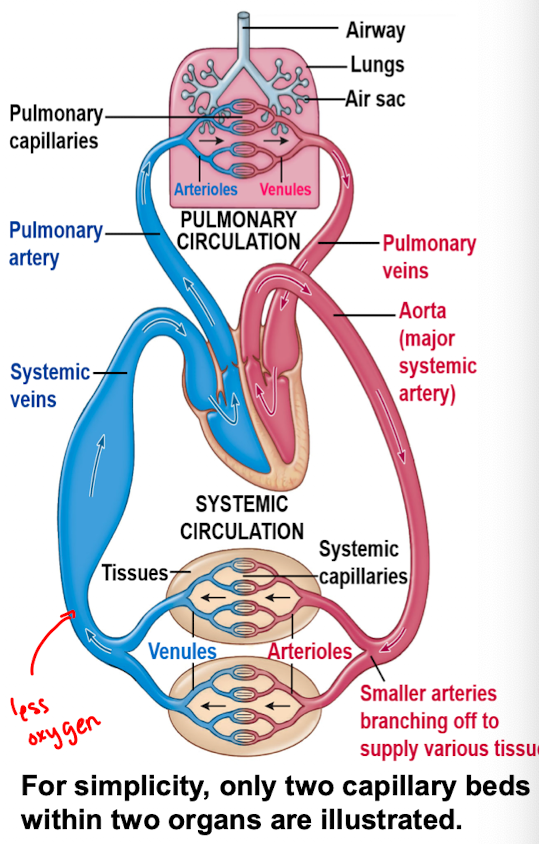
Microcirculation
the name given to the collection of arterioles, capillaries and venules
The larger the ____ area, the easier it is for things to be ____
cross-sectional; exchanged
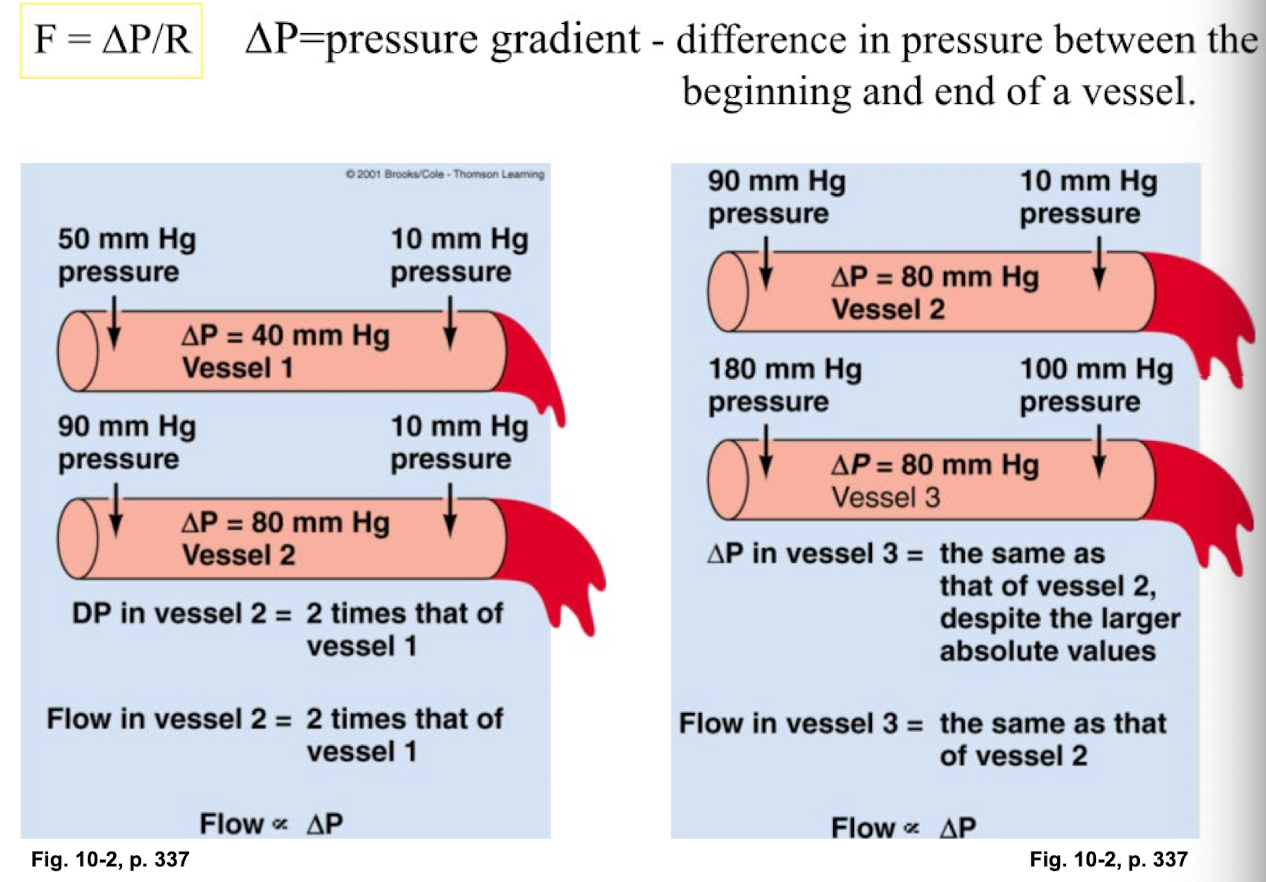
Blood flow is determined by …
pressure gradient in the vessels
resistance to flow caused by friction and viscosity of the blood
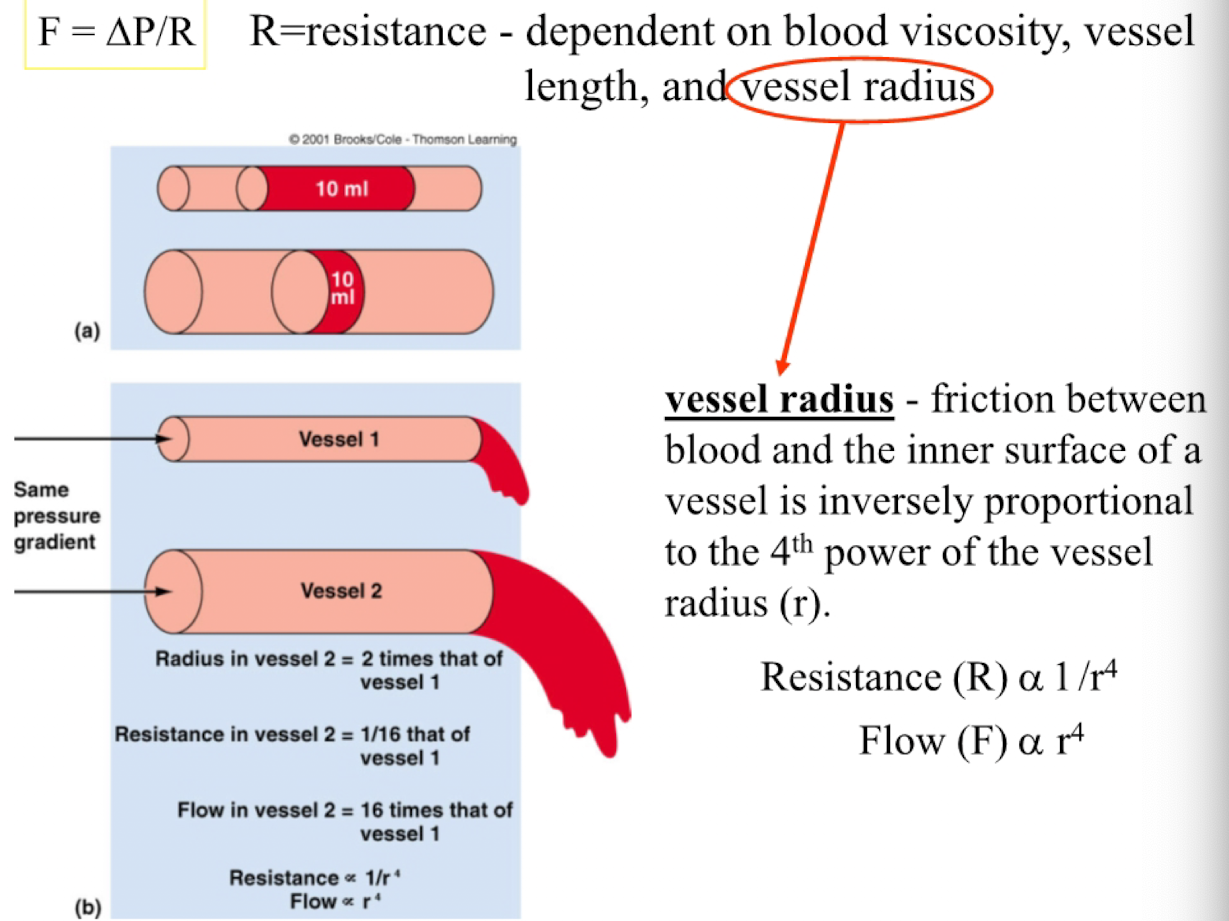
Blood flow equation
F = P/R
F= flow rate, volume of blood passing through a vessel per unit of time
alpha r^4
P = pressure gradient, difference in pressure btwn the beginning and end of a vessel
R = Resistance, resistance to flow depends on 3 factors
Blood viscosity
Vessel Length
Vessel radius
Blood Viscosity
friction developed in blood, determined by the concentration of plasma proteins, and the number of circulating red blood cells
Vessel length
friction between blood and the inner surface of a vessel is proportional to the vessel length
Vessel radius
friction btwn blood and inner surface of a vessel is inversely proportional to the 4th power of the vessel radius ( r )
resistance (R) alpha 1/r^4
Flow (F) alpha r^4
If all other variables remain constant, which of the following is not true of the amount of fluid that would flow through a vessel?
Doubling the radius of the vessel would result in 4 times more flow
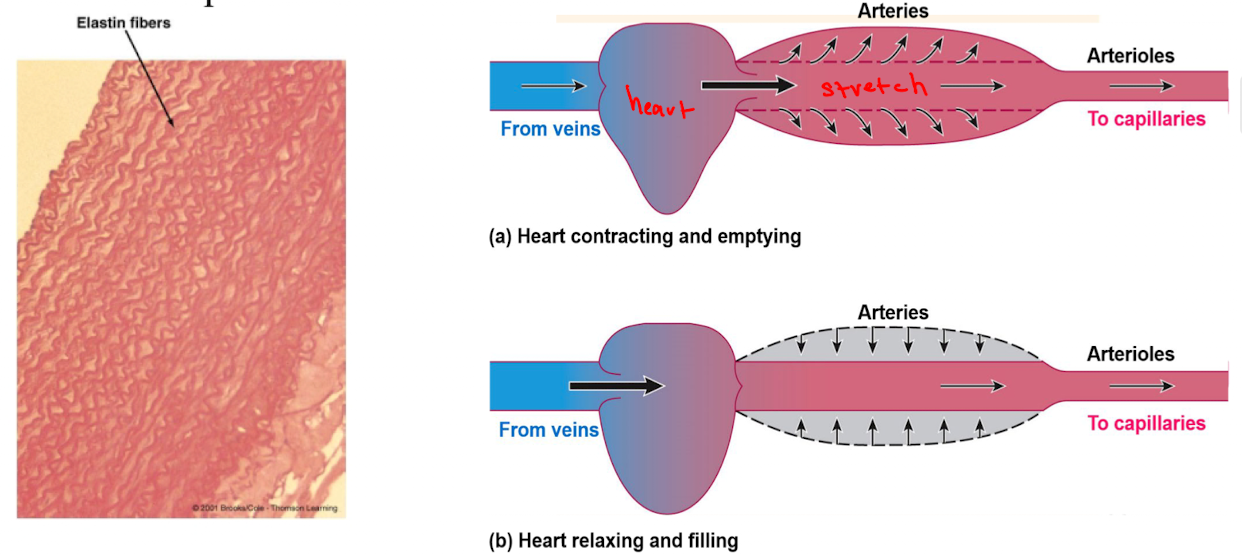
Arteries: good for
large vessels serve as conduit for the low resistance flow of blood and bc of their elasticity they act as a pressure reservoir
Pressure Reservoir
Can serve as a driving force during ventricular diastole. Due to elasticity of the artery walls (smooth muscle, collagen, elastin). Arteries can expand and store the pressure imparted by cardiac contraction. During relation the arterial walls recoil and maintain pressure
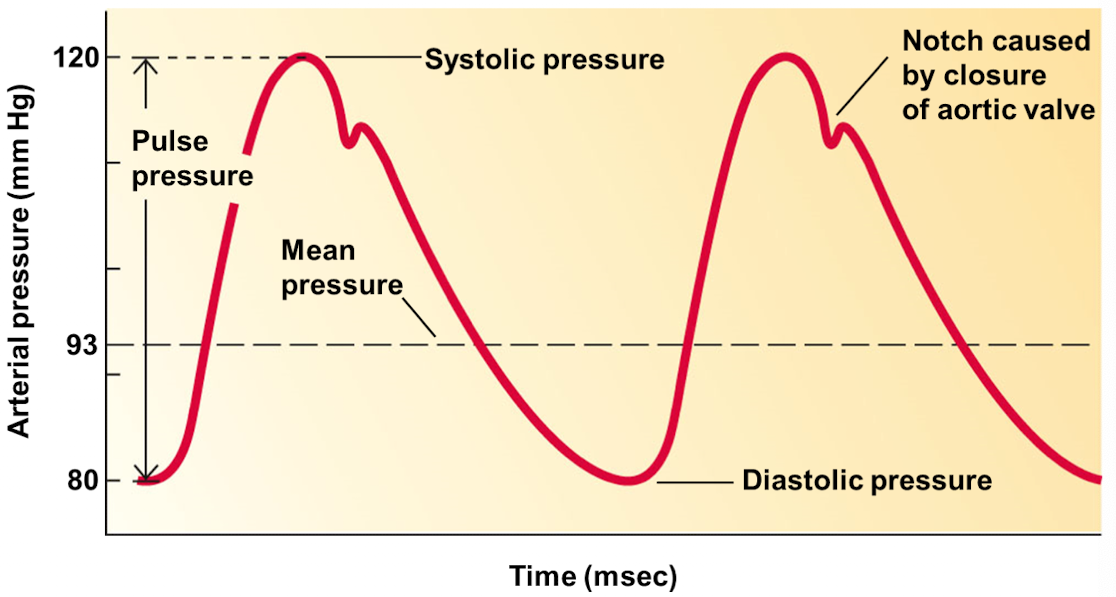
Pulse pressure
pressure difference between systolic pressure and diastolic pressure
Mean arterial pressure
pressure that is monitored and regulated by blood pressure reflexes
Mean arterial pressure = diastolic pressure + 1/3 pulse pressure
Sphygmomanometer
device used to measure systolic and diastolic arterial blood pressure
When cuff pressure is greater than 120 mm Hg …
no blood flows through the vessel
no sound is heard
When cuff pressure is between 120 and 80 mm Hg…
blood flow through the vessel is turbulent whenever blood pressure exceeds cutoff pressure
Intermittent sounds are heard as blood pressure fluctuates throughout the cardiac cycle
When cuff pressure is less than 80 mm Hg…
blood flows through the vessel in a smooth, laminar fashion
no sound is heard
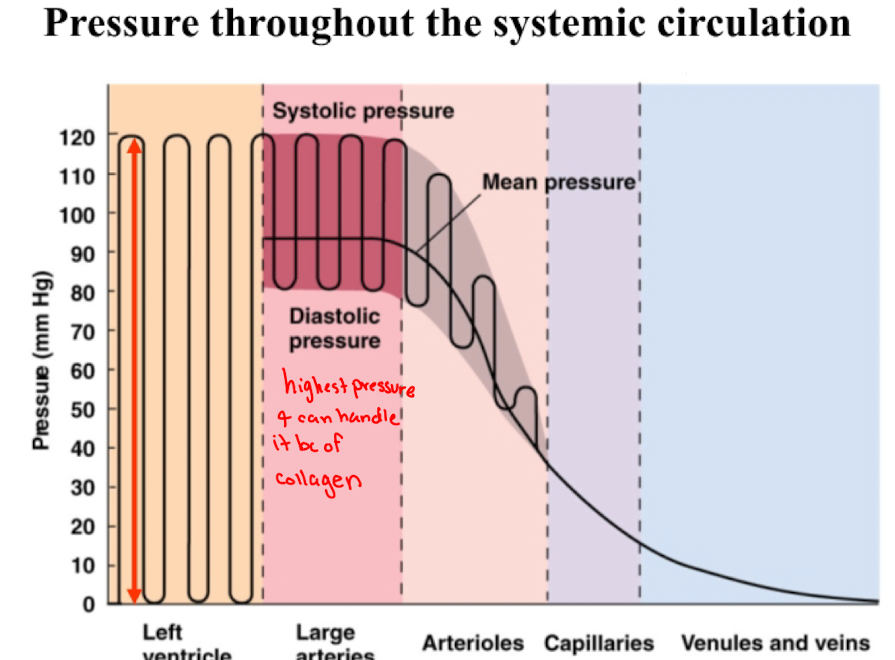
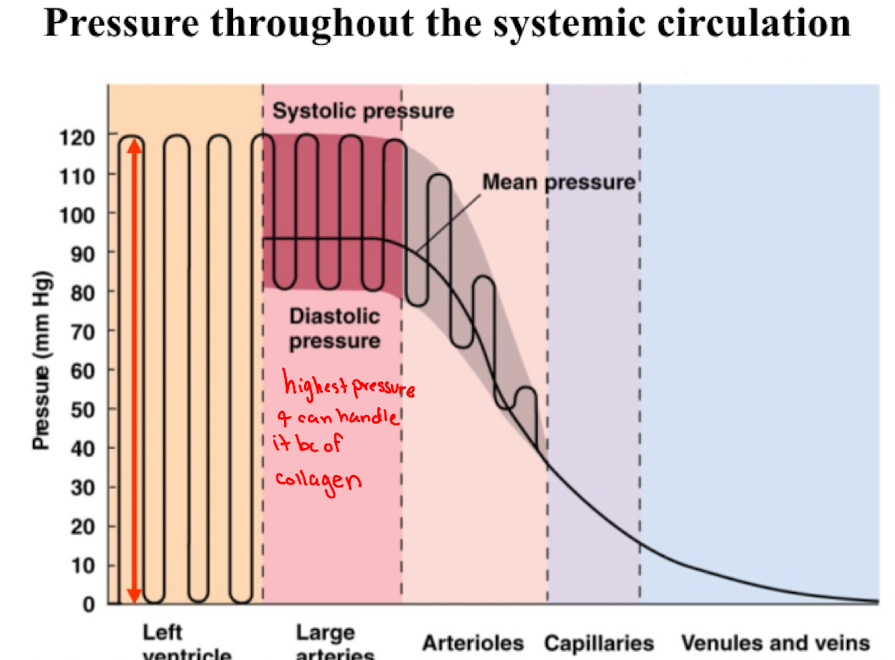
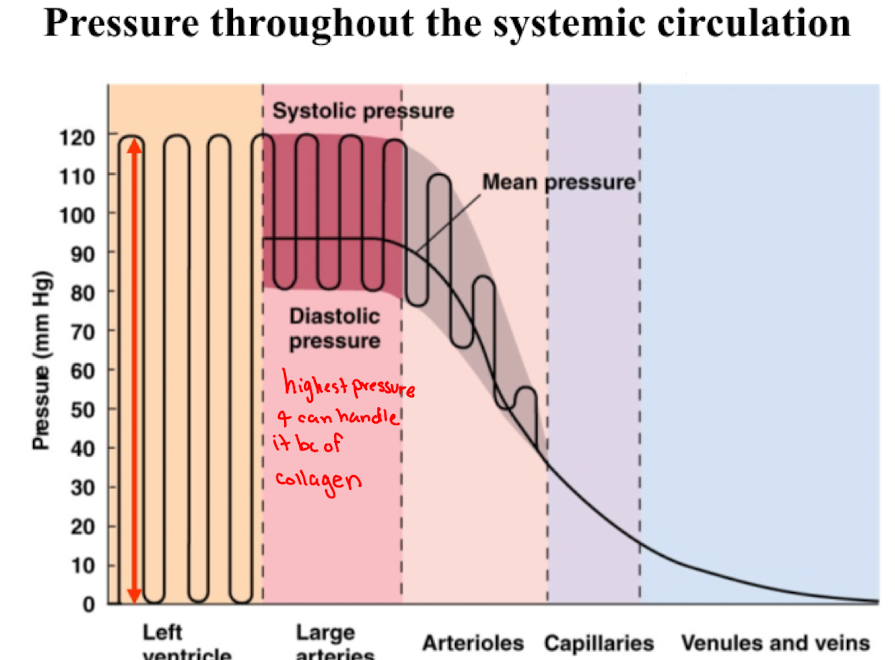
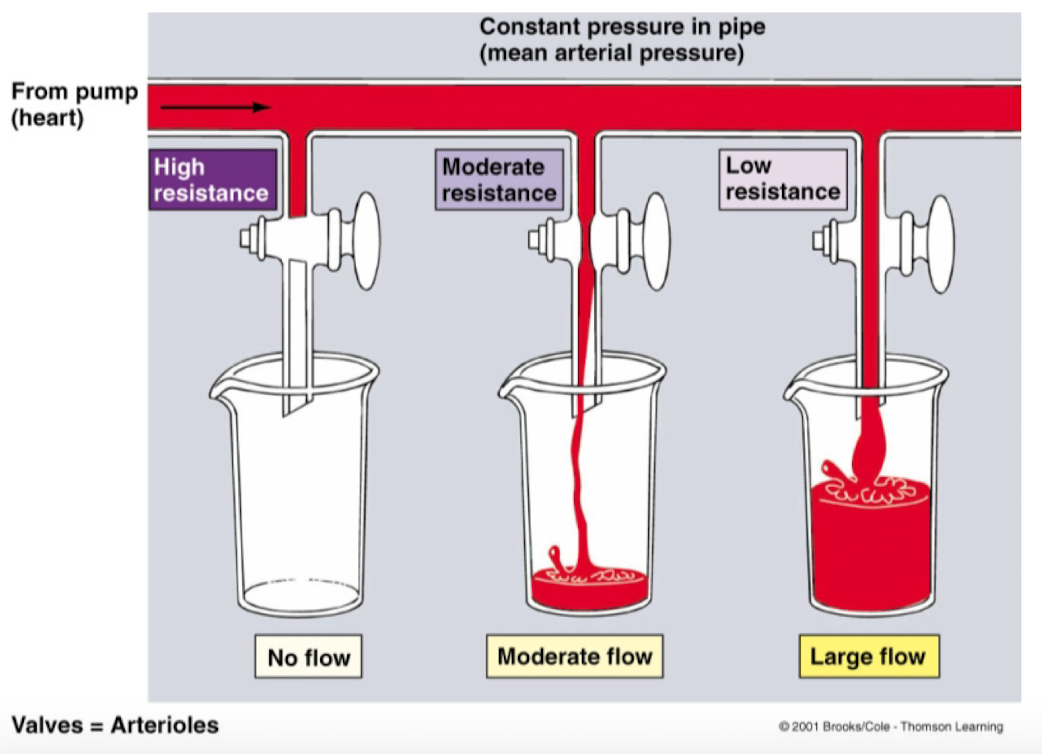
Left ventricular pressure
swings between a low of 0 mm Hg during diastole to a high of 120 mm Hg during systole
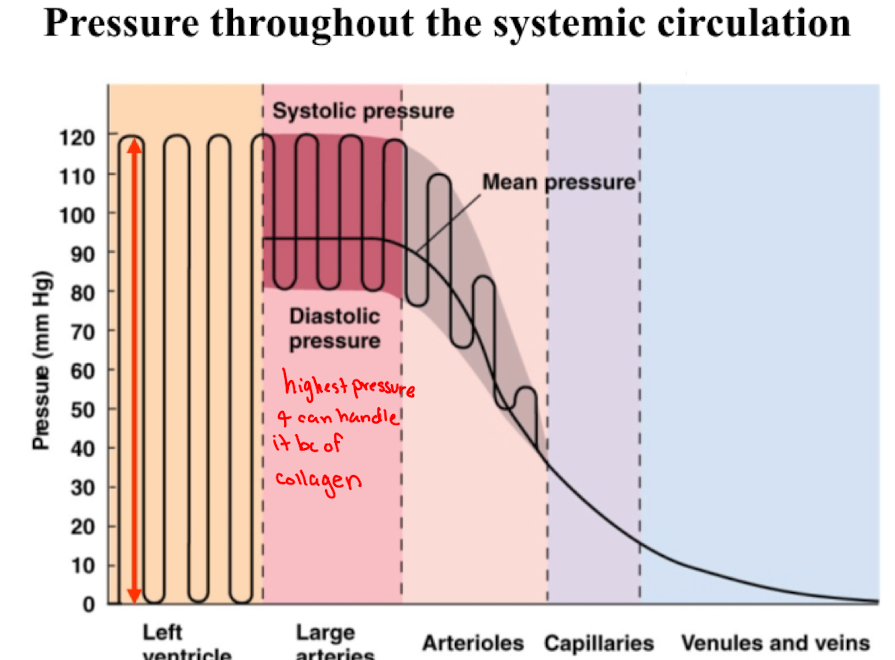
Arterial pressure
Fluctuates between a peak systolic pressure of 120 mm Hg an d allow diastolic pressure of 80 mm Hg
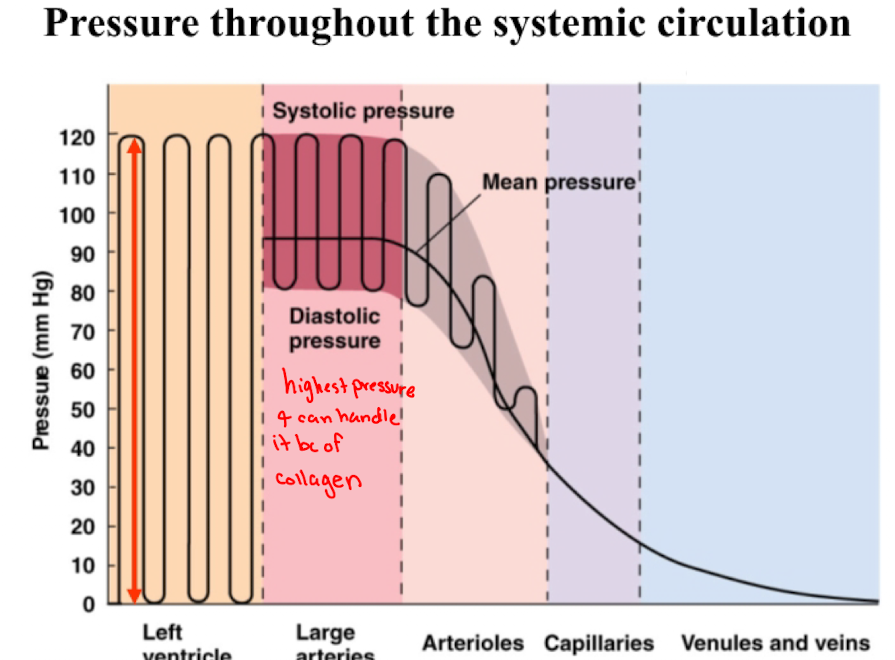
Arteriolar pressure
drops dramatically across the length of the arterioles such that the systolic-to-diastolic swings in pressure are converted to a non-pulsatile pressure when blood flows through the arterioles
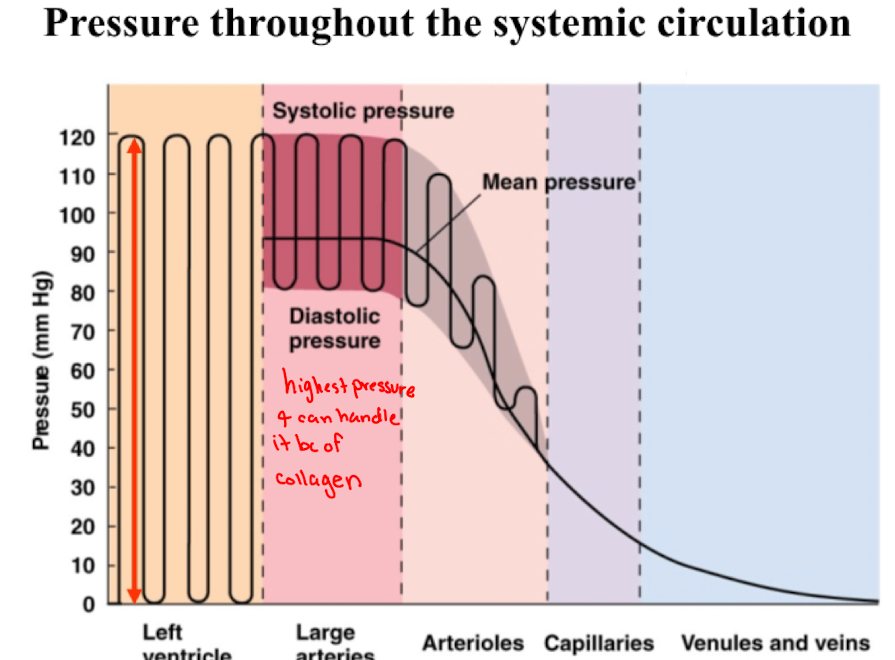
Pressure
continues to decline (but at a slower rate) as blood flows through the capillaries and venous system
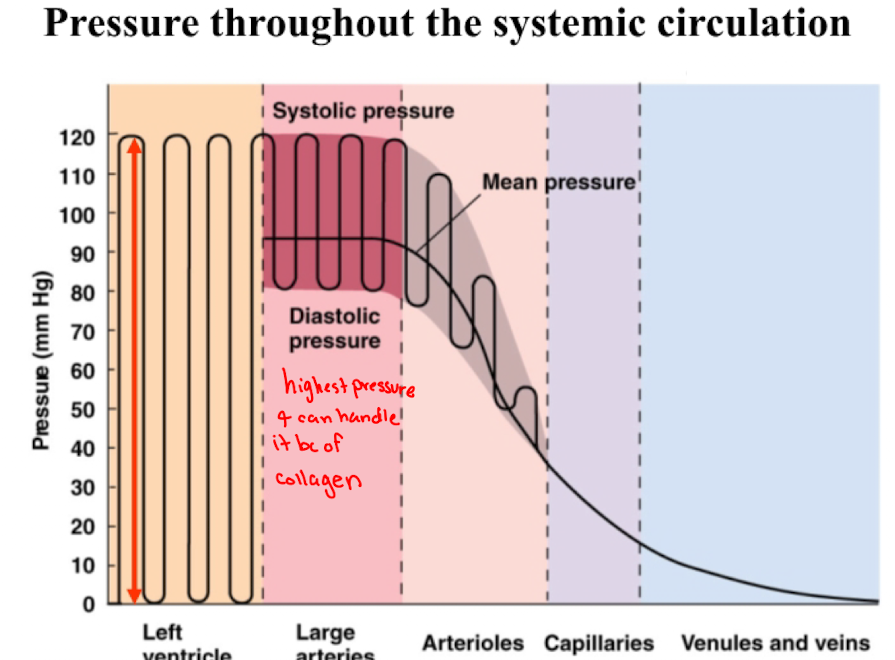
Cardiovascular Response to Exercise
More amount of blood flowing during exercise but the proportion of blood decreases
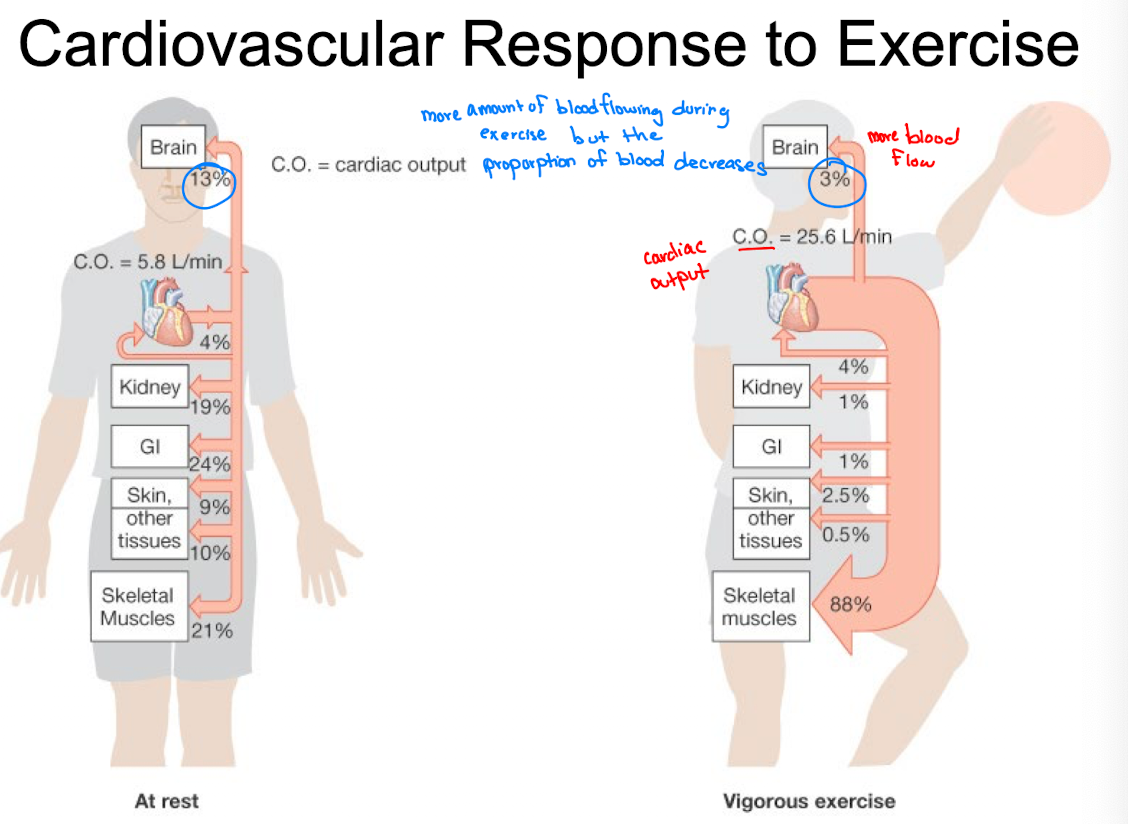
Arterioles
Source of vascular resistance in the circulatory system.
Arteriolar radius is regulated intrinsically and extrinsically to control cardiac output and arterial pressure
Intrinsic (or local) control
factors intrinsic to an organ or tissue. Subdivided into chemical and physical controls:
local chemical control
local metabolic changes
local physical control
Intrinsic- Local Metabolic Changes
Factors derived from metabolic activity causing dilation.
O2 concentration: reduced O2 during metabolic demand
CO2 concentration: increased CO2 during metabolic demand
pH: increases in CO2 and/or lactic acid lowers the blood pH
Extracellular K+ concentration: increased neuronal activity that outpaces the Na+/K+ ATPase
Osmolarity: increased solute concentration resulting from metabolic activity
Adenosine: released in cardiac muscle in response to metabolic demand
Prostaglandins: produced from the metabolism of fatty acids
Histamine release- released when tissues are damaged and leads to vasodilation accompanying an inflammatory response
Smooth muscle tone is controlled by…
the release of mediators, such as Nitric Oxide (NO), from the endothelial cells lining the inner walls of the arterioles
Intrinsic- Local Physical Control
Temperature: arteriolar smooth muscle tone is inversely proportional to temperature
Myogenic response: arteriolar smooth muscle responds to stretch by contracting
Which is true of arterial blood pressure during progressive dynamic exercise?
There is a progressive increase in systolic blood pressure and mean blood pressure but diastolic pressure changes very little
Capillary Exchange
exchange of materials btwn the blood and the interstitial space
Occurs by diffusion and bulk flow
interstitial fluid (plasma membrane) takes on the same composition as the arterial blood
Capillary Exchange: Diffusion
substances in the blood move independently of one another down their concentration gradients
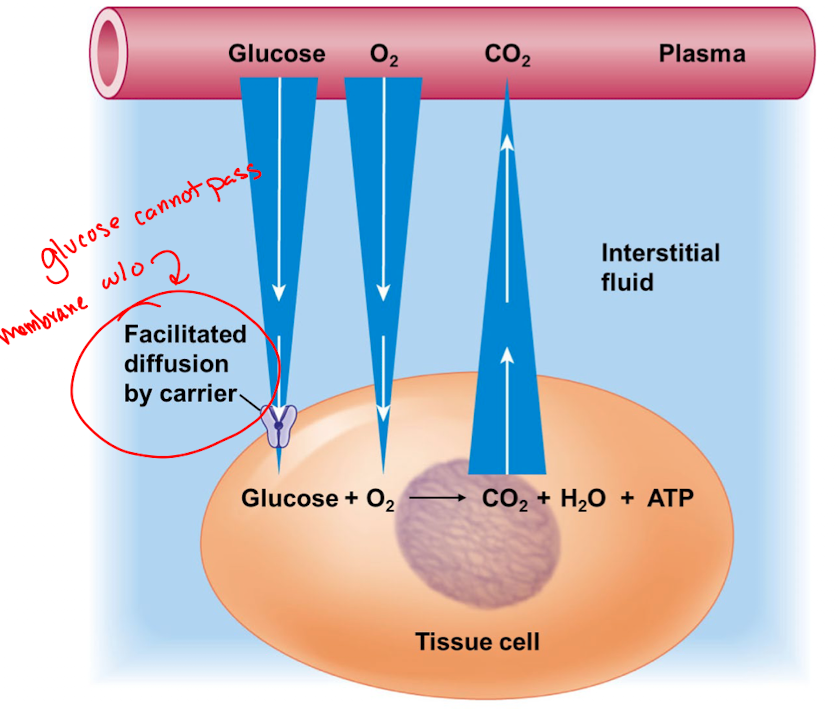
Transport across a typical capillary wall
lipid-soluble substances
small water-soluble substances
plasma proteins
exchangeable proteins
lipid-soluble substances pass through the endothelial cells
Small water-soluble substance pass through the pores
Plasma proteins generally cannot cross the capillary wall
Exchangeable proteins are moved across by vesicular transport

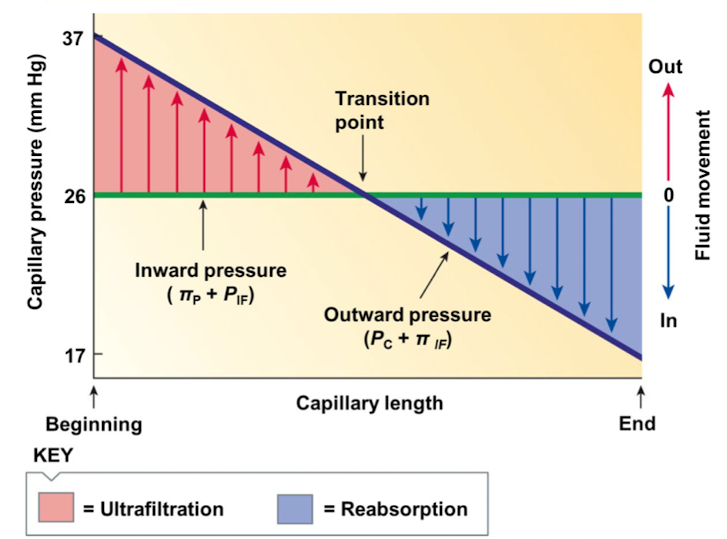
Capillary Exchange: Bulk Flow
mechanism for maintaining fluid balance btwn the blood and the extracellular space
pores in capillary walls permit the flow of plasma, but not proteins or blood cells
Ultrafiltration
bulk flow into the tissues, occurs when the net pressure is positive
reabsorption
bulk flow into the capillaries, occurs when the net pressures negative
Which types of blood vessels carries blood away from the heart?
arteries
What are capillaries
tiny blood vessels that connect arteries to veins
4 Factors that influence bulk flow and net pressure equation
capillary blood pressure (Pc)
plasma-colloid osmotic pressure (πp)
interstitial fluid hydrostatic pressure (PIF)
interstitial fluid-colloid osmotic pressure (πIF)
net pressure = (Pc + πIF) - (PIF + πp)
Capillary blood pressure (Pc)
hydrostatic pressure exerted on the inside of the capillaries. Forces fluid out of the capillaries and into the interstitial fluids
Plasma-colloid osmotic pressure (πp)
Osmotic force pushing water into the capillaries from the interstitial fluid. Controlled by the concetration of protein in the blood plasma
Interstitial fluid hydrostatic pressure (PIF)
hydrostatic pressure exerted on the outside of the capillary walls. Forces fluid into the capillaries from the interstitial fluid
Interstitial fluid-colloid osmotic pressure (πIF)
osmotic force pushing water out of the capillaries into the interstitial fluid
What capillary exchange/bulk flow variables are outward pressure
(Pc) - capillary blood pressure
(πIF) - interstitial fluid-colloid osmotic pressure
→ (Pc + πIF)
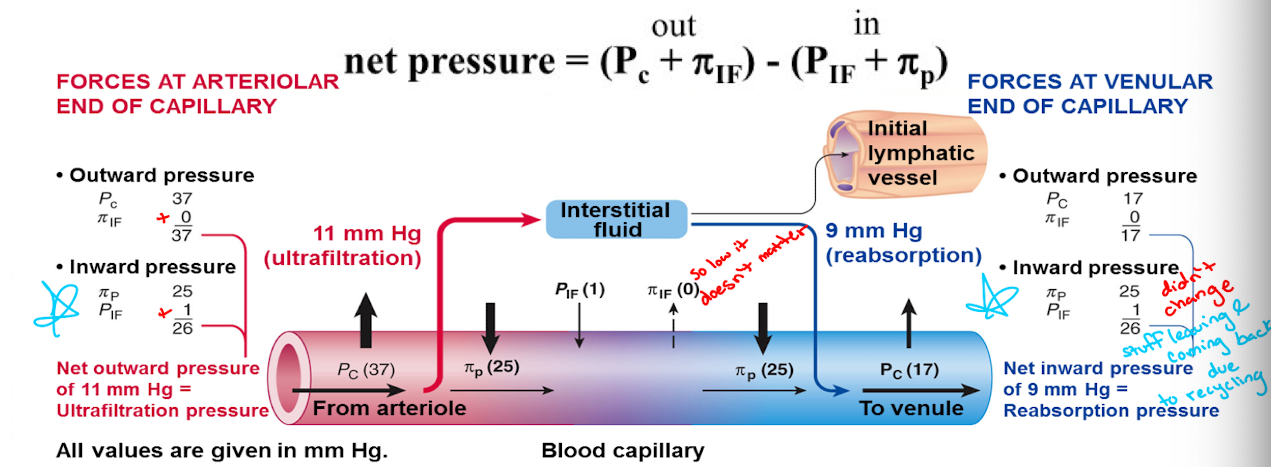
What capillary exchange/bulk flow variables are inward pressure
(πp) - plasma-colloid osmotic pressure
(PIF) - interstitial fluid hydrostatic pressure
→ (PIF + πp)
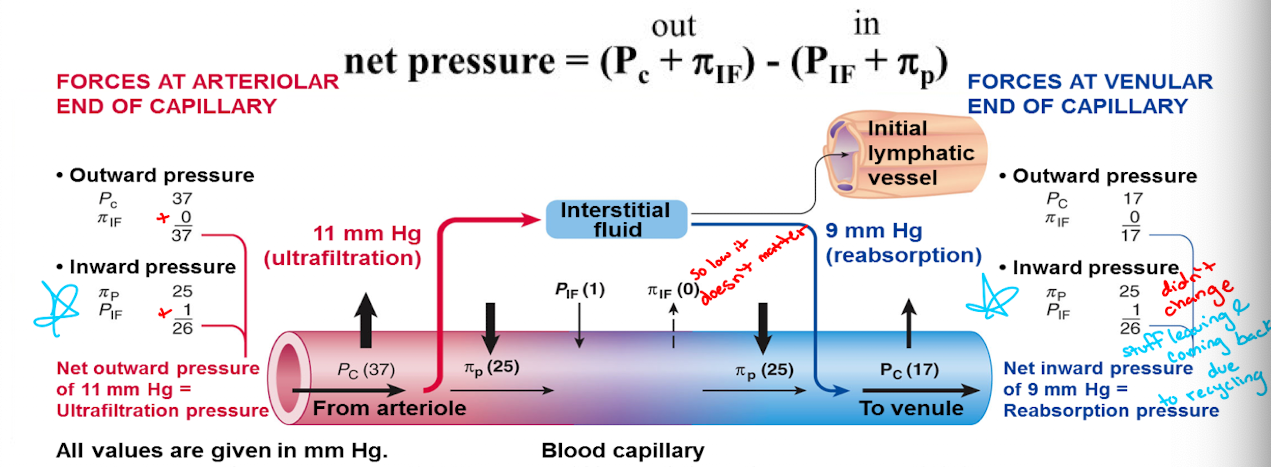
Net Filtration and net reabsorption along the vessel length
the inward pressure (PIF + πp) remains constant throughout the length of the capillary whereas the outwards pressure (Pc + πIF) progressively declines throughout the capillary’s length
Net filtration pressure is calculated by…
subtracting the blood colloid osmotic pressure from the capillary hydrostatic pressure
T/F: plasma proteins suspended in the blood cross the capillary cell membrane and enter the tissue fluid via facilitated diffusion. Why?
False; plasma proteins suspended in blood cannot cross the semipermeable capillary cell membrane and so they remain in the plasma within the vessel, where they account for the blood colloid osmotic pressure
Veins
vessels serve as a reservoir for blood and conduit for blood flow back to the heart
venous capacity
volume of blood the veins can accommodate
depends on the distensibility of the venous walls and the influence of any externally applied force
venous return
volume of blood entering each atrium per minute. Influenced by several factors
Factors influencing venous return (5)
sympathetic activity
skeletal muscle activity
venous valves
respiratory activity
cardiac suction
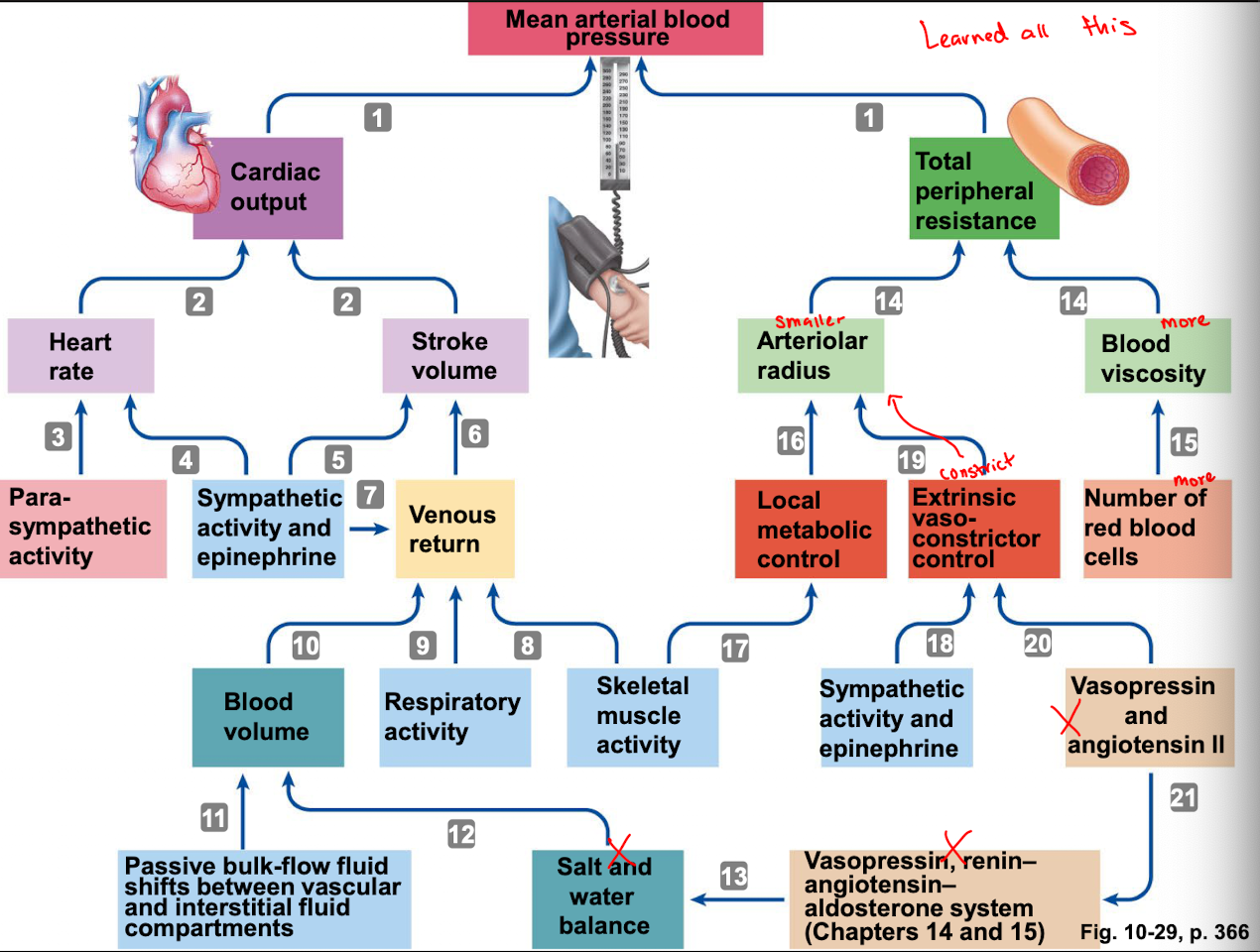
Factors influencing Venous Return: Sympathetic Activity
sympathetic stimulation produces vasoconstriction to increase venous pressure and enhance venous return
Factors influencing Venous Return:: Skeletal Muscle Activity
contraction of skeletal muscles compresses veins and increases venous pressure which counteracts the effect of gravity
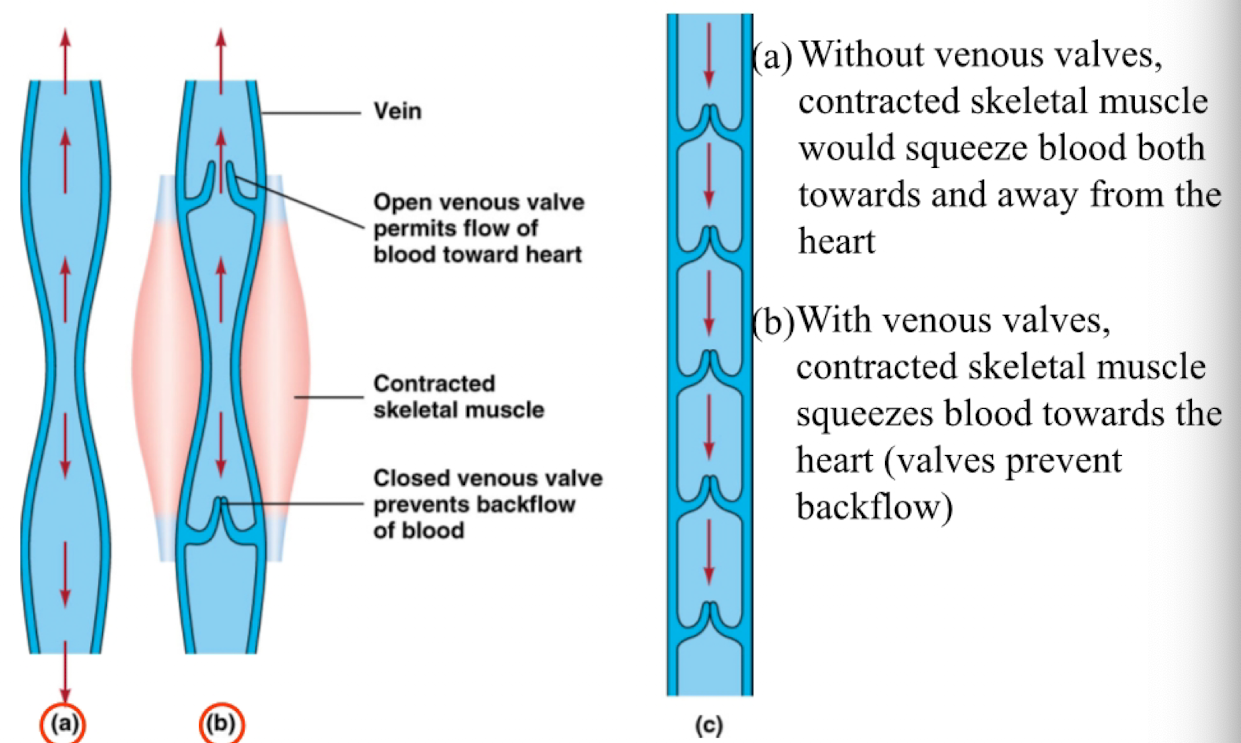
Factors influencing Venous Return: Venous Valves
located within the lumen of large veins and prevent the back flow of venous blood
a. without venous valves, contracted skeletal muscle would squeeze blood both towards and away from the heart
b, with venous valves, contracted skeletal muscle squeezes blood towards the heart (valves prevent back flow)
Factors influencing Venous Return: Respiratory Activity
Pressure within the chest cavity transiently decreases during respiration. This increases the pressure gradient between the veins in the lower exterminates and the chest
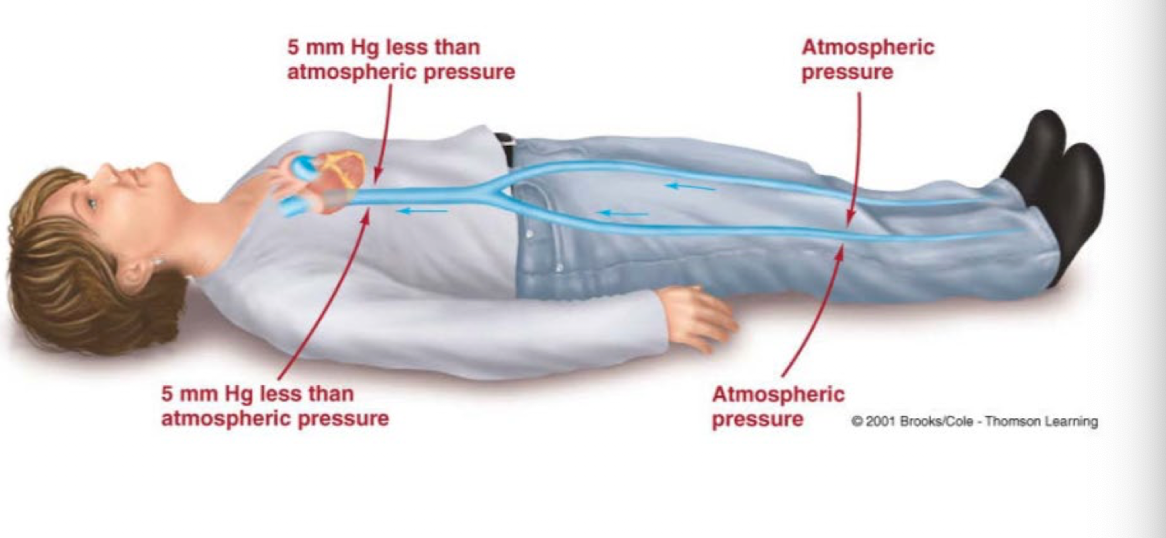
Factors influencing Venous Return: Cardiac Suction
during ventricular contraction atrial pressure transiently falls below 0mm go Hg. This increases the venous pressure gradient and sucks venous blood into the atria
Baroreceptor reflex
autonomically regulates cardiac output and total peripheral resistance
respond to changes in arterial blood pressure by elevating or reducing their rate of firing
signals alter the ratio of activity in the parasympathetic and sympathetic neurons of the cardiovascular control centers
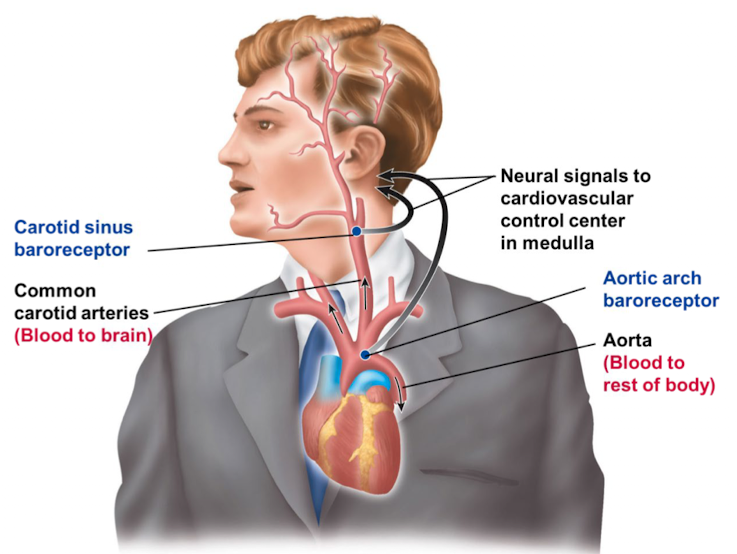
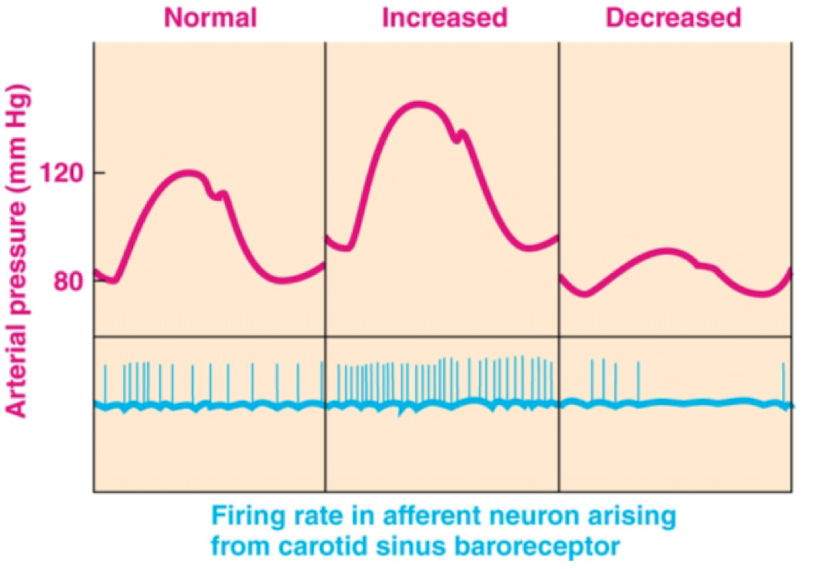
Baroreceptors: when arterial pressure increases and decreases what happens to firing rate?
are mechanoreceptors sensitive to changes in both mean arterial pressure and pulse pressure
constantly provide information about blood pressure
when arterial pressure increases, the firing rate of their afferent neuron increases. When arterial pressure decreases, the firing rate of their afferent neuron decreases
Hypertension, 2 classes of hypertension
blood pressure above 140/90 mm Hg
Primary hypertension: unknown cause accounts for 90% of cases
Secondary: occurs secondary to another known primary problem, accounts for 10% of cases
Hypotension
Blood pressure below 100/60 mm Hg
How many major types of blood have scientists discovered?
4: Types A, B, AB, O