TMOD (Conjunctiva)
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
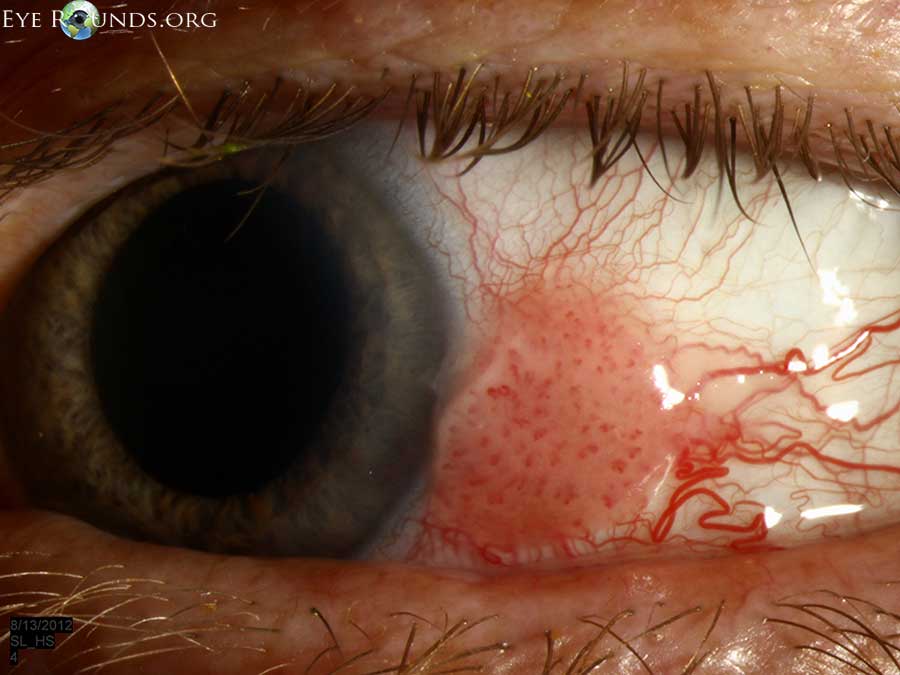
Pterygium
Fibrovascular growth destroying the Bowman’s layer
Related to chronic exposure to UV and ocular irritation (dry eye)
Induced WTR astigmatism
Pterygium Treatment/Management
Monitor
AT for comfort (PF if used >QID)
Educate to wear sunglasses
Surgical removal if enroaches across visual axis/reduces vision
If inflammation, tx with topical NSAID or steroid depending on severity
Pinguecula/Pingueculitis
Abnormal mounds of collagen on conj (never cornea)
Related to chronic UV exposure and ocular irritation (dry eye)
May be responsible for CL intolerence
Pinguecula/Pingueculitis Treatment/Management
Pinguecula
monitor
AT for comfort (PF if used >QID)
educate to wear sunglasses
surgical removal if AT doesn’t help
Pingueculitis
topical NSAID or mild steroid depending on severity

Cicatricial Pemphigoid
Usually in women >60yo
Autoimmune disease of the mucous membranes (ocular, oral, respiratory, genital tissues)
Type II hypersensitivity (drug-induced timolol, epinephrine, pilocarpine)
Inferior symblepharon, ankyloblepharon (connection of inferior and superior lid),discharge, hyperemia, keratitis, entropion, trichiasis, keratinization
Cicatricial Pemphigoid stages
Stage 1: chronic conjunctivitis with mild corneal involvement
Stage 2: cicatrization with conj shrinkage and foreshortening fornices
Stage 3: symblepharon, subepi scarring leading to distortion of lashes
Stage 4: ankyblepharon, severe corneal involvement (stromal ulcers, scarring, neo, diffuse keratinization)
Cicatricial Pemphigoid Treatment/Management
Systemic steroids or immunosuppressive agents
AT and punctal plugs
If present, tx corneal defects with antibiotics
Surgery may be needed for symblepharon, ankyloblepharon, entropion, trichiasis
Cicatricial Pemphigoid prognosis
Poor, chronic progressive disease and surgery often initiates exacerbations

Erythema Multiforme (Steven-Johnson Syndrome)
Caused by infection or poor rxn to medication (sulfonamides are most common)
Type III & IV hypersenitivity rxn
Target skin lesions/eruptions, symblepharon, ankyloblepharon, discharge, hyperemia, keratitis, entropion, trichiasis, keratinization
Early systemic signs
fever, malaise, HA, nausea/vomitting
Erythema Multiforme (Steven-Johnson Syndrome) Treatment/Management
AT and punctal plugs
If corneal defect, tx with antibiotics
If inflammation, tx with topical or oral steroids depending on severity
Surgery may be needed for symblepharon, ankyloblepharon, entropion, trichiasis
Amniotic membrane used in severe cases
Early systemic signs
fever, malaise, HA, nausea/vomitting
Erythema Multiforme (Steven-Johnson Syndrome) prognosis
Mortality in up to 30% of cases
Subconjunctival Hemorrhage
Bleeding under conj
Causee include increase intraorbital pressure: sneezing, coughing, straining, difficult bowel movement, or even HTN, aspirin/anticoagulant use or bleeding disorder (anemia or sickle cell)
Subconjunctival Hemorrhage Treatment/Management
No tx it will resolve in 2-3 weeks
Discontinue aspirin
If recurrent, refer to PCP to rule out bleeding disorder
Superior Limbic Keratoconjunctivitis (SLK)
When superior lid chafes the superior bulbar conj
friction caused by thyroid disease, dry eye, excessive CL wear
FB sensation, pain, burning (complaints outweigh signs)
Presents with inflammation and hyperemia and will stain with NaFl and filaments may also be present
Superior Limbic Keratoconjunctivitis (SLK) Treatment/Management
Tx underlying condition
1st line of tx is excessive use of AT and punctal plugs
If severe, silver nitrate can be applied for 10-20 seconds and then rinsed with saline then 1 week of antibiotic ointment
If filaments, tx with topical acetylcysteine
SLK due to CL responds well to steroids (but not SLK due to TED)
FU 2-4 weeks
Allergic Conjunctivitis
Type I hypersensitivity rxn
Complaint of itchy, watery eyes
Presents with papillae and possible chemosis
2 Types of Allergic Conjunctivitis
1.Seasonal Allergic Conjunctivitis
most common type
pollen and hay fever
2.Perennial Allergic Conjunctivitis
year round
dust and dander
Allergic Conjunctivitis Treatment/Management
Topical antihistamines and or steroids depending on severity
Coll compresses several times per day
For severe cases, FML for 2 days then QID for 1 week then taper then can switch to antihistamines and follow up in 2 weeks if steroids are used
Atopic Conjunctivitis
Associated with atopic dermatitis/eczema, allergic rhinitis, asthma - hereditary predilection for allergic disease
Complaint of itchy, watery eyes, photobia, pain
Presents with papillae and possible chemosis, symblepharon, neo, keratoconus, cataract
Concurrently seen with Atopic Dermatitis - Dennies lid
Atopic Conjunctivitis Treatment/Management
Topical antihistamines and or steroids depending on severity
Coll compresses several times per day
For severe cases, FML for 2 days then QID for 1 week then taper then can switch to antihistamines and follow up in 2 weeks if steroids are used

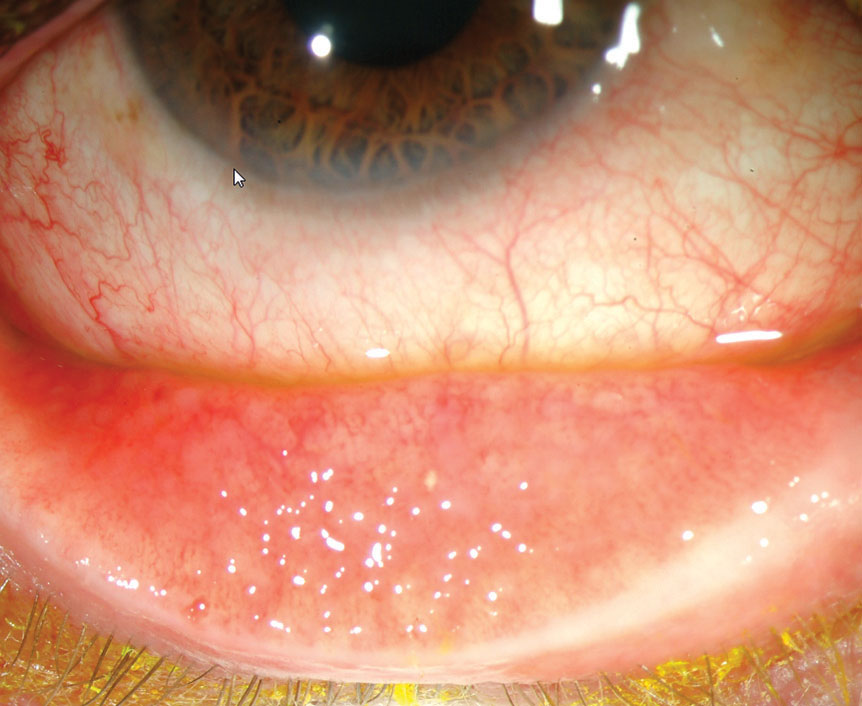
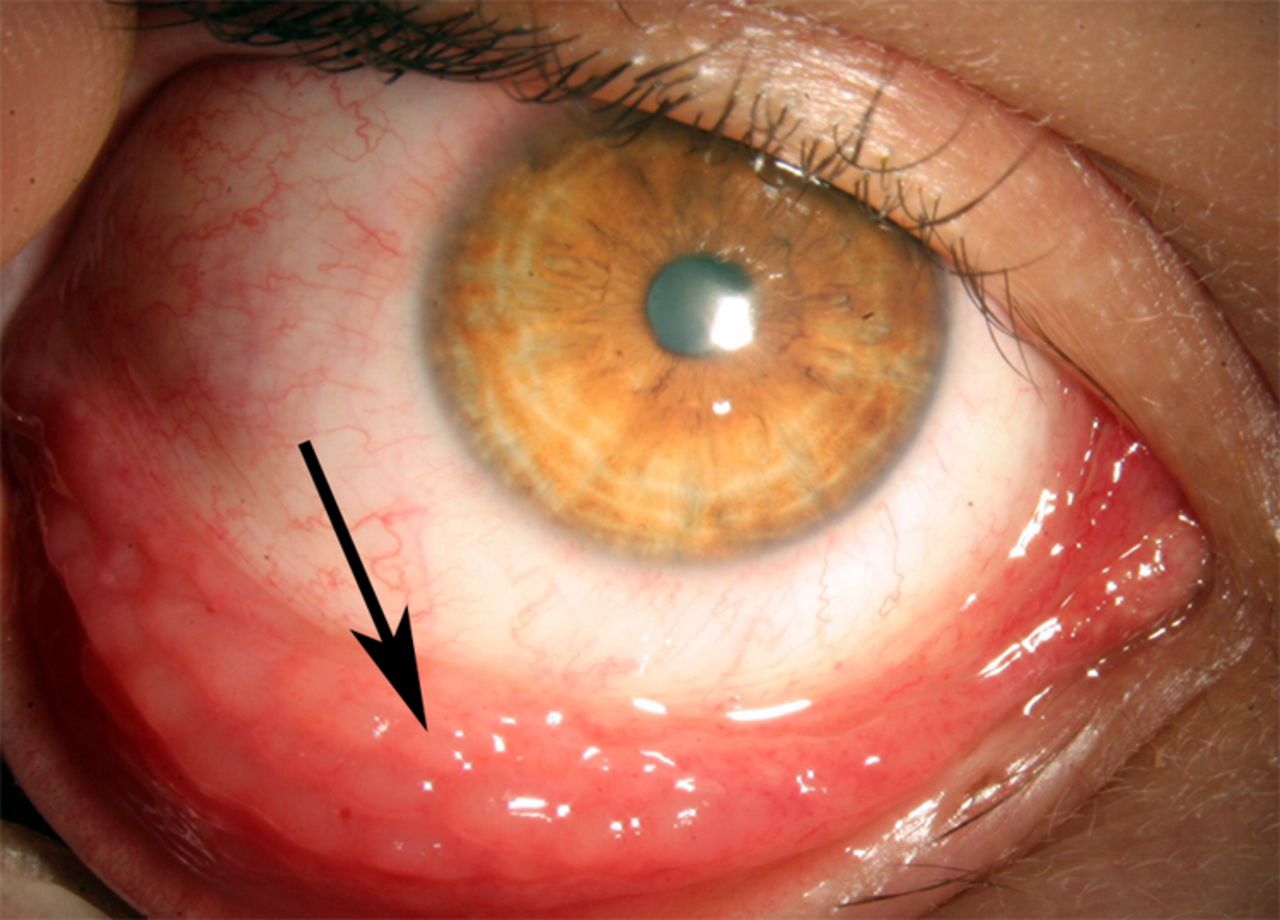
Vernal Conjunctivitis
Rare anomaly seen in boys under 10yo in hot climates and predilection for atopy
Outbreaks decrease in severity over time and resolve during puberty
Complaint of itchy, watery eyes, photobia, pain
Presents with papillae and possible chemosis, thick ropy discharge, Horner-Trantas dots (eosinophils), shield ulcer (sterile, superiorly located, well-delineated, grey infiltrate), large cobblestones in superior palpebral conj
Vernal Conjunctivitis Treatment/Management
Topical antihistamines and or steroids depending on severity
Coll compresses several times per day
For severe cases, FML for 2 days then QID for 1 week then taper then can switch to antihistamines and follow up in 2 weeks if steroids are used
Shield ulcer, tx with antibiotics and cyclo (if severe, oral antibiotics and steroid (after infection has cleared)
FU daily
Bacterial Conjunctivitis (non-gonococcal)
Most commonly caused by G+ bacteria (Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis)
Most common cause of conj in children <3yo
Knows when it occurred but not exact time
History of recent cold
Mucopurulent discharge, hyperemia, papillae, chemosis, papillae, lid swelling, NO corneal involvement and NO lymphadenopathy
Bacterial Conjunctivitis (non-gonococcal) Treatment/Management
Topical antibiotic
adults - fluoroquinalone, polytrim, tobramycin
children - polytrim or polysporin

Gonococcal Conjunctivitis
STI
Caused by Neisseria gonorrhoeae (which can attack intact corneal epithelium; along with Canadian-Corynebacterium Hockey-Haemophilus League-Listeria)
HYPERACUTE - knows the exact second it occurs
Presents with severe mucopurulent discharge, hyperemia, chemosis, papillae, lid swelling, pseudomembrane, +lymphadenopathy, may also have corneal ulcers typically superior (bacteria is attacking corneal epi and causing infectious keratitis)
Unilateral then bilateral
Gonococcal Conjunctivitis Treatment/Management
IM ceftriaxone (if cornea is not involved
IV ceftriaxone (if cornea is involved) and hospitalized
Fluoroquinolones (if PCN or cephalosporin allergy) and refer to infectious specialist
Evaluate for chlamydia also
Can send conj scrapings for immediate gram stain and culture (chocolate agar or thayer-martin agar)
G- diplococci
FU daily until improvement is noted then every 2-3 days until condition is resolved
Tx sexual partners with oral antibiotics

Ophthalmia Neonatorum (Newborn Conjunctivitis)
Develops within 4 days after birth (Neisseria gonorrhoeae is most common)
HYPERACUTE - knows the exact second it occurs
Presents with severe mucopurulent discharge, hyperemia, chemosis, papillae, lid swelling, pseudomembrane, +lymphadenopathy, may also have corneal ulcers typically superior (bacteria is attacking corneal epi and causing infectious keratitis)
Ophthalmia Neonatorum (Newborn Conjunctivitis) Treatment/Management
Erythromycin ointment prophylactically
If infection develops, give IM or IV ceftriaxone
Adult Inclusion Conjunctivitis (Chlamydial Conjunctivitis)
Chronic conjunctivitis, can last up to 12 months without treatment
Serotypes D-K
Large follicles inferior palpebral conj (even though bacterial infection), papillae, stringy mucous discharge, tender, +PAN palpable preauricular nodes
Adult Inclusion Conjunctivitis (Chlamydial Conjunctivitis) Treatment/Management
Single does of oral Azithromycin then oral doxycycline, erythromycin, or tetracycline for 1-2 weeks
FU every 2-3 weeks until resolution
Tx sexual partners with oral antibiotics
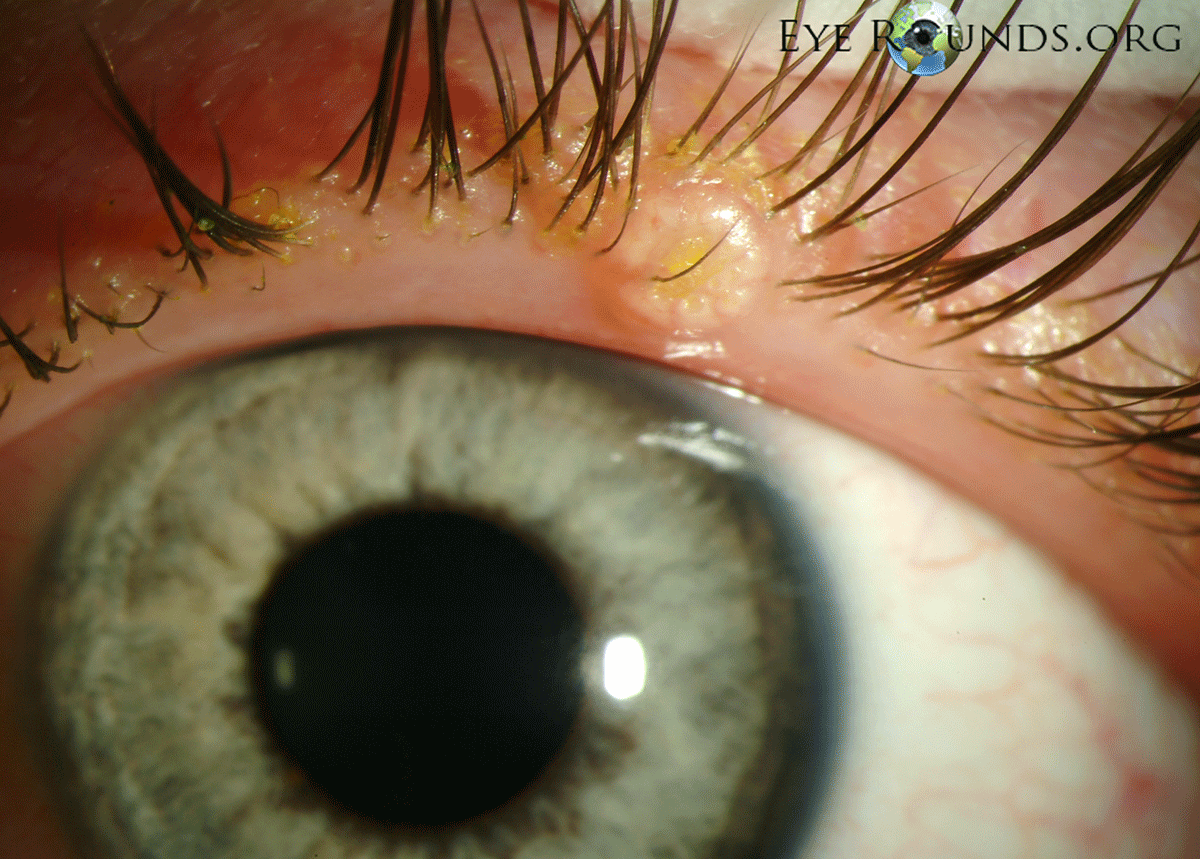
Trachoma (Chlamydial Conjunctivitis)
Chronic, can last up to 12 months without treatment
Serotypes A-C
Leading cause of preventable blindnessin the world
Follicles in superior palpebral conj (even though bacterial infection), papillae, stringy mucous discharge, tender, +PAN palpable preauricular nodes, Herpert’s pits (indentation from follicles), Arlt lines
Trachoma (Chlamydial Conjunctivitis) Treatment/Management
Single does of oral Azithromycin then oral doxycycline, erythromycin, or tetracycline for 1-2 weeks
FU every 2-3 weeks until resolution
Tx sexual partners with oral antibiotics

Adenoviral Conjunctivitis (Viral Conjunctivitis)
Most common cause of “pink eye” or viral conjunctivitis
Highly contagious for 14 days (via contact)
History of recent cold
FB sensation, Itching, burning, gritty feeling, follicles, +lymphadenopathy, serous discharge, hyperemia, lid edema
3 Types of Adenoviral Conjunctivitis (Viral Conjunctivitis)
1.Nonspecific
most common
2.Epidemic Keratoconjunctivitis
SEIs (2-3 wks after onset = no longer contagious)
severe pain
remember rule of 8 (serotype 8, symptoms after 8 days, SEI 8 days after symptoms)
3.Pharyngoconjunctival fever
swimming poool conjunctivitis
fever + sore throat + follicular conj
Adenoviral Conjunctivitis (Viral Conjunctivitis) Treatment/Mangement
FU 2-3 wks
Educate on contagious nature and avoid contact with others, also to clean bedsheets and towels
Mild/mod: Self resolves, can rec cool compresses & PF ATs
Severe: lotemax with taper
Molluscum Contagiosum
DNA pox virus spread via direct contact
Domes shaped umbilicated shiny nodules and lid margin (if multiple, HIV may be underlying etiology) & ruptured nodules lead to pannus and chronic conjuctivitis
Molluscum Contagiosum Treatment/Management
Excision, curettage, cryotherapy
Refer for HIV testing (Western Blot & ELISA)
Conjunctival Intraepithelial Neoplasia (CIN) → Squamous Cell Carcinoma
CIN is a precursor to SCC (most common conj malignancy in the US)
Usually in elderly caucasian males with heavy smokers, UV radiation, HPV
If <50yo, suspect HIV
Ocular irritation, FB sensation, dry eye
CIN appears as white, gelatinous dysplasia
SCC is a peripapillary, gelatinous lesion with abnormal loops of vessels
Conjunctival Intraepithelial Neoplasia (CIN) → Squamous Cell Carcinoma Treatment/Management
Refer for medical work up and MRI ot rule out invasion
Excision with biopsy, exenteration (remove globe and all contents of the eye socket), radiation
If recurrent, topical interferon alpha-2beta, mitomycin C (DNA synthesis inhibitor), or 5-fluorouracil can be consider
Conjunctival Intraepithelial Neoplasia (CIN) → Squamous Cell Carcinoma prognosis
Metastasis and orbital invasion is rare for SCC but mortality is 8%
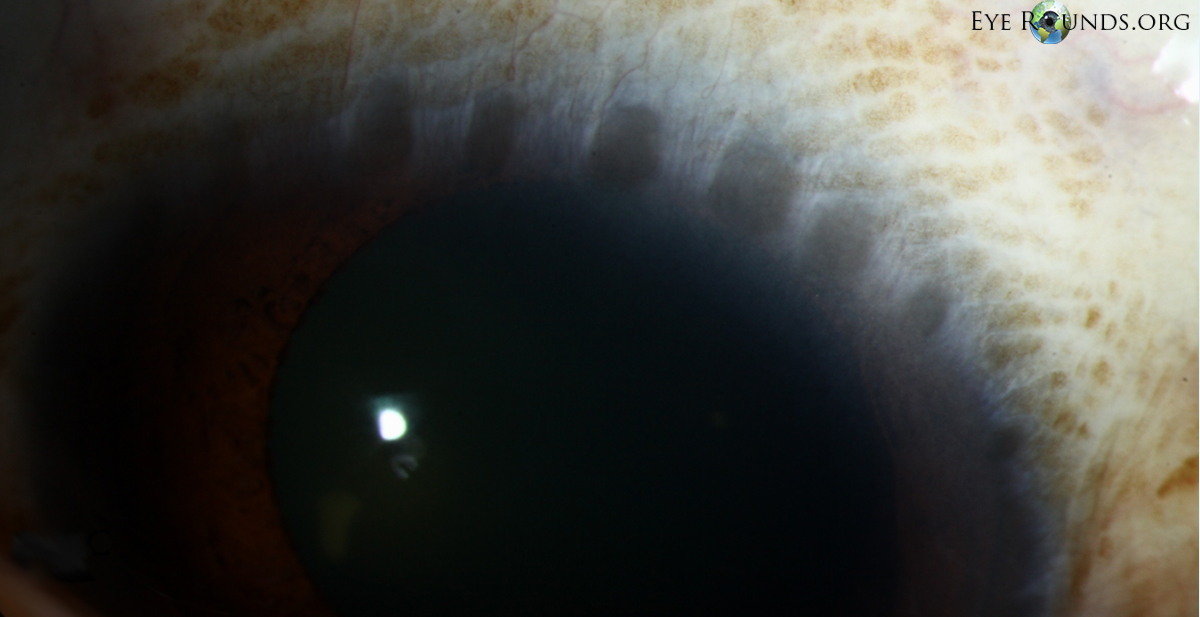
Primary Acquired Melanosis (PAM) → Malignant Melanoma
70% of Malignant Melanoma comes from PAM
Unilateral and mostly middle-aged caucasians
1st area of metastasis of malignant melanoma is the parotid and/or submandibular lymph nodes
Primary Acquired Melanosis (PAM) → Malignant Melanoma Treatment/Management
PAM - monitor with photos
Malignant Melanoma - excisional biopsy, cryotherapy, corneal epitheliectomy, exenteration (depending on severity)
If recurrent, tx with topical mitomycin C
Primary Acquired Melanosis (PAM) → Malignant Melanoma prognosis
Malignant Melanoma has a 45% mortality rate