Transport in Animals
1/20
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
Why do multicellular organisms need a circulatory system?
Need to exchange materials with their environments
Small SA : Vol ratio, cannot rely on diffusion for exchange of essential substances as compared to unicellular organisms
Carries fluids containing materials needed by organism, as well as waste materials needed to be removed
Heart
Hollow, muscular organ located in chest cavity
Pumps blood around the body
Specialised cardiac muscle tissue for repeated involuntary contraction without rest
Artery
Blood vessel which carries blood away from heart
Walls contain lots of muscle and elastic tissue, narrow lumen to maintain and withstand high blood pressure
Diameter: 0.4 - 2.5 cm
Arteriole
Small arteries which branch from larger arteries that connect to capillaries
Diameter:
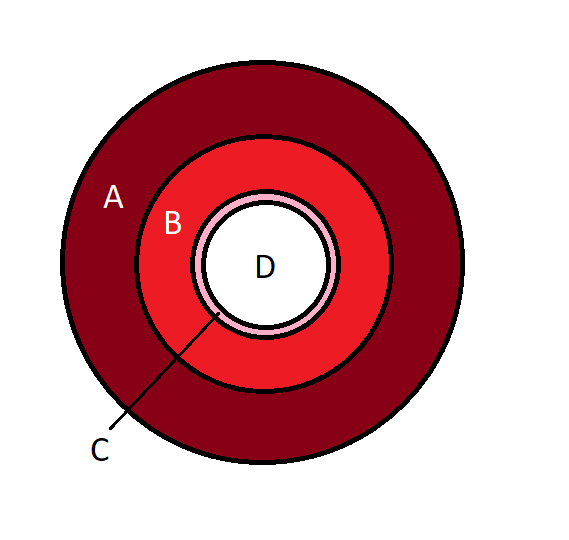
Artery Structure
A: Outer Layer, contains collagen fibres, some elastic fibers
B: Middle Layer, contains elastic fibres, collagen fibres and smooth muscle
C: Inner Layer, the endothelium; smooth single-cell layer of squamous epithelium
D: Narrow lumen, relative to thickness of wall
Capillary Structure
Wall made of endothelium, one cell thick
Lumen is 7 µm in diameter, just big enough for RBC to fit through
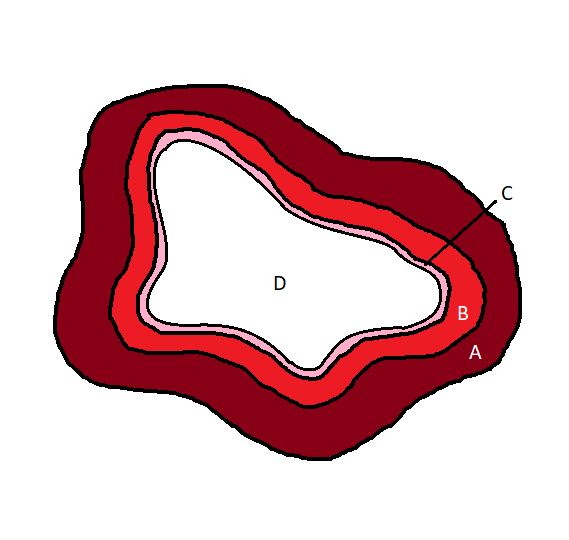
Vein Structure
A: Outer layer, mostly collagen fibres
B: Middle layer, very thin, containing some smooth muscle and elastic fibres
C: Inner layer, single-celled layer of squamous epithelium
D: Large lumen relative to thickness of wall, irregularly shaped
Also contains valves to prevent backflow of blood (not shown in diagram)
Red Blood Cell (RBC) / Erythrocyte
Approx. 7.5 µm in diameter
Biconcave disc shape for increased surface area
Contains haemoglobin (globular, conjugated protein containing 4 prosthetic haem groups)
No nucleus to allow more room to carry haemoglobin
Tissue Fluid vs. Blood
Blood
Cellular Components (RBCs, WBCs)
Larger proteins
Tissue Fluid
Similar to blood plasma as itself, however contains lower number of proteins
Carries dissolved solutes and small proteins, as larger proteins cannot fit through small fenestrations
Majority is water
Importance of water in blood
Water has high specific heat capacity, which means it is highly thermally stable so the haemoglobin is not altered by changes in temperature (the haemoglobin is very important for transportation of gases)
Is a universal solvent so important nutrients are transported in solute form in the blood
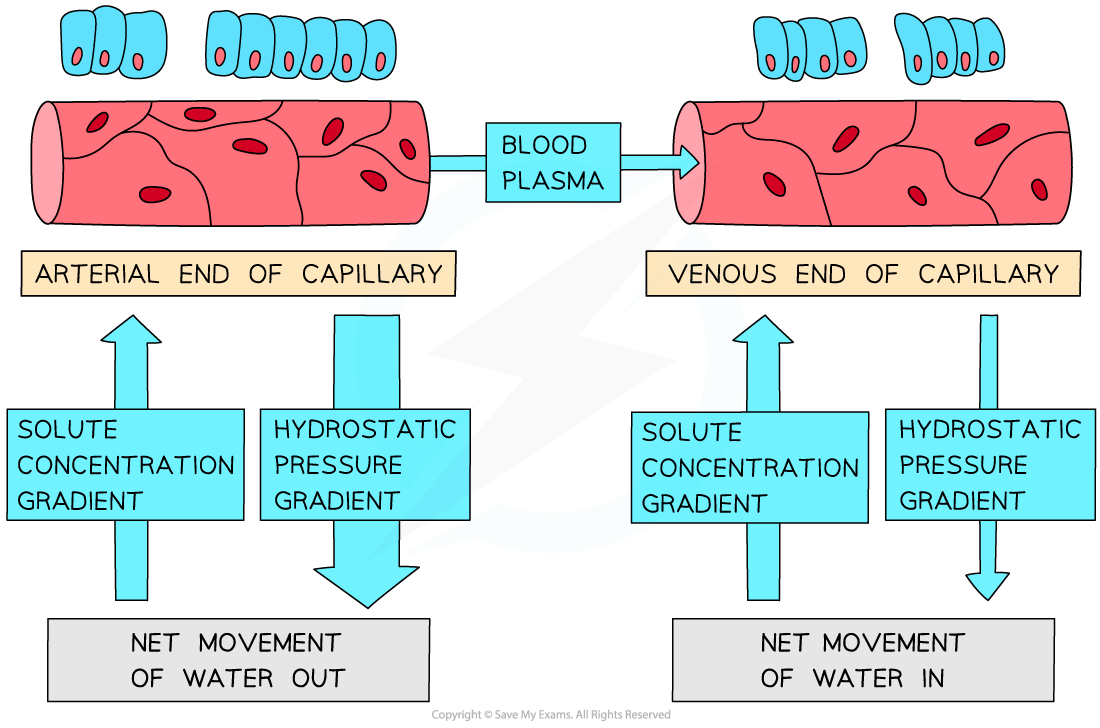
Tissue Fluid Formation
Formed from plasma leaking out through small fenestrations in the capillary walls to surround the cells of the body
Arterial end of capillary has higher hydrostatic pressure than venous end, so plamsa is pushed out of capillary
At venous end, less fluid is pushed out of capillary as pressure within capillary is reduces
Binding of oxygen to haemoglobin
Oxygen binds to haemoglobin to form oxyhaemoglobin
4O2 + Hb → HbO8
Binding of O2 causes conformational change of Hb structure which makes the binding of the next 3 O2 molecules successively easier
Dissociation process is reversed, as the last O2 molecule is hardest to dissociate
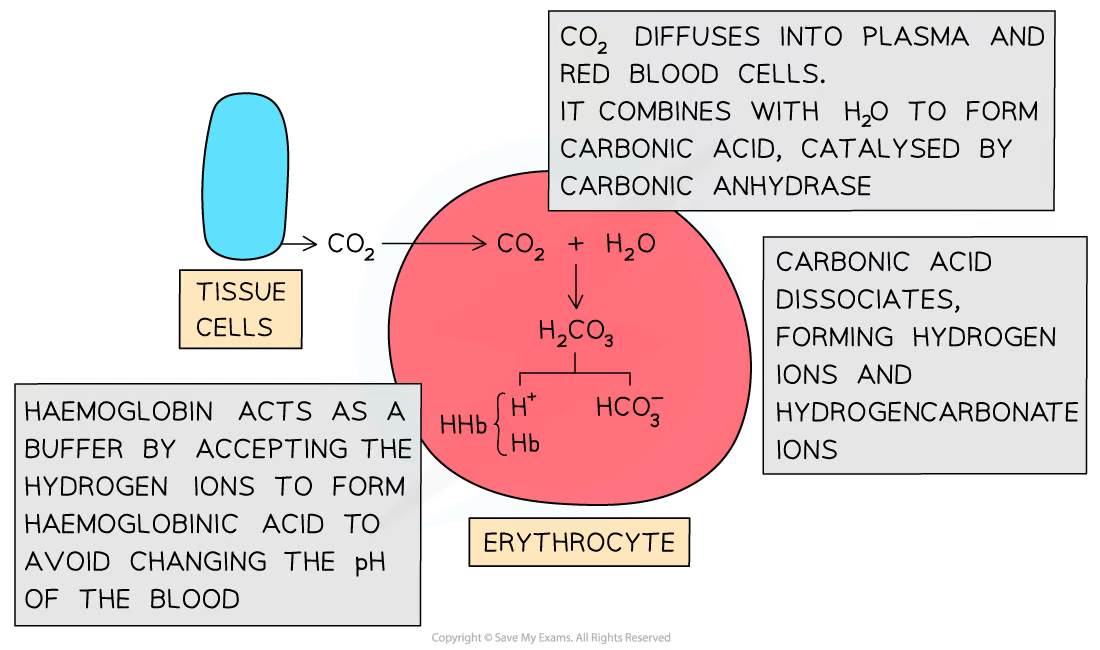
Carriage of Carbon Dioxide
CO2 moves from respiring tissue to RBC
Carbon Dioxide reacts with water to form carbonic acid (carbonic anhydrase catalyses this reversible reaction)
CO2 + H2O ⇌ H2CO3
Carbonic acid dissociates into H+ and HCO3- ions
H2CO3 → H+ + HCO3-
Chloride Shift
HCO3- ions formed from H2CO3 dissociation is transported out of RBCs via a transport protein in the membrane
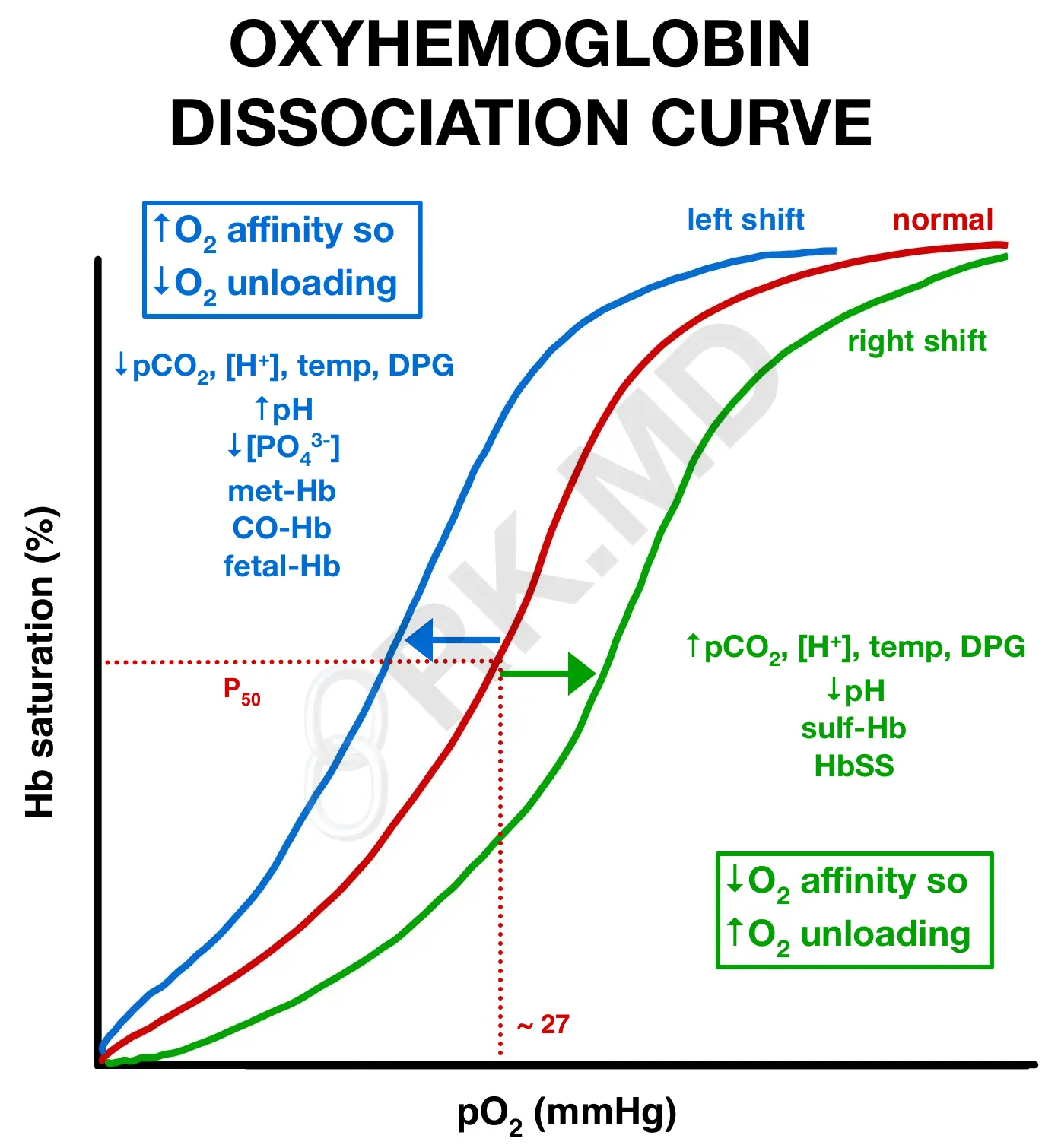
Oxygen Saturation Curves
Shift to right:
Increased acidity (H+ ions or CO2)
Increased temperature
Causes lower affinity for O2
(Low saturation of Hb even at higher partial pressures of O2)Also known as the Bohr Effect
Shift to left
Decreased acidity (H+ ions or CO2)
Decreased temperature
Causes higher affinity for O2
(High saturation of Hb even at lower partial pressures of O2)
Pathway of Blood (from Vena Cava)
Vena Cava → Right Atrium → Atrioventricular valve → Right ventricle → Semilunar valve → Pulmonary Artery → Lungs → Pulmonary Vein → Left Atrium → Atrioventricular valve → Left Ventricle → Semilunar Valve → Aorta → Body
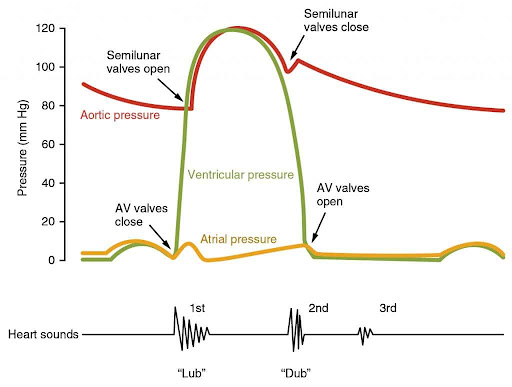
Atrial Systole
Atria walls contract
Pressure inside atria increase which exceeds pressure inside ventricles
Atrioventricular valves open and blood is pushed into ventricles
Ventricular Systole
Ventricle walls contract
Pressure inside ventricles increase which exceeds pressure inside the arteries (Pulmonary/Aorta)
Semilunar valves open and blood is pushed through the arteries, either towards the lungs in the pulmonary artery, or the rest of the body through the aorta
Ventricular Diastole
Interpreting Cardiac Pressure Graphs
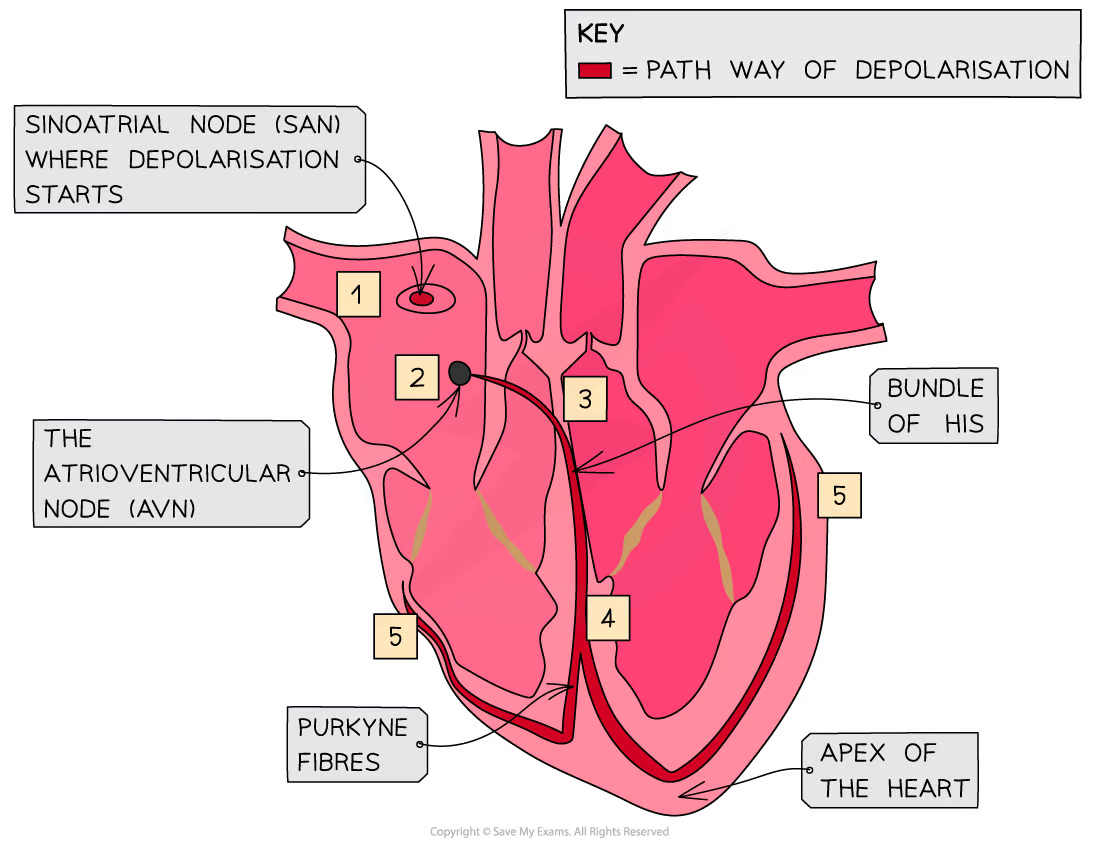
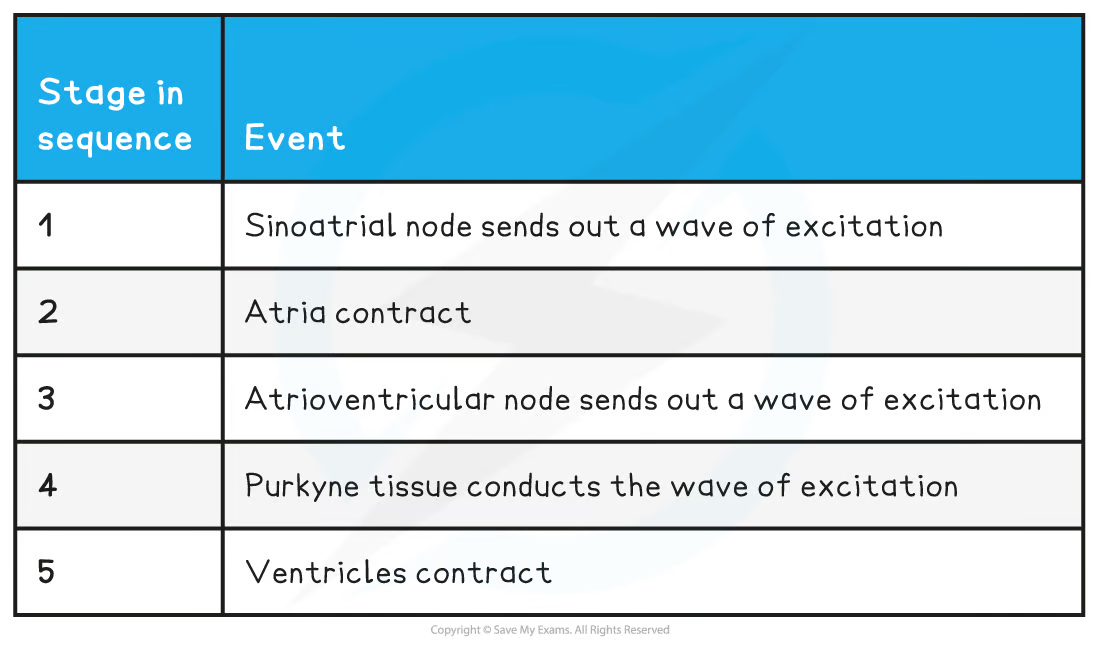
Sinoatrial node sends out wave of excitation.
Wave travels through the walls of atria, which contract.
Non conductive tissue stops the wave and directs it to atrioventricular node.
ANV absorbs wave, causing a delay, before channeling it down the septum.Purkyne tissue conducts the wave of excitation down the septum and up the ventricular walls.
Ventricles contract.