Chapter 29: Cardiac PT Care
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
Age-Related Cardiovascular Changes: Arterial Stiffening
- Large arteries (aorta) lose elasticity and become stiffer = higher systolic BP, wider pulse pressure (isolated systolic HTN common).
- ↑ systolic blood pressure / widened pulse pressure.
- Nursing care: BP & Fall Risk
Age-Related Cardiovascular Changes: LV Structural Changes
- hypertrophy and decreased compliance → diastolic dysfunction.
- LV walls thicken and relax more slowly; filling (diastole) is impaired even if ejection fraction is preserved. This predisposes to heart failure with preserved EF.
- Nursing implication: older adults may develop exertional dyspnea and pulmonary congestion with normal EF; monitor fluid status and activity tolerance.
What will decreased Maximal HR and reduced cardiac reserve result in for older adults?
- HR and the ability + CO with exercise decline.
- Nursing implication: older patients may have blunted HR response to activity/stress — use perceived exertion and watch for atypical symptoms.
What changes occur in the cardiac system with age?
- Pacemaker cells die out → ↑ arrhythmia risk (e.g., atrial fibrillation).
- SA node cell number falls and conduction tissue fibrosis increases susceptibility to brady-, heart block, and AF.
- Nursing implication: monitor ECGs, pulse irregularities, and med effects (e.g., beta blockers, digoxin)
Age-Related Cardiovascular Changes: Valve thickening and calcification
= aortic stenosis or contribute to valvular dysfunction.
- Nursing implication: listen for new murmurs; consider activity limits and referral for echo if symptomatic.
What does Increased peripheral vascular resistance and atherosclerotic changes in older adults mean?
- Vessel walls thicken, lumens narrow, and atherosclerosis incidence rises lead to an increased risk of CAD, PAD, stroke.
- Nursing implication: risk-factor management (lipids, smoking, diabetes control) and vascular assessments.
Age-Related Cardiovascular Changes: Decreased baroreceptor sensitivity
- orthostatic hypotension risk.
- Autonomic reflexes are blunted so BP and HR respond less effectively to position changes.
- Nursing implication: orthostatic BP checks, slow position changes, fall prevention.
What can low responsiveness to beta-adrenergic stimulation and stress hormones result in?
Reduced responses to inotropic and chronotropic drugs
- Nursing implication: expect smaller HR/BP changes after meds or stress; be cautious with drugs that further alter autonomic tone.
What does an increased tendency for thrombus formation/coagulation mean for older adults?
More clotting means increased risk for stroke/venous thromboemoblism
- -Nursing implication: assess VTE/stroke risk, prophylaxis when indicated, and monitor anticoagulation carefully.
What does a decreased exercise tolerance and increased symptom threshold for ischemia mean for older adults
change in symptoms when experiencing ischemia = (watch for fatigue, syncope, confusion) rather than classic chest pain.
- Nursing implication: maintain high suspicion for ischemia with nonspecific symptoms; timely assessment and diagnostics.
Additional Age-Related Cardiovascular Changes
- Increased collagen and fat in the heart wall
- Reduced heart contractility and response to stress
Left-Sided HF VS Right-Sided HR
- Right-Sided: Swelling Edema = Congestion of peripheral tissues
- Left-Sided: Pulmonary = - CO and + Pulmonary Congestion
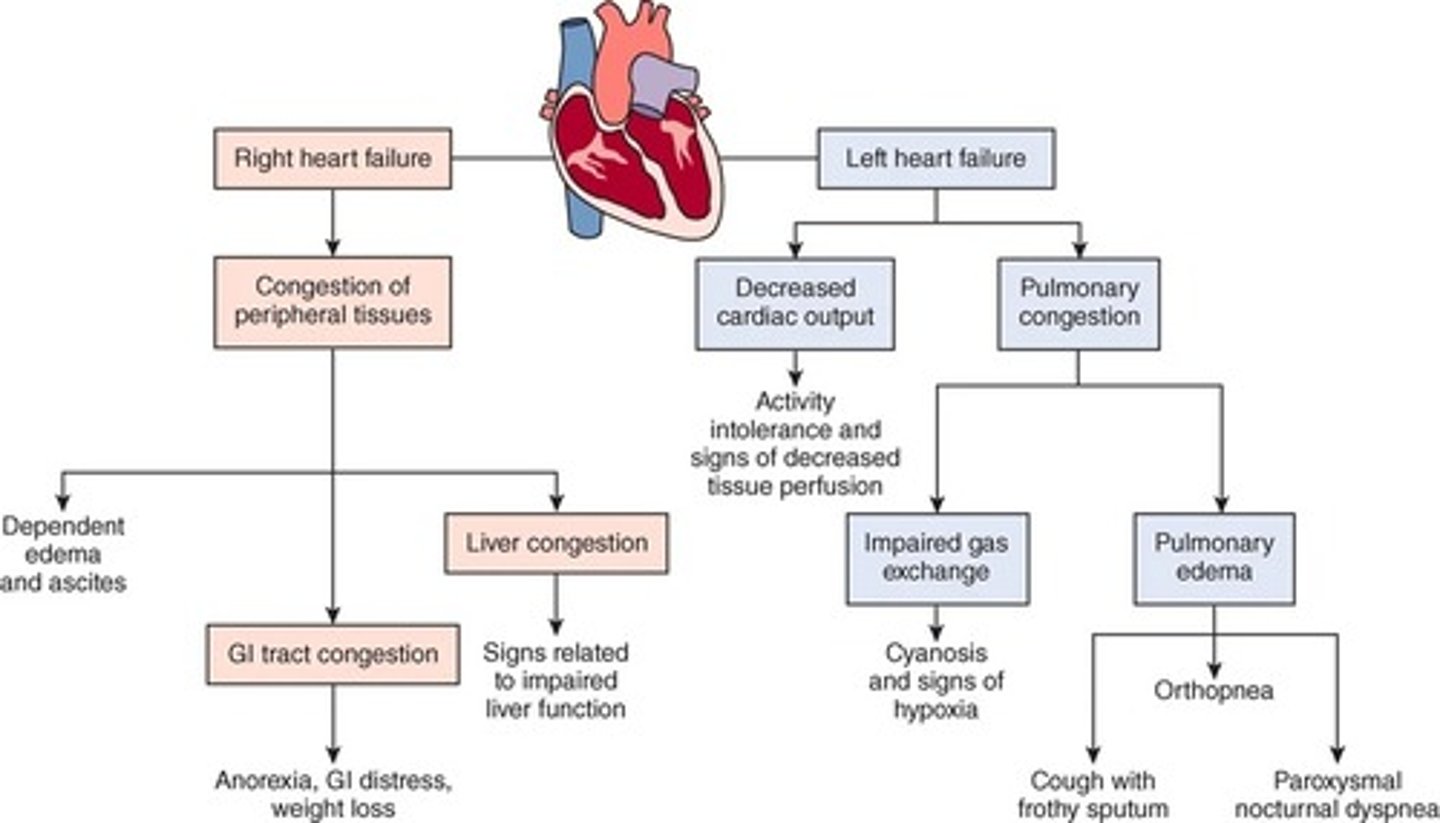
Left HF: Decreased CO leads to…
Activity intolerance and signs of decreased tissue perfusion
Left HF: Pulmonary Congestion leads to..
- Impaired Gas Exchange
- Pulmonary Edema
What will Left HF: Impaired Gas Exchange result in?
Cyanosis and signs of hypoxia
What will Left HF: Pulmonary Edema result in?
- Cough with frothy sputum
- Orthopnea
- Paroxysmal noctural dyspnea
Right HF: Congestion of peripheral tissues leads to....
- Dependent edema and ascities
- GI tract congestion
- Liver congestion
what will Right HF: GI Tract Congestion result in?
Anorexia, GI distress, wt loss
Signs of Right HF: Liver Congestion
nausea, vomiting, itchiness, and jaundice (yellowing of eyes/skin), followed by reduced appetite, fluid retention (ascites), and bleeding/clotting problems
Left HR Assessment
- Assess activity tolerance by asking whether the patient can perform normal ADLs or climb flights of stairs without fatigue or dyspnea.
- Ask about their ability to perform simultaneous arm and leg work (e.g., walking while carrying a bag of groceries).
What might a patient report due to LV failure?
- chest pain, palpitations, skipped beats, or a fast heartbeat.
- Perfusion to the myocardium is often impaired as a result of left ventricular failure, especially with cardiac hypertrophy.
- Dyspnea
How would a patient in early LHF describe their cough?
As irritating, nocturnal (at night), and usually nonproductive
What changes with a cough in severe LHF?
May come with frothy, pink-tinged sputum
Why does dyspnea occur with LHF?
- results from increasing pulmonary venous pressure and pulmonary congestion.
- Carefully question about the presence of dyspnea and how it developed.
- The patient may refer to dyspnea as "trouble catching my breath," "breathlessness," or "difficulty breathing."
Exertional Dyspnea
Shortness of breath during physical activity.
Orthopnea
Difficulty breathing when lying down (at rest)
What is paroxysmal Nocturnal Dyspnea
-sudden awakening with a feeling of breathlessness 2 to 5 hours after falling asleep
- Sitting upright, dangling the feet, or walking usually relieves this condition.
Signs of RHF
- Edema develops in the lower legs and may progress to the thighs and abdominal wall.
- Patients may notice that their shoes fit more tightly, or their shoes or socks may leave indentations on their swollen feet.
- They may have removed their rings because of swelling in their fingers and hands.
- Ask about weight gain.
- Nausea and anorexia
An adult may retain ____ to ____ L of fluid (10-15 lb [4.5-6.8 kg]) before pitting edema occurs.
4 to 7L
What symptom occurs in advanced HF?
- Ascites & increased abdominal girth may develop from severe liver congestion.
- fluid retention due to diuresis
- At rest, fluid in the peripheral tissue is mobilized and excreted, and the patient describes frequent awakening at night to urinate.
Signs/Symptoms of LHF
• Weakness
• Fatigue
• Dizziness
• Acute confusion
• Pulmonary congestion
• Breathlessness
• Oliguria (scant urine output)
what is Pulus Alternans
Alternating weak and strong beats and a regular rhythm
Nocturia
Excessive urination at night
What needs to be monitored (respiratory) with HF?
- Carefully monitor the patient's respiratory rate, rhythm, and character, as well as oxygen saturation.
- The respiratory rate typically exceeds 20 breaths/min.
Key Features of LV HF: Decreased CO
• Fatigue
• Weakness
• Oliguria during the day (nocturia at night)
• Angina
• Confusion, restlessness
• Dizziness
• Tachycardia, palpitations
• Pallor/Ash gray skin
• Weak peripheral pulses
• Cool extremities
Key Features of LV HF: Pulmonary Congestion
• Hacking cough, worse at night
•Dyspnea/breathlessness
• Crackles or wheezes in lungs
• Frothy, pink-tinged sputum
• Tachypnea
• S3/S4 summation gallop
Key Features of RV HF
• Systemic congestion
• Jugular (neck vein) distention
• Enlarged liver and spleen
• Anorexia and nausea
• Dependent edema (legs and sacrum)
• Distended abdomen
• Swollen hands and fingers
• Polyuria at night
• Weight gain
• Increased blood pressure (from excess volume) or decreased blood pressure (from failure)
What's the FIRST sign of HF?
A third heart sound, S3 gallop, is an early diastolic filling sound indicating an increase in left ventricular pressure
What lung sounds indicated HF?
Late inspiratory crackles and fine profuse crackles that repeat themselves from breath to breath and do not diminish with coughing
- Wheezing
What produces crackles in HF?
intraalveolar fluid and are often noted first in the bases of the lungs and spread upward as the condition worsens.
what is wheezing caused by?
bronchial lumen are narrowed, caused by engorged pulmonary vessels.
What can be assessed for RHF?
- On inspection, assess the neck veins for distention and measure abdominal girth.
- Hepatomegaly (liver engorgement), hepatojugular reflux, and ascites may also be assessed.
- When the fluid accumulates in the abdomen, pressure is placed on the stomach and intestines. This pressure can lead to early satiety and malnutrition.
- Assess for dependent edema. In ambulatory patients, edema commonly presents in the ankles and legs. When patients are restricted to bed rest, the sacrum is dependent and fluid accumulates there.
Psychosocial Assessment for HF
- At high risk for depression
- Assess patients and their families for anxiety and depression.
-Ask them about their usual methods of coping and any history of depression.
- If anxiety or depression is present, notify the primary health care provider for further assessment.
- Ask patients about their daily activities and how often they interact with the significant people in their life to help determine patient and family coping strategies.
Laboratory Assessment for HF
- Serum Electrolytes
- BUN
- Serum creatinine
- H&H
- B-type natriuretic peptide (BNP)
- Urinalysis
- ABG
In particular, what type of HF is diagnosed from B-type natriuretic peptide (BNP)?
Diastolic
Microalbuminuria
- Early indicator of decreased compliance of the heart and occurs before the BNP rises.
- It serves as an "early warning detector" that lets the primary health care provider know that the heart is experiencing early signs of decreased compliance long before symptoms occur.
Imaging Assessment for HF
- Chest x-ray
- Echo
- Radionuclide studies
- MUGA scans / multigated blood pool scans
Cardiomegaly
Enlargement of the heart, typically representing hypertrophy or dilation
Other Diagnostic Assessments for HF
- ECG
- Invasive hemodynamic monitoring
- Pulmonary artery pressure (PAP) (elevated in LHF)
- pulmonary artery occlusion pressure (PAOP) (elevated in LHF)
Analysis for HF
1. Decreased gas exchange due to ventilation/perfusion imbalance
2. Potential for decreased perfusion due to inadequate cardiac output
3. Potential for pulmonary edema due to left-sided HF
How do we increase gas exchange in HF pts?
- Ventilation assistance
- Monitor RR e/4 hours
- Auscultate breath sounds every 4 - 8 hours.
Interventions for HF: Increasing Perfusion
Collaborative care begins with nonsurgical interventions, but the patient may need surgery if these are not successful in meeting optimal outcomes.
What nonsurgical treatment can we giev to HF patients?
angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs).
function of Angiotension receptor neprilysin inhibitor (ARNI)
increase natriuretic peptides while suppressing the RAAS
Nutrition for HF pts?
- reduce sodium
- omit table salt (no added salt) = about 3 g daily.
- no ham, bacon, pickles
common drugs for HF pts?
diuretics
venous vasodilators
Morphine sulfate (reduce anxiety, decrease preload and afterload, slow respirations, and reduce pain associated with a myocardial infarction (MI)
Potassium-sparing diuretic, venous vasodilators (e.g., nitrates)
Nonsurgical Management for HF: Digoxin
- Digoxin, a cardiac glycoside, has been demonstrated to provide symptomatic benefits for patients in chronic heart failure (HF) with sinus rhythm and atrial fibrillation.
- Digoxin is absorbed from the GI tract erratically.
Nonsurgical Management for HF: Beta-Adrenergic Blockers
- Beta-adrenergic blockers (commonly referred to as beta blockers) improve the condition of some patients with HF.
- Prolonged exposure to increased levels of sympathetic stimulation and catecholamines worsens cardiac function. Beta-adrenergic blockade reverses this effect, improving morbidity, mortality, and quality of life for patients with HF.
Nonsurgical Management for HF: Aldosterone Antagonists
- Aldosterone antagonists (spironolactone or eplerenone) can reduce symptoms associated with HF and may be added to HF therapy in patients who remain symptomatic while taking an angiotensin-converting enzyme inhibitor (ACEI) and a beta blocker
- Aldosterone antagonists decrease the risk for dysrhythmias from hypokalemia
Nonsurgical Management for HF: HCN Channel Blocker
- Ivabradine is a first-in-class hyperpolarization-activated cyclic nucleotide-gated (HCN) channel blocker that slows the heart rate by inhibiting a specific channel in the sinus node.
- It has been shown to reduce the risk of hospitalization in patients with HF.
Nonsurgical Management for HF: Sodium-glucose Contransporter-2 inhibitor agents
- In the most recent heart failure guidelines, the recommendation for use of SGLT2i drugs (canagliflozin, empagliflozin) was included.
- This drug class was developed to treat type 2 diabetes mellitus. However, evidence shows a significant decrease in hospitalizations and mortality, as well as improved renal function in patients with HF.
Other Nonsurgical Management for HF
• Continuous positive airway pressure (CPAP)
• Cardiac resynchronization therapy (CRT)
• CardioMEMS implantable monitoring system
• Investigative gene therapy
Surgical Management for HF: Ventricular Assist Devices
- Patients with debilitating end-stage heart failure are often sent home on drug therapy and referred to hospice. However, ventricular assist devices (VADs) can dramatically improve the lives of many patients.
- For these patients, the VAD is considered destination therapy, meaning they will have the device for the rest of their lives.
Other Surgical Therapies for HF
Endoventricular circular patch cardioplasty
- Left ventricular surgical reconstruction
-
Expected Outcomes for Pulmonary Edema
- The most desirable outcome is that the patient will not develop pulmonary edema as a result of heart failure (HF).
- Monitor for signs of acute pulmonary edema, a life-threatening event that can result from severe HF (with fluid overload), acute myocardial infarction (MI), mitral valve disease, and possibly dysrhythmias
Key Features of Pulmonary Edema
• Crackles
• Dyspnea at rest
• Disorientation or acute confusion (especially in older adults as early symptom)
• Tachycardia
• Hypertension or hypotension
• Reduced urinary output
• Cough with frothy, pink-tinged sputum
• Premature ventricular contractions and other dysrhythmias
• Anxiety
• Restlessness
• Lethargy
Care Coordination and Transition Management for HF
- Patients who are not adequately prepared for discharge or do not have adequate community support and follow-up for self-management are at high risk for repeated hospital admissions for heart failure (HF).
- Two interventions have been shown to reduce readmission rates: early and intensive nursing care (at least one visit on the day of discharge and at least three nursing visits in the first posthospital week) and follow-up with the health care provider within 1 week of discharge.
Home Care Management for HF
- interventions focus on assessment and health teaching, which are reimbursable by Medicare and other third-party payers.
- They must adhere to the collaborative plan of care that includes dietary restrictions, activity, prescriptions, and drug therapy. They need careful, concise explanations of the self-management plan.
Self-Management Education for HF
- One standardized and commonly used self-management plan called MAWDS
- Ambulatory care clinics for patients with HF are also becoming increasingly common. Their purpose is to offer assessments, drug therapy, and health teaching.
Activity Schedule for HF
- Encourage patients with HF to stay as active as possible and to develop a regular exercise regimen (e.g., home walking program).
- Remind patients with persistent crackles and uncontrolled edema to begin exercise after their condition stabilizes. When exercise is indicated, teach the patient to begin walking 200 to 400 feet per day.
Advance Directives for HF
- HF is a chronic, progressive debilitating disease.
-The only potential cure is transplantation.
- Early in the diagnosis stage, patients and families should be made aware of the progressive nature of this disease process. About 50% of deaths from HF are sudden—many without any warning or worsening of symptoms.
Health Care Resources for HF
- A home care nurse, ambulatory care clinic, or nurse-led follow-up program may be needed to assess the patient's adherence to drug and nutrition therapy and to monitor for worsening or recurrent HF
- The American Heart Association (AHA) is an excellent community resource for educational information related to HF and heart disease.
Evaluation for HF
• Have adequate pulmonary tissue perfusion
• Have increased cardiac pump effectiveness
• Be free of pulmonary edema
MAWDS
medications, activity, weight, diet, symptoms
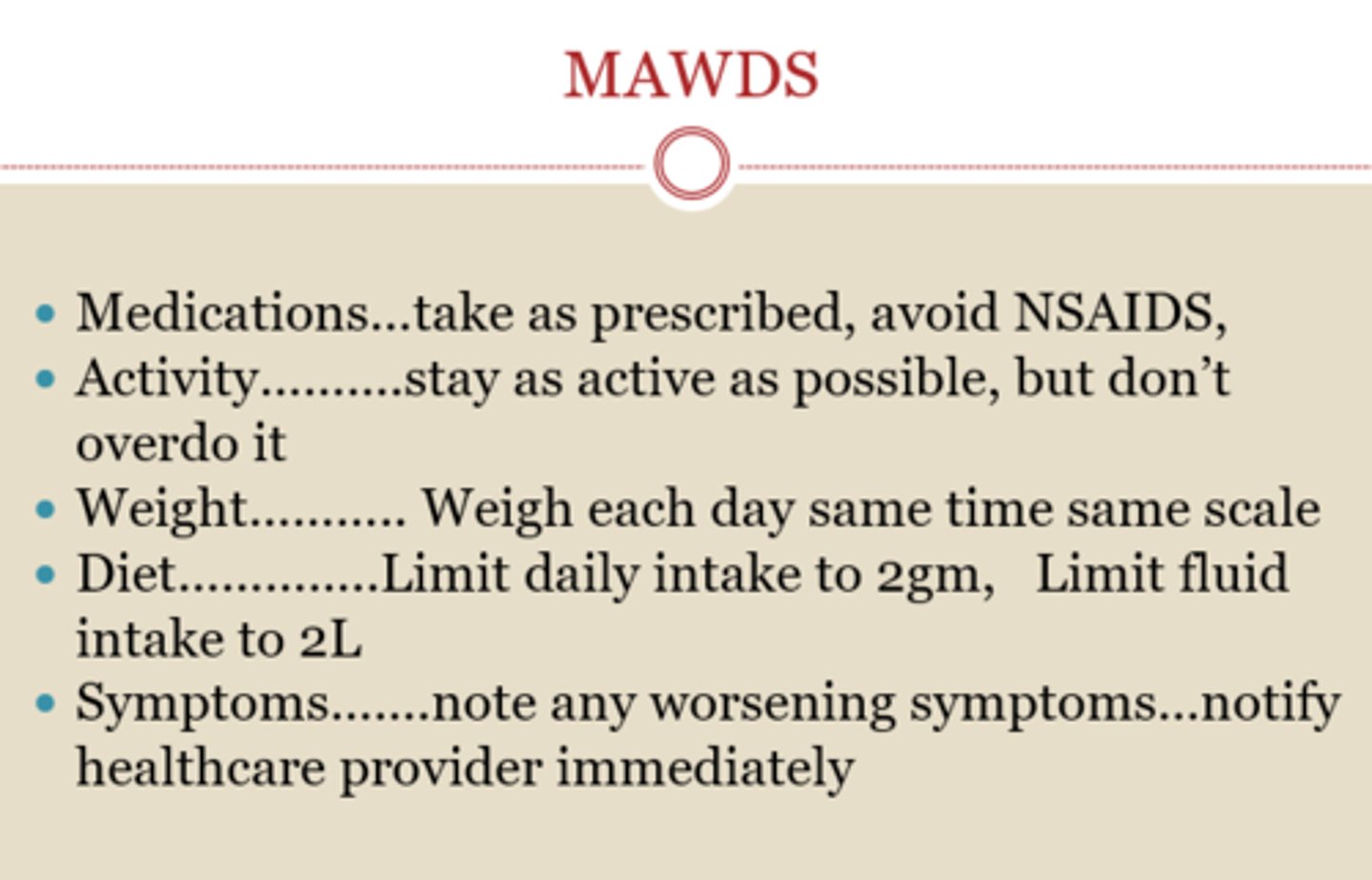
MAWDS: Medications
• Take medications as prescribed and do not run out.
• Know the purpose and side effects of each drug.
• Avoid NSAIDs to prevent sodium and fluid retention.
MAWDS: Activity
• Stay as active as possible but don't overdo it.
• Know your limits.
• Be able to carry on a conversation while exercising.
MAWDS: Weight
Weigh each day at the same time on the same scale to monitor for fluid retention.
MAWDS: Diet
• Limit daily sodium intake to 2 to 3 g as prescribed.
• Limit daily fluid intake to 2 L.
MAWDS: Symptoms
Note any new or worsening symptoms and notify the health care provider immediately.
RAAS
- Renin-angiotensin system (RAS) activation (also called renin-angiotensin-aldosterone system activation)
- Angiotensin receptor neprilysin inhibitors work with valsartan and sacubitril to increase natriuretic peptides while suppressing the RAAS
What results in activation of RAAS?
Reduced blood flow to thekidneys, a common occurrencein low-output states,
RAAS (from slide)
- Reduced blood flow to thekidneys, a common occurrencein low-output states, results inactivation of the renin-angiotensin system (RAS).
- Vasoconstriction becomesmore pronounced in response to angiotensin II, andaldosterone secretion causes sodium and water retention.
- Preload and afterload increase (due to fluid/salt ret.
- Angiotensin II contributes toventricular remodeling,resulting in progressivemyocyte (myocardial cell) contractile dysfunction overtime
What is the most common cause of mitral stenosis?
Rheumatic Fever
Rheumatic Fever Signs and Symptoms
- Tachycardia
- Cardiomegaly (enlarged heart)
- Development of a newmurmur or a change in an existing murmur
- Pericardial friction rub
- Precordial pain
- ECG changes (prolonged PR interval)
- Indications of HF
- Evidence of an existing streptococcal infection
-Penicillin or erythromycin tx of choice
Teach all patients..... (Rheumatic fever)
Teach all patients to remind their primary health care providers to provide appropriate antibiotic therapy if they develop the indications of streptococcalpharyngitis:• Moderate to high fever
• Abrupt onset of a sore throat
• Reddened throat with exudate
• Enlarged and tender lymph nodes
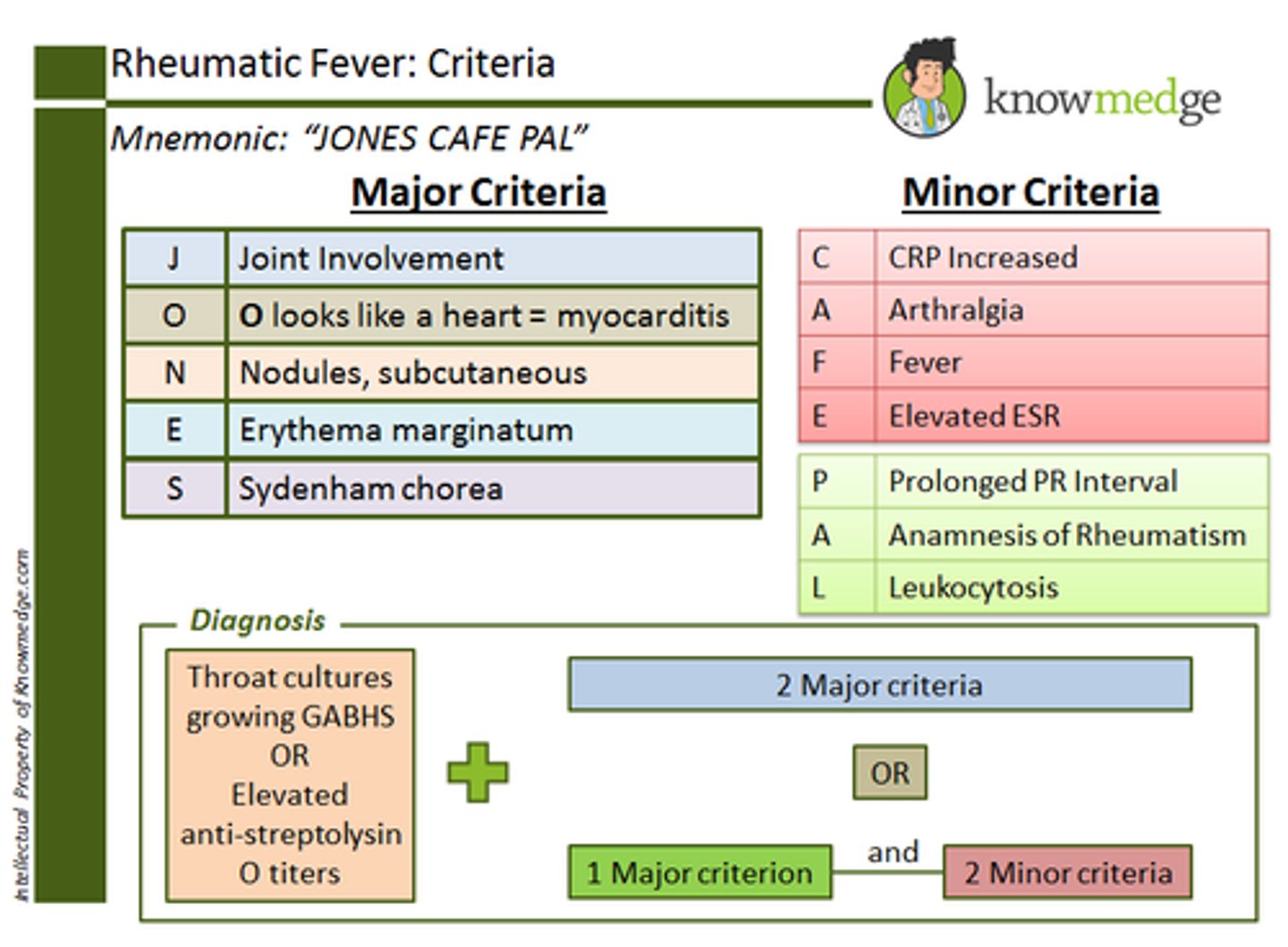
Diagnosis Criteria for Rheumatic Fever: JONES CAFE PAL
- Joint Involvement
- O looks like a heart = myocarditis
- Nodules, subcutaneous
- Erythema marginatum
- Sydenham chorea
- CRP Increased
- Arthalgia
- Fever
- Elevated ESR
- Prolonged PR Interval
- Anamnesis of rheumatism
- Leukocytosis
Infective Endocarditis
- A microbial infection (e.g., viruses, bacteria, fungi) involving the endocardium.
- Can occur in those who use IV drugs
Physical Assessment/Signs and Symptoms of Endocarditis
- Development of heart failure
- Evidence of systemicembolization
- Petechiae
- Splinter hemorrhages
- Osler nodes (on palms ofhands and soles of feet)
- Janeway lesions (flat,reddened maculae on handsand feet)
- Roth spots (Hemorrhagiclesions that appear as roundor oval spots on the retina)
- Positive blood cultures
Nonsurgical Management of Endocarditis
- The major component of treatment for endocarditis is drug therapy. Other interventions help prevent the life-threatening complications of the disease.
- Antimicrobials are the main treatment, with the choice of drug depending on the specific organism involved.
Surgical Management of Endocarditis
• Removing the infected valve (either biologic or prosthetic)
• Repairing or removing congenital shunts
• Repairing injured valves and chordae tendineae
• Draining abscesses in the heart
Diagnostic Assessment of Endocarditis
- Positive blood culture
- Transesophageal echocardiography (TEE)
What's a classic sx with renal infarction?
Flank pain
Petechiae
small, pinpoint hemorrhages

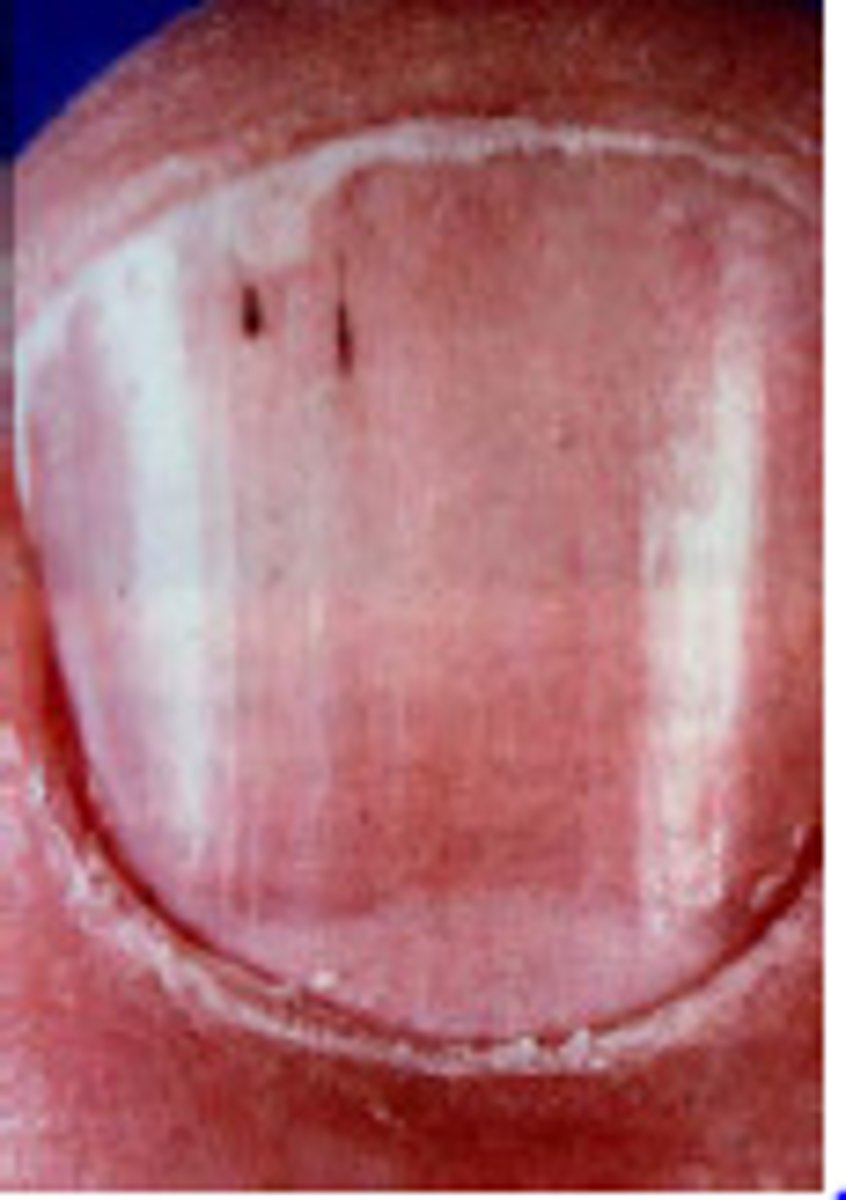
Splinter Hemorrhages
Appear as black longitudinal lines or small red streaks.
Most patients with Endocarditis have _____________?
Recurrent fevers from 99°F to 103°F (37.2°C to 39.4°C).
Possible ports of entry for infecting organisms of Infective Endocarditis
• The oral cavity (especially if dental procedures have been performed)
• Skin rashes, lesions, or abscesses
• Infections (cutaneous, genitourinary, GI, systemic)
• Surgery or invasive procedures, including IV line placement
Pulmonary Edema
Condition caused by too much fluid in the lungs. This fluid collects in the many air sacs in the lungs, making it difficult to breathe.
Mitral Stenosis
Thickening of the mitral valve due to fibrosis and calcification. The valve leaflets fuse and become stiff, and the valve opening narrows, which prevents normal blood flow from the left atrium to the left ventricle.
Mitral stenosis usually results from _____ _____, which can cause valve thickening by fibrosis and calcification.
Rheumatic carditis
What happens to the leaflets in mitral stenosis?
- the valve leaflets fuse and become stiff and the chordae tendineae contract and shorten.
- The valve opening narrows, preventing normal blood flow from the left atrium to the left ventricle.