Microbio Lab Practical 1
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
Why do we culture bacteria?
To isolate , identify and study microorganisms
Aseptic
free from disease-causing microorganisms
Aseptic technique
A procedure performed under sterile conditions.
Fomite
A physical object that serves to transmit an infectious agent from person to person.
Disinfect
to rid of infectious agents
Kill most but not all
Reduce the transfer of pathogens
Sterilize
to make free from microorganisms
Kill all bacteria
What are two reason why you needed to boil the media during the preparation?
To kill the microorganisms, and to dissolve the powder so it solidifies with the water
Why did you flame the mouth of the flask before and after you poured each plate?
To sterilize the mouth of the flask and prevent or minimize contamination
Why did you invert the plates for storage once they were solidified?
To lessen contamination risk from airborne particles and accumulation of water condensation that could compromise a culture
Does hand washing disinfect or sterilize your hands?
Disinfect
What should an optimal Bunsen burner flame look like?
Two cones

What is the hottest part of the Bunsen burner flame?
The innermost oval on the top
Why is it important to allow your loop or needle to cool before obtaining your bacterial sample?
So you don't kill your bacteria
Why is it important to flame your loop between each quadrant when you are using the streak plate method?
To kill off culture and move them around so it is not so concentrated in one place
What two reason might you use the streak plate method?
1. Isolate a pure culture 2. Steak for isolation in a mixed culture
When removing a cap from a tube to inoculate, you should plate cap on the bench (T/F)
F
You should use a large drop of oil for the 100x objective to ensure you can see the sample clearly (T/F)
F
How should you clean the 100x object after you are done using it?
Lens wipe
Describe how you would prepare a sweet mount of a bacterial sample. What would be different if you obtained the sample from broth vs a colony growing on agar?
Drop of water and bacteria
Broth is just a drop while agar is water droplet and bacteria scooped and mixed in with the droplet
Gram Staining Step
1) Primary Stain (Crystal Violet) (20 s)
2) Mordant (Grams iodide) (1 min)
3) Decolorize (ethanol) (few secs)
4) Secondary Stain (Sacranin) (1 min)
Gram positive Stain
purple/blue
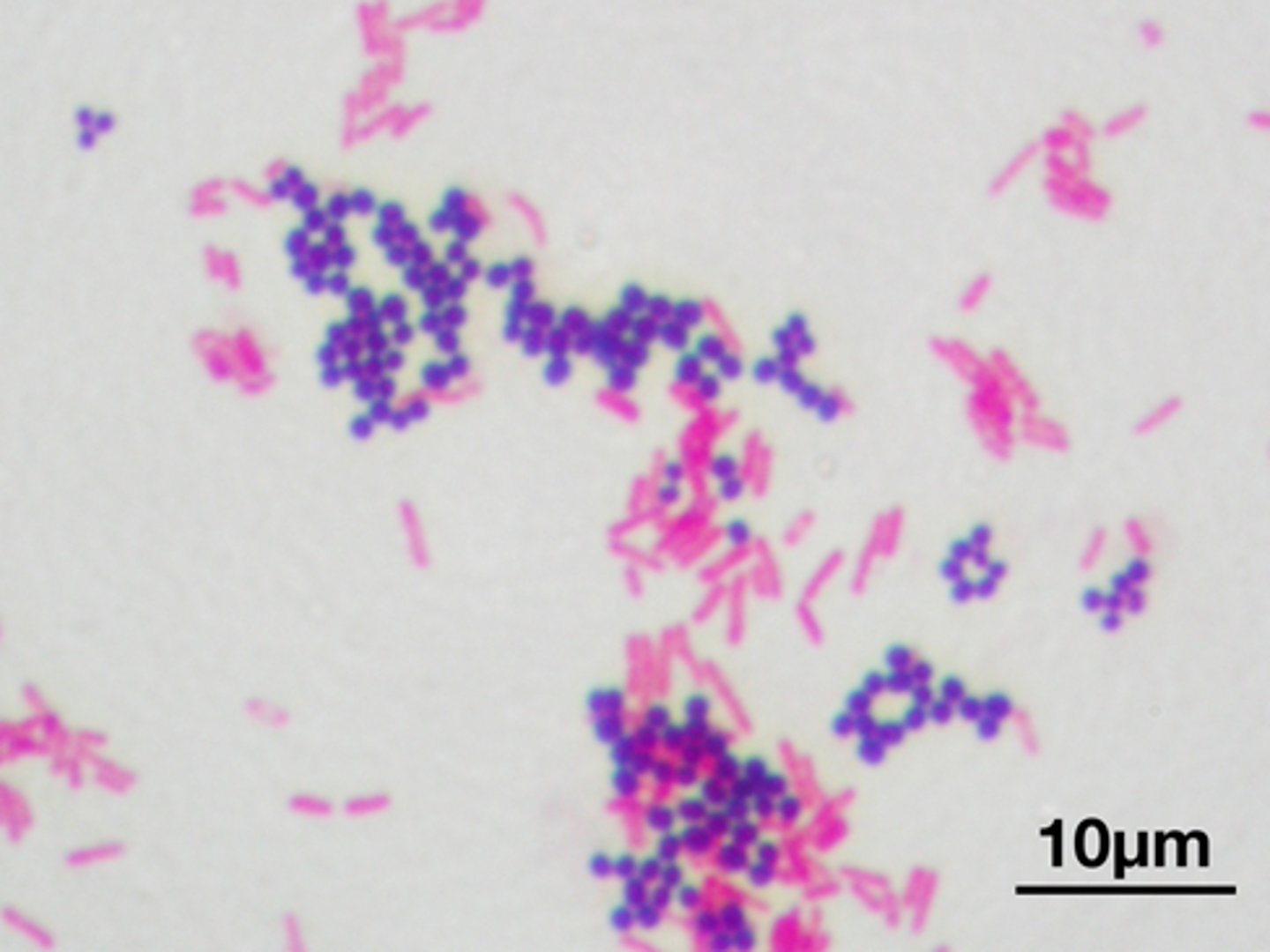
Gram Negative Stain
red/pink
Why do smears need to be fixed prior to staining?
So the cells do not wash off during staining, or kill them.
What are three possible ways to fix a slide?
1) Menthol (1 min)
2) heat by flame (<1 min)
3) Gentle Heat (10 min)
Which method of fixation is preferable and why?
Menthol because its the quickest and most reliable, doesn't damage the cells like heat does
What is the difference between a simple stain and differential stain?
Simple: One stain
Differential: More than one
Why do you need to make sure you do a very thin smear when preparing a bacterial smear?
Too much will make the bacteria pile on top of each other
What is a mordant and why is it used in staining?
Is a chemical used to "bond" dye and tissue together. Basically makes the dye stick.
What is the most critical step in gram stain? Why?
The decolorizing step because then everything would be the same color and defeat the purpose of staining
How do the cell walls differ between gram positive and gram negative?
Gram+ has a thicker PG layer than Gram -.
How do the properties of the stains used for gram differ from those used for a negative staining procedure
A negative staining procedure uses acidic dye and positive use basic dyes
Why do you want to use an old culture for endospore staining?
So that the bacteria can actually produce an endospore (from starvation)
Why do we steam the sample for the endospore stain and the acid fast stain?
To penetrate the spore
Which types of cells does an acid-fast stain help identify?
Atypical cell-walls, with myocolic acid
Are stained with the negative stain technique dead or alive? Are they any special precautions we need to make based on this?
They are still alive. Yes, using ethanol on everything after lab to kill bacteria.
What are two reason for using the negative staining technique?
1. Used for bacterial culture that are hard to stain with basic dyes
2. Fragile or easily distorted by fixation
Does a negative stain use an acidic or basic staining dye? What does this mean in terms of properties of the stain?
Acidic dye, it is a negative staining procedure
Dis what a negative stain looks under a microscope. Why does it appear that way?
The background is dark and the bacteria are light. It appears that way because the dye is negatively charged and is therefore repelled by the bacterial cell wall
Endospore Staining procedure
1. Primary Stain (Malachite Green)
2. Mordant (Heat)
3. Decolorize (water)
4. Counterstain (Safanin)
Acid-fast Staining procedure
1. Primary Stain (Carbofachsin)
2. Mordant (heat)
3. Decolorize (Acid alcohol)
4. Secondary Stain (Methylene Blue)
Do dead cells contribute to optical density (OD)?
yuh both
Optical Density
measures how well a medium can transmit light, is different from the actual density of the medium (ex. water has a higher optical density than air so light travels slower in water than air)
What is the benefit of the OD reading it if measure some cells that are dead?
It's very quick estimate of cell density
What is the purpose of plating the sterile medium?
To grow colonies, just that specific bacteria. To count bacteria. To compare/check for contamination
Why culture E. coli at 37 C?
It's the same temperature as the human body. Mimics gut environment
Which pipette (P10, P20, P200, P100)) should you use if you wanted to measure 50 ul
P 200
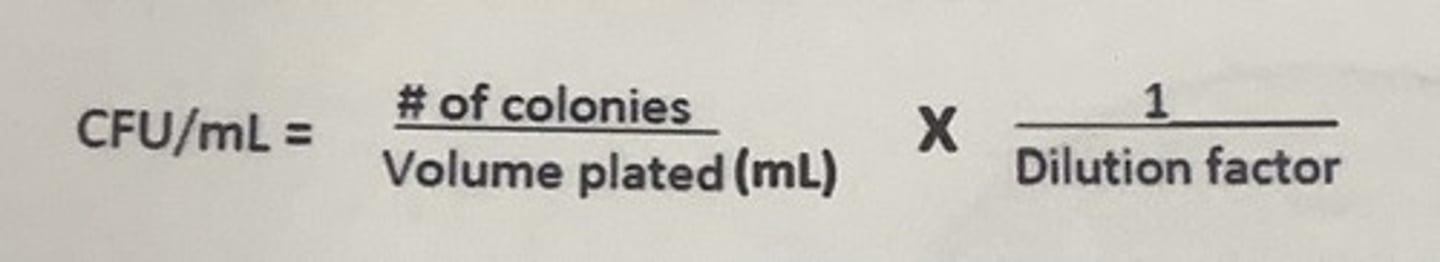
CFU/ ml formula
number of colonies/(dilution X amount plated)
What types of metabolism occurs in the presence of oxygen? Absence?
O2: Aerobic respiration
No O2: Anaerobic respiration
What damaging substances are produced during metabolism in the presence of oxygen?
Hydrogen perioxide
What enzyme does a culture have if it produced bubbles in the catalase tests? What does this enzyme do?
Catalase, helps protect bacteria from hydrogen peroxide
What gas do the bubbles contain in a positive catalase test?
oxygen gas
A culture with a positive oxidase test possess what enzyme?
Cytochrome oxidase
If a culture is oxidase positive, the bacteria must have respiration metabolism (T/F)
F
How would you classify an organism that grows optimally at 27 C
Mesophile
What is meant by cell morphology?
The appearance of the colony (color, shape, elevation, edge, etc)
What is meant by cell arrangement?
Diplo, stereo, tetrad, staphylococcus, etc
P20 capacity
2-20 ul
P200 capacity
20-200 ul
P1000 Capacity
100-1000 ul
Micropipette produced
1. Use thumbwheel to adjust desired volume
2. Put on tip
3. Depress knob to first stop
4. Stick tip into sample fluid
5. Release knob slowly and carefully to draw the same into the tip
6. Move the tip into the container you want to transfer liqud
7. push down slowly and evenly to the second stop
8. eject tip into waste beaker
Spread plate Procedure
1. Label bottom of plate
2. Light bunsen burner
3. Use P200 micropipette to transfer 100ul to surface of plate
4. Flame sterilize spreader by dipping it in ethanol, pass it though the Bunsen burner and allow the ethanol to burn off
5. allow to cool
6. touch the cooled spreader to the sample in the center of the agar and spread the sample across the entire surface while rotating the plate
7. Flame sterilize you spreader when done
Fixing bacteria Procedure
1. Label slide and draw a circle on the back of the of the slide with the wax pencil
2. add the bacterial culture to the top of the slide,
3. Smear the culture to spread it thin on the slide
4. Allow to air dry
5. Place slide on a slide rack over staining bucket. and cover smear with 95% methanol for at least 1 minute
6. Rinse off using water, do not shoot water directly on the smear
Gram Staining Procedure
1. Hold the slide with the bacterial smear with clothes pin
2. Cover smear with crystal violent for 20 seconds, rinse with water
3. Cover with gram's iodide for 1 min, rinse
4. Decolorize by holding the slide at a 45 degree angle and add ethanol droop by drop for a few seconds
5. Immediately rinse to remove the decolorized
6. Cover the smear from with safranin for one minutes, rinse
7.Blot the water from the slide between pieces of bibulous paper
8. Observe sample
Oxidase and Catalase test Procedure
1. Obtain swap
2. Use the swab with ascetic technique to obtain a sample of your culture, you want a lot. (only one side)
3. Smear part of the culture on the swab to a small area on a clean glass slide (for catalase)
4. Place swab upright in a test tube rack with the swab side pointing up (for oxidase)
5. Crush reagent ampule with finger, while pointing tip away from you or other people, but sure it is completely crushed and mixed
6. Squeeze 1-2 drops of the freshly mixed reagent onto the bacterial sample on the swabs, observe color change
- Purple: oxidase positive
- No color change: Oxidase negative
7. Fast catalase test: Use a small trader pipette to add a few drop of hydrogen peroxide solution directly on the bacteria
- Quick appearance of bubbling: Catalase positive
- No bubbles: Catalase negative