Week 4: Lymph nodes
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Lymph node locations in the neck
Submental • Submandibular • Facial • Pre-auricular • Post-auricular • Occipital • Jugulodigastric • Cervical chain superficial (lower ear and parotid) • Cervical chain deep • Supraclavicular • Infraclavicular • Posterior triangle
Neck levels
Level Ia – submental
Level Ib- submandibular
Level II - upper internal jugular
Level III- middle internal jugular (deep cervical) chain
Level IV- lower internal jugular (deep cervical ) chain
Level V- posterior triangle
Level VI- central (anterior) compartment
Clinical Indications for evaluation of lymph nodes in head and neck
To investigate a neck mass or palpable lump in the neck
To stage head and neck cancers (not often as other imaging is usually used –CT, MRI, PET scans)
To differentiate between normal (benign or reactive), or malignant nodes
For disease recurrence post thyroid Cancer or other cancers in the head/neck
Sonographic Technique
Use high frequency linear transducer (high frequency for better superficial resolution and colour doppler sensitivity
Ask patient to indicate the palpable LN if there is a palpable lump in the neck
Lay patient supine with neck extended (may need to turn patients head to open up the space)
After obtaining consent, palpate the lump noting size, compressibility (hard/soft), location, mobility, pain or surrounding lumps
Place probe directly over ROI and survey in long and trans
Can use a stand-off or extra gel if node is very superficial
Can use panoramic view to demonstrate multiple nodes
Measure the node in question in long and trans
Try to label landmarks around the lymph node to help identify the region node is located
Extend the examination beyond the node in question to assess surrounding nodes for a thorough assessment of the anterolateral neck
If a Lymph Node (LN) is identified need to document
Size (AP more important than length or width)
Size of cortex (if thickened)
Location - where it is and what level or region (if tricky then label adjacent anatomy)
Internal consistency (hilum or no hilum, any calcifications)
Vascularity pattern
Symmetrical vs asymmetrical
Matting ( are there multiple LN’s clustered that move together)
Number (are they localized or in two or more regions)
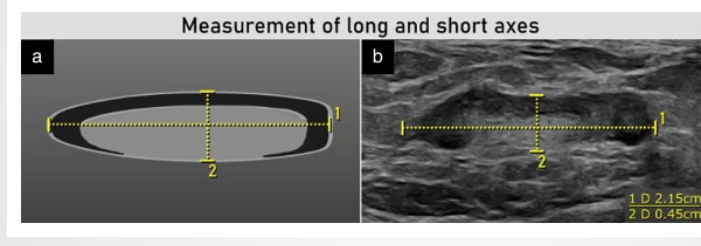
Documenting Size
Transverse usually not measured. Long axis and short axis measurement only . AP diameter/short axis most important and should be <1cm if normal
Cortex measurement
Taken at the widest point of cortical thickening perpendicular to the long axis of the lymph node
Cortical thickening
When the measurement at the widest point is equal to or wider than the medulla (fatty hilum)
Ultrasound Appearance of a NORMAL Lymph Node
Not palpable or painful unless superficial
Oval shaped short axis to long axis ratio = <0.5)
Rounded if located within SMG or Parotid Gland) • Measures <10mm AP diameter
Well defined
Internally – homogenous hypoechoic (usually with fatty hilum)
Presence of ‘fatty hilum’ (echogenic central hilum)
Even cortex
Colour doppler no or minimal colour (if colour present, usually in the hilum)
Hajek’s Classification of Cervical Lymph Nodes
Patient age, symptoms, medication, history (of any malignancy, being unwell, any prior studies or investigations)
Location: If hard to document region, take note of adjacent anatomy.
Number: Localized in one region or generalized in more than one region.
Matting:
Consistency: Hard/rubbery/soft.
Fixed vs Mobile: Fixed - ?malignancy, mobile - benign.
Pain/tenderness vs Painless: Painful/tender - inflammatory - benign, Painless - ?malignant.
Duration and Rate of Growth: Fast growing - suspicious, slow growing/stable over time - benign.
Matting
Term used to describe when a group of nodes are conglomerated
(clustered/merged together).
Does not always indicate malignancy.
Can be due to benign conditions such as infection and sarcoidosis
Sarcoidosis
Disease involving growth of inflammatory cells (granulomas) in any part of the body (most commonly lung and lymph nodes). Cause unknown, thought to be caused by body’s immune response to an unknown substance.
Reactive lymph node
Term to describe response due to inflammation in the absence of neoplasia.
Most common cause of LN enlargement and is non-neoplastic and reversible.
Considered a healthy response and doesn’t imply pathology within the node.
Reactive lymph node features
Features are not definitive and need correlation with clinical picture
Clinically: Swollen/tender/soft, can be multiple and bilateral.
Oval or elongated shape (wider than taller).
Measures <10mm AP diameter.
Margin: Unsharp border (can also be sharp if small).
Internally homogenous and hypoechoic.
Presence of fatty hilum.
Even cortex around hilum.
Generally increased hilar or central vascularity.
Tuberculosis Lymph Node features
Tuberculosis: An infectious disease caused by bacteria primarily affecting the lungs
Clinically – firm, non-tender, palpable one or more cervical masses.
Location: most often in supraclavicular fossa and post triangle.
Round shape.
Internally –hypoechoic, intranodal cystic necrosis.
Unsharp borders.
Loss of fatty hilum.
Varied color doppler (both benign and malignant features).
Main differential from malignancy:
Adjacent soft tissue edema.
Nodal matting (nodes grouped together).
Lymphomatous Lymph Node features
Lymphoma: cancer of the lymphatic system and can present with fever, night sweats and weight loss.
Clinically – long standing palpable firm, rubbery lumps, fixed and painless, can be localized.
Increase in size with serial exams.
Round shape (taller than wide).
Internally hypoechoic.
Margins: sharp borders.
Eccentric cortical thickening.
Loss of fatty hilum.
Both hilar and peripheral vascularity (mixed).
Malignant Lymph Node features
Clinically: palpable, hard, fixed painless lumps, localized, unilateral, or generalized spread.
Increase in size with serial scans.
Round shape (taller than wide).
Internally: hypoechoic, nodal necrosis.
Sharp border (unless extracapsular spread then ill defined).
Loss of fatty hilum.
Uneven cortical thickening.
Mixed or peripheral vascularity.