L4: The control of arteria blood pressure
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
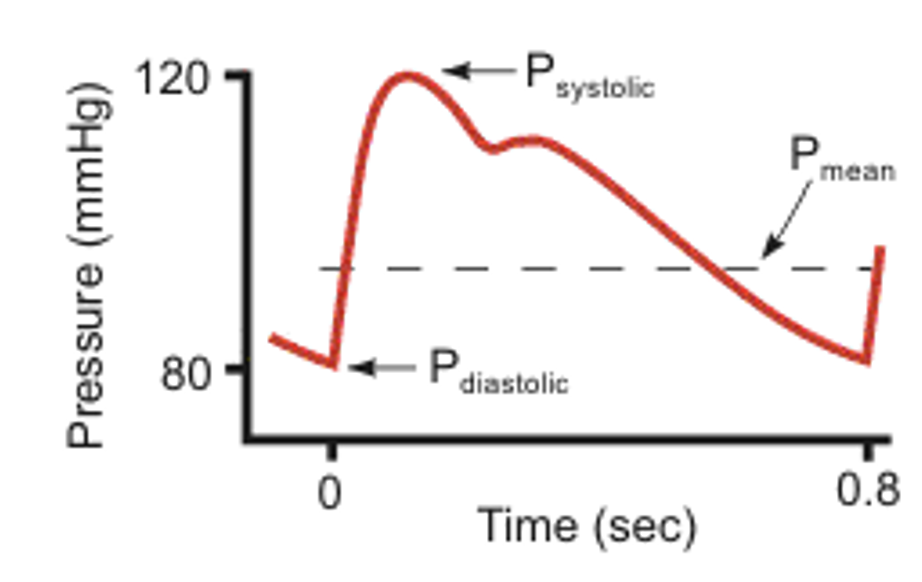
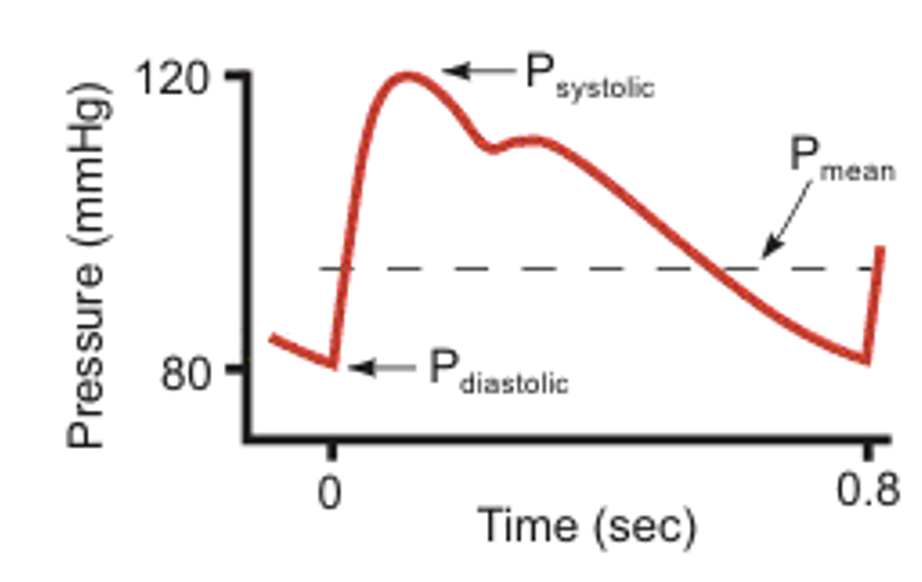
What is the mean arterial blood pressure ABP
the pressure measured within large arteries in the systemic circulation
split into systolic and diastolic blood pressure
Systolic blood pressure
→ 120mmHg normalling
peak when heart ejects blood into the aorta
This creates a pressure gradient towards the rest of the circulation
so blood flows away from the aorta and the aortic pressure reduces to a trough value…
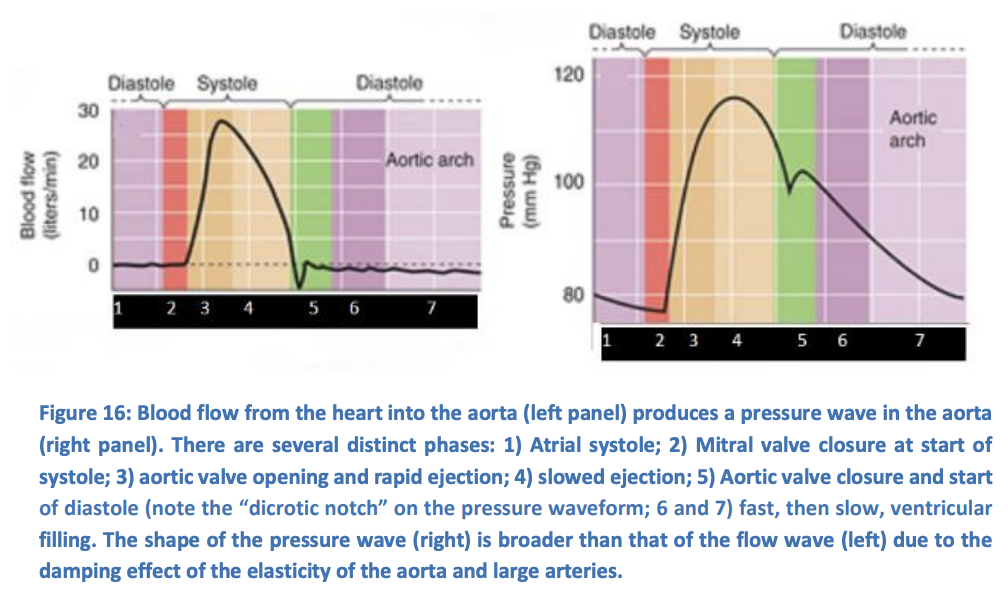
Diastolic blood pressure
→ 80 mmHg
the aortic pressure at a trough value
(before the heart beats raisess pressure again)
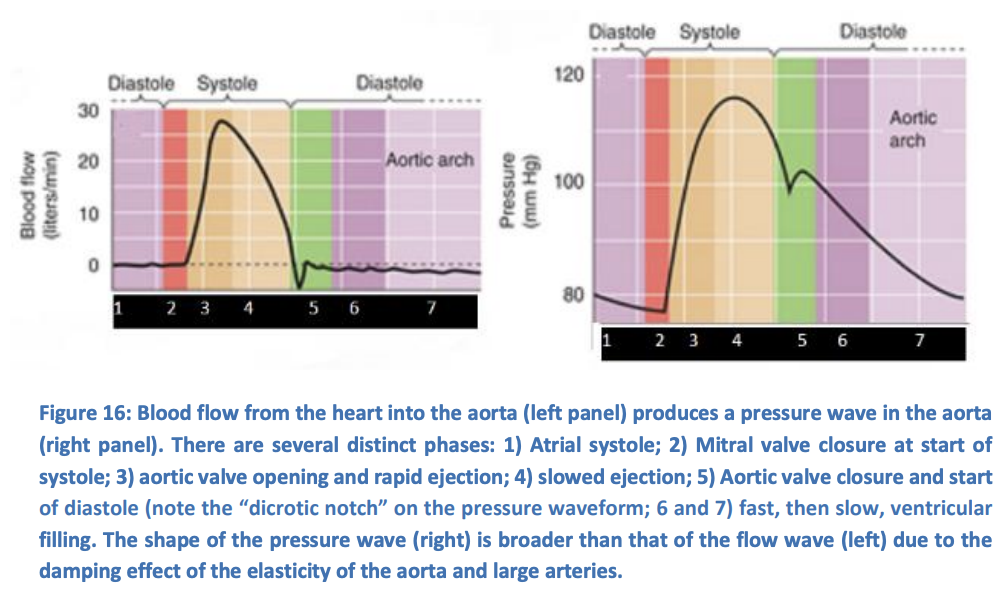
Why is the fall in pressure between the systolic and diastolic not smooth
dicrotic notch exists:
pressure in the aorta begin to exceed those in the ventricle
pressue in aorta begin to exceed those in the ventricle
quickly terminated by the closure of the aortic valve
→ produces a small ‘rebound’ pressure wave
What is the mean blood pressure? MAP
MAP: diastolic + 1/3(systolic-distolic)
note: pulse pressure= systolic-diastolic
How does MAP increase
with age
higher in men (between puberty and meopause)
Aortic valve leakage
BUT: ABP stays constant
Pulse pressure can increase if
arterial compliance reduces
e.g in atherosclerosis
if blood flow away faster in diastole
(i.e in exersise)
due to TPR drops
pathologically if valve leaks
Age
BUT ABP stays the same
But when the pulse pressure increases, what happens to MAP
MAP stays constant:
i.e systolic pressure rises but diastolic pressure falls
This strongly suggests that mean ABP is the principal regulated variable
This makes sense→ systolic may increases but diastolic must also fall
this ensures that pulse pressure does increase
but
MAP will stay constant
Why is ABP being the principal variable controlled by cardiovascular system, really useful?
keeping ABP constant→ blood flow to individual tissues can be regulated simply be controlling the local Arteriolar resistance
The circulation thereby approximates a constant pressure/variable flow system
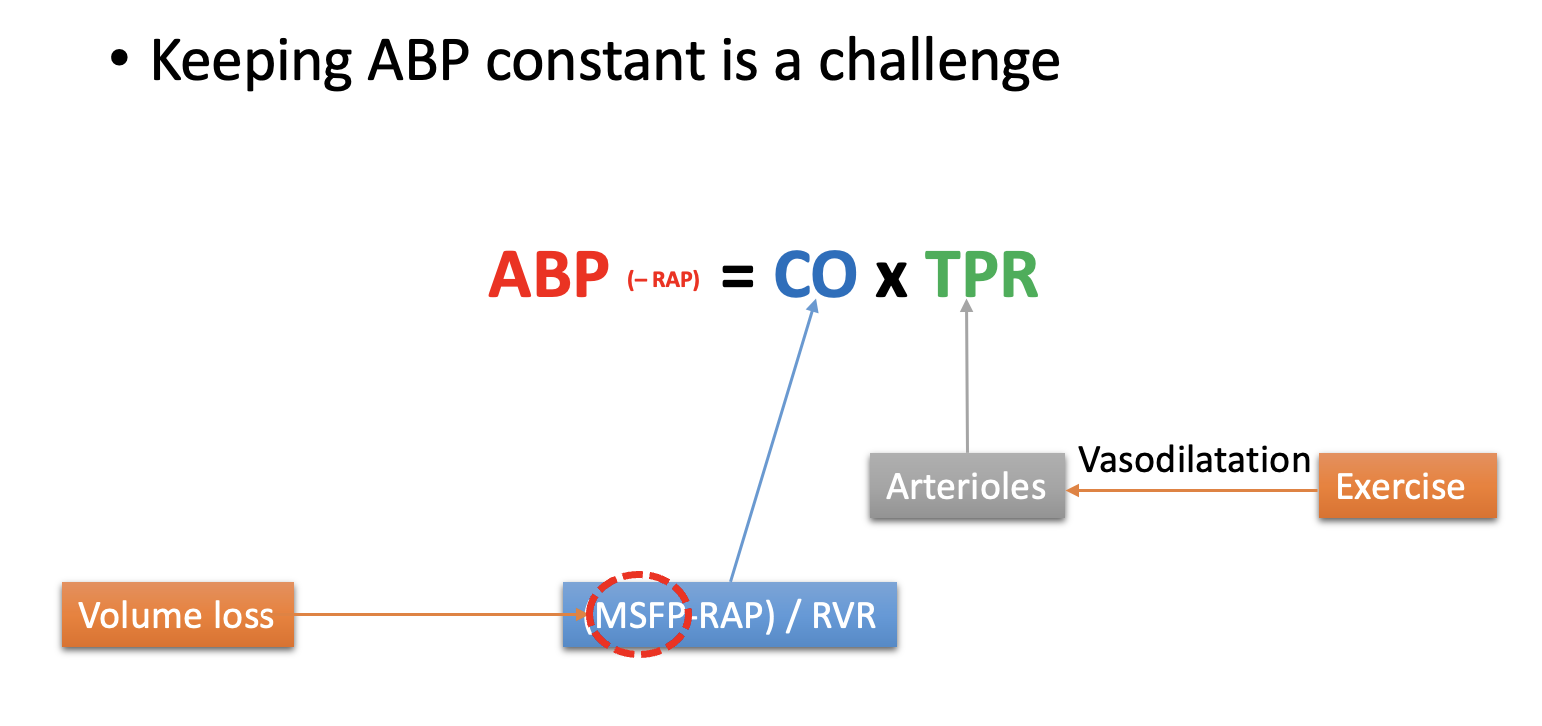
How does ABP relate to CO and TPR
CO and TPR are the principal determinants of ABP
physiological and pathalogical processes can change TPR
i.e exercise decreases TPR
blood loss reduces MSFP and CO
THEREFORE→ control processses are needed to maintain a relatively constant ABP
Rearranging Darcy’s equation for whole circulation
ABP= CO x TPR
highlights that changing CO or TPR will stress ABP control
and also
Changing CO or TPR can be used to control ABPR
Why are CO and TPR though to be largely indenependent
TPR→ primarily a function of arteriolar resistance
CO→ afterload does not greatly influence CO
THEREFORE: they provide two separate mechansims for regulation of ABP
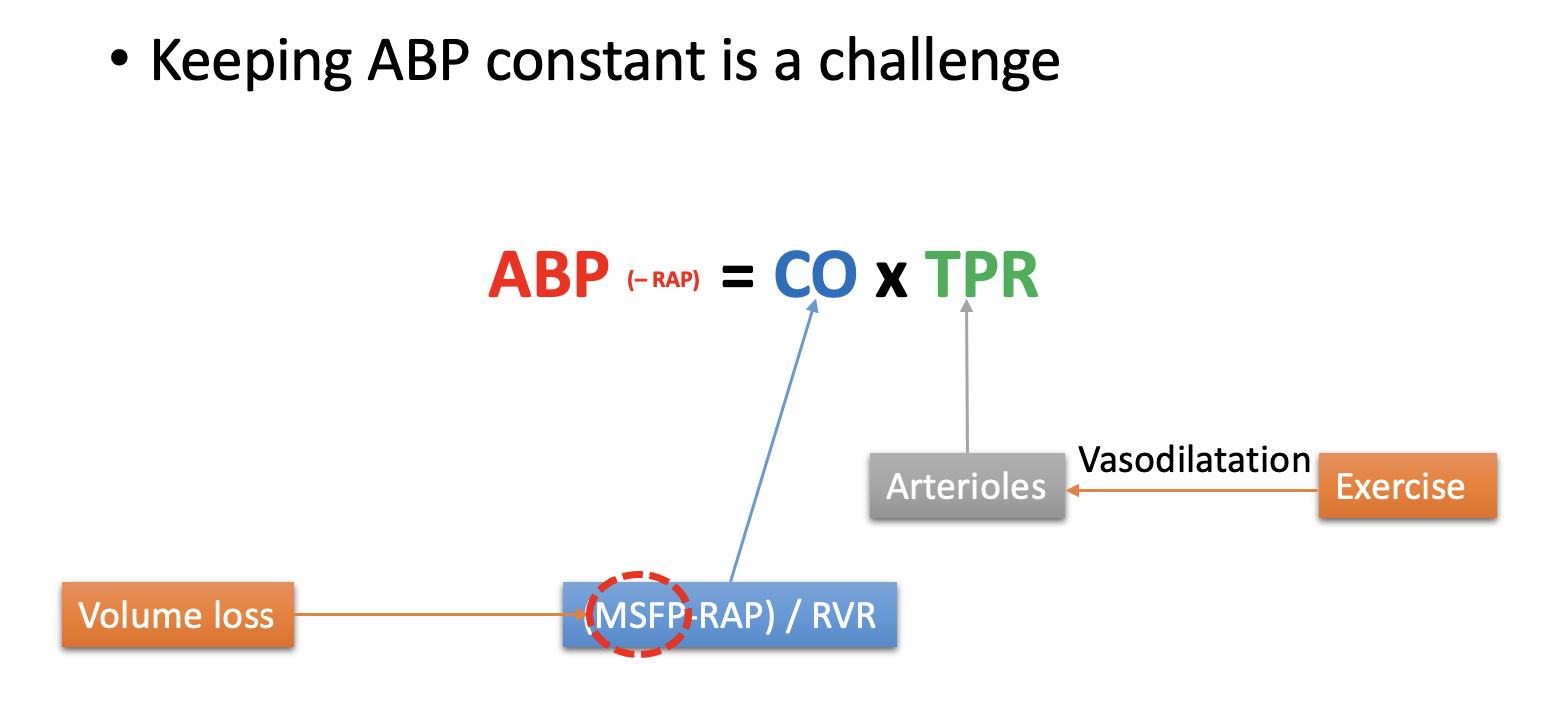
However, in order to regulate ABP, we must be able to monitor it
Another reason why ABP is the prinipal variable controlled is coz
CO and TPR cannot easily be monitored
but ABP can!
Three feed-back mechanisms for monitoring blood pressure
Feed-back systems
high blood pressure baroreceptors
arterial chemoreceptors
low pressure baroreceptors
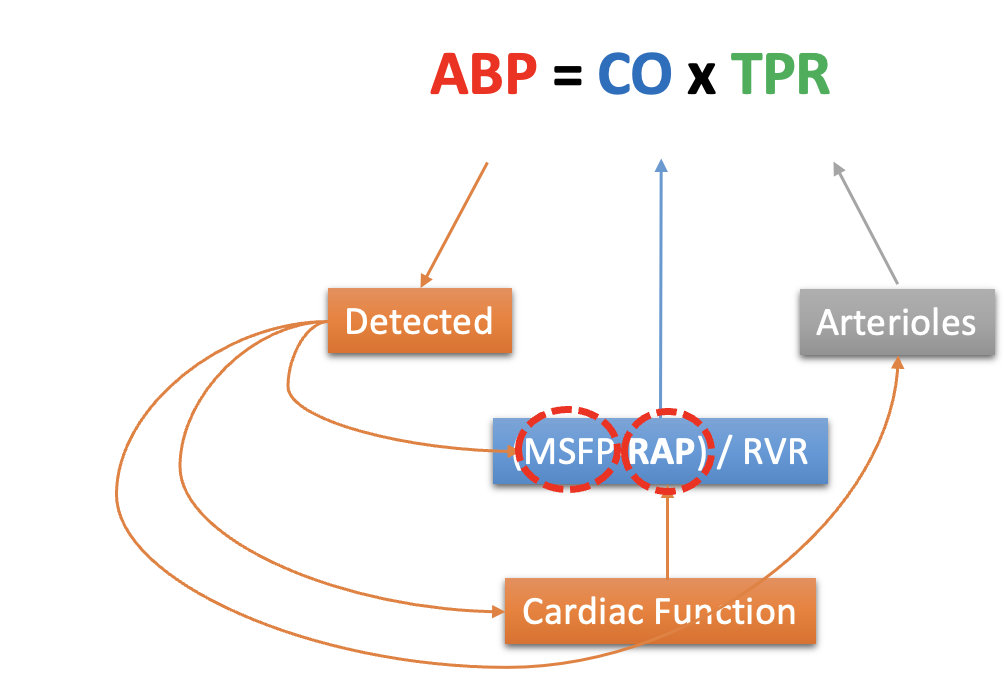
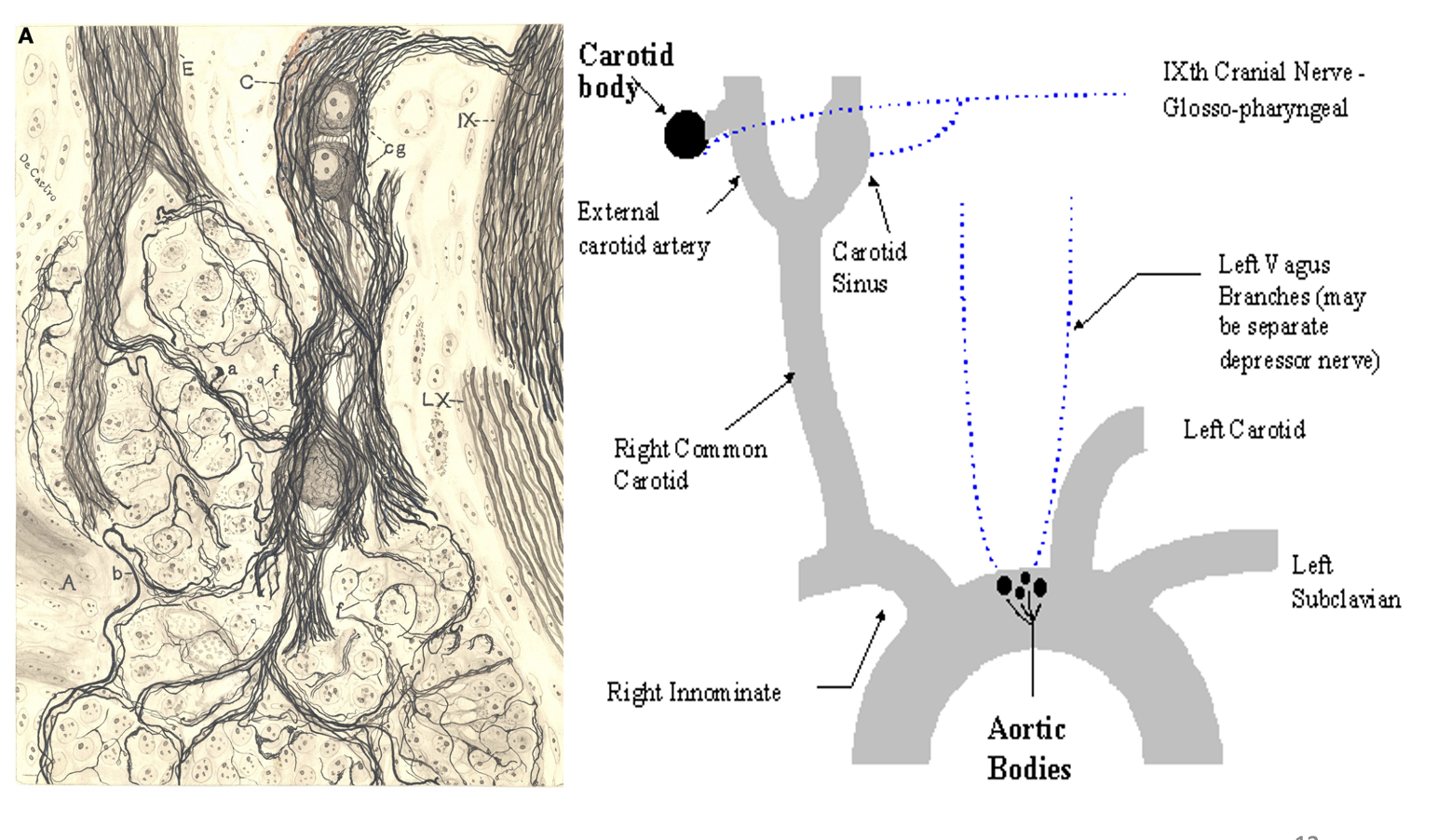
High pressure baroreceptors: what are they
mechanoreceptors at strategic high-pressure sites
Carotid sinus→ just beyond the bifuraction of the carotid artery
Aortic arch
also: afferent renal arterioles have one too
High pressure baroreceptors: structutre of the nerve
stretch-sensitive nerve endings
intermeshed within elastic lamellae
inregions with relatively little collagen and smooth muscle
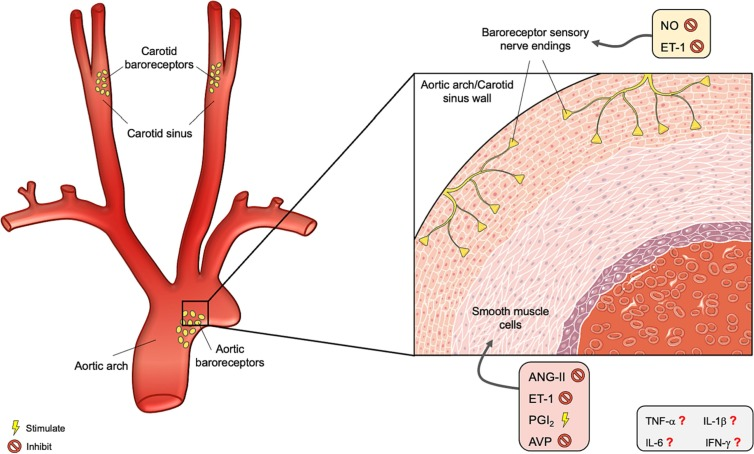
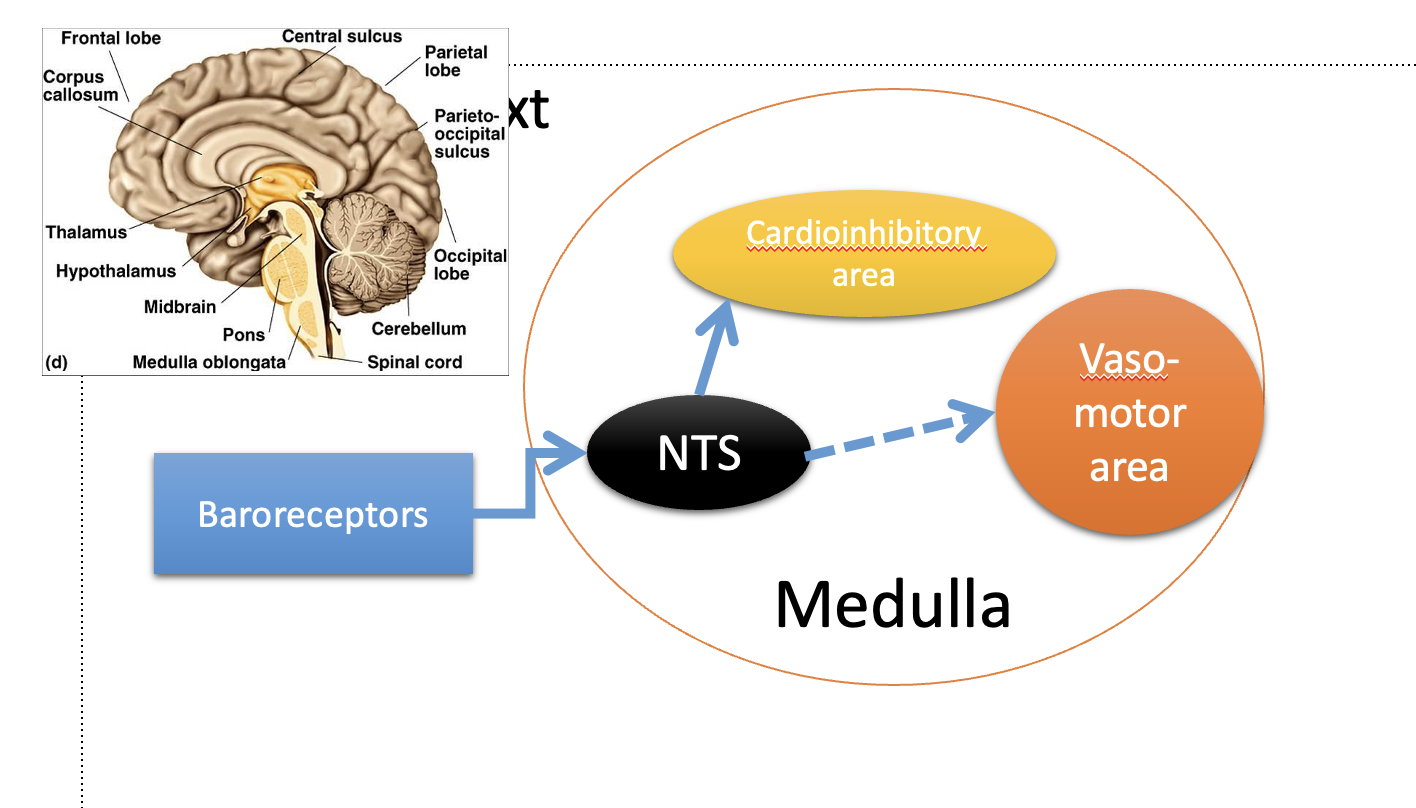
High pressure baroreceptors: what happens upon stretch
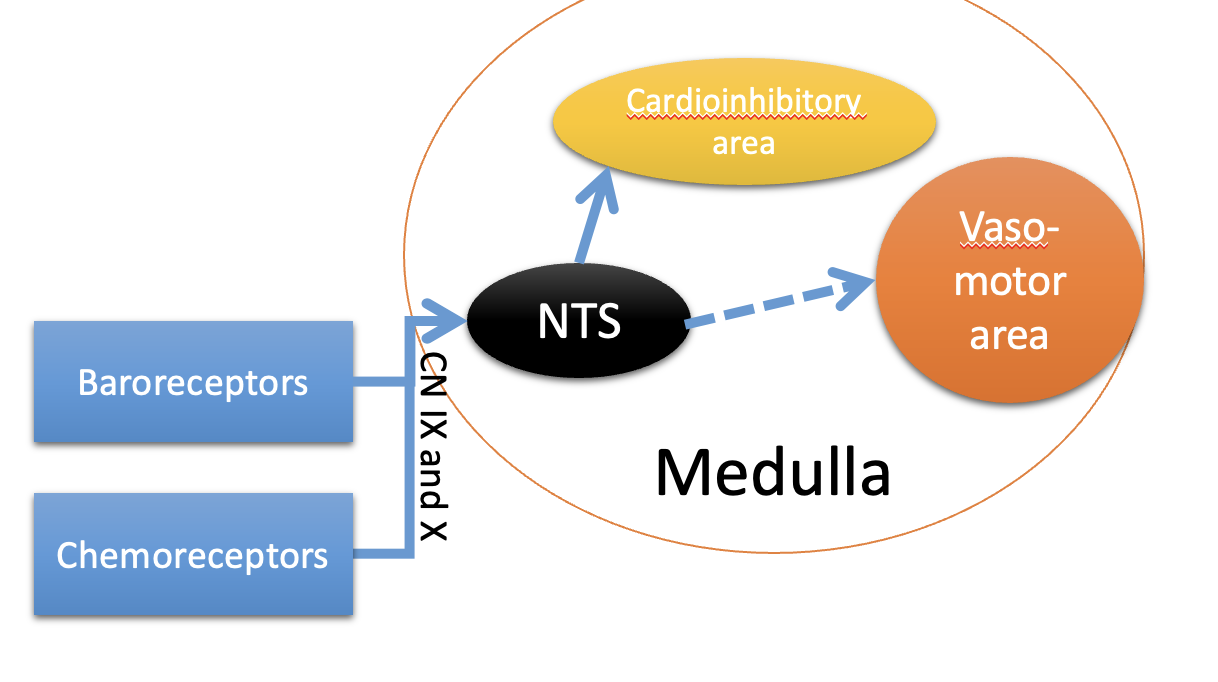
Triggers activity in baroreceptor fibres of
glossopharyngeal nerve ←(carotid sinus)
vagus ←(aortic arch)
Stimulates neurons in the Nuleus Tractus Solitarius (NTS) in the medulla
This inhibits the vasomotor centre
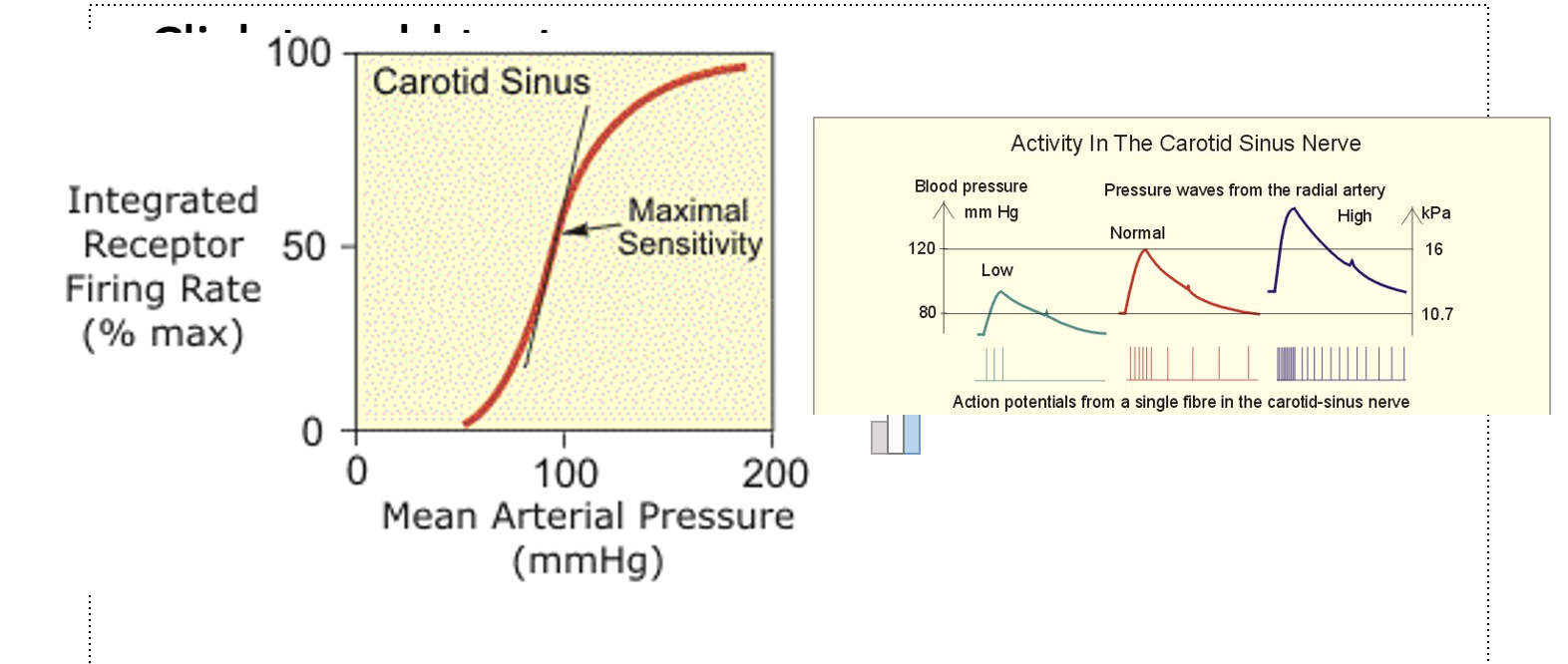
High pressure baroreceptors: advantage of different baroreceptor sensitivies
different baroreceptors have different sensitiviteis to blood pressure
enables groups of fibres to cover LARGE ranges of blood pressure
50-200 mmHg
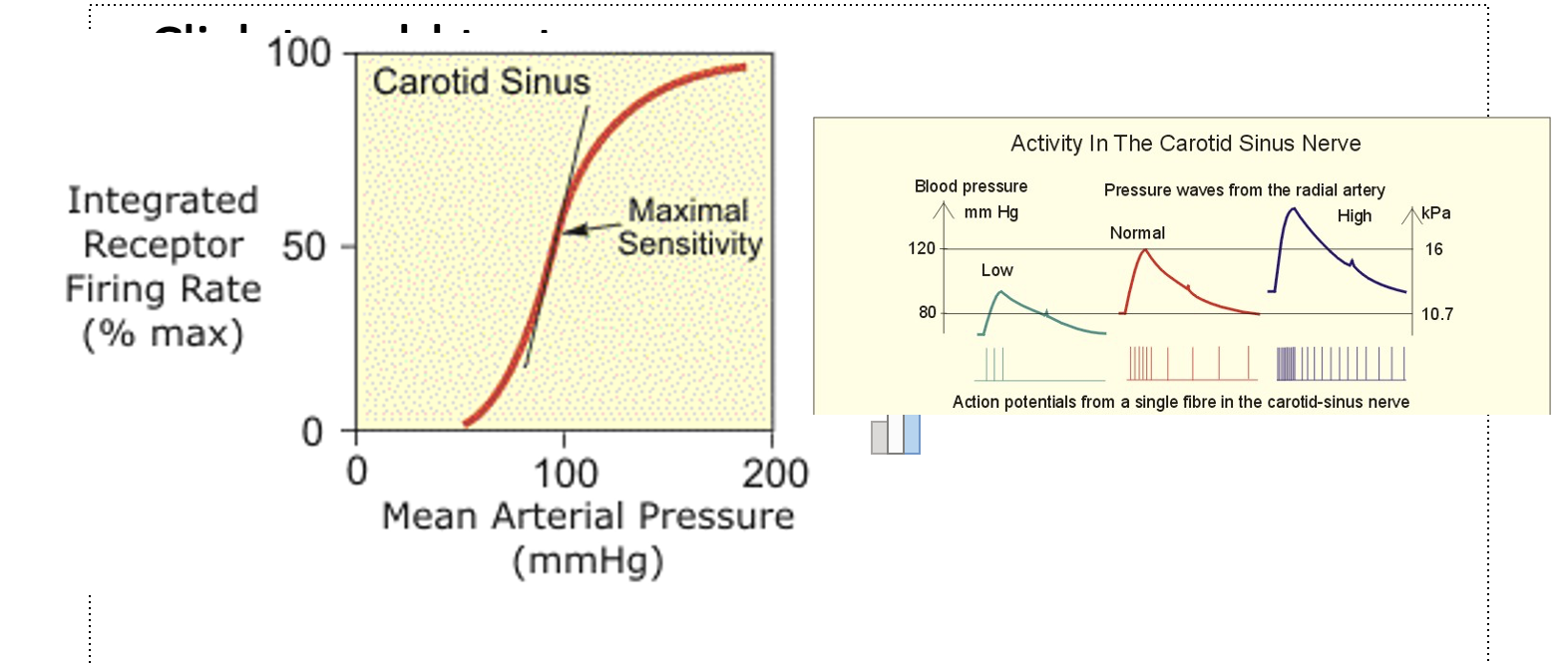
High pressure baroreceptors: Carotid sinus vs aortic arch
Carotid sinus is more sensitive than aortic arch
but
Aortic arch can respond as pressure above which the arotid sinus response saturates (i.e Aortic is sensitive to higher pressures tha ncarotid)
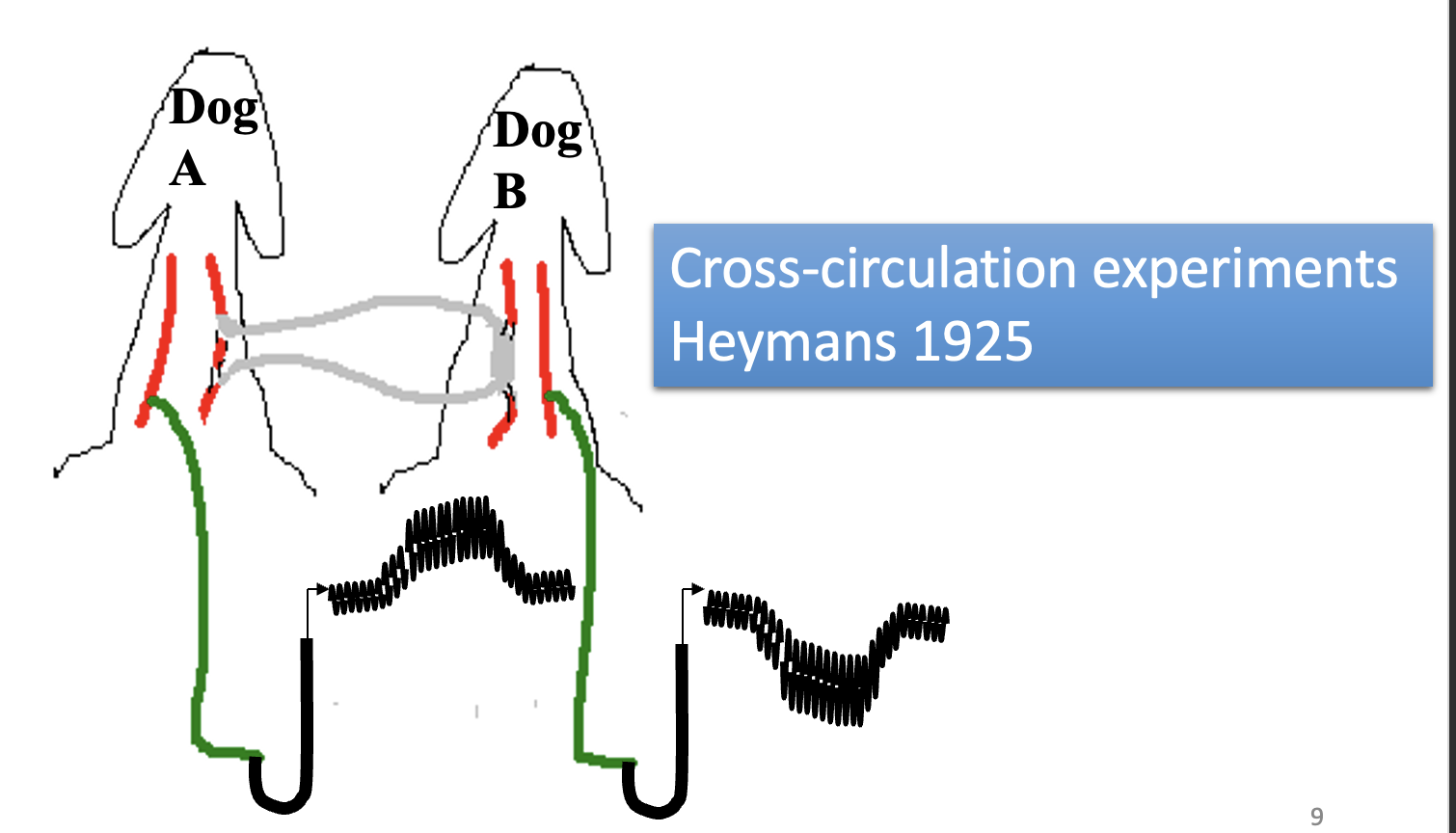
High pressure baroreceptors: cross- circulation experiment to show increased blood pressure at carotid sinus produced a reflec reduction in BP
Carotid sinus of dog B was connected into the dog A circulation
Dog A injected with noradrenaline
increases blood pressure
triggered a reflex fall in blood pressure in dog B
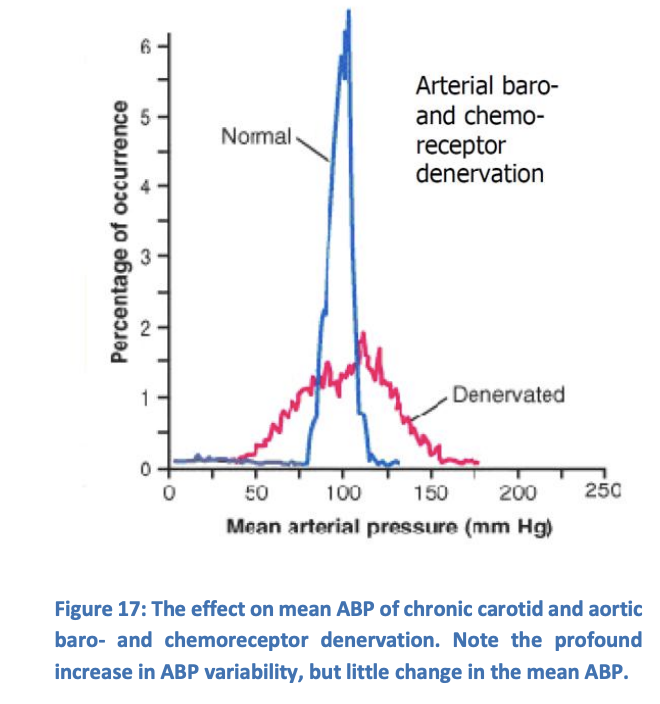
High pressure baroreceptors: What happens on the denervation of arterial baroreceptors
ABP becomes much more variable
why: physiological stress → change in acitivty or posture
BUT: mean ABP stays relatively constant
High pressure baroreceptors: what does this suggest about their importance
Variability→ high-pressure baro and chemorepecots in the short-term control of ABP
constant mean ABP→ suggests ABP is regulated by other mechanisms than the high-pressure repceotors
i.e if mean ABP changes→ high pressure baroreceptors reset and regulate to new mean ABP
thus, showing that these receptors are not responible for setting the mean ABP and are only short term
Arterial and central chemoreceptors: where are they
Carotid bodies
Aortic bodies
Medulla
Arteries
All but the arterial chemoreceptors mainly regulate ventilation:
arterial do have a role in ABP control when blood pressure
Arterial and central chemoreceptors: role of arterial chemoreceptors
role in ABP control when
blood pressure is very low
Po2 is very significantly reduced
role is important because the high pressure baroreceptors are relatively unresponsive under conditions of severe hypotension
Arterial and central chemoreceptors: how they work
Extreme condisions
carotid and aortic boddies detect low O2 delivery
medullary chemoreceptors detect high arterial CO2
via the resultant reduction in brain pH
Afferent signals from the arotid and aortic bodies travel by similar pathways to baroreceptors signals
carotid sinus→ glossopharyneal
vagus nerve→ aortic arch
Low pressure baroreceptors: importance
as high pressure baroand chemorecepetos do nothing on mean blood pressure
strongly suggests that longer-term control of ABP involves other detection mechanisms
also:
due to importance of MSFP in determining ABP
unsuprising that stretch receptors are exist in strategic low-pressure areas of the circulation
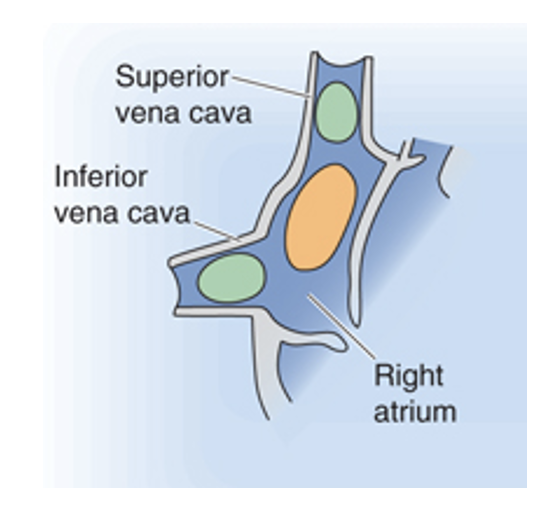
Low pressure baroreceptors: where found
strategic low pressure areas
junctions of atria with their corresponding veins
atria themselves
Cardiopulmonary baroreceptors
Low pressure baroreceptors: role
Especially detect RAP:
if RAP raised→ suggests circulation is over-filled
so the heart cannot maintain low venous pressures (so venous return will be lower)
i.e in heart failture and oedema as capillary pressures rise
if RAP low→ suggests that cardiac output is maximal for the current MSFP
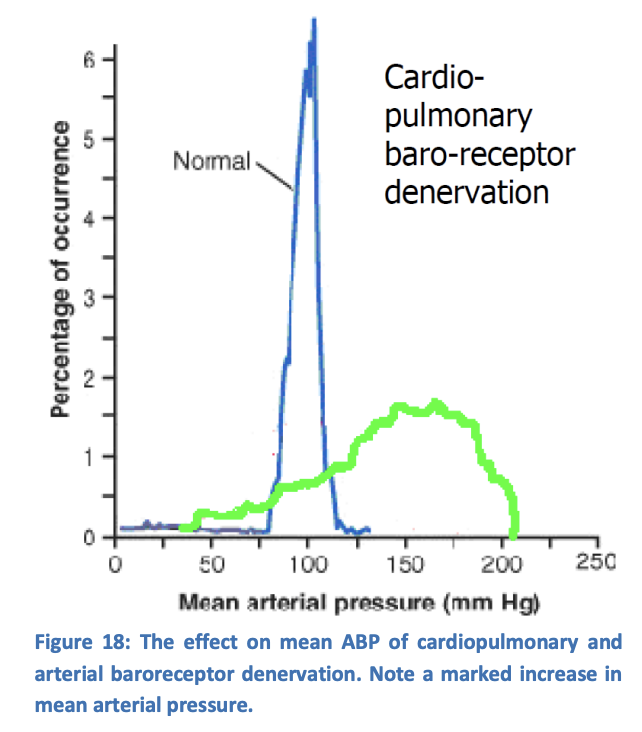
Low pressure baroreceptors: what happens if denervated (and arterial baroreceptors denerved too)
produce mean ABP rise
→ contrasts with the normal ABP seen with arterial baroreceptor denervation alone
Low pressure baroreceptors: how they work
pressure increase→ firing rate increases
afferent signals travel via vagus
to nucleus tactus solitarius NTS in medulla
to hypothalamus
can influence
ADH secretion
sympathetic acticty (esp. in renal nerves)
thirst
possibly sodium appetite
NET EFFECT→ reduces pressure→ produce fluid and sodium retention→ raising circulating volume and MSFP
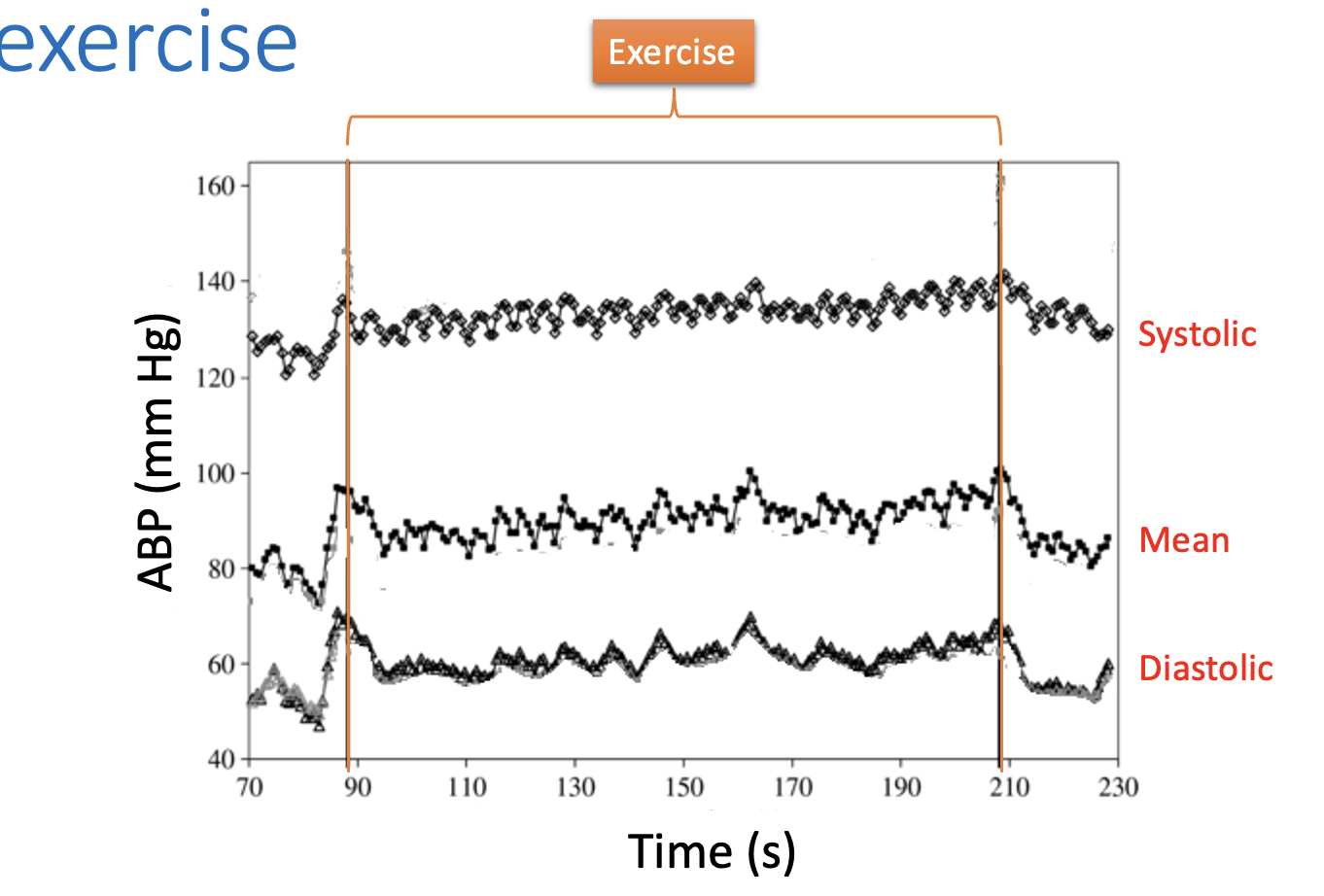
Feed-forward mechanisms to preserve ABP: why needed
common stresses on ABP regulation
do not cause detectable drops in ABP
so cannot be reliant on feedback
→ need ABP to trigger feed-forward mechansism to preserve ABP
Stresses:
exercise
stranding up
mild to moderate blood loss
Feed-forward mechanisms to preserve ABP: how can ABP drop be prevented in exercise
Inputs to medulla from:
cortex→ ‘decision’ to exerice
cerebellum→ as part of a co-ordinated motot ‘programmed’
muscle and join receeptors→ as direct response to movement
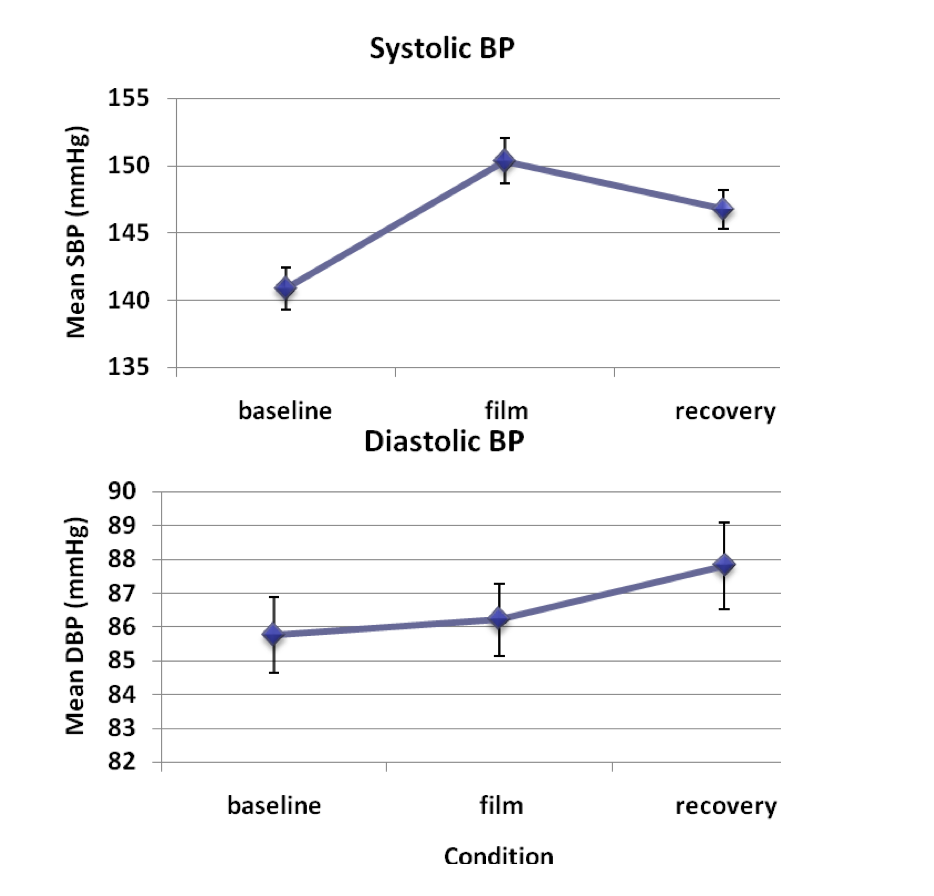
Feed-forward mechanisms to preserve ABP:other stresses that can cause rise in blood pressure
pain
emotions→ fear and anger
(from cortex and hypothalamus)
forms fight or flight preparation for dealing with whatever one is worried or frightened of
→ helping the body to deal with any incipient blood loss
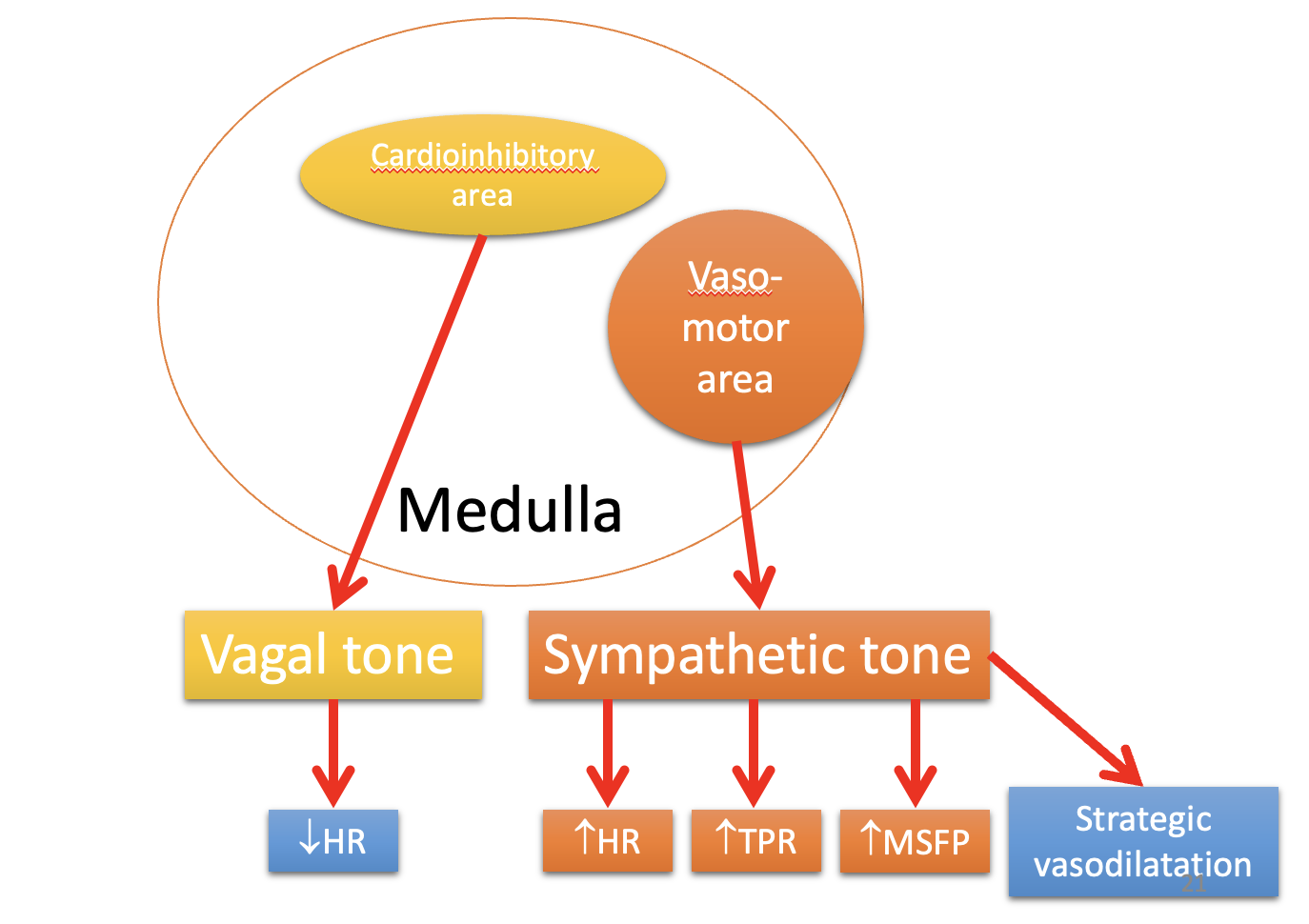
Integration of baroreceptors and feed-forard signals in the medulla
many of the feed-forward mechanisms feed into the same area of the brain
→ cardiovascular centre of the medulla
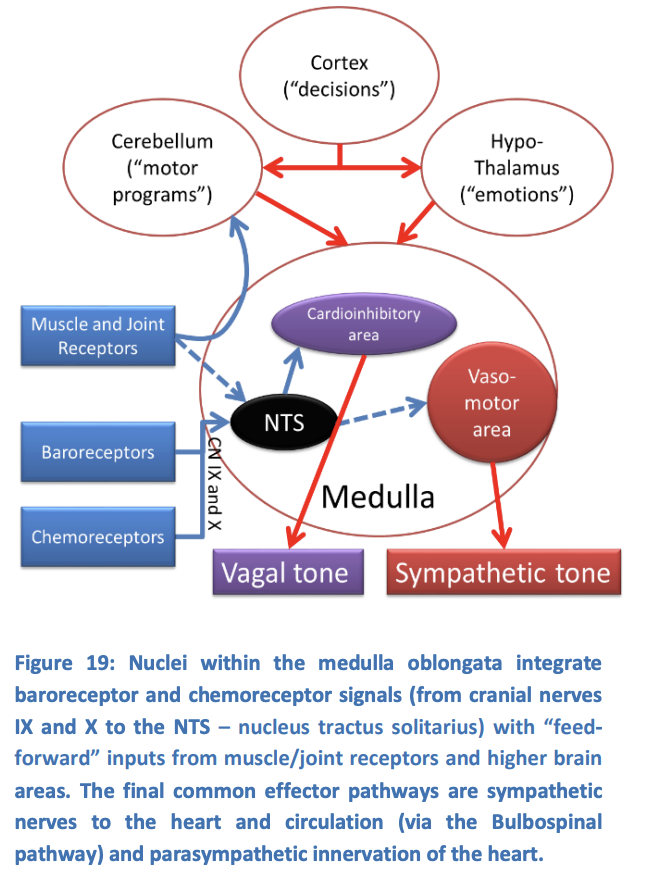
RESPONSE: medulla generates a response by…
informed sensory input from:
circulation
and more strategic inputs from higher brain centres
ENABLES→ it to control ABP via 2 major efferent pathways
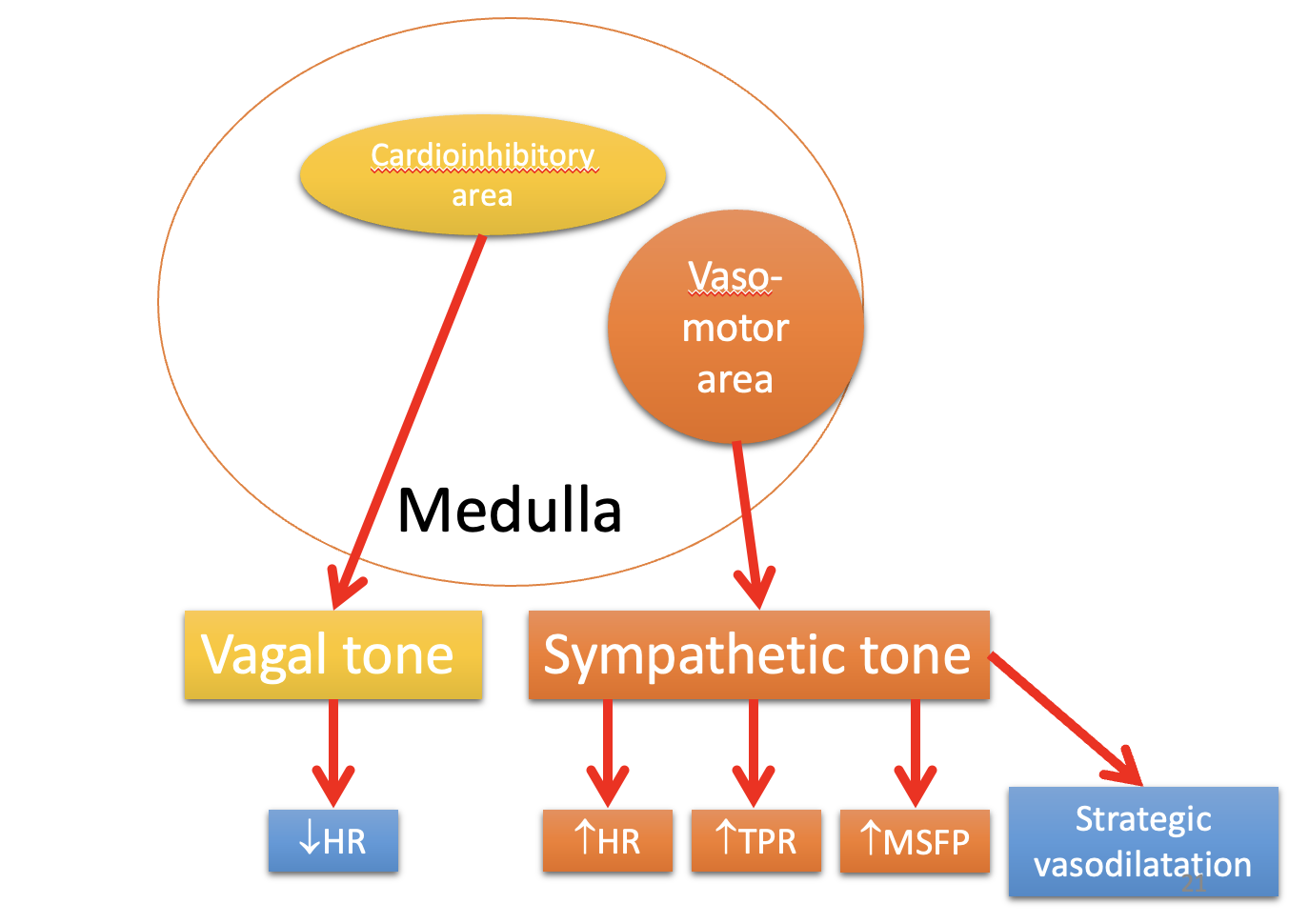
RESPONSE: ABP can be controlled via 2 major efferent pathways
sympathetic
parasymthatic
divisions of the autonomic nervous system
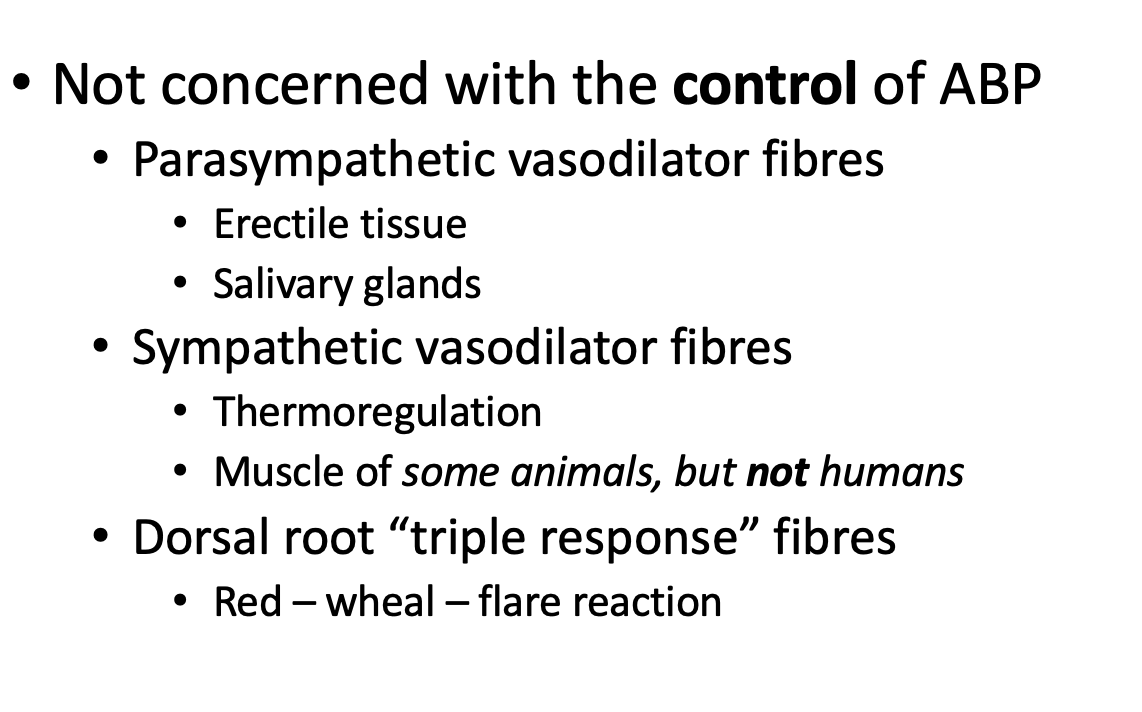
there are also other pathways that control local blood flow→ for specific processes
e.g sweating, salivation and digestion
RESPONSE: sympathetic outflows effect
act on vasculature
and the heart
also some preganglionic sympathetic fibres in the splanchhnic nerves that innervate the chromaffin cells of the adrenal medulla
RESPONSE: parasympathetic outflows effect
heart only
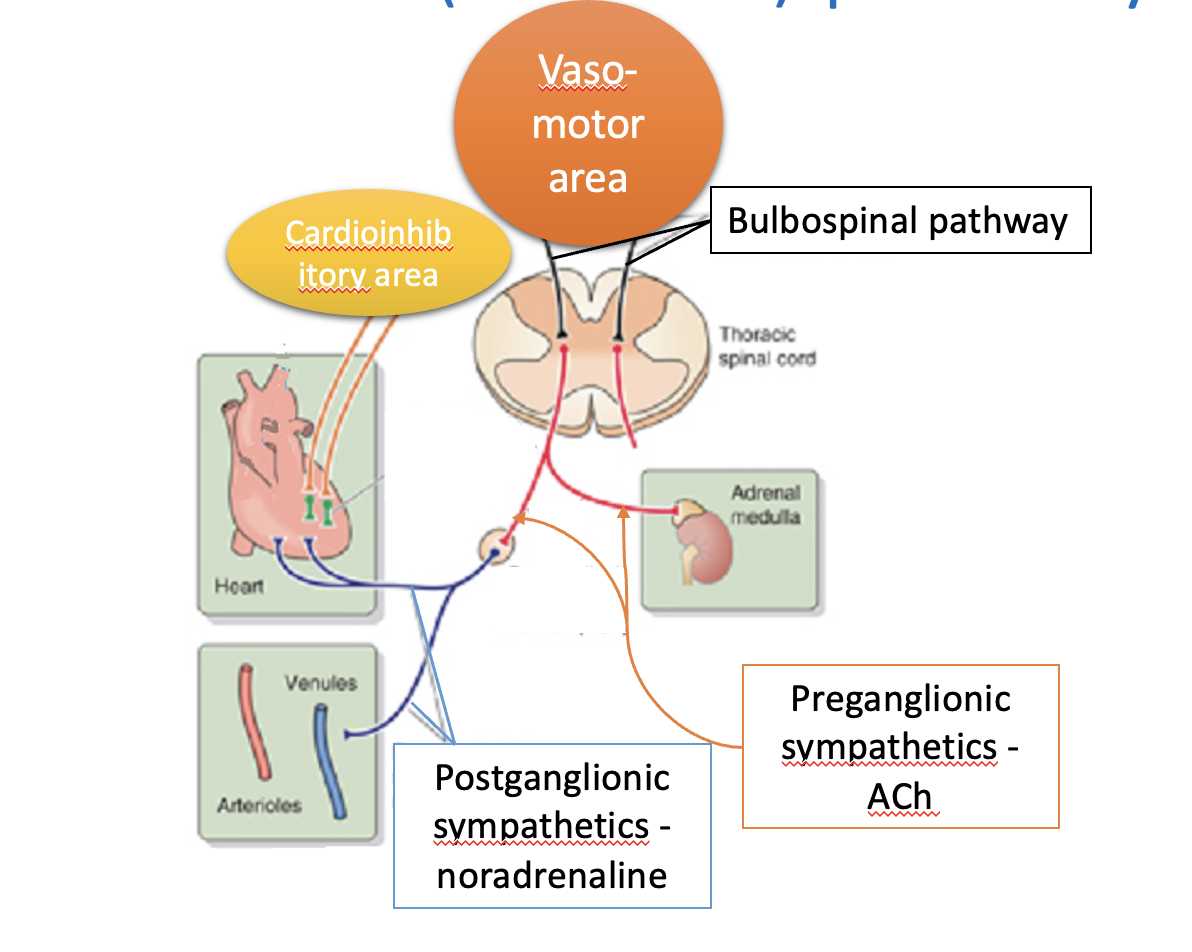
RESPONSE: sympathetic efferent pathways
bulbospinal pathways (i.e from medulla to spinal cord)→ activate pre-ganglionic pathways
primarily at glutamatergic synapses
between levels T1 and L3 of the spinal cord
these pre-ganglionic neurons synapse at nicotinic synapses to
postganglionic sympathetic neurons
found within prevertebral and paravertebral sympathetic ganglia
postganglionic sympathetic nerves involved in ABP run with large blood vessels to innervate:
muscular arteries
arteioles
veins
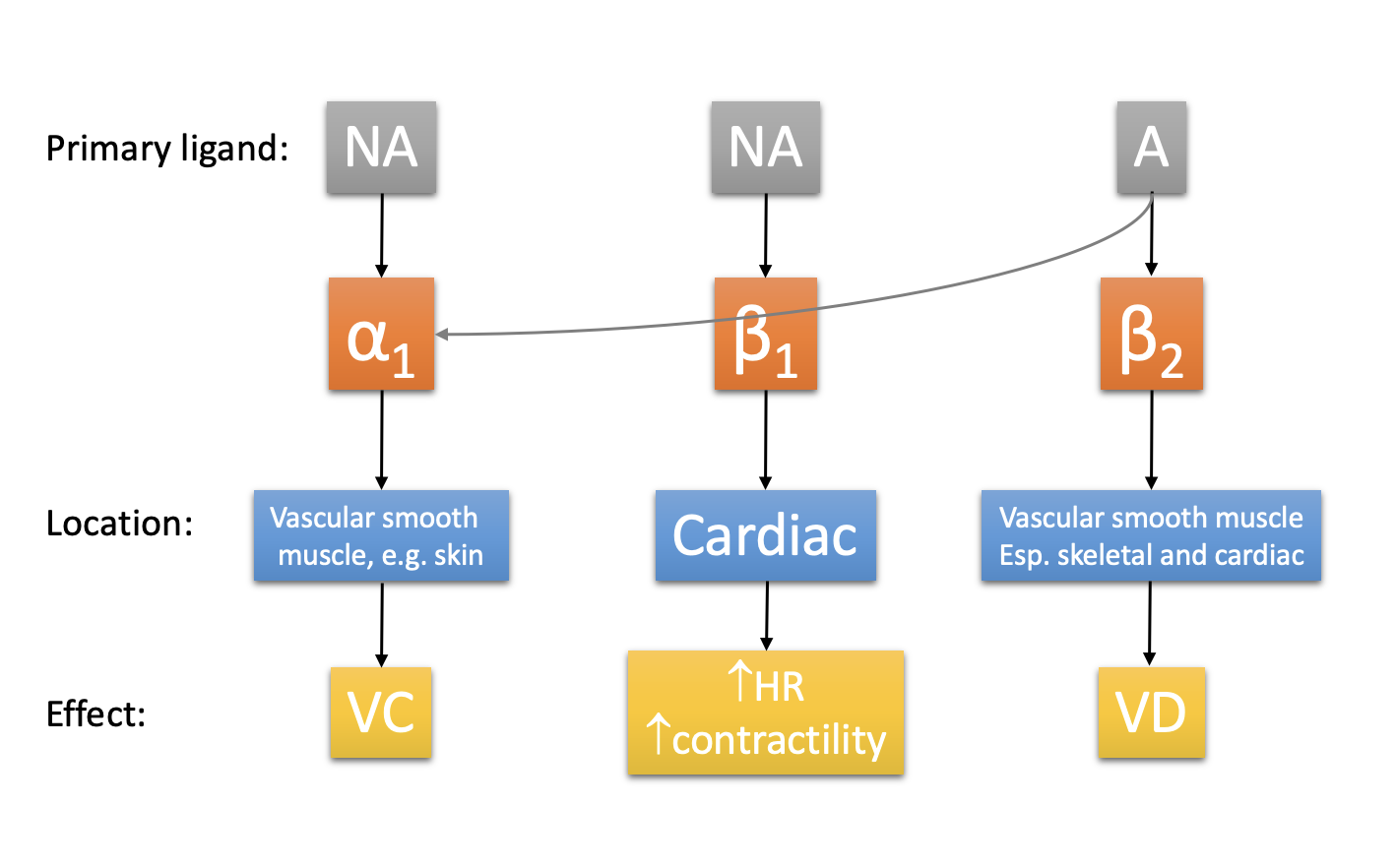
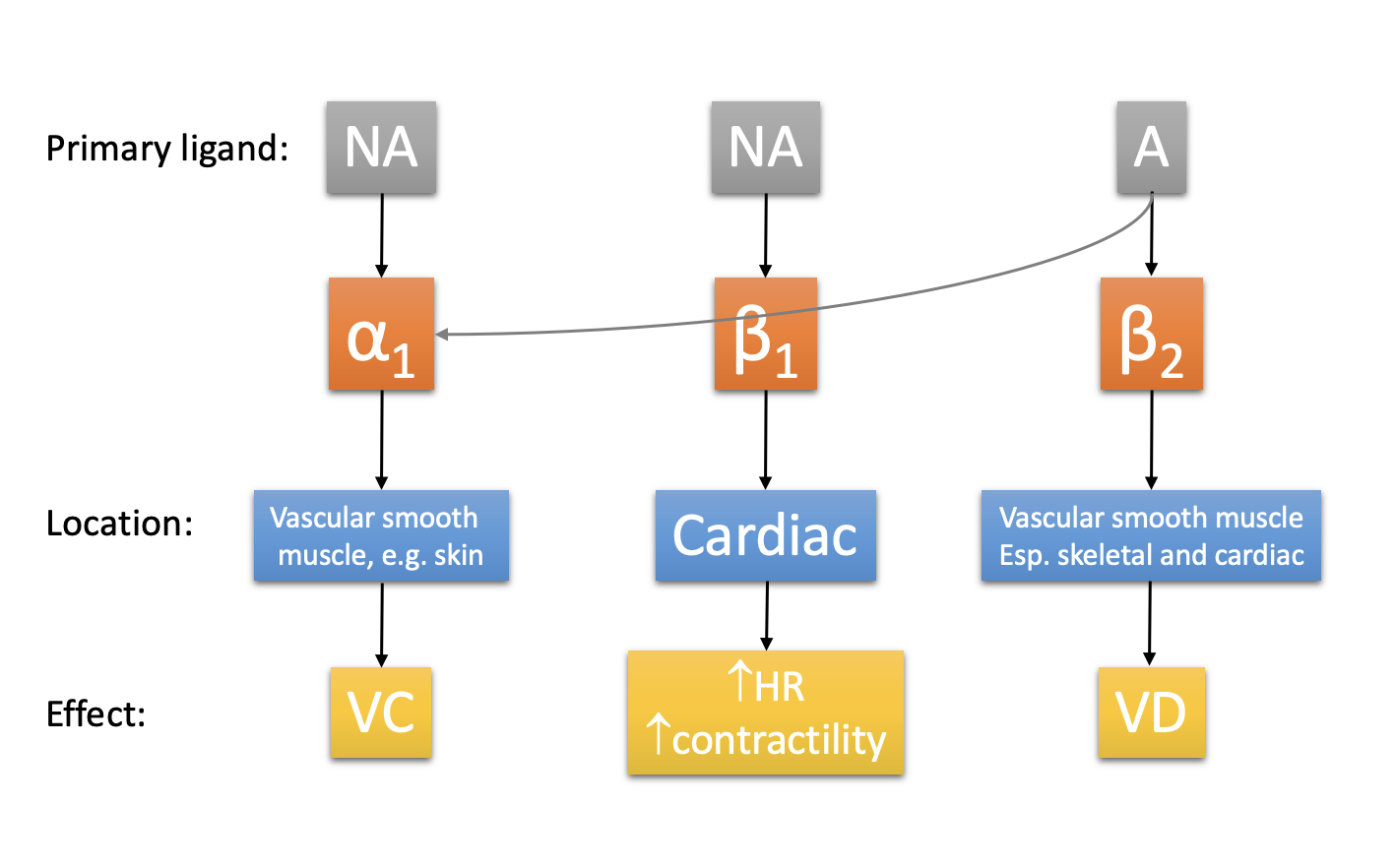
Increased sympathetic activity→
noradrenaline→ alpha 1 adrenoceptors
vasoconstriction (plus venoconstriction)
RESPONSE: effect of this sympathetic acitivsity
vasoconstriction→increases TPR
venoconstriction→ increases MSFP
redistribution of blood flow
some organs receive little significant sympathetic vasoconstrictor innervation:
arteries and arterioles supplying blain and heart
show little if any vasoconstriction during cardiovasuclar reflex responses
RESPONSE: sympathetic fibres are where
vasoconstrictor regions (blood vessels)
supply the heart
splanchic nerves
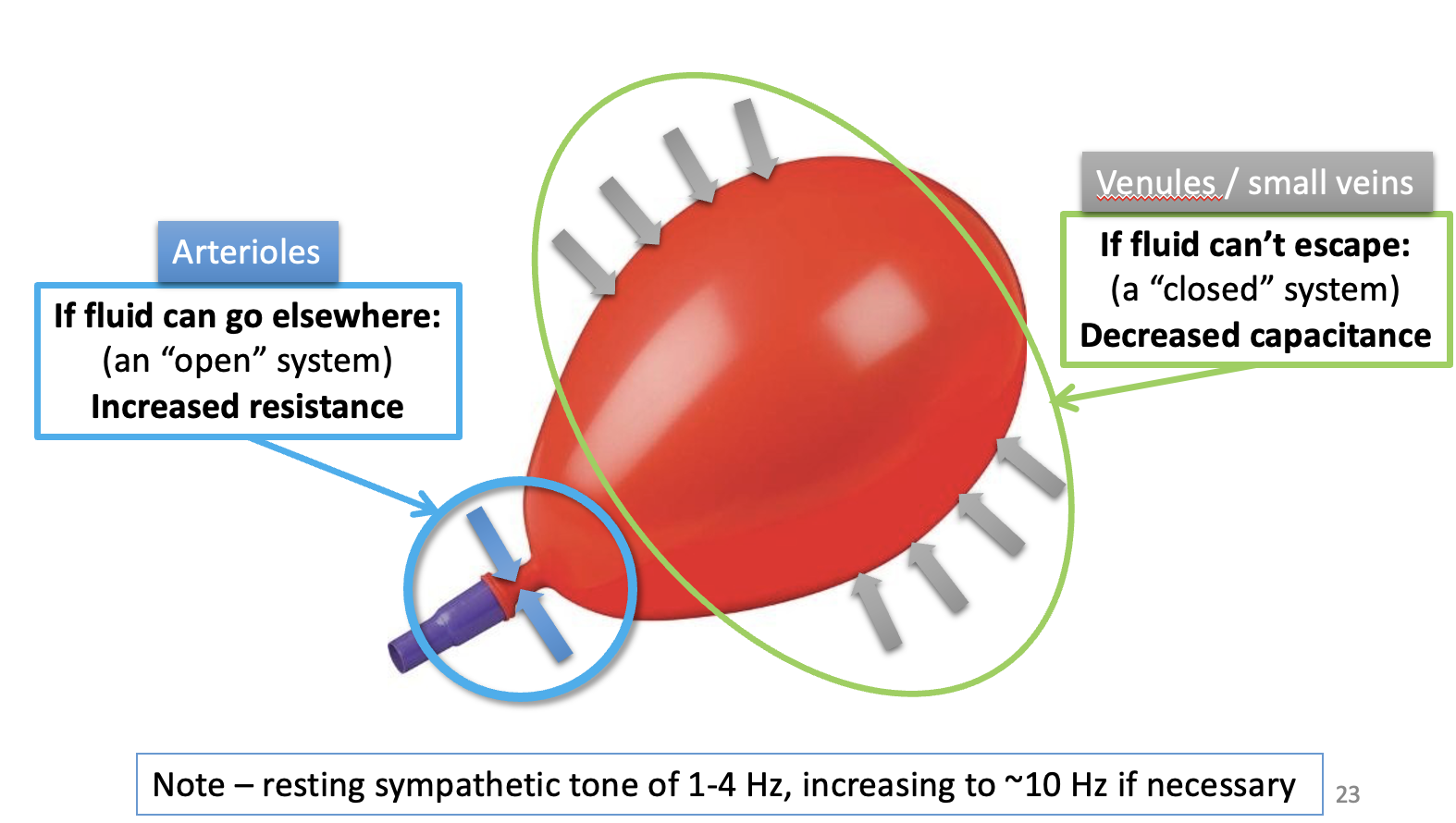
RESPONSE: 1. activity of sympathetic vasoconstrictor nerves
AT REST: tonically active
resting AP frequency of 1-4Hz
resting tone allows inhibition of sympathetic acitivity (baroreceptor reflex)
to reduce ABP if needed
IN ACTIVITY → EXTREMIS: increase activity
10 Hz
reduce blood flow to some tissues to almost 0
RESPONSE: 1. why useful to have resting sympathetic tone
resting tone allows inhibition of sympathetic acitivity (baroreceptor reflex)
→ to reduce ABP if needed
e.g spinal cord damage above T1 causes severe and rapid drop in blood pressure
by abolishing this resting sympathetic outflow
RESPONSE: 2. sympathetic fibres in the heart and effect
Cardiac accelerator nerves
Innervate the:
SA node
Atria
Ventricles
at rest→ have a low resting frequency
EFFECT: increase both heart rate and contracility
RESPONSE: 3. activity of splanchnia nerves
innervate chromaffin cells in adrenal medulla
stimulates adrenaline release into circulation
acts on heart and vasculature
in broadly similar manner to direct sympathetic innervation
via alpha 1 receptors
however…→ some tissues have different receptors
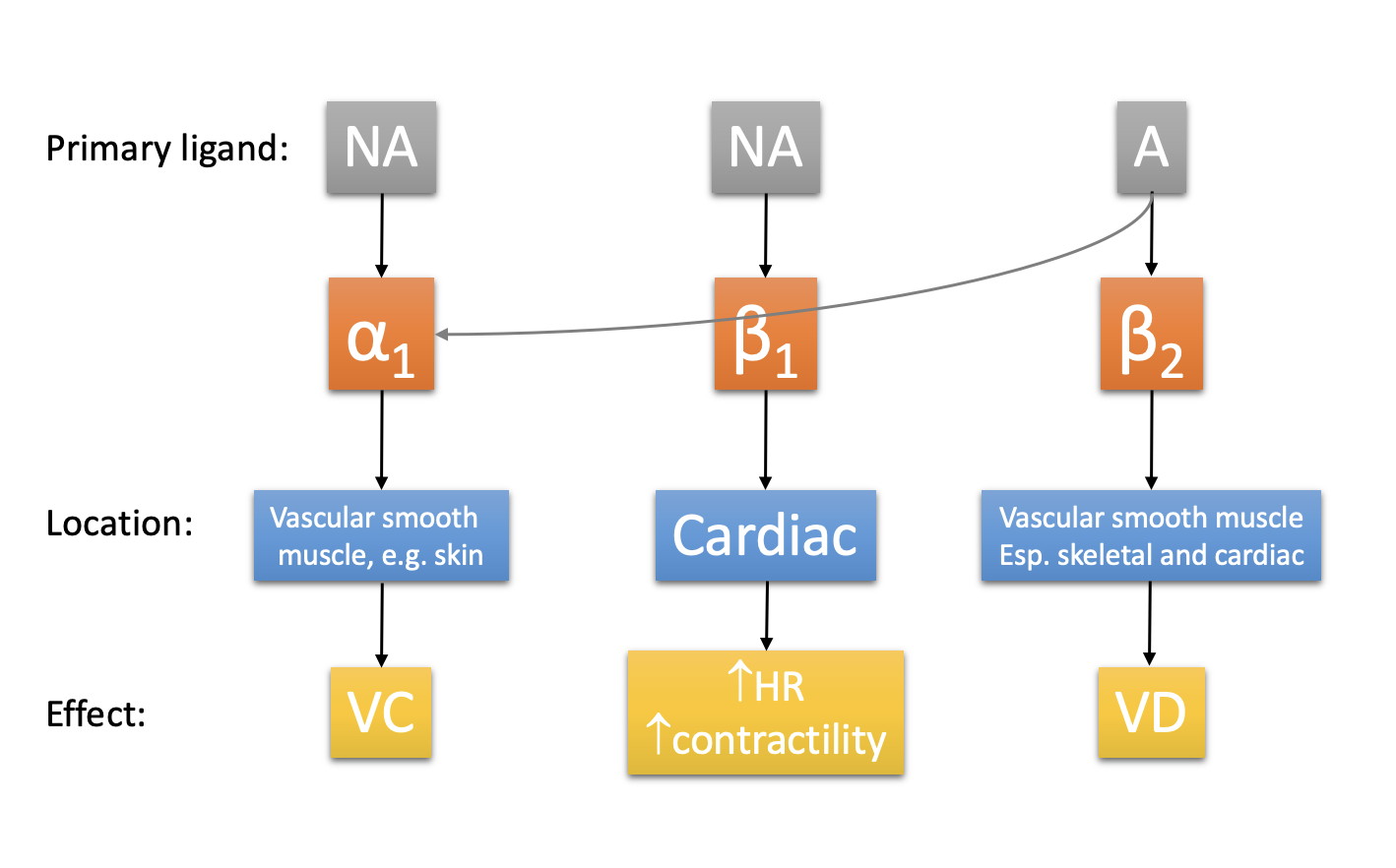
RESPONSE: 3. activity of splanchnia nerves continued (different different receptors in different tissues
coronary blood vessels and skeletal muscle
more beta2 than alpha 1 receptors
beta 2 receptors trigger vasodilatation
increasing coronary and skeletal muscle blood flow
note: noradrenaline from sympathetic nerves primarily acts on alpha 1 receptors
allows skeletal muscle blood flow to be limited if necessary
RESPONSE: Parasympathetic afferents pathway
vagus nerve innervates SA node, AV noe and cardiac conducting system
activity slows conduction through the heart
lengthens cardiac cycle
does not influence force
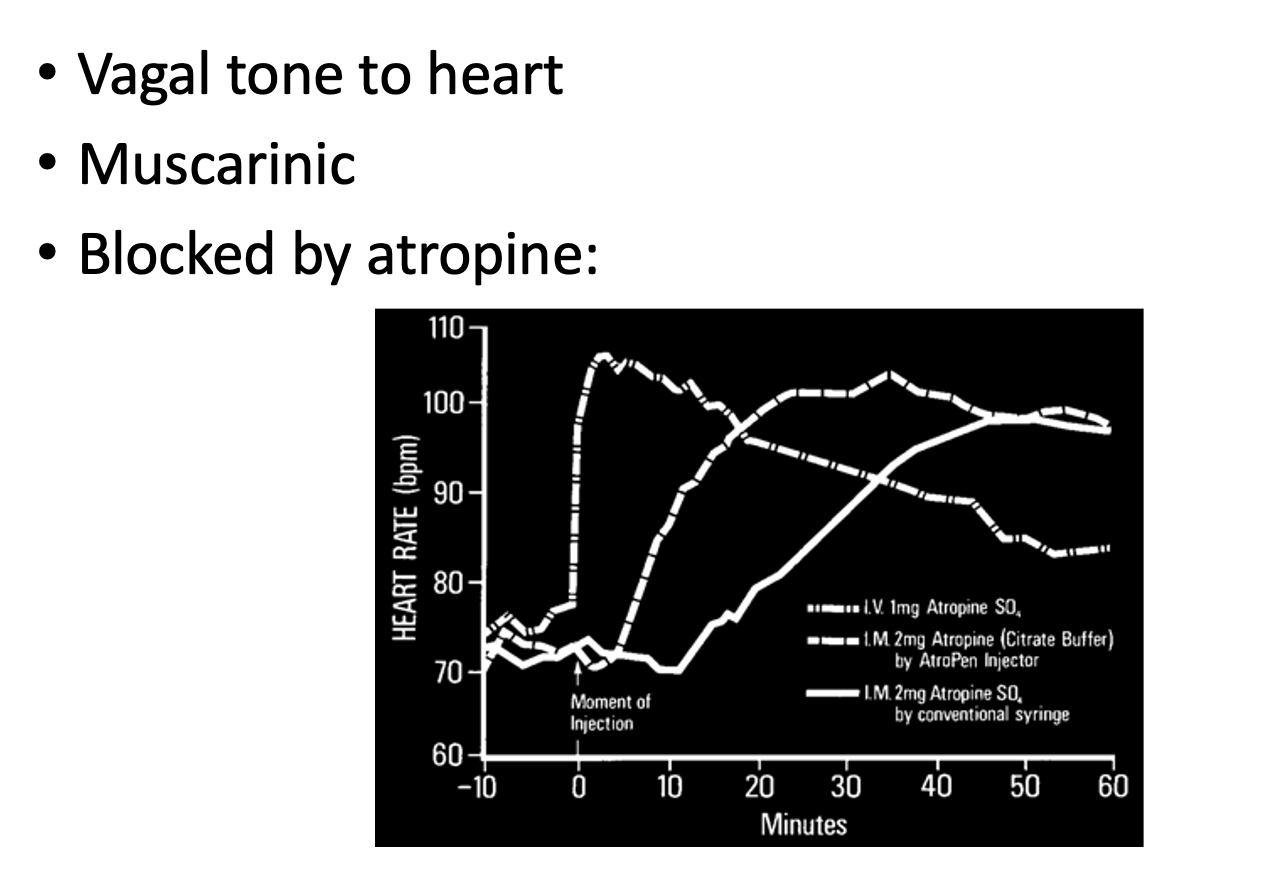
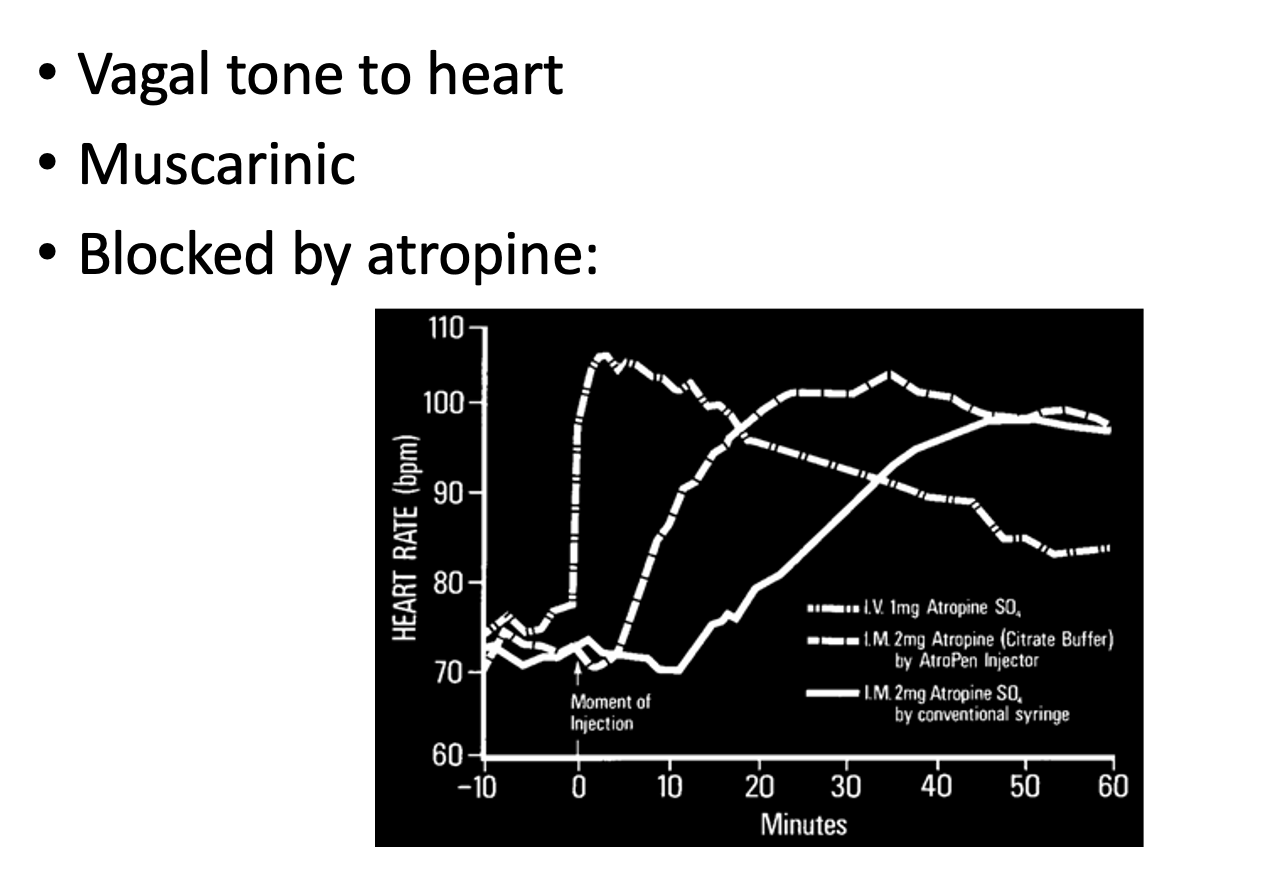
RESPONSE: vagal supply to the heart shows rate parasympathetic pathway because…
shows tonic activity
THEREFORE:
inhibition of the vagus nerve at rest (using atropine
significantly Accelerates the heart rate
Integration and effectiveness of circulatory control: why are there many challenges to blood pressure regulation in everyday life
Diverse acitivties
running, digestion, sweating and thinking
require blood flow to specific organs/sysms
NEED local vasodilation
THEREFORE: the resultant fall in TPR can be very large:
5 or 6 fold in whole-body intensive exercise
YET: mean ABP stays relatively constant
Integration and effectiveness of circulatory control: Since ABP=CO x TPR→ anyfall in TPR would
produce fall in ABP
UNLESS
there is an adequate response
What can this adequate response be?
small adjustments e.g by sympathetic vasoconstriction of
blood vessels
Some tissues:→ recieve more blood that is required to meet their metabolic demands at rest
skeletal muscle
skin
gastrointestinal tract
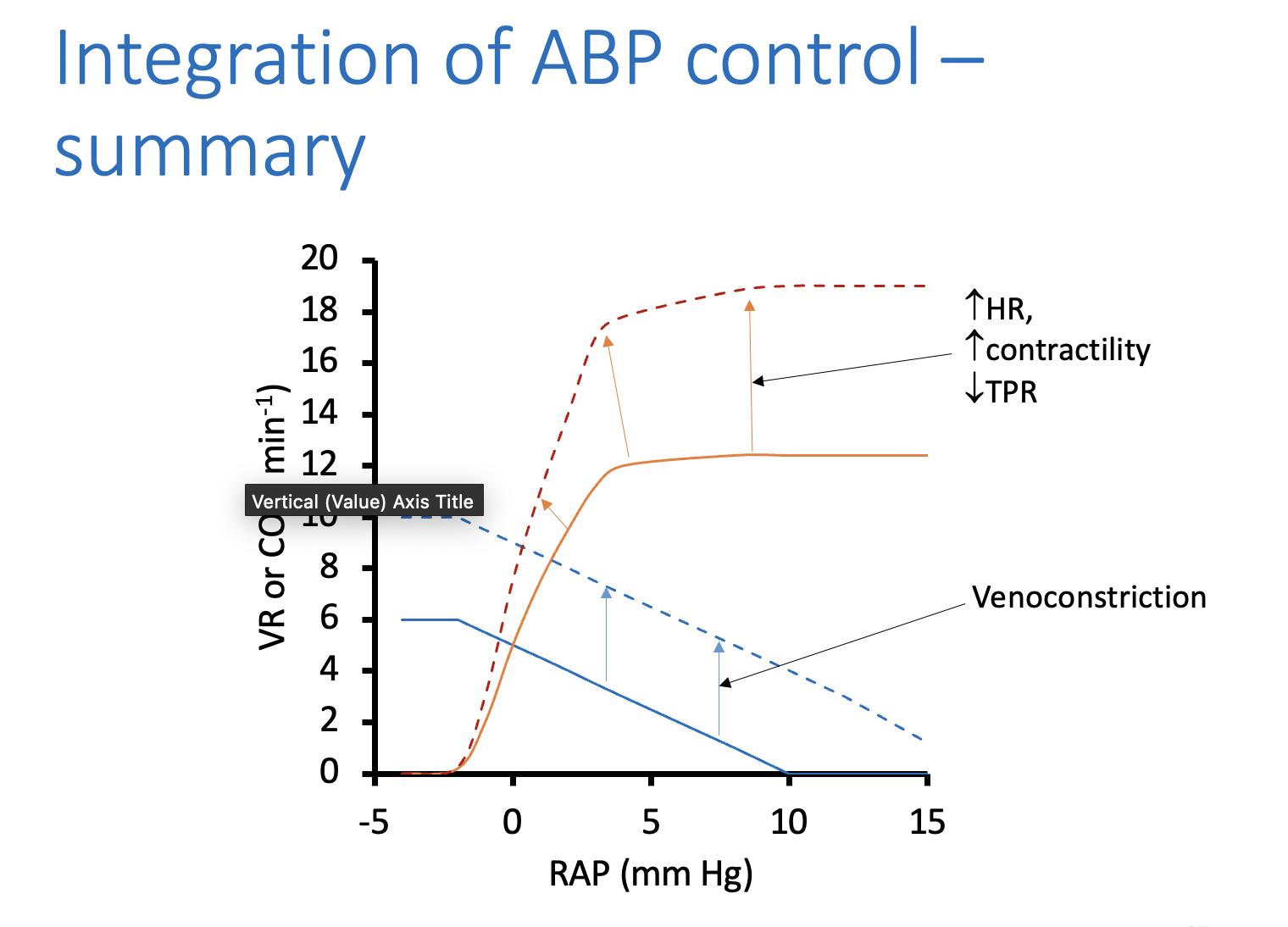
BUT what about significant falls in TPR
→ demands increase in CO
requires:
sympathetic venoconstriction to increase MSFP
in concert with
Reduced vagal and increased sympathetic stimulation of the heart
to incrase heart rate and contracility
ensuring raised MSFP produces a rise in CO without necessitating an increased RAP
TOGETHER→
increase CO
MAINTAIN mean ABP
This lecture is about short-term control of blood pressure→ during longer term…
circulating volume is a criticcal determinant of MSFP
HENCE→ ABP
Other efferent pathways affectingblood flow
Congestive cardiac failure: what is the heart failing to do
In severe, end-stage heart failure:
failture adequatley perfuse organs
resulting in organ failture
eventual death if untreated
In less severse heart failure:
necessary to think more carefully about heart’s precise role
Congestive cardiac failure: Hearts basic role and basic heart failture
Role: pump blood from veins→ arteries
failure:
implies that artrial pressure is too high
arterial pressure is too low
Congestive cardiac failure: But what does ‘too high’ Atrial pressure mean
Too high atrial pressure
should be close to 0
if higher→ impedes venous return
raise capillary pressures
non failing heat by Starling mechanism→ maintains RAP close to 0
Congestive cardiac failure: Too low ABP meaning
more complex because it is common to find symptoms of heart failture and hypertension in the same patient
heart failture develops when ABP is lower than the set point and cannot be raised
Congestive cardiac failure: how does the body normally respond to lower ABP
As it does a haemorrhage:
increased sympathetic drive
venoconstriction
arteriolar vasoconstrction
renal responses (retention of fluid)
THIS CAUSES:
raise in TPR and MSFP
Congestive cardiac failure: Effect of raising TPR and MSFP
normally→ TPR does not influence CO (starling mechanism)
but this may not be true in failing heart:
maintaining CO with increased TPR requires an increase in cardiac worka
similarly
CO is normally limited by the heart
THEREFORE
raising MSFP will not produce a significant increase in CO
→ INSTEAD: cause atrial pressure to rise
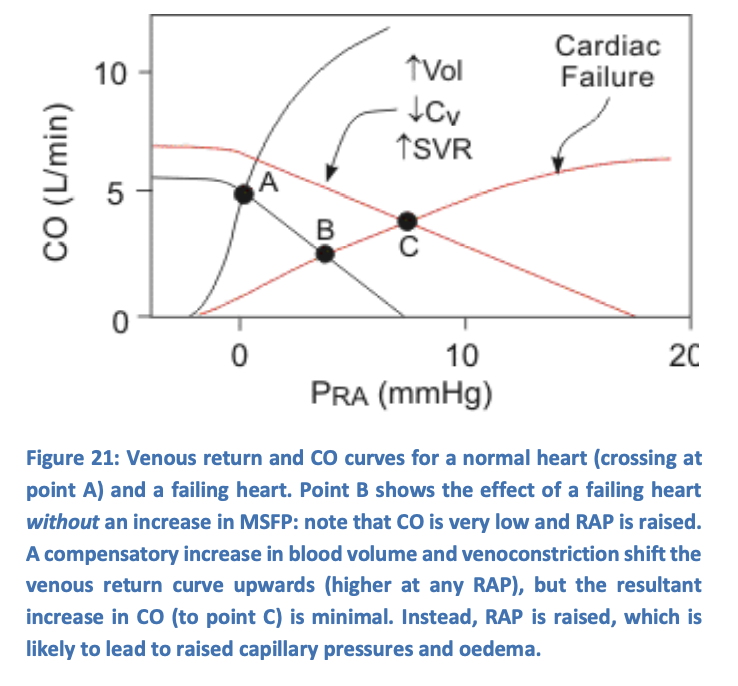
Congestive cardiac failure: symptoms of heart failture primarily result from
inability to adequately increase CO
reduces exercise capacity
may induce feelings of fatigue
increased atrial pressure
implies raised venous pressures
causes oedema:
peripheral oedema in right-sided heart hailture
pulmonary oedema in left-sided hart failture
Congestive cardiac failure: Need to understand physiology of heart failture to understand treatment
To improve cardiac output: (little can be done)
valve repair, pacing, coronary bypass
can treat failture resulting from valve disease, rhythm disorders and severse angiana (respectively)
To inhibit responses to low blood pressure
angiotensin converting enzyme (ACE inhibitors)
diurentics
→ produce significant symptomatic relief
lower MASFP and TPR
AS A RESULT: reduces the symptoms:
reduces oedmea nad reduce cardiac oxygen demand
perhaps even without decreasing CO!