Fundamentals Block 4: B and T Lymphocyte Development
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
where are B-cells developed and how do we measure development?
B-cell development occurs in the bone marrow and is dependent on successful BCR gene rearrangements
Stages of Development are identified based on surface proteins and the rearrangement of Ig genes
What are the four stages of B-cell development?
Pro-B Cell - DNA is spliced in order to create IGM heavy chain
→ CD19 and CD20 expression first identifiable here
Pre-B Cell - DNA is spliced in order to create the light chain genes
Immature B-cell - has IgM BCR on cell surface and tests for self reactivity. If it passes it leaves the bone marrow
Mature B Cells - complete development in secondary lymphoid tissue (express both IgM and IgD)
What are IL-7 and SCF?
IL-7 and Stem Cell Factor are critical cytokines for B-cell maturation
→ IL-7 and SCF sends growth signals to developing B-cells
What are the two checkpoints in B-cell development
Checkpoints are in place in order to ensure that the IgM heavy chain has two features:
1) Functional
→ checks for heavy chain structure and assesses whether the pre-BCR is capable of associating with Iga and IgB in order to send activation signals
→ The heavy chain is paired with a randomly made surrogate light chain
2) Not Self Reactive
→ following pairing of heavy and light chains - antigen binding site is tested for self-reactivity
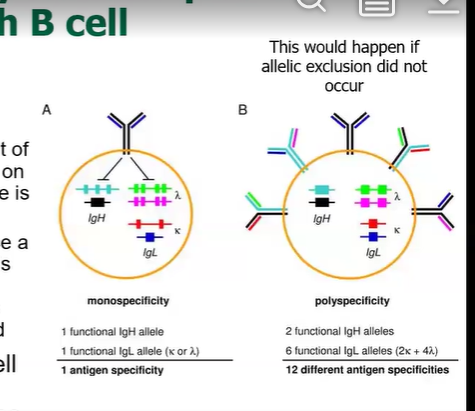
What is Allelic Exclusion
Heavy chains are made simultaneously via rearrangement of the VDJ genes across both the mother and the father’s chromosomes
→ once a functional heavy chain is transcribed, the other chromosome will be turned off
→ The same event occurs for the light chain as well
allelic exclusion allows us to prevent making a bunch of different antibodies with different antigen specificities
What happens if a BCR is self-reactive during testing?
If a BCR binds self-antigen strongly enough to activate signaling, the cell will undergo receptor editing in order to change its light chain
→ only the light chain can be modified if a BCR is self reactive
What are the two types of mature B-cells
Mature B-cells migrate to the spleen or lymph nodes and differentiate into two kinds of B-cells
→ Follicular B-Cells (form germinal centers) - formed from the T-dependent antigen pathway
→ Marginal Zone B-Cells - produce low affinity antibodies, short lived plasma cells that secrete IgM
What is T-cell development dependent on?
T-cell development is dependent on successful TCR gene rearrangement
→ goal is to create a T-cell with a receptor that can recognize self MHC but whose antigen specificity is randomly generated
→ this is done via interactions with cytokines: SCF and IL-7
What happens to the thymus one year after birth?
Human thymus will begin to degenerate by 1 year after birth
→ however this does not affect immunity drastically because the mature T-cell repertoire is long lived
→ older people are slightly immunocompromised because they cannot generate new T-cell responses
What is DiGeogre Syndrome
Thymus fails to develop
→ T-cells are absent and patient’s lack adaptive immunity
What are the stages of T-cell development marked by?
Thymocyte development is marked by the expression of CD4 and CD8 on the cell
1) Double Negative (both CD4 and CD8 not expressed)
2) Double Positive (both CD4 and CD8 expressed)
3) Single Positive (either CD4 or CD8 expressed)
What are the stages of T-cell development? (4)
1) committed double negative T-cell progenitor enters into the thymus; Beta chain rearrangement occurs
2) uncommitted double positive thymocyte has a functional beta chain → will undergo alpha rearrangement
3) committed double positive thymocyte has a functioning TCR and can undergo selection
4) Thymic epithelial cells will present antigens to Thymocytes in order to test for self-reactivity - depending on whichever MHC molecule the thymocyte will interact with will determine which CD4 or CD8 it will keep
What is the Selection process of Thymocyte development?
Newly developed Thymocytes must be tested in order to make sure they can recognize host MHC and are not self reactive. Comes in two steps
1) Positive Selection: Thymic Epithelial Cells have peptides presented on MHC Class I and II
→ test to see if the TCR can bind to MHC Class I or II
→ will keep CD4 if capable of binding to MHC Class II, will keep CD8 if capable of binding to MHC Class I
2) Negative Selection: testing for self reactivity
→ thymic epithelial cells will present self antigens
→ thymocytes that react to self-antigens will undergo apoptosis
What is Autoimmune Regulator
At the thymic epithelial cells there is a transcription factor known as AIRE
→ capable of turning on the expression of proteins from host cells from all around the body
→ allows for us to expose thymocytes to proteins from the heart, or kidney, or any other tissue in order to be more effective
What is APS-1
Absence of AIRE
→ causes thymocytes to not be properly selected - causes autoimmune manifestations